
Post-therapeutic Response Evaluation of Patients Receiving
Percutaneous Coronary Intervention at the Regional Hospital in
Bantul, Yogyakarta
Pramitha Esha Nirmala Dewi
Department of Pharmacy Profession, Faculty of Medicine and Health Sciences, Universitas Muhammadiyah Yogyakarta,
Indonesia
Keywords: Percutaneous Coronary Intervention, Response Evaluation, Yogyakarta
Abstract: Coronary Artery Disease (CAD) is the main cause of mortality in heart disease. Its treatment involves
complex therapies, such as pharmacological Percutaneous Coronary Intervention (PCI) to widen the clogged
artery and lifestyle intervention to decrease the severity of CAD and restenosis. The complexity of the
pharmacological therapy received by CAD patients may cause Adverse Drug Reaction (ADR) events.
Therefore, this study aimed to identify the response of CAD patients after receiving PCI therapy at the
Regional Hospital in Bantul, Yogyakarta. This descriptive research used retrospective data and a total
population sampling method. The samples were CAD outpatients who had received PCI at this hospital
from January to September 2017 and met the inclusion criteria. The sample size was 65 patients. The results
showed that the responses of the CAD patients to PCI therapy included restenosis symptoms (70.77%)
(namely, one restenosis symptom (43.08%) and two restenosis symptoms (27.69%)), uncontrolled lifestyle
intervention (namely, abnormalities in total cholesterol (58.62%), LDL cholesterol (93.10%), HDL
cholesterol (72.41%), triglyceride (70.69%), blood pressure (72.22%), and HbA1c (50%)), and adverse drug
reaction (4.62%).
1 INTRODUCTION
Coronary Artery Disease (CAD) is the main cause of
mortality in heart disease (WHO, 2011). Among the
33 provinces in Indonesia, the Special Region of
Yogyakarta has the 15th highest CAD cases that
affect 16,663 people according to the basic estimate
from doctor’s diagnosis and 36,104 people based on
doctor’s diagnosis on the exhibited symptoms
(National Primary Health Research, 2013). The high
number of CAD cases is caused by the influencing
risk factors (Anwar, 2004).
According to Rilantono (2012), the principle of
CAD treatment is generally a long-term effort to
improve cardiac function and increase life
expectancy. Apart from the use of pharmacological
drugs, CAD cases can diminish with mechanical
reperfusion using Percutaneous Coronary
Intervention (PCI). PCI uses a stent (ring) to reduce
the occurrence of sudden occlusion.
Based on the statistical report published by AHA
(2014), there is an increase in PCI procedure per
10,000 population. The number raised from 37.2
procedures per 10,000 people (37.2/10,000) in 1990-
1992 to 59.2/10,000 in 2002-2004. It reached
135.1/10,000 in men of 65-75 years old and
64.0/10,000 in women from the same age group. On
the contrary, the numbers of procedures in men and
women aged ≥75 years were 128.7/10,000 and
69.0/10,000, respectively. The revascularization of
coronary blood vessels with PCI increased from
264/100,000 in 2002 to 267/100,000 in 2005. Such
increase was higher than the rise of the Coronary
Artery Bypass Grafting (CABG) procedure in the
same years, i.e., from 121/100,000 to 94/100,000.
However, PCI may cause a problem, namely the
growth of tissue within the lumen of the arteries due
to the biological response of vascular injury that
causes the narrowing of arteries and the recurrence
of clogs within six months called restenosis (Levine
et al., 2011). The incidence of restenosis after PCI is
quite high, which is up to 30% six months after the
procedure (Aaronson & Ward, 2008).
26
Dewi, P.
Post-therapeutic Response Evaluation of Patients Receiving Percutaneous Coronary Intervention at the Regional Hospital in Bantul, Yogyakarta.
DOI: 10.5220/0008238800260032
In Proceedings of the 1st Muhammadiyah International Conference on Health and Pharmaceutical Development (MICH-PhD 2018), pages 26-32
ISBN: 978-989-758-349-0
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
Apart from taking medical interventions, the risk
of CAD can be managed with obedience to a healthy
lifestyle (lifestyle intervention). After receiving a
PCI procedure, patients are always advised to apply
a healthy lifestyle to reduce future cardiovascular
events. Also, lifestyle changes may advance the
benefits of the medical therapy and revascularization
procedures (Ruß et al., 2009).
Consuming different types of drugs routinely,
CAD patients need evaluation and monitoring to
achieve effective treatment. Therefore, the
comprehension of treatment failure and adverse drug
reaction (ADR), especially in chronic diseases such
as CAD, is necessary (Depkes RI, 2009).
Accordingly, a study identifying the patients’
response to PCI procedures, including the
occurrence of restenosis symptoms afterward like
chest pain and shortness of breath, the risk factor
control (namely, total cholesterol level, LDL
cholesterol, HDL cholesterol, triglyceride level,
blood pressure, and HbA1c), and Adverse Drug
Reaction (ADR) at the Regional Hospital in Bantul,
Yogyakarta is necessarily interesting.
2 MATERIALS AND METHOD
2.1 Materials
This study used the medical records of the
outpatients at Panembahan Senopati Regional
Hospital in Bantul, Yogyakarta as the research
materials.
2.2 Methods
This descriptive study relied on the collection of
retrospective data. These data were acquired from
the medical record of the research subjects, namely
65 CAD outpatients who had received PCI
procedures at Panembahan Senopati Regional
Hospital from January to September 2017. The
research subjects were selected with a total
population sampling technique.
2.3 Data Analysis
The response of the CAD patients after receiving
PCI procedures at the hospital was analyzed
descriptively. The data were presented qualitatively
and quantitatively in percentage. The assessed
response included restenosis symptoms (i.e., chest
pain and shortness of breath), controls over the risk
factor (i.e., total cholesterol, LDL cholesterol, HDL
cholesterol, triglyceride, blood pressure, and
HbA1c), and adverse drug reaction. These responses
were identified using in-depth analysis with
references to related literature.
3 RESULTS AND DISCUSSION
3.1 Patients’ Characteristics
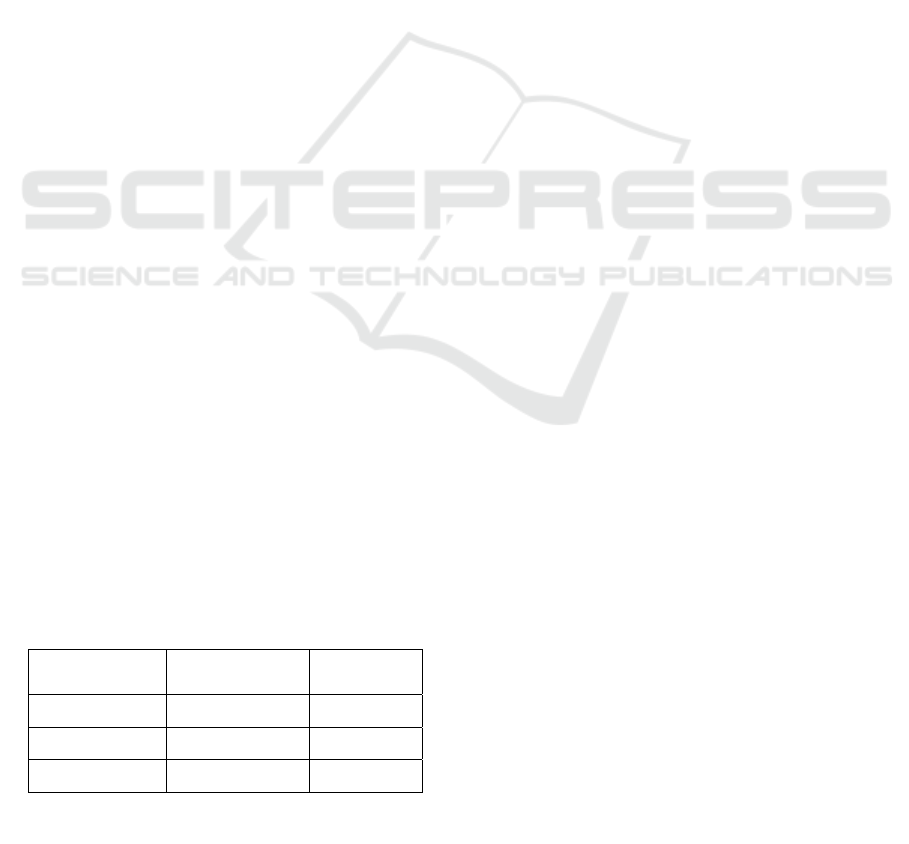
3.1.1 The Characteristics Of Patients by Sex
The characteristics of patients by sex (Table 1) were
analyzed to determine the ratio of male to female
patients. The samples consisted of 51 male
outpatients (78.46%) and 14 female outpatients
(21.54%). Compared with women, men have a
higher risk of CADs with earlier occurrences.
However, the risk of COD in women increases after
menopause. Women produce estrogen as natural
protection against hypercholesterolemia and CAD.
Also, unhealthy lifestyles, such as smoking habit,
can also increase the risk factors for men (Sallam &
Watson, 2013).
The results showed that all female CAD patients
receiving PCI had reached menopause. According to
AHA (2014), the prevalence of PCI therapy for
CAD was higher in men (83.0/10,000) than in
women (38.7/10,000) because women have more
stable angina and fewer blockages in their blood
vessels (Lundberg & King, 2012; Nowakowska et
al., 2008).
3.1.2 The Characteristics of Patients by Age
The age grouping of the CAD patients in this
research is presented in Table 2. It shows that the
incidence of CAD is dominant in the age group of ≥
45 years. This finding is in line with the theory that
states that the risk level of CAD is higher at the age
of 40 years and over (AHA, 2014).
The results of this study are in line with the
National Primary Health Research (2013), which
Table 1: The characteristics of patients by sex
Sex
N
umber of
p
atien
t
s (n)
(%)
Male 51 78.46
Female 14 21.54
Total 65 100
(Source: Primary data analysis, 2018)
Post-therapeutic Response Evaluation of Patients Receiving Percutaneous Coronary Intervention at the Regional Hospital in Bantul,
Yogyakarta
27
indicates that the prevalence of CAD based on
doctor’s diagnosis and patient’s symptoms increase
with age. The highest group found at age 65-74
years that is 2.0% and 3.6 % but decreased slightly
in the age group ≥75 years that is 1.7% and 3.2%.
This research only found seven (7) CAD patients
aged ≥75 years (10.77%). This number is probably
attributable to the life expectancy in Indonesia,
which makes the population size of the CAD
patients at this group age seem small. Based on the
Statistics Indonesia (BPS, 2016), the life expectancy
of the Indonesian population increases from one year
to another. For instance, it extended from 69.8 years
in 2010 to 70.6 years. However, it has not reached
75 years.
3.1.3 The Characteristics of Patients Based
on Comorbidities
The data obtained from the medical history showed
that all patients in this study had comorbidities,
namely dyslipidemia, hypertension, dyspepsia,
Congestive Heart Failure (CHF) and hyperuricemia
(Table 3). Some of which are identified as the risk
factors of CAD. According to Karikaturijo (2010),
CHF is one of the complications of CAD. This
condition occurs when the arterial blood vessels
narrow and, therefore, decrease the oxygen supply to
the heart. Consequently, the heart muscle weakens.
Dyslipidemia had the highest proportion in this
research. Dyslipidemia, as well as hypertension, is
the risk factor of CAD. The results showed that after
receiving PCI procedures, the CAD outpatients at
the Regional Hospital in Bantul, Yogyakarta who
had dyslipidemia also showed the symptoms of
hypertension. Dyslipidemia and hypertension are
both known to have a close relationship with the
incidence of CAD because continuous high blood
pressure in CAD patients would result in damaged
blood vessels, allowing the accumulation of fatty
plaque and eventually the blockage of the blood
vessels (Budiman et al., 2015).
The other coexisting disease in CAD patients
after the PCI therapy was dyspepsia. Suspected
polypharmacy in CAD management may cause
upper gastrointestinal disorders. Aspirin as an
antiplatelet in CAD patients can cause
gastrointestinal disturbances. Dyspepsia, nausea, and
vomiting occur in 2-6% of patients after taking
aspirin (Meylers, 2006).
The association of uric acid with the incidence of
cardiovascular disease is still controversial and
under investigation (Torpy et al., 2009). An
experimental study reveals that uric acid stimulates
the release of chemo-attractant protein-1,
interleukin-1b (IL-1b), interleukin-6 (IL-6), and
tumor necrosis factor-a (TNF-a). Therefore, uric
acid may contribute to the development of vascular
disease and atherosclerosis through pro-
inflammatory pathways (Ruggiero et al., 2006).
3.2 The Effect of Drug Use Profile on
The Cardiovascular System
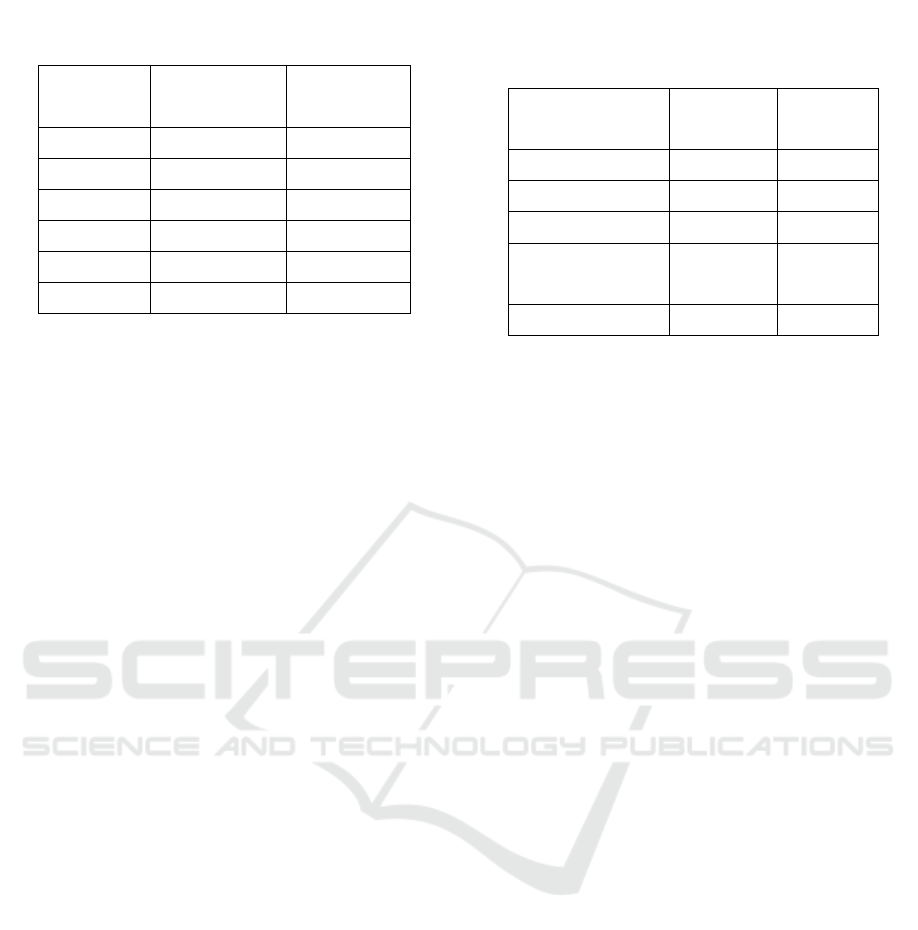
Table 4 shows that the CAD patients who have
received PCI therapy take acetylsalicylic acid,
clopidogrel, bisoprolol fumarate, candesartan, and
simvastatin. In this study, acetylsalicylic acid or
aspirin was quite largely used by the CAD patients
after receiving the therapy. For patients without
resistance or allergic to aspirin, or without bleeding
tendency, aspirin has to be given immediately to
continue their lifetime (AHA, 2011). The clinical
trials in Aaronson & Ward (2008) reveal that aspirin
at low doses can decrease infarcts and mortality by
more than 50%.
Clopidogrel has been proven as effective as
aspirin in the prevention of ischemic events in at-
risk patients. Clopidogrel and aspirin affect different
Table 2: The characteristics of patients by age
Age
(years old)
N
umber of
patients (n)
(%)
35-44 3 4.62
45-54 13 20.00
55-64 25 38.46
65-74 17 26.15
≥75 7 10.77
Total 65 100
(Source: Primary data analysis, 2018)
Table 3: The characteristics of patients based on
comorbidities
Comorbidities
N
= 65 (%)
Dyslipidemia 58 89.23
Hypertension 17 26.15
Dyspepsia 16 24.62
Congestive Heart
Failure (CHF)
10 15.38
Hyperuricemia 10 15.38
(Source: Primary data analysis, 2018)
MICH-PhD 2018 - 1st Muhammadiyah International Conference on Health and Pharmaceutical Development
28
pathways in the coagulation process. Therefore, their
combination can be administered to patients
undergoing stenting, and it has been proven to
reduce ischemic events by 20% in patients with
NSTEMI or unstable angina compared with the
single use of aspirin (Yusuf et al., 2001).
Beta blockers are used to treat hypertension,
angina, supraventricular heart arrhythmias,
myocardial infarction, and chronic heart failure
(Aaronson & Ward, 2008). A meta-analysis of 147
randomized controlled trials with 464,000 patients
proposes beta-blockers as the first-line therapy in
CAD patients. In the first two years after myocardial
infarction, beta blockers can reduce cardiovascular
events twice than other antihypertensive agents
(Law et al., 2009).
Besides beta-blockers, another widely prescribed
antihypertensive drug found in this research was
candesartan from the Angiotensin Receptor Blocker
class (ARB). Sakamoto et al. (2016) develop a
randomized controlled trial involving 1,145 patients
who received different treatments after the PCI
procedures, namely (1) candesartan plus standard
medical treatment and (2) conventional medical
treatment during the follow-up in the succeeding
three years. They prove that the administration of
candesartan soon after PCI treatment does not
improve the prognosis, but it reduces some cardiac
events for three (3) years.
Statins are the drug of choice for lowering LDL
cholesterol, and they are used up to the highest
tolerable dose to achieve targeted LDL cholesterol
concentrations (PERKI, 2013). According to Cerit et
al. (2016), patients who have stable CAD after PCI
and receive a long-term statin therapy are associated
with increased epicardial perfusion.
The description of the response of patients to
Percutaneous Coronary Intervention therapy is as
follows:
3.3 Restenosis Symptoms
The results showed that after PCI, CAD patients
could experience re-blockage (restenosis). The
restenosis symptoms observed in this research
included chest pain and dyspnea (Table 5).
Not every sampled patient in this research
exhibited the symptoms of restenosis. Nineteen (19)
patients (29.23%) had no symptoms of restenosis, 28
patients (43.08%) showed one symptom of
restenosis, and the remaining 18 patients (27.69%)
had two symptoms of restenosis. According to
Aaronson & Ward (2008), restenosis can occur in
30% of CAD patients within six months after the
PCI procedure. The results of this research showed
that CAD patients experienced the symptoms of
restenosis within ≤6 months (23.08%) and >6
months (76.92%) after the procedure.
3.4 Lifestyle Intervention
The goal of lifestyle intervention is to prevent
cardiovascular complications in patients with DM,
cholesterol, and hypertension to improve their
Table 4: The drug use
p
rofile
Type of drugs N= 493 (%)
Acetylsalicylic
acid
59 11.97
Clopidogrel 47 9.53
Bisoprolol
fumara
t
e
55 11.16
Candesartan 45 9.13
Simvastatin 60 12.17
O
t
hers 227 46.04
(Source: Primary data analysis, 2018)
Table 5: The incidence of restenosis
The incidence of
restenosis
Number of
patients (n)
(%)
N
o restenosis 19 29.2
1 symptom
(chest pain or
d
y
spnea)
28 43.1
2 symptoms
(chest pain and
d
y
spnea)
18 27.7
Total 65 100
(Source: Primary data analysis, 2018)
Table 6: The distribution of CAD patients with
dyslipidemia disease according to total cholesterol
levels post PCI therapy
Total cholesterol
N
= 58 (%)
N
ormal
(<200 mg/dL)
24 41.38
Abnormal
(≥200 mg/dL
34 58.62
(Source: Primary data analysis, 2018)
Post-therapeutic Response Evaluation of Patients Receiving Percutaneous Coronary Intervention at the Regional Hospital in Bantul,
Yogyakarta
29
glycemic control and reduce the occurrence of
dyslipidemia and hypertension (Blumenthal et al.,
2011). The following tables show the results of the
laboratory analysis of CAD patients with the
comorbidities of dyslipidemia, hypertension, and
diabetes mellitus (DM).
Tables 6, 7, 8, and 9 show that after receiving the
pharmacological and PCI procedures, the number of
patients with abnormal cholesterol levels is higher
than the normal ones. This condition indicates that
not every sampled patient in this research adheres to
the suggested pharmacological therapy and lifestyle.
According to Sari & Husna (2016), there is a
relationship between lifestyle and the ability to
control cholesterol in patients with
hypercholesterolemia. Unhealthy lifestyles may
induce high cholesterol levels. The choice of
lifestyle is influenced by the prominent development
of the era, such as the emergence of an environment
that somehow enables excessive consumption of
junk food, low physical activity, and lack of health
awareness. According to the ESC/EAS Guidelines
for the Management of Dyslipidaemias (ESC, 2011),
lifestyle interventions, including a dietary plan that
reduces saturated fatty acids, have a major impact on
LDL levels. An additional of 1% energy from the
saturated fat increases LDL levels by 0.02-0.04
mmol/L or 0.8-1.6 mg/dL.
The recommendations of the Eighth Joint
National Committee (JNC 8) on the blood pressure
targets for hypertensive patients without diabetes
mellitus and Chronic Kidney Disease (CKD) aged
<60 years and ≥60 years are <140/90 mmHg and
<150/90 mmHg, respectively. Meanwhile, in
hypertensive patients with diabetes mellitus or CKD,
the targeted blood pressure is different, that is
<140/90 mmHg (James et al., 2013).
In this research, there were 17 patients with
hypertension and 1 patient with Hypertensive Heart
Disease (HHD). Among these 18 patients, 13
(72.22%) had blood pressure above the target.
Meanwhile, the remaining five patients had normal
blood pressure (27.78%) (Table 10). This finding
indicates that not every patient in this research
adheres to the suggested pharmacological therapy
and lifestyle.
Lifestyle interventions for hypertensive patients
include weight loss for overweight or obese patients,
the reduction of salt intake to 1,5 grams per day, and
Table 7: The distribution of CAD
p
atients with
dyslipidemia disease according to LDL cholesterol
levels post PCI therapy
LDL cholesterol N= 58 (%)
N
ormal
(<100 mg/dL)
4 6.9
Abnormal
(≥100 mg/dL)
54 93.1
(Source: Primary data analysis, 2018).
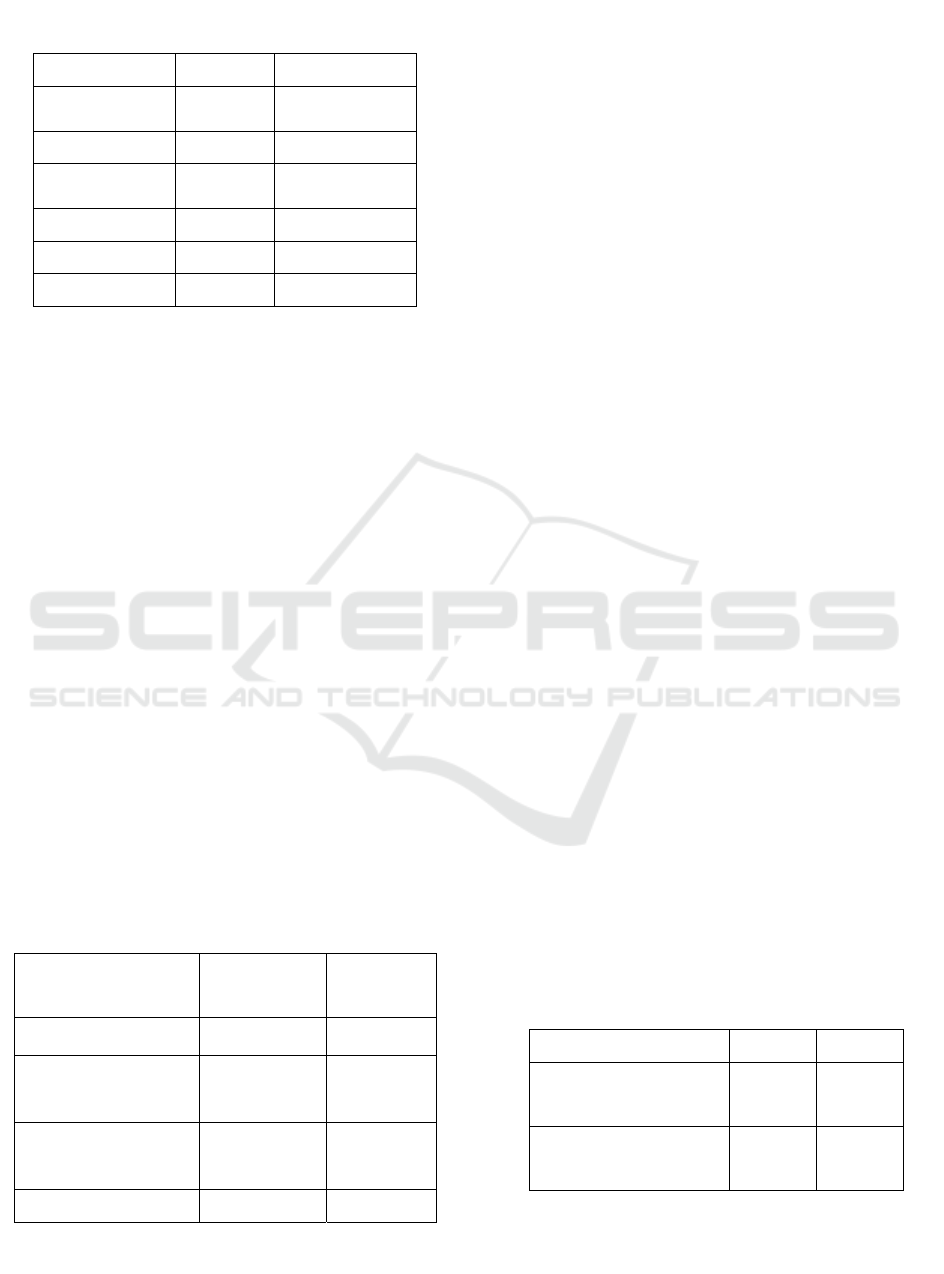
Table 9: The distribution of CAD
p
atients with
dyslipidemia disease according to triglycerides post
PCI therapy
Triglycerides
N
= 58 (%)
N
ormal
(<150 mg/dL)
17 29.31
Abnormal
(≥150 mg/dL)
41 70.69
(
Source: Primar
y
data anal
y
sis
,
2018
)
Table 8: The distribution of CAD
p
atients with
dyslipidemia disease according to HDL cholesterol
levels post PCI therapy
HDL cholesterol N= 58 (%)
Normal
(≥40 mg/dL)
16 27.59
Abnormal
(<40 m/dL)
42 72.41
(Source: Primary data analysis, 2018)
Table 10: The distribution of CAD
p
atients with
hypertension according to blood pressure levels post
PCI therapy
Blood pressure
levels
N
= 18 (%)
N
ormal 5 27.78
Abnormal 13 72.22
(
Source: Primar
y
data anal
y
sis, 2018
)
Table 11: The distribution of CAD
p
atients with
diabetes mellitus disease according to HbA1c post
PCI therapy
HbA1c
N
= 8 (%)
N
ormal
(<7.0 %)
4 50
Abnormal
(≥7.0 %)
4 50
(Source: Primary data analysis, 2018)
MICH-PhD 2018 - 1st Muhammadiyah International Conference on Health and Pharmaceutical Development
30
regular physical activity. They also advise more
consumption of fruits and vegetables (300 grams)
and the reduction of saturated fat and cholesterol
intake (ESC, 2016).
Based on the results of this research, eight CAD
patients had Diabetes Mellitus (DM) after PCI
therapy. Half of them had normal HbA1c
(hemoglobin glycate) level, whereas the remaining
50% had abnormal HbA1c levels (Table 11). This
finding indicates that not every patient in this
research adheres to the recommended
pharmacological therapy and lifestyle.
According to the consensus PERKENI (2015),
physical exercise is one of the pillars in the
management of DM if not accompanied by
nephropathy. It is useful for maintaining the body’s
fitness and improving insulin sensitivity. It is not the
only factor that controls the HbA1c levels of DM
patients, but a good dietary intake (as recommended)
and oral hypoglycemic drugs or insulin also play a
role in shaping blood sugar levels.
3.5 Pharmacological Management
In this study, three (3) patients experienced the side
effects of Adverse Drug Reactions (ADRs) (Table
12), namely cough, as induced by the administration
of captopril and ramipril.
Captopril and ramipril are from the class of
Angiotensin Converting Enzyme Inhibitor (ACEi)
drug that inhibits Renin-Angiotensin System (RAS).
ACE is an important enzyme in the renin-
angiotensin system that converts angiotensin I to
angiotensin II on the surface of endothelial cells.
Angiotensin II is proven to cause vasoconstriction in
blood vessels. The inhibition of this enzyme can lead
to vasodilation and, consequently, decreased blood
pressure (Herman & Bhimji, 2017).
In addition to lowering blood pressure with the
inhibition of angiotensin II formation, ACEi also
inhibits bradykinin degradation and stimulates the
synthesis of other vasodilators, such as prostaglandin
E2 and prostacyclin. Bradykinin increases in the
body, accumulates in the respiratory tract, and then
stimulates the incidence of a dry cough (Zamora &
Parodi, 2010; Nishio et al., 2011).
4 CONCLUSIONS
Based on the results of this research, several
responses of CAD patients to PCI therapy include
restenosis symptoms (70.77%)―consisting of 1
restenosis symptom (43.08%) and 2 restenosis
symptoms (27.69%), uncontrolled lifestyle
intervention―such as abnormalities in total
cholesterol (58.62%), LDL cholesterol (93.10%),
HDL cholesterol (72.41%), triglyceride (70.69%),
blood pressure (72.22%), and HbA1c (50%), and
adverse drug reaction (4.62%).
ACKNOWLEDGMENTS
This research was supported by Universitas
Muhammadiyah Yogyakarta, Indonesia. The author
would like to thank the research assistant, Monia
Agni Wiyatami, for her insight and time that greatly
assisted the research.
REFERENCES
American Heart Association (AHA), 2011, 2011
ACCF/AHA/SCAI Guideline for Percutaneous
Coronary Intervention, Available at:
http://circ.ahajournals.org/content/124/23/e574
American Heart Association (AHA), 2014, Heart Disease
and Stroke Statistics-2014 Update, Available at:
http://ahajournal.org.com [Accessed 24 May 2018]
Anwar, B, 2004, Dislipidemia sebagai Faktor Risiko
Penyakit Jantung Koroner, Bachelor Thesis,
Universitas Sumatera Utara, Sumatera Utara.
Aaronson, PI, & Ward, JPT, 2008, At a glance: Sistem
kardiovaskular, Jakarta: Penerbit Erlangga, p. 75, 93
Badan Pusat Statistik (BPS), 2016, Angka Harapan Hidup
Indonesia 2010-2014, Available at:
https://databoks.katadata.co.id/datapublish/2016/08/08
/angka-harapan-hidup-indonesia-2010-2014 [Accessed
15 April 2018]
Blumenthal, RS, Foody, JM, & Wong, ND, 2011,
Preventive Cardiology: A Companion to Braunwald's
Heart Disease, Philadelphia: Elsevier/Saunders, p. 374
Budiman, Sihombing, R, & Pradina, P, 2015, Hubungan
Dislipidemia, Hipertensi Dan Diabetes Melitus
Dengan Kejadian Infark Miokard Akut, Andalas
Journal of Public Health, 10(1)
Cerit, L, Duygu, H, Gulsen, K, & Gunsel, A, 2016, Effect
of Statins on Coronary Blood Flow After Percutaneous
Coronary Intervention in Patients With Stable
Coronary Artery Disease, Neth Heart J, DOI
Table 12: The incidence of ADR
The incidence
of ADR
Number of
patients (n)
(%)
No side effects 62 95.38
Side effects 3 4.62
Total 65 100
(Source: Primary data analysis, 2018)
Post-therapeutic Response Evaluation of Patients Receiving Percutaneous Coronary Intervention at the Regional Hospital in Bantul,
Yogyakarta
31

10,1007/s12471-016-0883-x
Depkes RI, 2009, Sistem Kesehatan Nasional, Jakarta.
Europian Society of Cardiology (ESC), 2011, ESC/EAS
Guidelines for the Management of Dyslipidaemias,
European Heart Journal, 32, pp. 1769-1818,
doi:10,1093/eurheartj/ehr158
Europian Society of Cardiology (ESC), 2016, European
Guidelines on Cardiovascular Disease Prevention in
Clinical Practice, European Heart Journal,
DOI:10,1093/eurheartj/ehw106
Herman, LL, & Bhimji, SS, 2017, Angiotensin Converting
Enzyme Inhibitors (ACEI), In: StatPearls [Internet],
Treasure Island (FL): StatPearls Publishing; 2018 Jan-,
Available at:
https://www,ncbi,nlm,nih,gov/books/NBK431051/
James PA, Oparil S, Carter BL, et al. 2013. Evidence-
based guideline for the management of high blood
pressure in adults: report from the panel members
appointed to the Eighth Joint National Committee
(JNC 8). JAMA; 311:507 – 520
Karikaturijo, 2010, Penyakit Jantung Koroner, Universitas
Pembangunan Nasional Veteran, Jakarta.
Law, MR, Morris, JK, & Wald, NJ, 2009, Use of Blood
Pressure Lowering Drugs in The Prevention of
Cardiovascular Disease: Meta-Analysis of 147
Randomised Trials in The Context of Expectations
From Prospective Epidemiological Studies, BMJ,
338:b1665.
Levine, GN, Bates, ER, Blankenship, JC, Bailey, SR,
Bittl, JA, Cercek, B, et al., 2011, 2011
ACCF/AHA/SCAI guideline for percutaneous
coronary intervention, J Am Coll Cardiol 58(24), pp.
2550-83.
Lundberg, G & King, S, 2012, Coronary
Revascularization in Woman, Clin Cardiol, 35(3), pp.
156-9, DOI: 10.1002/clc.21976.
Meylers, 2006, Side Effects of Drugs, 15th ed, Oxford:
Elsevier
Nishio, K, Kashiki, S, Tachibana, H, & Kobayashi, Y,
2011, Angiotensin-converting enzyme and bradykinin
gene polymorphisms and cough: A meta-analysis,
World Journal of Cardiology, 3 (10), pp. 329-336
Nowakowska, AA, Grabczewska, Z, Koziński, M,
Sukiennik, A, Swiatkiewicz, I, Grześk, G, Radomski,
M, Bogdan, M, Kochman, W, & Kubica, J, 2008,
Gender differences and in-hospital mortality in
patients undergoing percutaneous coronary
interventions, Kardio Pol, 66(6), pp. 632-9, discussion
640-1.
Perhimpunan Dokter Spesialis Kardiovaskuler Indonesia
(PERKI), 2015, Pedoman Tatalaksana Sindrom
Koroner Akut, Jilid 3, Jakarta: Jurnal Kardiologi
Indonesia.
Rilantono, LI, 2012, 5 Rahasia Penyakit Kardiovaskular
(PKV), Jakarta: Badan Penerbit Fakultas Kedokteran
Universitas Indonesia, pp. 132, 138, 168, 185
Riset Kesehatan Dasar (National Primary Health
Research), 2013, Badan Penelitian dan
Pengembangan Kesehatan Kementerian RI Tahun
2013, Accessible at:
http://www.depkes.go.id/resources/download/general/
Hasil%20Riskesdas%202013.pdf [Accessed 20 May
2018]
Ruß, M, Werdan, K, Cremer, J, Krian, A, Meinertz, T, &
Zerkowski, H-R, 2009, Different Treatment Options in
Chronic Coronary Artery Disease: When Is It the
Time for Medical Treatment, Percutaneous Coronary
Intervention or Aortocoronary Bypass Surgery?
Deutsches Ärzteblatt International, 106(15), pp. 253–
261, Available at:
http://doi,org/10,3238/arztebl,2009,0253
Ruggiero, C, Cherubini, A, Ble, A, Bos, AJG, Maggio, M,
Dixit, VD, & Ferrucci, L, 2006, Uric Acid and
Inflammatory Markers, European Heart Journal,
27(10), pp. 1174–1181, Available at:
http://doi,org/10,1093/eurheartj/ehi879
Sakamoto, T, Nakao, K, Ogawa, H, Hokimoto, S, Tsujita,
K, Koide, S, Yamamoto, N, Shimomura, H,
Matsumura, T, Oshima, S, et al., 2016, Impact of
candesartan on cardiovascular events after drug-
eluting stent implantation in patients with coronary
artery disease: The 4C trial, Journal of Cardiology,
ISSN: 1876-4738, 67(4), pp. 371-7
Salam, T, & Watson, KE, 2013, Predictor of
cardiovascular risk in women, Womens Health, 9(5),
pp. 491-498.
Sari, EY, & Husna, C, 2016, Gaya Hidup Dengan
Kemampuan Mengontrol Kolesterol Pada Pasien
Hiperkolesterolemia di RSUD dr, Zainoel Abidin,
Bachelor Thesis, Fakultas Keperawatan, Universitas
Syiah Kuala.
Torpy, JA, Writer, MA, & Burke, AE, 2009, Coronary
Heart Disease Risk Factors, JAMA, 302(21), p. 2388.
World Health Organization (WHO), 2011, Global Atlas on
Cardiovascular Disease Prevention and Control,
Geneva: World Health Organization,
Yusuf, S, Zhao, F, Mehta, SR, Chrolavicius, S, Tognoni,
G, & Fox, KK, 2001, Effects of clopidogrel in addition
to aspirin in patients with acute coronary syndromes
without ST-segment elevation, N Engl J Med, 345, pp.
494–502.
Zamora, SG, & Parodi, R, 2010, Cough and
Angioedema in Patients Receiving Angiotensin-
Converting Enzyme Inhibitors. Are They Always
Attributable to Medication?, Revista Argentina
De Cardiología, 79(2), March-April 2011.
MICH-PhD 2018 - 1st Muhammadiyah International Conference on Health and Pharmaceutical Development
32
