
The Effectiveness of Skin Barrier on Medical Adhesive Related Skin
Injury in Neonates at Perinatology Dr. Cipto Mangunkusumo
Hospital Jakarta
Novardian
1
, Suhendar Sulaeman
2
, Nyimas Heny Purwati
2
and Widia Sari
3
1
Nurse at Neonatal Intensive Care Unit, Dr. CiptoMangunkusumo Hospital Jakarta, Indonesia
2
Lecture at Nursing Department, University of Muhammadiyah Jakarta, Indonesia
3
Lecture at Nursing Department, Esa Unggul University, Indonesia
Keywords: MARSI, Skin Barrier, Transparant Dressing, Neonates.
Abstract: Skin damage is one of the serious problems in neonates. One of causing of medical adhesive that is MARSI.
Skin damage on neonates will cause discomfort and affect the process of babies care. Based on AWHONN
recomended that skin barrier aplication to reduce MARSI The aim of this study are to identify the
effectiveness of transparant dressing with skin barrier and transparant dressing without skin barrier to
prevent MARSI in neonates attached infusion at Perinatology Dr. Cipto Mangunkusumo Hospital Jakarta.
The design of this study was pre experimental with non equivalent without control group. The sampling
methode used is total sampling. Total sample in this research are 80 neonates getting infussion (40 neonates
with gestational age ≤ 34 weeks, and 40 neonates with gestational age ≥ 34 weeks) who were divided into 4
groups. The data collected using NSCS (neonatal skin condition scale) questionaire with score 3-9. The
analysis used is Wilcoxon. The result of this research found that use of transparant dressing with skin barrier
in neonates with gestational age ≤ 34 weeks and neonates with gestational age ≥ 34 weeks is effective for
reducing MARSI incident (p< 0,05).Transparant dressing with skin barrier recomended use to prevent of
MARSI.
1 INTRODUCTION
Skin damage is one of the serious problems in
neonates. One of causing the using of medical
adhesive that is MARSI (Medical adhesive related
skin injury). MARSI has been defined as an
occurrence in which erythema and or other
manifestation of cutaneous abnormal (including but
not limited to vesicle, bulla, erosion, or tear) persists
30 minutes or more after removal of the adhesive
(McNichol, Lund, Rosen, & Gray, 2013)
In 2017, The Townsvile Hospital and health
service in the neonatal unit, found that prevalence of
skin damage in neonates was 9.25%-43%. This
result shows that prevalence of MARSI is high.
There are some factors that causing of skin
damage on neonates such as using of medical
adhesive, gestation age and birth weight. In 2013, a
study found that causing of skin damage were 22,4%
of the using of vascular catheter, 14% of non-
invasive continous positive airway pressure delivery
device, and 17,8% of oxygen saturation and
temperature. Based on the data that causing of skin
damage are using of medical devices.
Another factor causing of skin damage is
premature birth. Because of this condition will cause
distruption of the skin structure particularly stratum
corneum. Consequently, will increase
transepidermal water loss (TEWL) in neonates
which will cause termoregulation disturb,
dehydration and electrolite imbalance (Kuller et al.,
2006; Lambe, 2001; Lund, 2014; Nonato & Lund,
2001; M. O. Visscher, 2009).
The conditions require appropriately
management to prevent MARSI. One of them
management of MARSI is recomended by
Association of Women’s Health Obstetric and
Neonatal Nurses (AWHONN) and National
Association of Neonatal Nurse (NANN) is skin care
in neonates (Kuller et al., 2006).
The guideline skin care in neonates involve
assessment of newborn skin, umbilical cord care,
circumsision care, diaper rash, using medical
Novardian, ., Sulaeman, S., Purwati, N. and Sari, W.
The Effectiveness of Skin Barrier on Medical Adhesive Related Skin Injury in Neonates at Perinatology Dr. Cipto Mangunkusumo Hospital Jakarta.
DOI: 10.5220/0008222801870192
In Proceedings of the 1st International Conference of Indonesian National Nurses Association (ICINNA 2018), pages 187-192
ISBN: 978-989-758-406-0
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
187
adhesive, TEWL, skin damage, intravena
infiltration, and skin nutrition (Kenner & Lott,
2007). Skin damage on neonates will cause
discomfort and affect the process of babies care.
To increase comfort of babies is needed role of a
nurse according to theory of comfort by Kolcaba
(Alligood, 2014).
Based on Consensus AWHONN (Association of
Women Health, Obstetric and Neonatal Nurses) in
2007 recommended that medical adhesive choice
and skin barrier application are as alternative to
reduce MARSI (McNichol et al., 2013). Skin barrier
is a product to protect skin which will provide a
protective layer between epidermis and adhesive.
Skin barrier availables in liquid wipes, applicators,
or spray formulated from various substances such as
acrylic, polymer organic and anorganic, and silicon.
The aim of this study are to identify the
effectiveness of transparant dressing with skin
barrier and transparant dressing without skin barrier
to prevent MARSI in neonates attached infusion at
Perinatology Dr. Cipto Mangunkusumo Hospital
Jakarta.
2 METHODS
This study was pre experimental with non equivalent
without control group (non randomized without
control group pretest-postest). The studies using
research assistant. The result of interreliability test
was p<0,05. Participants were 80 neonates divided
into 4 groups. Group 1 were 20 neonates with
gestational age ≤34 weeks applied by transparant
dressing with skin barrier. Group 2 were 20 neonates
with gestational age ≤ 34 weeks applied by
transparant dressin without skin barrier. Group 3
were 20 neonates with gestational age ≥ 34 weeks
applied by transparant dressing with skin barrier.
Group 4 were 20 neonates with gestational age ≥ 34
weeks applied by transparant dressing without skin
barrier
Firstly, group 1 and 3 were evaluated using
NSCS (Neonatal Skin Condition Scale) observation
sheet before applied with medical adhesive, was
applied 3M Cavilon No Sting Barrier Film 3344E, 1
ml Product USA and then leave around 30 seconds.
Then, cover skin with using a transparant dressing
(3M Tegadern film 6cm x 7cm). Change of the
medical adhesive was done after 3 days or when skin
area looked dirty.
At the same time, for group 3 and 4 transparant
dressing is used. The skin was evaluated for
conditions using the NSCS observation sheet.
The data collected using Observation sheet with
NSCS (neonatal skin condition scale) with score 3-9.
The NSCS instrument is recommendation from
AWHONN. The data was analyzed using SPSS 2.0.
Since the data not normally distributed, Wilcoxon
was used for statistical analysis.
Ethical clearance for this study was granted from
ethics committe Cipto Mangunkusumo Hospital.
3 RESULTS
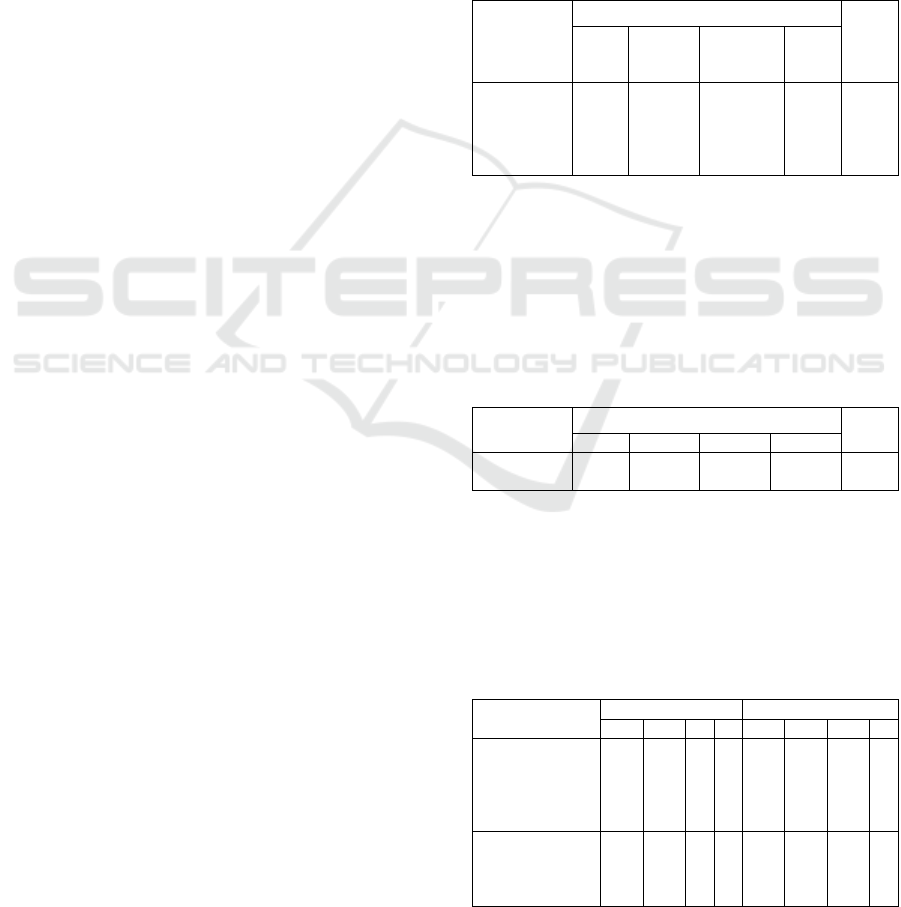
Table 1: Characteristics of Respondents in each group
based on gender (n=80).
Characteristics
Group
p value
I (n=20)
f (%)
II (n=20)
f (%)
III (n=20)
f (%)
IV
(n=20)
f (%)
1.Male
2.Female
3.Ambiguos
9 (45)
11
(55)
0 (0)
11 (55)
9 (45)
0 (0)
8 (40)
11 (55.5)
1 (5)
11 (55)
8 (40)
1 (5)
0.701
Table 1 show that the majority of respondent
were female in group 1 and 3 (55% and 55.5%,
respectively) and male in group 2 and 4 (55% in
both group). The test of homogenity result shows
value of 0.701 which means that the characteristics
of respondent homogeneus.
Table 2: Characteristics of Respondents in each group
based on NSCS before intervention (n=80).
Characteristics
Group
p value
I (n=20) II (n=20) III (n=20) IV (n=20)
NSCS score
3.70
(0.73)
3.70
(0.57)
3.75
(0.85)
3.85
(0.75)
0.441
Table 2 shows that the test of homogenity NSCS
score from each group with p value =0.441. This
shows characteristics of respondent in each group
based on NSCS score before intervention is
homogeneus.
Table 3: MARSI score in neonates with gestational age ≤
34 weeks (n=80).
f (Score) Percentage(Score)
3 4 5 6 3 4 5 6
1.Transparant
dressing + skin
barrier
a. Before
b
. Afte
r
9
12
8
7
3
1
0
0
45
60
40
35
15
5
0
0
2.Without skin
barrier
a. Before
b
. Afte
r
7
4
12
9
1
7
0
0
35
20
60
45
5
35
0
0
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
188
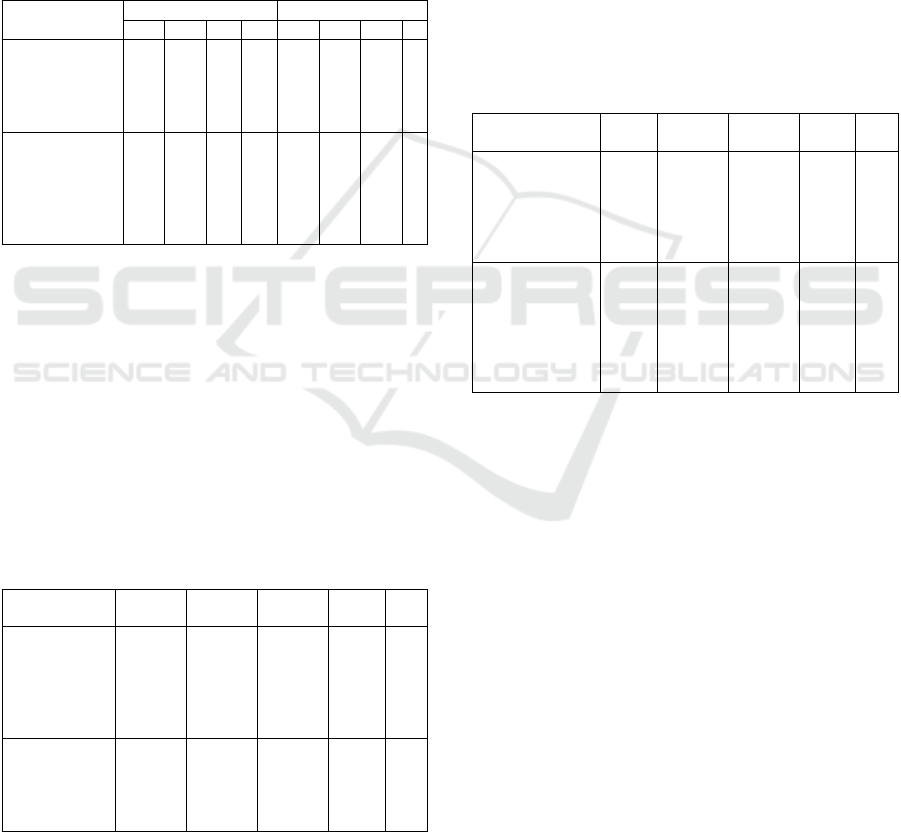
Table 3 show that MARSI score before and after
intervention transparant dressing with skin barrier no
increase MARSI incident. The majority of MARSI
score was 3 (45%) before intervention and after
intervention was 3 (60%).
The data show that there was a change in
MARSI score before and after intervention
transparant dressing without skin barrier. Before
intervention, MARSI score 5 only 1 respondent
(5.0%), but after intervention transparant dressing
MARSI score 5 becomes 7 neonates (35.0%).
Table 4: MARSI score in neonates with gestational age ≥
34 weeks.
Frequen
t
(Score) % (Score)
3 4 5 6 3 4 5 6
1.Transparant
dressing with
skin barrier
a. Before
b
. Afte
r
9
11
8
8
2
0
1
1
45
55
40
40
10
0
5
5
2.Transparant
dressing
without skin
barrier
a. Before
b
. Afte
r
6
4
12
9
1
6
1
1
30
20
60
45
5
30
5
5
Table 4 show that MARSI score before and after
given intervention transparant dressing with skin
barrier not increase MARSI incident. The majority
MARSI score is 3 (45%) before intervention and
after intervention is 3 (55%).
The data also shows that MARSI score before
and after intervetion transparant dressing there is a
change. Before intervention MARSI score 5 only 1
respondent (5%), but after intervention MARSI
score 5 to be 6 respondent (30%).
Table 5: Difference in average of MARSI score before and
after intervention in neonates with gestational age ≤ 34
weeks.
Mean SD
Mean
ran
k
Pv n
1.Transparant
dressing with
skin barrier
a. Before
b. After
c. (∆)
3.7
3.45
-0,25
0.733
0.605
3.00
0.02
5
20
2. Without
skin barrier
a. Before
b. After
c. (∆)
3.7
4.15
0.45
0.571
0.745
0.00
4.00
0.01
4
20
Table 5 shows that in the intervention group
given transparant dressing with skin barrier there
was no increase in the MARSI score with the
difference before and after the intervention was -
0.25. The statistical test results obtained p = 0.025
with 95% CI. It can be concluded that there is a
difference between the MARSI score before and
after skin barrier intervention.
The table also shows that in the group with
transparent dressing without skin barrier intervention
there was also an increase in the MARSI score. The
difference between before and after the intervention
is 0.45. This is shows that after transparent dressing
there is an increase in skin irritation in infants. The
statistical test results obtained a value of p = 0.014
so it can be concluded that there is a difference
between the MARSI score before and after given
transparantdressing.
Table 6: Difference in average of MARSI score before and
after intervention in neonates with gestational age ≥ 34
weeks.
Mea
n
SD
Mean
ran
k
Pv n
1.Transparant
dressing with
skin barrier
a. Before
b. After
c. (∆)
3.75
3.55
-0.2
0.851
0.759
2.50
0.04
6
20
2.Transparant
dressing
without skin
barrier
a. Before
b. After
c. (∆)
3.85
4.20
0.35
0.745
0.835
4.00
4.57
0.03
5
20
Based on table 6, shows that in group III given
transparent dressing intervention with skin barrier
there was no increase in MARSI score. The
difference between before and after the intervention
is -0.2. The results of the statistical test obtained p =
0.046, it can be concluded that there is a difference
between the MARSI score before and after the
transparant dressing intervention with the skin
barrier.
The table above also explains that in group IV
given transparent dressing dressing without skin
barrier there was an increase in MARSI scores. The
difference between before and after the intervention
is 0.35. This shows that after the transparent
installation of the dressing without the skin barrier
there is a deterioration of the skin condition in the
baby. The statistical test results obtained p = 0.035,
so it can be concluded that there is a significant
difference between the MARSI score before and
after being given a transparant dressing intervention
without the skin barrier.
The Effectiveness of Skin Barrier on Medical Adhesive Related Skin Injury in Neonates at Perinatology Dr. Cipto Mangunkusumo Hospital
Jakarta
189

4 DISCUSSION
1. Gender
The majority gender of neonates in each group is
male. In theory, it was not found that gender affected
damage to skin integrity. The research conducted by
Alfiyanti (2012) stated that there was no significant
relationship between gender with the incidence of
compressive wounds in children treated in PICU.
The study showed that gender factors did not affect
the occurrence of damage to skin integrity
(Alfiyanti, Nurhaeni, & Eryando, 2012).
2. Gestational Age
In this research, each respondent was divided into
groups based on gestational age ≤ 34 weeks and ≥ 34
weeks. In premature babies, skin barriers have not
developed properly so that babies has damageskin
integrity (M. Visscher & Narendran, 2014). The
structure of skin integrity, especially the stratum
corneum, is associated with gestational age because
skin barriers develop 24 to 34 weeks after birth, so
that premature infants have a thin epidermal layer
and less stratum corneum (M. O. Visscher, 2009).
3. The effectiveness of transparant dressing with
skin barrier and transparant dressing without skin
barrier in neonates given infussion on MARSI
a. Transparant dressing with skin barrier
application
The average MARSI score before and after given
skin barrier decreases. So it can be concluded that
the use of an effective skin barrier to prevent skin
damage due to the use of medical adhesive or other
adhesive devices. The use of a skin barrier
application will provide a protective layer between
the epidermis and medical adhesive. This study the
barrier skin used was in the form of Cavillon no
sting barrier 3M product film. After the application,
the barrier liquid will evaporate and leave a
protective layer that is transparant and breathable for
up to 72 hours.
In the gestational age of ≥ 34 weeks, the use of
skin barriers also causes a decrease in the incidence
of MARSI with a difference in value (∆) The
statistical test results obtained p = 0.046 so that it
can be concluded that there are differences in the
average use of skin barriers before and after
intervention in infusion infants with a gestational
age of ≥ 34 weeks. In groups with a gestational age
of ≥ 34 weeks there was a greater difference in value
than gestational age ≤ 34 weeks. This is due to
gestational age of ≥ 34 weeks so that anatomically
the epidermis and stratum corneum have begun to
function so that the skin will be bluish pink and
smooth or white (Kenner & Lott, 2007).
The use of skin barriers has been recommended
to skin care for neonates who are treated (Telofski,
Morello, Mack Correa, & Stamatas, 2012). That was
because the structure of the baby's skin is different
from that of an adult. Research conducted by Kuller
et al., (2006) states that the use of medical adhesive
in infants is a major factor cause of skin damage in
infants treated at the NICU. Invasive procedure also
causes the baby to have iatrogenic injury. These
injuries can cause damage to the integrity of the skin
including burns and lesions due to the use of
disinfectants, erythema and hollows on the skin due
to the use of monitoring probe devices (Kenner &
Lott, 2007).
The difference value before and after being given
a skin barrier application thus indicating that the
skin barrier is more effective in preventing MARSI
incident or other skin damage. The use of skin
barriers in this study does not cause improvement in
the baby's skin, but prevents further damage to the
baby's skin due to medical adhesive.In addition to
the use of adhesives, skin damage in premature
babies is also caused by many things, one of which
is gestational age of ≤ 34 weeks. The gestational
age is associated with not yet developing the skin
layer perfectly, especially the stratum corneum is
still small.
This research is in line with research conducted
by Brondon et al., (2010) which states that the use of
skin protection such as the no sting barrier film will
reduce TEWL and maintain skin integrity in infants.
This study was conducted in 69 infants with a
gestational age ≤ 33 weeks for 18 months. Every
baby gets treatment for 2 weeks (Brandon, Coe,
Hudson-Barr, Oliver, & Landerman, 2010).
b. Transparant dressing without skin barrier
application
The average MARSI score before and after the
intervention was given using transparant dressing,
there was an increase in the MARSI score. The
statistical test results so that it can be concluded that
there are differences in the average before and after
the intervention using transparent dressings without
skin barriers to the incidence of MARSI in infants
with gestational age of ≤ 34 weeks given infusion.
The high difference value indicates that the skin
changes towards negative, where there is an increase
in skin irritation in the baby after being given
transparant dressing without the skin barrier. It can
be seen in Table 2 that after the use of transparent
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
190

dressing, the score of MARSI 5 becomes 7
respondents, where before the intervention the
MARSI 5 score is only 1 respondent.
One of the recommended use of transparant
dressings is 3M Tegaderm. This Tegaderm film
consists of elastic film with adhesive that is free of
latex and hypoallergenic and is breathable which
allows the exchange of oxygen and water vapor well
so that the skin will remain moist. In addition to this,
conditions are transparant, making it easier to
observe skin conditions due to invasive actions that
occur.
The use of transparant dressings is often used
both in adults and children. Research conducted by
Inoue & Matsuda (2015) in 25 patients showed that
the use of transparant film dressings in press wounds
was more cost effective compared to hydrocoloid
dressings (Inoue & Matsuda, 2016). In premature
babies, recommends using transparant dressings to
maintain skin integrity in infants (Lund, 2014). This
is different from this study, where the use of
transparant dressing increases the incidence of
MARSI in premature infants. The increase is due to
the structure of the baby's skin that is still not fully
developed, so the use of transparant dressing will lift
the epidermis layer of the baby's skin and TEWL
increases so that the baby's skin will be more
damaged. Another possibility is that the increase in
MARSI scores on the use of transparant dressing
applications without skin barriers can also be caused
due to the wrong technique of releasing transparent
dressings, it is not using stretch methods so that the
risk increases MARSI.
In the infants with gestational age of ≥ 34 weeks
there was also an increase in the MARSI score
before and after the use of transparant dressing
without skin barrier with a difference. But the
difference in value is smaller when compared to the
infant with gestational age of ≤ 34 weeks. This is
due to the development of the skin structure in the
baby. The statistical test results so it can be
concluded that there was a significant difference in
the use of transparent dressings without skin barriers
before and after intervention in infants with
gestational age of ≥ 34 weeks given infussion. The
difference that occurs in neonatal skin is an increase
in the MARSI score, so the use of transparant
dressing without a skin barrier will worsen the
condition of the baby's skin.
The limitations of this study are the removal of
the medical adhesive in each babies is not the same
because several conditions, like dirty, contains blood
and babies move the room.
5 CONCLUSIONS
In this study, it was shown that the use of transparant
dressings with skin barriers was effective in prevent
of MARSI.
It is recommended that the use of transparant
dressings with skin barrier to prevent of MARSI as a
guidelines in infant skin care, especially in infants
with gestational age of ≤ 34 weeks.
The limitations of this study are the removal of
the medical adhesive in each babies is not the same
because of several conditions, like dirty, contains
blood and babies move the room.
ACKNOWLEDGEMENTS
The preparation of this paper was supported by
Magister of Nursing University of Muhammadiyah
Jakarta, Neonatology intensive care unit at Dr. Cipto
Mangunkusomo Hospital Jakarta and 3M Company.
REFERENCE
Alfiyanti, D., Nurhaeni, N., & Eryando, T. (2012).
Pengaruh Perawatan Kulit Berdasarkan Skor Skala
Braden Q Terhadap Kejadian Luka Tekan Anak Di
Pediatric Intensive Care Unit (Picu) Rs. Tugurejo Dan
Rs. Roemani Semarang. Prosiding Seminar Nasional,
1(1).
Alligood, M. R. (2014). Nursing Theorists and Their
Work. Nursing Theorists and Their Work (8th edn).
https://doi.org/10.5172/conu.2007.24.1.106a
Brandon, D. H., Coe, K., Hudson-Barr, D., Oliver, T., &
Landerman, L. R. (2010). Effectiveness of No-Sting
skin protectant and Aquaphor on water loss and skin
integrity in premature infants. Journal of
Perinatology, 30(6), 414–419. https://doi.org/10.1038/
jp.2009.174
Inoue, K. C., & Matsuda, L. M. (2016). Cost of dressings
for prevention of sacral pressure ulcers. Revista
Brasileira de Enfermagem, 69(4), 641–645.
https://doi.org/10.1590/0034-7167.2016690404i
Kenner C, Lott J. (2007). Comprehensive Neonatal Care:
An Interdisciplinary Approach. 4thed. New York:
Elsevier Inc.
Kuller, J., Lott, J. W., Raines, D. A., Osborne, J. W.,
Lund, C. H., & Lane, A. T. (2006). Neonatal Skin
Care: Clinical Outcomes of the AWHONN/NANN
Evidence-Based Clinical Practice Guideline. Journal
of Obstetric, Gynecologic & Neonatal Nursing, 30(1),
41–51. https://doi.org/10.1111/j.1552-6909.2001.tb01
520.x
Lambe, M. B. (2001). Topical agents in infants. Newborn
and Infant Nursing Reviews, 1(1), 25–34.
The Effectiveness of Skin Barrier on Medical Adhesive Related Skin Injury in Neonates at Perinatology Dr. Cipto Mangunkusumo Hospital
Jakarta
191

https://doi.org/10.1053/nbin.2001.21835
Lund, C. (2014). Medical Adhesives in the NICU.
Newborn and Infant Nursing Reviews, 14(4), 160–165.
https://doi.org/10.1053/j.nainr.2014.10.001
McNichol, L., Lund, C., Rosen, T., & Gray, M. (2013).
Medical adhesives and patient safety: State of the
science: Consensus statements for the assessment,
prevention, and treatment of adhesive-related skin
injuries. Journal of the Dermatology Nurses’
Association. https://doi.org/10.1097/JDN.
0000000000000009
Nonato, L. B., & Lund, C. H. (2001). Transepidermal
water loss in the intensive care nursery: Measuring
techniques and research recommendations. Newborn
and Infant Nursing Reviews, 1(1), 11–20.
https://doi.org/10.1053/nbin.2001.22121.
Telofski, L. S., Morello, A. P., Mack Correa, M. C., &
Stamatas, G. N. (2012). The Infant Skin Barrier: Can
We Preserve, Protect, and Enhance the Barrier?
Dermatology Research and Practice, 2012, 1–18.
https://doi.org/10.1155/2012/198789.
Visscher, M., & Narendran, V. (2014). Neonatal Infant
Skin: Development, Structure and Function. Newborn
and Infant Nursing Reviews, 14(4), 135–141.
https://doi.org/10.1053/j.nainr.2014.10.004.
Visscher, M. O. (2009). Update on the Use of Topical
Agents in Neonates. Newborn and Infant Nursing
Reviews. https://doi.org/10.1053/j.nainr.2008.12.010.
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
192
