
The Experiences of HIV Status Disclosure among Pregnant and
Postpartum Women: A Systematic Review of Qualitative Evidence
Ira Rahmawati
1
and Ratna Dewi
2
1
Poltekkes Kemenkes Malang. Kota Malang, Jawa Timur 65119, Indonesia
2
Department of Nursing, Esa Unggul University, Arjuna Utara no. 9, West Jakarta, Indonesia
Keywords: HIV/AIDS, Disclosure, Experience, Pregnant Women, Postpartum Women, PMTCT, Systematic Review.
Abstract: Disclosure of HIV status among HIV-positive pregnant and postpartum women may significantly improve
their uptake and adherence in the prevention of mother-to-child transmission of HIV programs. However,
many women choose not to disclose their status because of several factors. This review aimed to understand
the experiences of HIV-positive women on HIV-status disclosure during pregnancy and postpartum period.
Five databases were searched to identify relevant qualitative studies published in English language from 2000
to 2017. A three-step search strategy was utilized in this review. An initial limited search of CINAHL and
PubMed was undertaken followed by analysis of the text words contained in the title and abstract, and the
index terms used to describe article. A second search using all identified keywords and index terms was
conducted across all included databases. Thirdly, the reference list of all identified articles was searched for
additional studies. Studies that met inclusion criteria were considered, which include qualitative studies,
participants of the study were HIV positive pregnant or postpartum women and studies that aimed to
understand the experiences of HIV-positive women on HIV-status disclosure in the context of pregnancy and
post-partum period. Qualitative papers selected for retrieval were assessed by two independent reviewers for
methodological validity prior to inclusion in this review using the standardized critical appraisal instruments
from the Joanna Briggs Institute Qualitative Assessment and Review Instrument (JBI-QARI). Data extraction
was also conducted using the JBI-QARI. Three qualitative studies were included in this review. Twenty
themes were extracted, which were then aggregated into six categories and three synthesized findings. The
six categories namely reasons for disclosure and non-disclosure HIV-positive status to the partner, family,
and friends, positive and negative experiences of disclosure and pattern of disclosure. The reasons for
disclosure and non-disclosure of HIV-positive status among women during pregnancy and the postpartum
period are different depending on to whom they disclose. Some of the women experienced negative outcomes
of disclosure such as violence, which may negatively influence their decision to disclose in the future. Lastly,
HIV-positive women need continuing support and counselling to cope with the outcomes of disclosure
practice.
1 INTRODUCTION
About 2. 6 million children under the age of 15 were
living with HIV globally in 2015, with 150. 000
children were newly infected in 2015 (The Joint
United Nations Program on HIV/AIDS [UNAIDS],
2015). Mother-to-child transmission of HIV is
correlated with 90% of HIV infection in children at
the age of 0-6 years old (Sendo, Cherie, & Erku
2013). The transmission of HIV from an HIV-
positive mother to her child can occur during
pregnancy, delivery and breastfeeding. Prevention of
mother-to-child transmission (PMTCT) of HIV
programmes which involve the use of antiretroviral
drugs for the HIV-positive pregnant and breast-
feeding women and a short course of antiretroviral
drugs for the infant have been reported to reduce the
rate of HIV transmission among children to nearly
zero (World Health Organization [WHO], 2013;
Sendo, Cherie, & Erku, 2013). However, the success
of the PMTCT program is dependent upon disclosure
of HIV-seropositive to partners, families and others
in the community (Tam, Amzel, & Phelps, 2015).
Disclosure of HIV status is essential for
preventing HIV transmission and early intervention.
In the context of pregnancy and perinatal particularly,
Rahmawati, I. and Dewi, R.
The Experiences of HIV Status Disclosure among Pregnant and Postpartum Women: A Systematic Review of Qualitative Evidence.
DOI: 10.5220/0008199900310041
In Proceedings of the 1st International Conference of Indonesian National Nurses Association (ICINNA 2018), pages 31-41
ISBN: 978-989-758-406-0
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
31

disclosure of HIV status by women to their sexual
partners is crucial for the prevention of HIV from
mother to child during pregnancy, birth and through
breast-feeding (Rujumba et al., 2012; Visser,
Neufeld, de Villiers, Makin, & Forsyth, 2008).
Indeed, several studies revealed that women who had
disclosed to their partners were found to be more
likely to bottle-feed their infants and more likely to
participate in PMTCT programmes than women who
had not disclosed (Farquhar et al., 2001; Rujumba et
al., 2012). However, disclosure of HIV status remains
a challenge for pregnant and postpartum women
(Tam, Amzel, & Phelps, 2015). Studies have
documented that the rate of HIV-status disclosure is
low, especially among women in developing
countries, which ranged from 16. 7% to 86%, with the
lowest rate of HIV serostatus disclosure occurred
among women in antenatal care
(Medley, Garcia-
Moreno, McGill, & Maman, 2004).
HIV-related stigma, fear of partner violence, loss
of financial support and blame for bringing the HIV
infection into family prevent many women from
disclosing their HIV-status (Bwirire et al., 2008;
Rujumba et al., 2012). Studies have revealed that non-
disclosure of the HIV status may contribute to non-
adherence to ART, as women do not want to be seen
taking the ART drugs (Madiba & Letsoalo, 2013).
Another study reported that pregnant women choose
to deliver at home to prevent stigma that may arise
following disclosure to the health care providers
(Ujiji et al., 2011). Lastly, feeding counselling and
post-delivery infant prophylaxis may be less likely to
occur in the context of non-disclosure (Kasenga,
Hurtig, & Emmelin, 2010).
Disclosure is defined as the willingness of an
HIV-infected person to reveal their status to another
person, which can be their spouse, family, health
providers or friends (Adeoye-Agboola et al. 2016). It
involves a process of decision-making, which is
influenced by numerous factors including motivation,
communication skills, psychological state and
anticipated reactions (Visser et al., 2008). Disclosure
of HIV status is a complex process involving multiple
and continuing decisions about who to tell, how to tell
and how much to tell (Makin et al., 2008; Moses &
Tomlinson, 2013).
A systematic review on HIV-status disclosure
among pregnant and postpartum women in sub-
Saharan Africa found that individual characteristics
associated with greater chances of disclosure include
first pregnancy, lower level of internalized stigma,
younger age and knowing someone with HIV. Other
factors that positively correlated with disclosure of
HIV status include characteristics of the household
such as living without extended family or co-spouses.
Lastly, characteristics of the partner associated with
higher disclosure rate include higher level of
educations, no history of domestic violence and
financial independence (Tam, Amzel, & Phelps,
2015).
Understanding women’s experiences on
disclosure of HIV status during pregnancy and
postpartum period could provide inputs on how to
improve the uptake and adherence of PMTCT
programs.
To our knowledge, no systematic reviews have
synthesized the experiences of HIV disclosure among
HIV-positive pregnant and postpartum women. A
preliminary search for systematic reviews on this
topic was carried out in Cochrane Library, Joanna
Briggs Institute Database of Systematic reviews &
Implementation Reports, PubMed, CINAHL and
PROSPERO. No existing systematic reviews were
found in these databases that synthesize the
experiences of HIV-positive women on HIV-status
disclosure in the context of pregnancy and postpartum
period. Aware of this fact, this review aims to
synthesize the findings from studies that explore the
experiences of HIV-positive pregnant and postpartum
women on HIV-status disclosure.
2 METHODS
2.1 Inclusion Criteria
2.1.1 Type of Participants
This review included studies that involve HIV-
infected women who are pregnant or in the post-
partum period and 18 years old and above.
2.1.2 Phenomena of Interest
This review sought to understand the views and
experiences of HIV-positive women on HIV-status
disclosure in the context of pregnancy and post-
partum period.
2.1.3 Context
This review included studies that explore the HIV-
positive women’s experiences on HIV-status
disclosure during pregnancy and in the context of
vertical transmission. This review included studies
that conducted in all health care settings (HIV/AIDS
clinics, in-patients, out-patients, rural and urban
community) and all countries. This review considered
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
32

all studies that investigate the views and experiences
of HIV-positive pregnant women on HIV disclosure
to the partner, family members, and friends.
2.1.4 Types of Studies
This review considered all forms of qualitative study
designs such as grounded theory, phenomenology,
ethnography, action research and other descriptive
qualitative study published in English language.
2.2 Search Strategy
The search strategy aimed to find both published and
unpublished studies. A three-step search strategy
following the Joanna Briggs Institute (JBI) guidelines
was utilized in this review. An initial limited search
of CINAHL and PubMed was undertaken followed
by analysis of the text words contained in the title and
abstract, and of the index terms used to describe
article. A second search using all identified keywords
and index terms was conducted across all included
databases. Thirdly, the reference list of all identified
reports and articles was searched for additional
studies. Studies published in the English language
were considered in this review.
The databases searched included CINAHL,
PubMed, EMBASE, PsycINFO and Scopus. The
search for unpublished studies included reports and
guidelines from professional organizations
(UNAIDS, WHO) and ProQuest.
Initial keywords used were: experiences, views,
perception, HIV, AIDS, disclosure, HIV disclosure,
HIV-positive women, HIV-positive pregnant women,
pregnancy and PMTCT (prevention of mother-to-
child transmission of HIV).
2.3 Method of Review
Qualitative papers selected for retrieval were assessed
by two independent reviewers for methodological
validity prior to inclusion in this review, using the
standardized critical appraisal instruments from the
Joanna Briggs Institute Qualitative Assessment and
Review Instrument (JBI-QARI). Any disagreement
that arose between the two reviewers were resolved
through discussion, or with a third reviewer.
2.4 Data Collection
Qualitative data were extracted from studies included
in this review using the standardized data extraction
tool from JBI-QARI. The extracted data which
include specific details about participants,
phenomenon of interest, study methods, and
outcomes of significance to the review question and
specific objectives. Information regarding the cultural
and geographical settings, method of data analysis
used in the primary studies and the author’s
conclusions were also extracted. Findings were
extracted from the papers by two reviewers working
independently. The two reviewers then discussed and
reached consensus on the levels of credibility of the
findings and the final construction of the findings
were aggregated.
2.5 Data Synthesis
Qualitative research findings were, where possible
pooled using JBI-QARI. This involved the
aggregation or synthesis of the findings to generate a
set of statements that represent that aggregation,
through assembling the findings rated according to
their quality, and categorizing these findings on the
basis of similarity in meaning. These categories were
then subjected to a meta-synthesis in order to generate
a single
comprehensive set of synthesized findings
that could be used as a basis for evidence-based
practice. Where textual pooling was not possible, the
findings were presented in narrative form.
3 RESULTS
3.1 Description of Studies
Following a comprehensive search, 316 articles were
identified (Figure 1). A total of 119 duplicates were
removed leaving 197 articles to be assessed. A total
of 182 article were excluded on reviewing the titles
and abstracts, leaving 15 articles for full text review.
Of these, 12 papers were excluded for not meeting the
inclusion criteria such as included multiple
participants (participants were both HIV-positive and
HIV-negative pregnant women or participants were
HIV-positive pregnant women and their partners) and
the results were not presented as qualitative findings.
This left three studies eligible for critical appraisal.
After assessing the quality of these papers the three
papers were included in this review.
The Experiences of HIV Status Disclosure among Pregnant and Postpartum Women: A Systematic Review of Qualitative Evidence
33
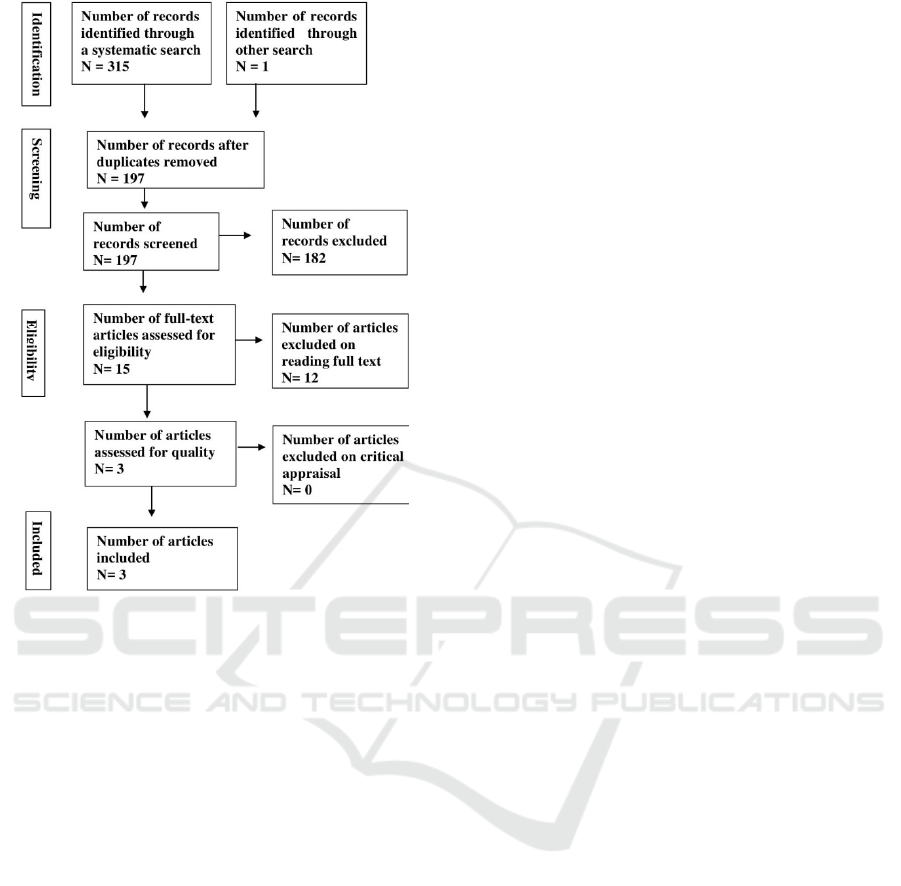
Figure 1: Flow chart of the search and study selection
process.
This review included three qualitative studies
conducted mainly in a South African setting. All the
studies were published within the past 11 years, i.e.
from 2005 to 2013. The three included studies are
described below.
The study by Visser et al.
was conducted in four
antenatal clinics that provide health services to an
urban population in Tshwane, South Africa. 293 HIV-
positive pregnant women were interviewed during
pregnancy (mean gestational age of 28 weeks) with
open-ended questions. These women were referred by
HIV counsellors from the antenatal clinics. The
Interviews were conducted by trained research
assistants in the participants’ language: IsiZulu,
Tswana or Sepedi. Content analysis from Stemler
2002, were performed and two researchers interpreted
the data independently. The reasons for HIV-
disclosure and non-disclosure and also the reactions
after disclosure experienced by the participants are
identified.
Varga, Sherman & Jones’s
study was conducted
in the antenatal clinic of Coronation Women and
Children’s Hospital (CWCH) in Johannesburg, South
Africa. The study carried out using a grounded theory
approach, thus the data collection used a series in-
depth interview and fieldwork. A total of 31 positive
mothers who have been tested for HIV for the first
time during their pregnancy were interviewed at the
clinic by a female interviewer in the participants’
language of choice. Each participant was interviewed
at least twice. The fieldwork was conducted between
December 2003 and August 2003. Qualitative data
from the interviews and observations were
transcribed and translated. Thematic analysis was
performed using QSR NUD*IST (1997) qualitative
data analysis package, and a regular meeting between
the researchers was scheduled to discuss experiences
and observations during data collection.
Moses & Tomlinson’s study
was conducted in an
urban community about 20 kilometers outside Cape
Town in the Western Cape province of South Africa.
The study used a longitudinal ethnographic approach
to trace women’s experiences from late pregnancy
until the end of the first year of motherhood. Hence,
the fieldwork was conducted for 24 months, started in
November 2008. Ten HIV-positive women were
recruited via HIV counsellors during their antenatal
clinic visits. Data collections used in the study are in-
depth interviews with the participants, informal visits
to participants’ homes, infant observations and clinic-
visit observations. The research team includes two
researchers who conducted all the interviews and two
fieldworkers who conducted the observations
together with the two researchers. The interview
topics evolved on the individual basis over the course
of the fieldwork and thus, not all women were asked
all questions. Data which include detailed field notes
and interview transcriptions was analyzed using a
critical interpretative phenomenological approach
(IPA) with ideographic perspectives. Thus, two of the
women’s experiences are then chosen to be explored
in more details as they highlight the range of
complexity and fluidity of disclosure experiences
across the group.
3.2 Methodological Quality
All papers assessed for quality were included in the
review (Table 1). Two papers indicated the
methodological approaches used which include a
grounded theory and ethnographic approach.
Meanwhile, the last study did not clearly indicate the
methodological approach used in the study. In
qualitative studies, the researchers face ethical
challenges in all phases of the research, from
designing to reporting. One of the ethical challenges
that should be acknowledged and addressed is the
researchers’ potential impact on the participants and
vice versa. However, all included studies did not
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
34
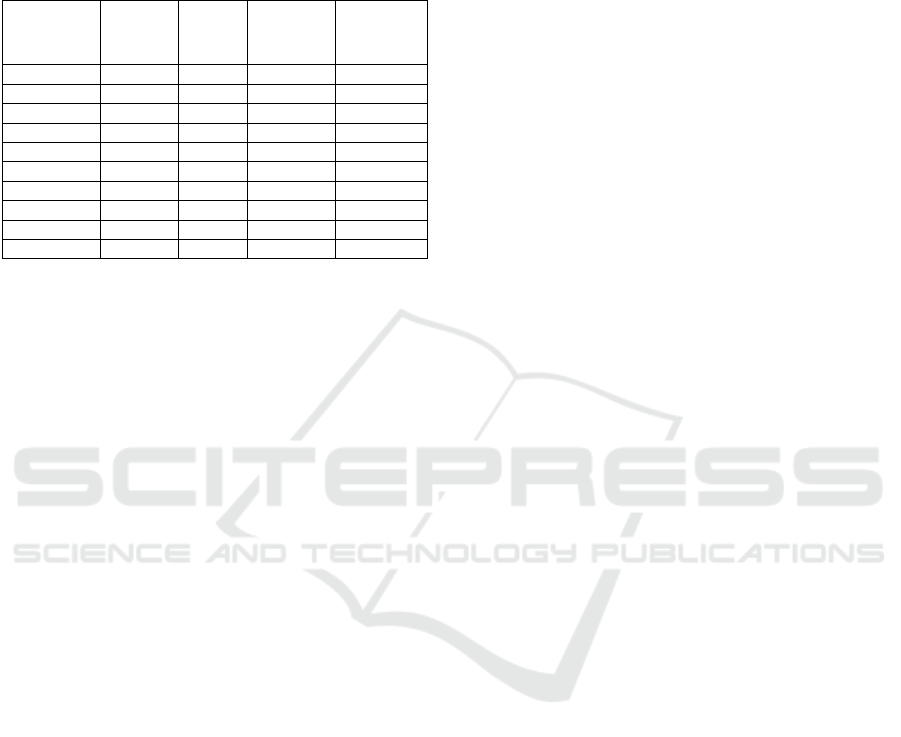
clearly indicate the influence of the researcher on the
research and participants. Therefore, the extent to
which the findings may have been influenced by the
researcher is unclear.
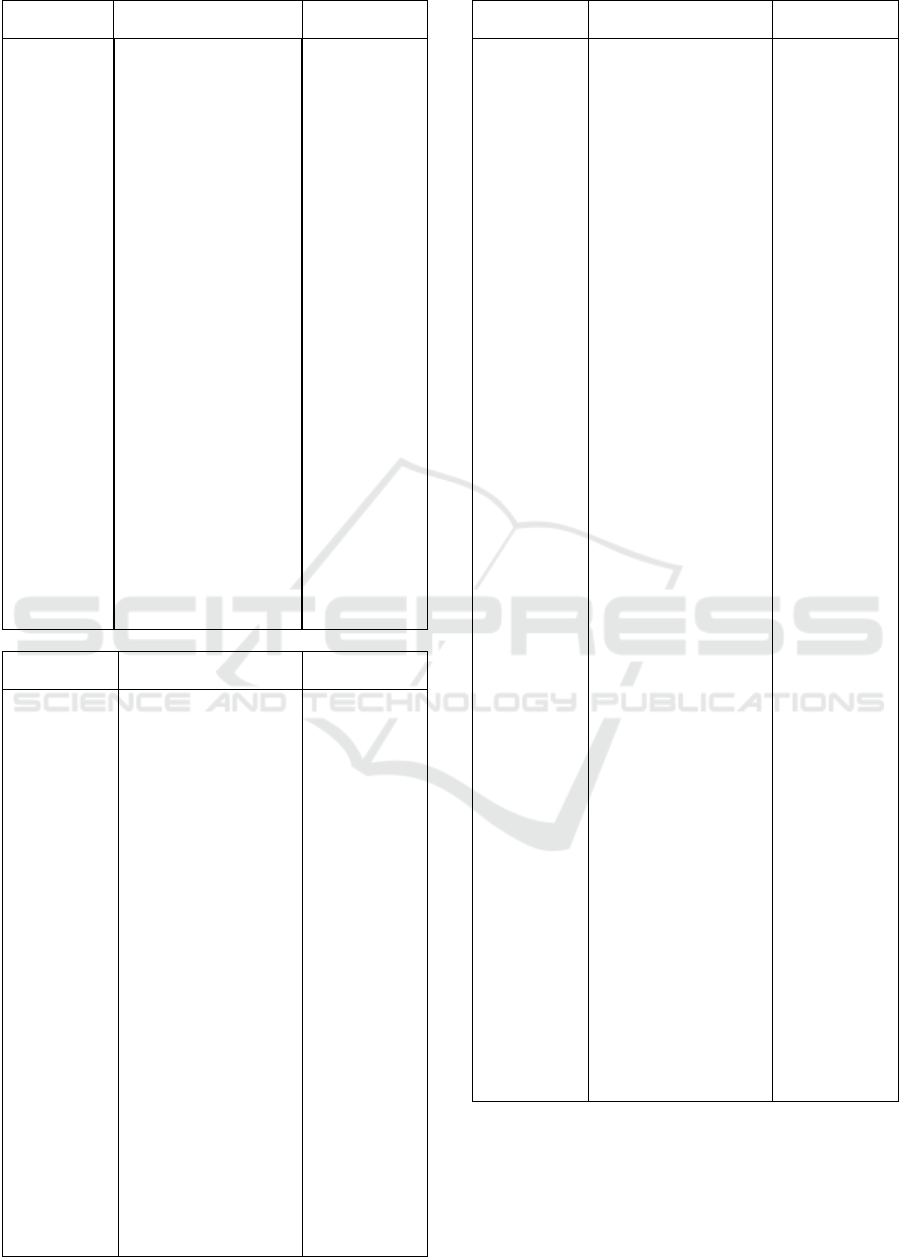
Table 1: Assessment of methodological quality.
Citation 1 2 3 %
Q1 U Y U 33,3
Q2 Y Y Y 100
Q3 Y Y Y 100
Q4 Y U U 33,3
Q5 U Y Y 66,6
Q6 Y Y Y 100
Q7 N N N 0
Q8 N Y N 33,3
Q9 Y Y Y 100
Q10 Y U Y 66,6
*1: Visser MJ, Neufeld S, de Villiers A, Makin JD & Forsyth
BWC (2008), 2: Varga CA, Sherman GG & Jones SA (2005), 3:
Moses S & Tomlinson M (2013);
*Q1-Q10 arethe Joanna Briggs Institute(JBI) Critical Appraisal
Checklist for Qualitative Research; Y:yes, U:unclear, N:no.
3.3 Findings of the Review
A meta-synthesis was carried out according to the
framework provided by JBI. There were 20 findings,
which were rated as unequivocal (U: 11) and credible
(C: 9) (Appendix V). The findings were aggregated
into six categories based on the similarity in meaning.
The six categories were then meta-aggregated into
three synthesized findings are illustrated in more
detail in Appendix (VI).
Synthesized finding one:
The reasons for disclosure and non-disclosure of
HIV-positive status among women during pregnancy
and the postpartum period are different depending on
to whom they disclose. Appropriate support
mechanisms should be offered to help these women
to deal with the outcomes of disclosure their fear and
violence when it really occurs. Health worker
mediated disclosure, couple counselling or
collaboration with support groups for women living
with HIV may be utilized to support these women.
This synthesized finding consists of three categories:
1. Reasons for disclosure and non-disclosure to the
partner
The most common reason given by the HIV-
positive women for disclosing to their partners
was to inform them of the risk of HIV
transmission. Another significant reason included
a sense of responsibility given the relationship.
The example of women’s expression:
“He has the right to know as the father of the
expected child. I had the responsibility to
disclose” (U) (Visser et al. P.1140).
Some women chose to not disclose the HIV status to
their partners because they fear of being abandoned
and blamed, and afraid that their partners will become
violent towards them.
“I do not know how to tell him. He often says he
would kill me if I told him that I’m infected
because he does not have HIV” (C)
(Visser et al.
P. 1141).
2. Reasons for disclosure and non-disclosure to the
family
HIV-positive women disclosed to the family
because they need support from people they trust.
These women have also disclosed their status to
solicit care for their baby and to ensure breast-
feeding avoidance. The following statements
were example of the women’s expressions:
“I told them [family members] exactly why [the
baby] is using a bottle. As soon as I found out
about my result I told them I have been tested and
that I am HIV-positive so I will have to give the
bottle and I am not supposed to breast-feed. After
that, they stopped pressuring me. My mother [is
now] supportive and helps me to make bottles and
feed [the baby] properly” (C) (Varga, Sherman &
Jones. 2006. P. 957).
In contrast to the reasons for non-disclosure to the
partner, a common reason
for non-disclosure to the
family is to protect them from the stigma:
“My mother is sick. She had a stroke. I can’t tell
her because it will affect her health” (U) (Visser
et al. 2008., P. 1141).
3. Reasons for disclosure and non-disclosure to
friends
Some of these women chose to disclose to their
friends, especially the close one to garner
emotional support as they experienced the
relationship as supportive and trusting. The
following statement was expressed by one of the
participants:
“I told… when I came back from the clinic
because I was so hurt and wanted someone to
share the pain with me” (U) (Visser et al.,
2008P.1140).
Meanwhile, the most common reasons given by the
participants for not disclosing to their friends was the
lack of trusting relationship. One of the women said:
“I am not close to them and don’t know what they
will say behind my back"
The Experiences of HIV Status Disclosure among Pregnant and Postpartum Women: A Systematic Review of Qualitative Evidence
35

Synthesized finding two:
HIV-positive women need continued support and
counselling to cope with disclosure practice as they
may experience negative outcomes of disclosure that
can negatively affect their lives and the wellbeing of
the infant.
This synthesized finding comprises two
categories:
1. Positive outcomes of disclosure
Some of the participants have reported positive
responses of disclosure from their partner or family.
The following statement was example of a woman’s
experience when disclosing the HIV-status to her
mother:
“She was very hurt, she cried but she accepted
and was supportive. I felt better after telling her”
(U) (P. 1141).
An example of a women’s positive experience of
disclosure to her partner:
“It was a shock at first but [now] we support each
other all the way. When one is down the other lifts
that one up … [after I told him] …we slept holding
each other as though we knew death [was] coming
…our love became stronger [after I disclosed]”
(U)
(Varga, Sherman & Jones, 2006, P. 957).
2. Negative outcomes of disclosure
Negative consequences of HIV-status disclosure
described by some of the percipients include
emotional rejection and indifferent reactions. The
women’s expressions describing negative outcomes
of disclosure included:
“[My husband’s family] started separating out
my things from the rest … they would lay
everything out for me, saying they wanted make
sure I had everything [I need]. I had my own
plates and cups and the would say ‘here use this.
Just use it and wash it right away’. They tried to
be polite and caring but I could see it [my HIV
status] made them uncomfortable ...” (C)
(Varga,
Sherman & Jones. 2006, P. 958).
Synthesized finding three:
Disclosure of HIV status is a complex process
comprising varied modes and patterns. Women may
also experience disclosure as fluid rather than
absolute, which means they could shift from being
ready to disclose to not being ready. Therefore,
counsellors or health care providers should continue
to engage the HIV- positive women around how
ready they feel to share their status, and keep the
clients’ status confidential to prevent involuntary
disclosure.
One category namely disclosure patterns support
this synthesized finding
Several women disclosed voluntarily to the
primary target and did it in a simple and direct
manner:
“I just went home and told him” (U)
(Varga,
Sherman & Jones. 2006, P. 955).
“I just said it straight out, I am [HIV]-positive”
(U)
(Varga, Sherman & Jones. 2006, P. 955).
In contrast, some of the women chose to disclose
indirectly to avoid a conversation about death or
blame of infection:
“My sister used to dislike people [infected] with
HIV. We were listening to this radio program
[about people living with HIV] and I said I didn’t
like the way she was talking about the people they
were interviewing. I said, ‘don’t speak badly
about these people. You yourself don’t know
where you stand [you yourself could be infected].
Some of us have had to face this [issue of living
with HIV] already’. I think she realized after that
[that I am HIV-positive]” (C)
(Varga, Sherman &
Jones. 2006, P. 956).
Interestingly, some of the women in these studies
have experienced disclosure of HIV status as a fluid
and non-linear process. This means that a dichotomy
of disclosure as having either took place or not, did
not always fit with women’s experiences.
“No I did not tell him …because he lives with my
friend, they live in the same yard; they talked
about it over there. So when he had already heard
about it over there, I said ‘yes I have it, you must
decide what you are going to do’. I just agreed.
He came to ask me, and I told him” (Moses &
Tomlinson, 2013, P. 672).
4 DISCUSSION
The synthesized findings formulated in this review
provide insights into factors that can influence the
women’s decision to disclose or not disclose their
HIV-status. This review also depicts the complexity
of HIV-status disclosure process experienced by the
women during their pregnancy and early motherhood.
This review has identified a range of reasons and
motivations for disclosure or nondisclosure of HIV
status among pregnant and postpartum women. The
women shared their HIV status to their partner
mainly because of a sense of responsibility to their
partner and to raise awareness of the risk of HIV
transmission. In contrast, the women choose to
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
36

disclose to close family members or friends to seek
emotional and practical supports. These women have
also disclosed to their family to garner support and
care for the infant as well as to ensure breast-feeding
avoidance as HIV can be vertically transmitted
through breast milk.
Meanwhile, the key factors identified as playing
role in unwillingness to disclose included fear of
violence and abandoned. Fear of abandoned was
correlated with intense fear of losing financial
support for the infant (Rujumba et al. 2012). Other
factors that negatively associated
with disclosure
included previous history
of domestic violence,
financial dependency and living with an extended
family (Tam M, Amzel A, & Phelps BR 2015).
The
implication here is that counsellors or heath care
providers should consider varying personal and
social contexts in preparing women for disclosure.
For example, women who are not working and highly
dependent on their partner may need more
counselling and help for disclosure and persuading
their partner to undertake HIV testing.
Disclosure of HIV status, especially among
pregnant women, has been found to be correlated with
lower HIV transmission rates from mother to infants
and increased maternal and infant adherence to ARV
therapy (Torpey et al. 2012; Kirsten et al., 2011).
These underline the importance of encouraging HIV
disclosure in PMTCT programmes. However,
Interventions to facilitate a safe disclosure should be
provided to minimize the risk of negative outcomes
from disclosure. The interventions may include
strategies to increase communication and relationship
building skills and working with the women to create
an individualized disclosure plan (Tam M, Amzel A,
& Phelps BR 2015; Walcott 2013).
This review reveals that discourse of HIV status
is a complex and continues process comprising
varied patterns and types. Social circumstances,
cultural norms, HIV-related media and personal
characteristics shaped how these women disclosed
(Varga, Sherman & Jones 2006). Some women chose
to disclose in a simple and direct manner, while
others disclosed indirectly to avoid conversations
that may lead to a discussion about death or blame
for infection.
Some women have experienced
involuntary disclosure caused by the media that
created a public association between particular
perinatal health practices and HIV infection. For
example advertising a particular brand of milk for
HIV-pregnant women (Varga, Sherman & Jones
2006)
.
Confidentially breach by the primary target
has also been identified as a cause of involuntary
disclosure in this review. Strategies should be
employed to prevent involuntary disclosure as it was
frequently reported to cause negative consequences
including emotional rejection and withdrawal of
material supports.
Strategies that may be utilized to reduce the
incidence of involuntary disclosure include a
promotion or branding the PMTCT programmes as a
general pregnancy health, training of the health
workers and involvement of the community in HIV
education.
An active participation of the community
in HIV education may also help to reduce HIV-
related stigma, one of the significant barriers to HIV
disclosure (Walcott et al. 2013; Arrey et al. 2015).
This review has also captured an interesting
phenomenon, that is women may experience HIV
disclosure as a non-linear and non-absolute process.
This means that the women’s experiences on HIV
disclosure not always moving from non-disclosure to
disclosure, but could change from being ready to
disclose to not being ready. Therefore, an ongoing
counselling should be provided for HIV-positive
women to engage them around how ready they feel
to disclose their status. The health workers should
also understand that the non-linear and non-absolute
process of disclosure may serve protective functions
for these women and should be respected.
As previously mentioned, after disclosing the
HIV status, women experienced varying reactions.
Although some women reported a supportive and
strengthened partner relationship as a result of the
disclosure, negative reactions were not also
uncommon. Some women expressed a guilty and
isolated feeling following their partner and family’s
reactions to the disclosure. Previous systematic
reviews have reported the similar negative outcomes
of HIV disclosure experienced by the women which
included violence, blame abandonment and disbelief
(
in order to reduce these negative outcomes, the
PMTCT education should also targets the family
members, partners and broader community rather
than merely focus on women (Medley et al. 2004;
Tam, Amzel & Phelps 2015).In cases where the
women did
experienced a violent reaction from their
partners and family, the health workers should be
ready to help with resources that can be accessed
such as the involvement of the domestic violence
agency.
The WHO has endorsed four approaches to
prevent HIV transmission in mothers and their
infants. These include the prevention of HIV
transmission to potential mothers, the prevention of
unintended pregnancy among HIV-positive women,
the prevention of mother-to-child transmission of
HIV and the provision of support, care and treatment
The Experiences of HIV Status Disclosure among Pregnant and Postpartum Women: A Systematic Review of Qualitative Evidence
37

for mothers, and their infants, families and partners
(Medley et al. 2014). The success of each element of
the four PMTCT approaches will depend on
disclosure of HIV status by the women to their
partners and family members.
Studies have identified several strategies to
facilitate a safe disclosure in the context of antenatal
care. Partner’s involvement in PMTCT programmes
is reported to be associated with increased women’s
adherence to the PMTCT recommendations
including ART therapy and non-breastfeeding
practice (Medley et al. 2014; Tam, Amzel & Phelps
2015). Couple counselling and testing during
antenatal care is one of the most favoured approaches
to increase partner involvement in
PMTCT programmes. This approach will also
eliminate the burden of HIV-status disclosure as the
couple will be tested for HIV at the same time and
thus, no one can be blamed for infecting the other
(Medley et al. 2014; Tam, Amzel & Phelps 2015).
Furthermore, home-based couple counselling and
testing can be an alternative way to increase partner
involvement and safe disclosure during ANC.
Providing HIV testing and counselling at homes was
reported to be feasible and acceptable to the health
care workers, pregnant women and their partners
(Walcott et al., 2013).
5 CONCLUSIONS
This review highlights the complexity of HIV
disclosure experienced by HIV-positive pregnant and
post-partum women. The motivations for disclosure
or non-disclosure and how these women disclosed the
status were moderated by several factors which
include personal circumstances, social contexts, and
environmental situations. The counsellors or health
workers should understand the different process
involved in disclosure to family and partners. This
review also shows that women may experience
disclosure as a fluid and non-linear process and
therefore, it important that the health workers
continuingly explore the women’s readiness to share
their status with the others.
REFERENCES
Adeoye-Agboola, D. I., Evans, H., Hewson, D., & Pappas,
Y., (2016), Factors influencing HIV disclosure among
people living with HIV/AIDS in Nigeria: a systematic
review using narrative synthesis and meta-analysis,
Public Health, vol. 136, pp. 13-28, doi:
10.1016/j.puhe.2016.02.021.
Arrey, AE, Bilsen, J., Lacor, P., Deschepper, R., (2015),
“It’s My Secret”: Fear of Disclosure among
SubSaharan African Migrant Women Living with
HIV/AIDS in Belgium, PLoS ONE, vol.10, no. 3,
:e0119653.
Bwirire, L. D., Fitzgerald, M., Zachariah, R., Chikafa, V.,
Massaquoi, M., Moens, M., Schouten, E. J., (2008),
Reasons for loss to follow-up among mothers registered
in a prevention-of-mother-to-child transmission
program in rural Malawi, Transactions of the Royal
Society of Tropical Medicine and Hygiene, vol. 102, no.
12, 1195-1200. doi: 10.1016/j.trstmh.2008.04.002.
Farquhar, C., Mbori-Ngacha, D. A., Bosire, R. K., Nduati,
R. W., Kreiss, J. K., & John, G. C., (2001), Partner
notification by HIV-1 seropositive pregnant women:
Association with infant feeding decisions, AIDS, vol.
15, no. 6, 815-817. doi: 10.1097/00002030-200104130-
00027.
Kasenga, F., Hurtig, A.-K., & Emmelin, M., (2010), HIV-
positive women's experiences of a PMTCT programme
in rural Malawi, Midwifery, vol. 26, no. 1, pp. 27-37.
doi: http://dx.doi.org/10.1016/j.midw.2008.04.007.
Madiba, S., & Letsoalo, R., (2013), HIV Disclosure to
Partners and Family among Women Enrolled in
Prevention of Mother to Child Transmission of HIV
Program: Implications for Infant Feeding in Poor
Resourced Communities in South Africa, Global
Journal of Health Science, 5(4), 1-13. doi:
10.5539/gjhs.v5n4p1
Makin, J. D., Forsyth, B. W., Visser, M. J., Sikkema, K. J.,
Neufeld, S., & Jeffery, B., (2008), Factors affecting
disclosure in South African HIV-positive pregnant
women. AIDS Patient Care STDS, vol. 22, no. 11, pp.
907-916. doi: 10.1089/apc.2007.0194
Medley, A., Garcia-Moreno, C., McGill, S., & Maman, S.,
(2004), Rates, barriers and outcomes of HIV serostatus
disclosure among women in developing countries:
Implications for prevention of mother-to-child
transmission programmes. Bulletin of the World Health
Organization, vol. 82, no. 4, pp. 299-307.
Moses, S., & Tomlinson, M., (2013), The fluidity of
disclosure: A longitudinal exploration of women's
experience and understanding of HIV disclosure in the
context of pregnancy and early motherhood. AIDS Care
- Psychological and Socio-Medical Aspects of
AIDS/HIV, vol. 25, no. 6, pp. 667-675, doi:
10.1080/09540121.2012.736606.
Rujumba, J., Neema, S., Byamugisha, R., Tylleskär, T.,
Tumwine, J. K., & Heggenhougen, H. K., (2012).
“Telling my husband I have HIV is too heavy to come
out of my mouth”: pregnant women's disclosure
experiences and support needs following antenatal HIV
testing in eastern Uganda. Journal of the International
AIDS Society, vol. 15, no. 2, p. 17429. doi:
10.7448/IAS.15.2.17429.
Sendo, E. G., Cherie, A., & Erku, T. A., (2013), Disclosure
experience to partner and its effect on intention to
utilize prevention of mother to child transmission
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
38
service among HIV positive pregnant women attending
antenatal care in Addis Ababa, Ethiopia. BMC Public
Health, vol. 13, pp. 765-765, doi: 10.1186/1471-2458-
13-765.
Tam, M., Amzel, A., & Phelps, B. R., (2015), Disclosure of
HIV serostatus among pregnant and postpartum women
in sub-Saharan Africa: a systematic review, AIDS Care,
vol. 27, no. 4, pp. 436-450. doi:
10.1080/09540121.2014.997662.
The Joint United Nations Programme on HIV/AIDS,
(2015), Fact sheet 2016, Retrieved from:
http://www.unaids.org/sites/default/files/media_asset/
UNAIDS_FactSheet_en.pdf.
The World Health Organization, (2013), HIV/AIDS:
Mother-to-child transmission of HIV [online].
Retrieved from:
http://www.who.int/hiv/topics/mtct/about/en/.
Torpey K., Mandala J., Kasonde P., Bryan-Mofya G.,
Bweupe M., Mukundu J., et al, (2012), Analysis of HIV
Early Infant Diagnosis Data to Estimate Rates of
Perinatal HIV Transmission in Zambia. PLoS ONE.
vol. 7, no. 8.
Ujiji, O. A., Ekström, A. M., Ilako, F., Indalo, D.,
Wamalwa, D., & Rubenson, B., (2011), Reasoning and
deciding PMTCT-adherence during pregnancy among
women living with HIV in Kenya, Culture, Health and
Sexuality, vol. 13, no. 7, pp. 829-840, doi:
10.1080/13691058.2011.583682
Varga, C. A., Sherman, G. G., & Jones, S. A., (2006), HIV-
disclosure in the context of vertical transmission: HIV-
positive mothers in Johannesburg, South Africa. AIDS
Care, vol. 18, no. 8, pp. 952-960. doi:
10.1080/09540120500356906.
Visser, M. J., Neufeld, S., de Villiers, A., Makin, J. D., &
Forsyth, B. W. C., (2008), To tell or not to tell: South
African women's disclosure of HIV status during
pregnancy, AIDS Care, vol. 20, no. 9, pp. 1138-1145.
doi: 10.1080/09540120701842779.
Walcott MM, Hatcher AM, Kwena Z, Turan JM., (2013),
Facilitating HIV status disclosure for pregnant women
and partners in rural Kenya: a qualitative study, BMC
Public Health, vol. 13, no. 1, pp. 1-25.
APPENDIX
Extracted Findings
Extracted
themes
Illustrative quotes
Level of
credibility
Visser et al.
(2008)
Disclosing HIV
status to raise
risk
awareness for
changes in
lifestyles
Responsibility/
obligation
given the
relationship
Being in
supportive
and trusting
relationships
Explanation of
behaviour,
illness and
death
“I told him to inform
him that we are both
HIV positive and
that we need to
change our life
styles” Visser et al.
(P. 1140).
“He has the right to
know as the father
of the expected
child. I had the
responsibility to
disclose” Visser et
al. (P. 1140).
“There is no other
person but my
mother I could tell,
knowing that she’d
help me. She
understands. A
mother is a mother”
Visser et al. (P.
1140).
“I wanted them to know
what killed me and
ask them to look
after my children
when I am dead”
Visser et al. (P.
1140).
Unequivocal
Unequivocal
Unequivocal
Credible
Fear of violence
Protect others
from the
results
Lack of trusting
relationships
Experiencing
supportive
and accepting
reactions of
HIV-status
disclosure
“I don’t know how to tell
him, he often says
he would kill me if I
told him that I am
infected because he
does not have HIV”
Visser et al. (P.
1141).
“My mother is sick. She
had a stroke. I can’t
tell her because it
will affect her
health” Visser et al.
(P. 1141).
“I am not close to them
and don’t know
what they will say
behind my back”
Visser et al. (P.
1141).
“She was very hurt, she
cried but she
accepted and was
supportive. I felt
better after telling
her” Visser et al. (P.
1141).
Credible
Unequivocal
Credible
Unequivocal
The Experiences of HIV Status Disclosure among Pregnant and Postpartum Women: A Systematic Review of Qualitative Evidence
39
Experiencing
indifferent
reaction
when
disclosing
HIV status
to the
partner
“He just looked at me and
turned the other way
without saying a
word. He acts as if I
did not tell him a
serious thing” Visser
et al. (P. 1141).
Credible
Extracted
themes
Illustrative quotes
Level of
credibility
Varga,
Sherman, Jones
(2006)
Voluntary
direct
disclosure
Voluntary
indirect
disclosure
Involuntary
disclosure of
HIV status
“I just went home and told
him”, “I just said it
straight out” Varga,
Sherman, Jones (P. 955).
“My sister used to dislike
people [infected] with
HIV. We were listening to
this radio program [about
people living with HIV]
and I said I didn’t like the
way she was talking about
the people they were
interviewing. I said,
‘don’t speak badly about
these people. You
yourself don’t know
where you stand [you
yourself could be
infected]. Some of us
have had to face this
[issue of living with HIV]
already’. I think she
realized after that [that I
am HIV-positive]” Varga,
Sherman, Jones (P. 956).
“They show everything on
TV [quoting a
documentary on the
nevirapine controversy]
...’mothers who are
infected, they use this and
that [nevirapine and infant
formula]. They are
infected and they get this
Pelargon for free at the
hospital’ 10 o’clock in the
morning they are showing
this thing. We were
watching and [my family]
asked why I use that milk
[Pelargon] they show on
the TV to feed the baby.
Do I get it for free at the
hospital like they [the
HIVpositive women
featured in the
documentary] do? So I
lied to them. I told them
the hospital is selling this
milk, you pay for your
monthly supply. They
never said anything more
Unequivocal
Credible
Credible
Extracted
themes
Illustrative quotes
Level of
credibility
Disclosing
HIV-status to
ensure breast
feeding
avoidance
about it, but I couldn’t
stop wondering if now
they think I am [HIV]-
positive” Varga, Sherman,
Jones (p. 956).
“I told them [family
members] exactly why
[the baby] is using a
bottle. As soon as I found
out about my result, I told
them I have been tested
and that I am
Unequivocal
HIV-positive so I will
have to give the bottle
and I am not supposed to
breastfeed. After that,
they stopped pressuring
me. My mother [is now]
supportive and helps me
to make bottles and feed
[the baby] properly”
Varga, Sherman, Jones
(P. 957).
Disclosure is
necessary to
solicit care
and support
for the infant
Experiencing
strengthened
partner
relationship
after HIV
disclosure
“After I got very sick
…my boyfriend panicked.
It was better to cough it
up [disclose] in case
things got worse. So we
just told them. We needed
to support in case
something happens to me
…I think about [the
baby’s] future, if it
happens that I die. Now
her future is secure [there
will be someone to look
after her]” Varga,
Sherman, Jones (P. 957).
“It was a shock at first but
[now] we support each
other all the way. When
one is down the other lifts
that one up … [after I told
him] …we slept holding
each other as though we
knew death [was] coming
…our love became
stronger [after I
Unequivocal
Unequivocal
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
40
Extracted
themes
Illustrative quotes
Level of
credibility
Feeling self-
conscious,
trapped and
isolated
following
family
reactions after
HIV-status
disclosure
disclosed]” Varga,
Sherman, Jones (P. 957).
“[My husband’s family]
started separating out my
things from the rest …
they would lay everything
out for me, saying they
wanted make sure I had
everything [I need]. I had
my own plates and cups
and the would say ‘here
use this. Just use it and
wash it right away’. They
tried to be polite and
caring but I could see it
[my HIV status] made
them uncomfortable …on
my side [of the family]
they are too [heavy
emphasis] supportive.
They are too concerned.
They are always asking
me ‘Are you okay? Are
you getting sick?’ so now
I have started feeling
guilty …they are too
focused on me. [I feel as
though] my life is longer
[my own] Varga,
Sherman & Jones (P.
958).
Credible
Extracted
themes
Illustrative quotes
Level of
credibility
Moses &
Tomlinson
(2013)
Experiencing
HIV-status
disclosure as a
non-absolute
and non-linear
process
Indirect
disclosure
“I’m not gonna tell [my
mother]. Maybe she’s
gonna find out. But my
mother, I don’t know but
if I remember it was,
maybe it was 2005 or
2006, I did tell my
mother, but like in a nice
way, it was like a joke.
No, she said to me, ‘oh
you’re sick but you are
drinking, smoking, what
about your life?’ it ends
there, we never talk
about it again, so I don’t
know maybe she still
remembers that or not”
Moses & Tomlinson (P.
672).
“No I did not tell him
…because he lives with
my friend, they live in the
same yard; they talked
about it over there. So
when he had already
heard about it over there,
Credible
Credible
Extracted
themes
Illustrative quotes
Level of
credibility
Disclosing
HIV status to
garner
emotional and
practical
support
Fear of being
blamed and
abandoned
I said ‘yes I have it, you
must decide what you are
going to do’. I just
agreed. He came to ask
me, and I told him”
“I asked him; ‘what if
you could go and get
tested? Or maybe I am
making an example: ‘if I
turned out positive, what
would you do?’ … I was
joking, I wanted to see
what he was going to do”
Moses & Tomlinson (P.
672).
“Pumla was very
stressed…she said to me
‘how are [my] children
going to grow without
their father?’… as Pumla
talking you could feel
her frustration anger,
saying that ‘if only I
hadn’t fallen pregnant’,
and ‘why did my
boyfriend ask for another
child only to find out that
he’s going to leave them.
Who’s going to look
after his children?’ but
she is happy that her
sister-in-law is
supporting her at all
times” Moses &
Tomlinson (P. 673).
“Because if I tell him, he
will leave me here with
this baby, because he will
say I am the one who
brought this to him”
Moses & Tomlinson (P.
670).
Credible
Unequivocal
The Experiences of HIV Status Disclosure among Pregnant and Postpartum Women: A Systematic Review of Qualitative Evidence
41
