
Nevus Comedonicus, a Rare Case: Dermoscopic and
Histopathological Findings
Adniana Nareswari
1*
, Mardiana
1
, Nugrohoaji Dharmawan
1
, Oyong
2
1
Dermatovenereology Department Medical Faculty of Sebelas Maret University/ Dr. Moewardi General Hospital,
Surakarta, Indonesia
2
Pathology Anatomy Department Medical Faculty of Sebelas Maret University/ Dr. Moewardi General Hospital,
Surakarta, Indonesia
Keywords: Nevus, nevus comedonicus, adnexal hamartoma.
Abstract: Nevus comedonicus is a very rare adnexal hamartoma of pilosebaceous apparatus, with approximately 200
cases reported in the literature so far. It appears as cluster of adjacent dillated follicular openings with firm
pigmented keratin plugs resembling comedones. The comedones oftentimes arranged in linear or
zosteriform pattern, paralled to Blaschko’s lines. The lesions are commonly unilateral, although bilateral
occurence have been reported. The predilection sites are face, neck, upper arms, chest and abdomen. We
report a case of a 5-year-old boy with open brown to black comedones in a linear pattern localized on the
back of the left thigh that appearing since birth. The lesions gradually increased in number and size. The
plugs were firm and difficult to be extracted mechanically, leaving a big pore on the skin. Pain, itch and
discharge were not obtain. There were some episodes of infection, due to manual removal done by his
mother which left some hypertrophic scars. The patient was otherwise healthy, without any congenital
abnormalities, extracutaneous lesion, and internal involvement. Dermoscopic examination revealed the
distinctive pattern consisting of pigmented, sharply demarcated keratin plugs of 1-3 mm in diameter, some
open pores, multiple structurless, various shades of brown homogenous circular areas surrounding the plugs.
Punch biopsy of the lesion histologically showed an aggregation of dilated follicular infundibulum with
laminated keratinous material plugging. The follicular walls were comprised of several keratinocyte layers.
Based on the history taking, typical features of the lesion, dermoscopic and histopathological findings, this
patient was then diagnosed with nevus comedonicus.
1 INTRODUCTION
Nevus comedonicus is an extremely rare
developmental abnormality of the pilosebaceous
unit, which presenting as a constellation of dilated
follicular orifices filled with dark keratinous plugs.
It was first described as ‘comedo nevus’
(Kofmann,1895).
Its prevalence has been estimated
from 1 in 45,000 to 1 in 100,000, affecting any race
and gender (Kaliyadan,2017).
Retrospective study
conducted in Mexico City from 1971 to 2001,
among 417,511 paediatric patients , 443 displayed
epidermal naevi, but only 5 of them diagnosed as
nevus comedonicus (Vidaurri,2004). In Indonesia
itseft, there is no data on nevus comedonicus
prevalence.
The diagnosis of nevus comedonicus is relatively
easy. It has a typical and different feature compared
to other epidermal nevi. Dermoscopy, a safe non-
invasive easy-to-repeat diagnostic method mainly
used in melanocytic lesion helps in establishing the
diagnosis of nevus comedonicus (Winciorek,2011).
However the use of this tool is rare, and only a few
reports has been published regarding its use. A
typical histopathological feature confirms the
diagnosis in uncertain case.
This study aimed to present a rare case of nevus
comedonicus with regard to its clinical,
dermoscopic, histopathological features and the use
of dermoscopy in this rare condition.
2 CASE
A 5-year-old Indonesian boy presented to our
outpatients clinic, Dermatovenereology Department,
Nareswari, A., Mardiana, ., Dharmawan, N. and Oyong, .
Nevus Comedonicus, a Rare Case: Dermoscopic and Histopathological Findings.
DOI: 10.5220/0008160204810484
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 481-484
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
481
dr. Moewardi General Hospital, Surakarta, Indonesia
for evaluation of open brown to black, firm and
protude comedones, localized to the back of his left
thigh in a linear pattern along Blaschko’s lines
(Figure 1), which has occured since birth. His
mother reported that the lessions gradually increased
in number and size with time. The patient ever been
evaluated in our hospital when he was 1 month old.
At that time he received various topical treatments
but there was no satisfactory improvement.
The parents took him again to our outpatient
clinic after years due to their concern about this
asymptomatic lesion which became increased in
number and size. There were no complaints of pain,
itch and discharge. His mother tried to remove the
plugs herself which left a big pore on the skin and
caused some episodes of infections. Though it
healed, it left some hypertrophic scars. Medical
history was unremarkable with no similiar complaint
in his family. The parents denied for consanguity.
Pregnancy and labor were uneventful. The mother
also denied for any drug consumption during
pregnancy.
Clinical examination on his back of the left thigh
revealed multiple, comedo-like openings with brown
to black, firm keratin plugs dispersed over a
hypopigmented, linear spot of 20 cm x 4 cm, with
some hypertrophic scars on it. His vital signs, body
weight and height were normal for his age. There
was no other cutaneous findings on the other part of
body.
Ophthalmological and neurological examinations
did not reveal any abnormality. Laboratory findings
(complete blood count, liver functions and kidney
functions) were unremarkable. The dermoscopic
revealed the distinctive pattern consisting of
pigmented, sharply demarcated keratin plugs of 1-3
mm in diameter, some open pores, multiple
structurless, various shades of brown homogenous
circular areas surrounding the plugs (Figure 2A). A
3 mm punch biopsy was obtained from his back of
the left thigh. Histopathological examination
showed an aggregation of dilated follicular
infundibulum with laminated keratinous material
plugging. The follicular walls were comprised of
several layers of keratinocytes. Epidermis was
within normal limit (Figure 2B). This patient was
diagnosed with nevus comedonicus based on the
history taking, clinical examination which pictured
the typical lesion of nevus comedonicus,
dermoscopic and histopathological finding.
3 DISCUSSION
Nevus comedonicus is an extremely rare
dermatological problem with an estimated
occurrence of 1 case in every 45,000–100,000
individuals (Kaliyadan,2017). A study by Inoue et
al., reported that there were only 200 cases until the
year of 2000 (Inoue,2000). A retrospective study
conducted in Mexico City from 1971 to 2001,
among 417,511 paediatric patients , 443 displayed
epidermal naevi, but only 5 of them diagnosed as
nevus comedonicus (Vidauri,2004).
There has not
been any data about the prevalence or even the case
report of nevus comedonicus in Indonesia so far.
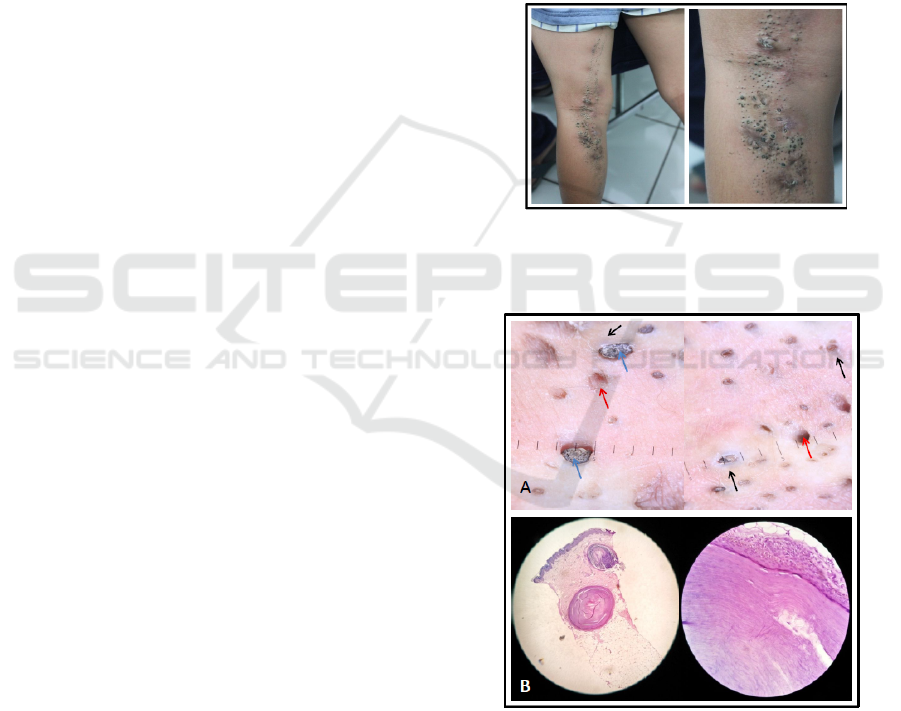
Figure 1. Nevus comedonius on the back and left thigh. A
cluster of firm, pigmented, protrude comedo-like papules
in a linear pattern along Blaschko’s line.
Figure 2. A: Dermoscopy of nevus comedonicus. Multiple
dillated follicular openings (red arrow) with pigmented
keratin plugs 1-3 mm in diameter (blue arrow) and
structurless, various shades of brown homogenous circular
areas surrounding the plugs (black arrow). B:
Histopathology of nevus comedonicus. Laminated
keratinous material plugging on dermis and epidermis
within normal limit. The follicular walls are comprised of
several keratinocyte layers.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
482

Approximately 50% of nevus comedonicus cases
appear at birth, with the other 50% developed
symptoms during childhood, usually before the age
of 10 years. There is no predilection for race or
gender (Pierson,2003).
Clinically, nevus comedonicus present as a
collection of discrete, dilated follicular ostia plugged
with horny brown to black pigmented keratin. The
lesions are most commonly found on face, neck,
upper arms, chest and abdomen, usually arranged in
groups, bands, or in a linear pattern along
Blaschko’s lines (Solomon,1975).
Normally it is
unilateral but can be bilateral in certain case
(Mahran,2017).
Nevus comedonicus is classified
into two groups, reflecting the severity of the
condition: the first group is characterized by the
presence of slightly pronounced skin lesions or
comedo-like changes, which represent only a
cosmetic defect, the second one presents with severe
cutaneous symptoms including large cysts with
scarring, often with a tendency to recurrence with
the formation of fistulas and abscesses
(Guldbakke,2007).
Nevus comedonicus in unusual
cases, may appear as an extensive inflammatory
lesion involving large areas of the body, with
inflammation and residual scarring (Kirtak,2004).
Several disorders have been known to be
associated with nevus comedonicus. Cases showing
any of these findings are included in nevus
comedonicus syndrome, an entity considered within
the larger group of epidermal nevus syndrome.
Nevus comedonicus syndrome is characterized as a
combination of nevus comedonicus with ocular
defect (cataracs, corneal erosion), skeletal defect
(syndactily, clinodactily, preaxial polydactily,
absence of a ray of hand bones, scoliosis, vertebral
defects) and neurologic defect (microcephaly,
mental deficiency, dysgenesis of corpus callosum)
(Happle,2010). In our patient, the nevus
comedonicus present alone without any other
cutaneous or extracutaneous lesion and also no
abnormalities found in ophtalmological and
neurological examination.
In our patient, the dermoscopic examination
revealed the distinctive pattern consisting of dark,
sharply demarcated keratin plugs of 1-3 mm in
diameter, some open pores, numerous structurless,
circular and barrel shaped, homogenous areas with
hyperkeratotic plugs of various shades of brown.
These features were suggestive of nevus
comedonicus. Winciorek and Spiewak defined
dermoscopic features of nevus comedonicus as
numerous circular and barrel-shaped homogenous
areas in light and dark-brown shades with
remarkable keratin plugs (Winciorek,2013).
Dermoscopy as a diagnostic tool is safe, non-
invasive and easy-to-repeat prosedure which is
mainly used in melanocytic lesion. Its also helpful in
diagnosing nevus comedonicus (Winciorek,2011).
However, the use of this diagnostic tool has not been
widely applied, only two reports have been
published (Winciorek,2013) (Vora,2017).
Dermoscopy is useful in differentiating nevus
comedonicus from comedones of acne and other rare
epidermal nevi, such as sebaceous nevus and hair
follicle nevus. Comedones of acne vulgaris show
numerous, homogenous areas, light and dark-brown,
sometimes black in color, depending on the type of
acne, open or closed comedones, predominantly
circular and situated superficially on dermoscopy.
Sebaceous nevus shows bright, yellow spot which
are not associated with hair follicles. Many follicular
openings and interfollicular “pseudo-pigment
network” on dermoscopy characterized hair follicle
nevus (Okada,2008).
Histopathological examination of nevus
comedonicus demonstrate a wide, deep invagination
of the epidermis filled with keratin. These
invaginations resemble dilated hair follicle; in fact,
as evidence that they actually represent rudimentary
hair follicles, occasionally found in the lower
portion of an invagination one or even several hair
shafts (Elder,2009). These similiar with histological
findings of our patient. Histologically it is important
to differentiate it with comedonal acne. In
comedonal acne, the pilosebaceous units are
complete whereas those in nevus comedonicus are
poorly formed. Furthermore in nevus comedonicus,
hyperkeratosis and papillomatosis are frequently
seen in the interpapillary epidermis and absent in
comedonal acne. Dilated pore of Winer can
sometimes be confused with nevus comedonicus
histologically. However, this condition is usually
observed in the elderly and can be differentiated
clinically.
Clinical findings themself can be used to
establish the diagnosis of nevus comedonicus as the
diagnosis of nevus comedonicus is predominantly
clinical. The differentiation of nevus comedonicus
from other epidermal nevi is easy as the former
shows presence of “comedones”, which on
extraction will leave a big pore on the skin surface.
The finding of groups of lesions paralleled to
Blascko’s lines ruled out comedonal acne. In the
majority of cases, dermoscopy may prove helpful
while biopsy is only indicated in uncertain cases.
Nevus Comedonicus, a Rare Case: Dermoscopic and Histopathological Findings
483

4 CONCLUSION
Diagnosing nevus comedonicus is relatively easy,
however clinician should be aware of the potential
association of nevus comedonicus with other
cutaneous lesion and extracutaneous features, such
as occular, skeletal and neurologic abnormalities as
nevus comedonicus syndrome. Furthermore, our
case report shows a typical feature and dermoscopic
findings of nevus comedonicus wich is rarely
described in literature. This case report also prove
that dermoscopy examination, a simple non-invasive
diagnostic tool is very helpful in diagnosing nevus
comedonicus. We recommend this tool to
differentiate the diagnosis of other rare epidermal
nevi, such as sebaceous nevus and hair follicle nevus
while histopathological examination should be
performed only in uncertain cases.
REFERENCES
Elder, D.E., Elenitsas, R.,et al., 2009. Lever’s
Histopathology of The Skin. 10th re. Ed. Lippincott
Williams & Wilkins. P.793.Happle R.2010.The group
of epidermal nevi syndrome Part I - Well defined
phenotypes. J Am Acad of Derm. Vol 63: 1-23.
Guldbakke, K. K., Khachemoune, A., Deng, A., & Sina,
B., 2007. Naevus comedonicus: a spectrum of body
involvement. Clinical and Experimental Dermatology:
Clinical dermatology, 32(5), pp. 488-492.
Inoue, Y., Miyamoto, Y., & Ono, T., 2000. Two cases of
nevus comedonicus: successful treatment of keratin
plugs with a pore strip. Journal of the American
Academy of Dermatology, 43(5), pp. 927-929.
Kaliyadan, F., & Bhimji, S., 2017. Nevus comedonicus; in
StatPearls. Treasure Island, StatPearls Publishing.
Kirtak, N., Inaloz, H. S., Karakok, M., Erguven, H. G., &
Ozgoztasi, O., 2004. Extensive inflammatory nevus
comedonicus involving half of the body. International
journal of dermatology, 43(6), pp. 434-436.
Kofmann, S., 1895. A case of rare localization and
spreading of Comedones. Arch Dermatol Syphilol, 32,
177-178.
Mahran, A.M., Abdelsamea, G.M., Mekkawy, M.M.,
2017. Bilateral nevus comedonicus succesfully treated
with topical adapalene: a case report. Clinical
Dermatology Journal, Vol 2 issue 6.
Okada, J., Moroi, Y., Tsujita, J., et al., 2008. Hair follicle
nevus – a dermoscopic approach. Eur J Dermatol. 18:
185-7.Pierson D, Bandel C, Ehrig T et al.2003.Benign
epidermal tumors and proliferations. In: Dermatology
(Bolognia JL, Joseph LJ, Rapini RP, eds). London:
Mosby.1712–1713.
Solomon, L. M., & Esterly, N. B., 1975. Epidermal and
other congenital organoid nevi. Current problems in
pediatrics, 6(1), 3-56.
Vidaurri‐de la Cruz, H., Tamayo‐Sánchez, L., Durán‐
McKinster, C., De La Luz Orozco‐Covarrubias, M., &
Ruiz‐Maldonado, R., 2004. Epidermal nevus
syndromes: clinical findings in 35 patients. Pediatric
dermatology, 21(4), 432-439.
Vora, R. V., Kota, R. S., & Sheth, N. K., 2017.
Dermoscopy of Nevus Comedonicus. Indian
dermatology online journal, 8(5), pp. 388-388.
Winciorek, G.K., & Śpiewak, R., 2011. Basic dermoscopy
of melanocytic lesions for beginners. Postępy Hig
Med Dośw (Online). 65, p. 501-508.
Kamińska-Winciorek, G., & Śpiewak, R., 2013..
Dermoscopy on nevus comedonicus: a case report and
review of the literature. Advances in Dermatology and
Allergology/Postȩpy Dermatologii i
Alergologii, 30(4), 252-254.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
484
