
Case Report: A Case of Full Expressivity Piebaldism
Itrida Hadianti
1
, Prasta Bayu Putra
1
, Sekar Sari Arum Palupi
1
, Hanggoro Tri Rinonce
2
, Irianiwati
2
,
Hardyanto Soebono
1
, Sunardi Radiono
1
1
Department of Dermatology & Venereology, Faculty of Medicine, Universitas Gadjah Mada / Dr. Sardjito General
Hospital, Yogyakarta, Indonesia
2
Departement of Anatomical Pathology, Faculty of Medicine, Universitas Gadjah Mada / Dr. Sardjito General Hospital,
Yogyakarta, Indonesia
Keywords: piebaldism, full expresivity, new mutant.
Abstract: Piebaldism is a rare inherited disease with a specific clinical manifestation. Here with, we reported a case
of piebaldism in a 17-year-old boy with the feature of a severe phenotype (full expressivity). White
forelock, poliosis, and depigmented patch observed on midline forehead and neck along with ventral and
lateral trunk, mid-arms, thighs, knees, and the lower leg area were found. Hyperpigmented macule between
depigmented lesions were found in all the lesions. The patient was a new mutant since his both parents were
normal. The diagnosis was established based on clinical appearance, histopathological examination, and
immunohistochemistry staining with S100, HMB45, and Fontana-Masson.
1 INTRODUCTION
Piebaldism (OMIM #172800) is an rare autosomal
dominantly inherited pigment anomaly characterized
by a congenital white forelock and leukoderma on
the frontal scalp, forehead, ventral trunk and
extremities (Oiso,2012). Its first descriptions date
back to early Egyptian, Greek and Roman writings
an it has been observed throughout history in
families with a distinctive, predictable congenital
white forelock (Spritz,1994). Although piebaldism is
a skin condition which occurs in limited and fixed
areas, it remains a social problem in patients so that
piebaldism therapy becomes a challenge to date
(Thomas,2004). The absence of melanocyte in
affected areas of the skin and hair is due to mutation
of the KIT protooncogenes, which affects the
differentiation and migration of melanoblast.
Piebaldism can also be caused by heterozygous
mutation in the gene encoding the zinc finger
transcription factor SNAI2 (Sanchez,2003)
(Taieb,2016).
The incidence of piebaldism is estimated to be
less than 1 among 20,000 people. Piebaldism
reported in all races with equally number between
women and men. The incidence of such cases is
estimated to be less than 1 among 20,000 people
(Agarwal,2012).
Medical record data of Dr. Sardjito
General Hospital showed that no case of piebaldism
were recorded for last 5 years and this is the first
case report of full expressivity piebaldism in
Indonesia.
Here with, we reported a case of piebaldism in a
17-year-old boy with the feature of a severe
phenotype. Piebaldism is a rare case, so this paper
may add some knowledge in giving a differential
diagnosis of skin disorders in the form of patch
depigmentation. Piebaldism become a challenge for
the dermatologist in diagnosis and therapy.
2 CASE
A 17-year-old boy from Purbalingga, Central Java,
came to the Dermatology and Venereology
Outpatient Clinic of Dr. Sardjito General Hospital
Yogyakarta, with the chief complaint of white
patches on his face and almost the entire body. He
had a white patches on the forehead and neck along
with white hair on the frontal part of the head.
Leukoderma appearance was also found in the chest,
abdomen, mid-arms, thighs, knees, and the lower leg
area. There were no complaints of visual
impairment, hearing loss, or expansion of the skin
Hadianti, I., Putra, P., Palupi, S., Rinonce, H., Irianiwati, ., Soebono, H. and Radiono, S.
Case Report: A Case of Full Expressivity Piebaldism.
DOI: 10.5220/0008160004730476
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 473-476
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
473
lesion areas of the patient. He never had any therapy
for the compaints before and no history of atopy and
drug allergy. Both of his parents were reported
without pigmentary disorders. The patient denied
any previous similar history of complaints, atopy,
drug allergy nor diabetes in the family members.
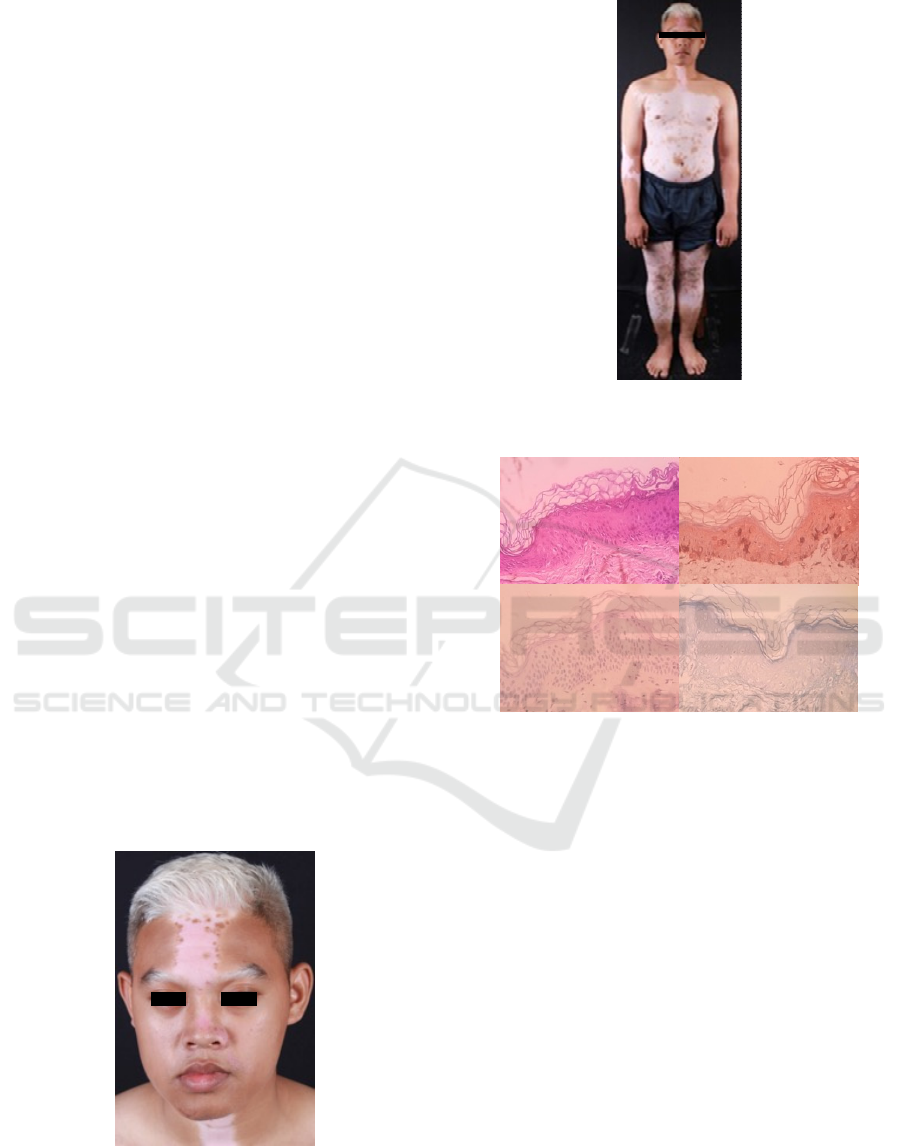
The general condition was good and dermatology
status showed a white forelock and poliosis on the
hair and medial eyebrow (Figure 1). There was
depigmented patch along the forehead until the nose
with hyperpigmented macule on the border area.
There were similar lesions on the neck, chest,
abdomen, the extensor sides of upper extremities,
thighs, knees, and up to the lower limbs in the form
of depigmented patches with edges and those of
which are hyperpigmented and normal pigmentation
macules (Figure 2). There was white hair on the
depigmented lesion. On the upper right and left back
showed ill-defined border of hypopigmented patches
and multiple hyperpigmented macules spread among
them. No skin lesions were found in the vertebral
area, hands, and feet. The differential diagnosis
presented for the patient was piebaldism, vitiligo and
Waardenburg syndrome.
Skin biopsy of depigmented area in the chest was
performed. Histopathologic examination revealed
basket weave type orthokeratosis, focal spongiosis,
and basal epidermal cell vacuolization. Melanocyte
and melanin were not found in the basal layer. There
was mild infiltration of inflammatory cells in the
perivascular and peri-appendicular area of the
dermis (Figure 3A). We also performed
immunohistochemistry staining with s100 and
Human Melanona Black 45 showed no positive
expression on melanocyte (Figure 3B&C). No
epidermal melanin were observe in Fontana-Masson
staining (Figure 3D).
Figure 1. White forelock and poliosis on the hair and
medial eyebrows.
Figure 2. Depigmented patch on neck, chest, abdomen,
and extremities in simetrically distribution.
Figure 3. Hematoxylin Eosin (A), S100 (B), HMB 45
(C), and Fontana-Masson (D) staining (x40)
The diagnosis of piebaldism was established by
clinical appearance, histopathological examination,
and immunohistochemistry staining with S100,
HMB45, and Fontana-Masson. The therapy was not
given to the patient due to family consideration of
the possibility for healing, the extent of the area of
the body involved, and also the transportation
problem.
3 DISCUSSION
Piebaldism is a pigmentation disorder that is
inherited by autosomal dominant means and rarely
occurs. It is mainly due to mutation in the KIT gene
(Xu,2016). KIT protooncogene encodes the cell-
surface receptor transmembrane tyrosine kinase for
the steel factor, an embryonic growth factor
(Thomas,2004). The formation of color of the skin,
A
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
474

hair, and eyes is determined by a multistep process:
(i) melanoblast migration to the skin of the embryo;
(ii) proliferation and survival of the melanocytes in
the basal layer of the epidermis; (iii) biogenesis of
the melanosomes in the melanocytes; (iv) production
of melanin granules in the melanosomes in the
melanocytes; (v) translocation of melanosomes from
the perinuclear region to peripheral region of the
melanocytes ; (vi) transfer of the melanosomes from
the melanocytes to the keratinocytes; and (vii)
translocation of the transferred melanin granules
from peripheral region to the supranuclear region of
the keratinocytes. Damage during the initial step
bring migration of the melanoblast in embryo and
induces most or all of the loss of the melanocytes in
the ventral skin and hair after birth. This is due to
melanoblasts originating from neural crest located in
the dorsal area and then migrating to the ventral area
(Oiso,2012).
The term piebald stems from the Latin word for
“magpie” and is used to describe animals whose
bodies are covered in blck and white patches
(Huang,2016). Piebaldism has a clinical picture of
white forelock and leucoderma in the scalp of the
frontal region, forehead, ventral trunk, and
extremities. Patients with piebaldism have hair and
skin depigmentation that is visible since birth, which
is relatively stable and persistent. White forelock
would often form a triangle shape and might result
as the only one manifestation in 80-90% of cases,
although the involvement can also be found on the
hair and skin in the area of the forehead that occurs
altogether (Oiso,2012). The description of poliosis is
based on the presence of localized patch on the
white hair. Poliosis can also affect the eyebrow and
eyelashes. There is a depigmented patch on the skin
with an irregular shape found on the face, trunk, and
extremities with symmetrical distribution. In
general, there are hyperpigmentation islands within
and at the border of the depigmentation area
(Thomas,2004). Patients with piebaldism may
develop café-au-lait spots (Oiso,2012). Pigmentary
anomalies in piebaldim are typically restricted to the
hair and skin. Some patients may get spontaneous
repigmentation, either partially or completely,
especially after injury (Thomas,2004).
Genetic analysis revealed that there was a
consistent relationship between genotype and
phenotype of piebaldism. Clinical manifestations
and phenotypic severity of piebaldism strongly
correlate with the site of mutations within the KIT
gene. Dominant negative missense mutation of the
intracellular tyrosine kinase domains appear to yield
the most severe phenotypes, while mutations of the
amino terminal extracellular ligand binding domain
result in haploinsufficiency and are associated with
the mildest forms of piebladism. Intermediate
phenotype are seen with mutation near the
transmembrane region (Thomas,2004). The severe
form shows a tipical white forelock on the frontal
scalp and relatively larger leukoderma on the chest,
abdomen, arms, and legs. The mild type may only
show relatively smaller leukoderma on the ventral
trunk and / or an extremity without a white forelock.
The moderate phenotype has an intermediate
appearance between the mild and severe form
(Oiso,2012)(Spritz,1994). In our patient, there was a
complaint of white patches on the body and white
hair on the front of the head that appeared from the
moment of birth. The stable depigmentation of the
patch depigmentation in the patient is suitable for
the description of piebaldism. This patient was
considered as severe phenotype and full expressivity
based on skin involving area and and location of the
lesion.
Melanocytes were not found or considered to be
diminished on the histopathologic examination taken
from the depigmentation patch. While in the
hyperpigmentation area, there is a normal number of
melanocytes found (Spritz,2009) (Thomas,2004)
(Treadwell,2015). Immunohistochemistry staining
with s100 is expressed un neural crest-derived cell
(melanocyte, Schwann cells, glial cells),
chondrocytes, fat cells, macrophages, Langerhans
cells, dendritic cells, some breast epithelial cells and
sweat glands. Another staining used in this case is
Human Melanoma Black 45 which expressed in
melanocyte that are synthesizing melanin. To
revealed melanin pigment in the basal layer that
usuallu not discernible in Hemathoxylin-Eosin-stain
section, requires a Fontana-Masson Stain for
confirmation (High,2012). We performed routine
histopathological examination and immuno-
histochemistry staining with S100, HMB45, and
Fontana-Masson thus proving that no melanocytes
nor melanin pigment in the basal layer.
Piebaldism therapy is still a challenge. Sunscreen
treatment is recommended to prevent burns and to
reduce carcinogenic potential
(Thomas,2004)(Milankov,2014). Facial makeup
application or pigmentation agents might be used to
disguise the area involved, even though it may only
be temporary. Various surgical techniques have been
performed, such as a combination of dermabrasion
and skin grafting with normal pigmentation to the
area of depigmentation, with or without
phototherapy, of which it may be of benefit to some
patients (Oiso,2012) (Thomas,2004)(Maderal,2017).
Case Report: A Case of Full Expressivity Piebaldism
475

In our patient, we planned a skin grafting for
treatment but the patient and family considerate to
not given the therapy regarding the healing
possibility, the extent of the body area involved,
including also the transportation problems.
4 CONCLUSION
A case of piebaldism in a 17-year-old boy with
full/complete phenotype expressivity was reported.
Routine histopathological examination with
hematoxylin-eosin staining cannot distinguish the
depiction of piebaldism, vitiligo, and Waardenburg
syndrome. The diagnosis of piebaldism in this
patients is based on anamnesis and physical
examination in accordance with the severe
phenotype, of which a typical white forelock
appearance was found on the scalp of the frontal
region and broad leukoderma on the chest, abdomen,
both arms, and legs. There are various alternative
therapies in the case of piebaldism, but the patient
rejected any therapy due to considerations of healing
possibility, the extent of the body area involved, and
also the patient's transportation problem.
REFERENCES
Agarwal, S., Ojha, A., 2012. Piebaldism: A Brief report
and review of the literature. Indian Dermatol Online J.
3, 144-147.
High, W.A., Tomasini, C.F., & Argenziano, G.Z. I., 2012.
Basic Principles of Dermatology. In Dermatology 3
rd
ed. London, Elsevier. 0:29-33.
Huang, A., & Glick, S.A., 2016. Piebaldism in history-
“The Zebra People”. JAMA Dermatol. 152:1261.
Maderal, A. D., & Kirsner, R. S., 2017. Use of Epidermal
Grafting for Treatment of Depigmented Skin in
Piebaldism. Dermatologic Surgery, 43(1), 159-160.
Milankov, O., Savić, R., & Radulović, A., 2014.
Piebaldism in a 3-month-old infant: Case
report. Medicinski pregled, 67(3-4), 109-110.
Oiso, N., Fukai, K., Kawada, A., & Suzuki, T., 2012.
Piebaldism. Journal of Dermatoogy, 39, 1-6
Sánchez‐Martín, M., Pérez‐Losada, J., Rodríguez‐García,
A., González‐Sánchez, B., Korf, B. R., Kuster, W., ...
& Sánchez‐García, I., 2003. Deletion of the SLUG
(SNAI2) gene results in human piebaldism. American
Journal of Medical Genetics Part A, 122(2), pp. 125-
132.
Spritz, R. A., 1994. Molecular basis of human
piebaldism. Journal of investigative dermatology, 103,
137-140.
Taïeb,. A, Morice‐Picard, F., Ezzedine, K., 2016. Genetic
disorders of pigmentation. In Rook’s Texbook of
Dermatology 9
th
ed.; London, Wiley Blackwell, 70, 3.
Thomas, I., Kihiczak, G. G., Fox, M. D., Janniger, C. K.,
& Schwartz, R. A., 2004. Piebaldism: an
update. International journal of dermatology, 43(10),
pp. 716-719.
Treadwell, P. A., 2015. Systemic conditions in children
associated with pigmentary changes. Clinics in
dermatology, 33(3), pp. 362-367.
Xu, X. H., Ma, L., Weng, L., & Xing, H., 2016. A novel
mutation of KIT gene results in piebaldism in a
Chinese family. Journal of the European Academy of
Dermatology and Venereology, 30(2), 336-338.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
476
