
A Case Report: The Efficacy of Human Amniotic Membrane
Mesenchymal Stem Cells-Conditioned Medium (hAMMSC-CM) for
Treating Plantar Pedis Trophic Ulcer in Leprosy Patients
Karina Dyahtantri Pratiwi
1
, Trisniartami
1
, Medhi Denisa Alinda
1
, Bagus Haryo Kusumaputra
1
, Linda
Astari
1
, M Yulianto Listiawan
1
, Indropo Agusni
1
, Fedik A Rantam
2,3
, Cita Rosita Sigit Prakoeswa
1
1
Department of Dermatology Venereology, Faculty of Medicine Universitas Airlangga, Dr Soetomo General Hospital,
Surabaya, Indonesia
2
Stem Cell Research and Development Center, Universitas Airlangga, Surabaya, Indonesia
3
Virology and Immunology Laboratory, Department of Microbiology, Faculty of Veterinary Medicine, Universitas
Airlangga, Surabaya, Indonesia
Keywords: amniotic membrane stem cells, plantar ulcer, leprosy
Abstract: Leprosy is an endemic disease in many countries with consequences of neuropathy that may leads to plantar
trophic ulcer. The management of trophic ulcers is difficult due to its recurrent and recalcitrant
characteristics. Placental derived cells are known to release factors with potential immunomodulatory and
trophic activities. In this study we use the human amniotic membrane mesenchymal stem cells-conditioned
medium (hAMMSC-CM) gel to promote the wound healing of trophic ulcer. A-50-years-old female
presented with a trophic ulcer over the sole of her right foot since 3 years ago. The patient gave a history of
decreased sensation over the right foot and was a known case of lepromatous leprosy released from
treatment 2 years back after completing multibacillary multi-drug therapy for 1 years. Cutaneous
examination revealed a single non-healing ulcer over the plantar aspect of the right foot with pale
granulation tissue and seropurulent discharge at the base. Touch and pain sensation were lost over the foot
and up to the lower leg one-third of the leg. The result of microbiology Mycobacterium leprosy examination
was bacterial index (BI) 0 and morphological index (MI) was negative. A diagnosis of plantar pedis trophic
ulcer in a treated case of leprosy was made. The ulcer managed by given topical hAMMSC-CM gel and
covered with transparent film dressings. Application of gel was done every 3 days, and weekly evaluation
included measurement of the size and the depth of the ulcer was done. The patient was treated with
hAMMSC-CM for 8 weeks. The ulcer was significantly resolved, but there was no complete healing.
1 INTRODUCTION
Trophic ulcer that may occur in leprosy patient due
to their nerve impairment is a condition of an ulcer
that lack of nutrition. It is defined as a pressure ulcer
caused by external trauma to a part of the body that
is in poor condition because of disease, vascular
insufficiency or loss of afferent nerve fibres by
Mosby in 2016 (Puri, Venkateshwaran, and Khare,
2012).
Plantar tophic ulcer is a physical disability
that occurs in 10-20% of leprosy patient.
Conventional therapies such as normal saline
dressings and surgical debridement do not show a
satisfactory improvement (Sari, Listiawa, and
Indramaya, 2018).
2 CASE
A 50 years old female presented with an ulcer over
the sole of her right foot since 3 years ago. The
patient gave a history of decreased sensation over
the right foot and was a known case of lepromatous
leprosy released from treatment 2 years back after
completing multibacillary multi-drug therapy for 1
years. She had been treated intermittently with
topical antibiotics in addition to normal saline
dressing for her ulcer, but complete resolution was
never achieved. Cutaneous examination revealed a
single non-healing ulcer measuring 1,8 x 1,8 x 0,4
cm over the plantar aspect of the right foot with pale
granulation tissue and seropurulent discharge at the
base.Touch and pain sensation were lost over the
442
Pratiwi, K., Trisniartami, ., Alinda, M., Kusumaputra, B., Astari, L., Listiawan, M., Agusni, I., Rantam, F. and Prakoeswa, C.
A Case Report: The Efficacy of Human Amniotic Membrane Mesenchymal Stem Cells-Conditioned Medium (hAMMSC-CM) for Treating Plantar Pedis Trophic Ulcer in Leprosy Patients.
DOI: 10.5220/0008159304420445
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 442-445
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

foot and up to the lower leg one-third of the right
leg. Nerve thickening and regional
lymphadenopathy were absent. The routine
laboratory examinations were normal. There’s no
increasing of blood glucose level and no glucose in
urine examination. The result of microbiology
Mycobacterium leprosy examination was bacterial
index (BI) 0 and morphological index (MI) was
negative.
Figure 1: (a). A single non-healing trophic ulcer
measuring 1,8 x 1,8 x 0,4 cm over the plantar aspect of the
right foot with pale granulation tissue and seropurulent
discharge at the base. (b), (c), and (d) the healing process
of the ulcer treated with hAMMSC gel every 3 days for 8
weeks.
Based on the clinical findings, a diagnosis of
plantar pedis ulcer in a treated case of leprosy was
made. The initial treatment for the ulcer was sterile
normal saline debris. After obtaining a clean ulcer,
wound area and wound depth measurements were
performed. Then the ulcer was given framycetin
gauze dressing (FGD) and sterile gauze above the
FGD but there was no clinical improvement after 8
weeks. On the next following week, the ulcers begin
to be given topical hAMMSC-CM gel and covered
with transparent film dressings. Application of gel
was done every 3 days, and weekly evaluation
included measurement of the size and the depth of
the ulcer was done. The patient was treated with
hAMMSC-CM for 8 weeks. The ulcer was
significantly resolved, but there was no complete
healing.
3 DISCUSSION
The global registered prevalence of leprosy by The
World Health Organization (WHO) at the end of
2015 was 0.2 cases per 10.000 people. The number
of new cases reported globally in 2015 was 2,9 new
cases per 100.000 people.
As the latest data
published by WHO in the Weekly Epidemiological
Record defines leprosy as a public health problem
in countries where the prevalence of the disease
exceeds one case per 10.000 inhabitants (Oliviera et
al., 2017). Indonesia was in the third rank of leprosy
endemic country. About 5.284 new cases reported
by East Java health profile in 2015.
Skin ulcers, such as those seen in patients with
leprosy, are a serious public health problem. Infected
chronic ulcers can lead to amputation of the affected
limbs. The well-being and selfesteem of these
individuals may be diminished by pain, loss of the
ability to walk, and loss of independence. The
appearance and unpleasant odour of the lesions may
lead to social isolation. Most lesions in patients with
leprosy are located on the lower limbs. Lower-
extremity ulcers in patients with leprosy patients can
be divided into two categories: leprous ulcers (due to
the disease itself) and neuropathic ulcers (due to
nervous system involvement). Plantar ulcers can
cause a loss of protective sensitivity or lack of
sensation in the plantar region from damage to the
tibial nerve. Other factors increase the risk of
developing plantar ulcers, including paralysis,
volume loss of intrinsic foot muscles, loss of the fat
pad under the metatarsal head, anhidrotic skin,
biomechanical alterations, and/or deformities (e.g.,
foot drop, structural bone alterations) (Walsh,
DeJong, Meyers, and Portaels, 2015; Rohatgi,
Naveen, Salunke, Someshwar, Jerajani, and Joshi,
2016).
An expert in leprosy, Dr. Paul Wilson Brand
(19142003), made major contributions to the
understanding of the pathogenesis of the
neurological complications of leprosy. It was
considered that leprosy patients had nonhealing
tissues and that nothing could be done about them.
Neuropathic ulcers on the sole of feet usually
develop at sites exposed to repetitive high pressures
during activities of daily living like walking or
working (Puri, Venkateshwaran, and Khare, 2012;
Rohatgi, Naveen, Salunke, Someshwar, Jerajani, and
Joshi, 2016).
The excessive pressure causes a hypertrophic
reactive response of the local keratinocytes causing
local hyperkeratosis. Hence at points of abnormal
weight bearing and friction, callus formation may
A Case Report: The Efficacy of Human Amniotic Membrane Mesenchymal Stem Cells-Conditioned Medium (hAMMSC-CM) for Treating
Plantar Pedis Trophic Ulcer in Leprosy Patients
443
occur. This callus finally cracks and breaks leading
to ulceration. Hence, the risk of an ulcer is even
higher when a callus is present. Importance of
shaving callus at the margins of the ulcer and callus
removal has shown reduction in dynamic plantar
pressures in the forefoot by 30% during barefoot
walking (Walsh, DeJong, Meyers, and Portaels,
2015; Rohatgi, Naveen, Salunke, Someshwar,
Jerajani, and Joshi, 2016).
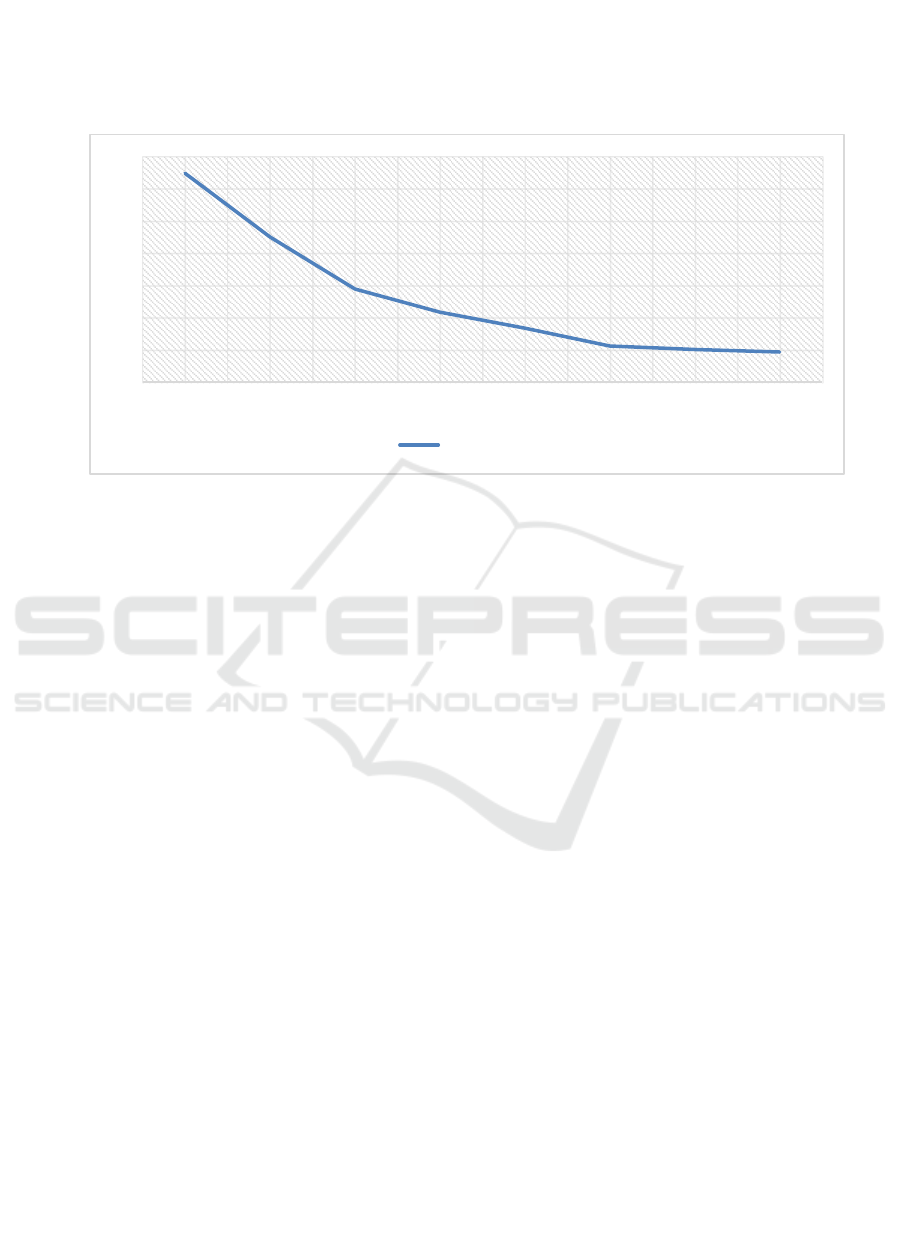
Figure 2: Healing progression. Ulcer treated with hAMMSC-CM not healed completely in 8 weeks.
The slow recovery of natural wound healing has
resulted in the entry of exogenous wound healing
treatments. Many treatments have proved to quicken
the healing. This resulted in the discovery of more
advanced treatments, such as tissue engineering,
gene therapy, platelet-rich plasma, growth factors
(GF) and stem cells (SC) therapy. Among these, SC
has become the centre of attraction in wound healing
by promoting microvascular remodelling. Reports
have shown that SC plays a major role in
strengthening wound healing by secreting a
multitude of trophic and survival signals including
GF, chemokines and cytokines. They serve as a tool
among cells to communicate and these molecules
can be traced in the conditioned medium (CM) or
spent medium harvested from cultured cells
(Jayaraman et al., 2013).
Lee et al. (2011) reported that CM of human
embryonic stem cell (hESC)-derived endothelial
precursor cells (EPC) containing high level of GF
and cytokines such as epidermal growth factor
(EGF), basic fibroblast growth factor (bFGF),
fractalkine, granulocyte-macrophage colony-
stimulating factor (GM-CSF) and interleukin (IL)-6
were successfully used in the treatment of excisional
wound healing in rats (Jayaraman et al., 2013).
In embryonic development, the mesodermal
layer harbors multipotent progenitors that give rise
to bone, cartilage, muscle and other mesenchymal
tissues. Based on this embryonic perspective and
previous reports from our group and others, a
hypothetical and comprehensive scheme, proposed
that in adult bone marrow (BM), a population of
mesenchymal stem cells (MSCs) could likewise give
rise to a spectrum of mesenchymal tissues by
differentiating along separate and distinct lineage
pathways (Caplan and Correa, 2011).
The approach has a high proliferative capacity,
immunomodulatory activity, is low immunogenic,
and non-tumorigenic. In its clinical application,
hAMMSC-CM has a few advantages such as
procurement procedures pose no morbidity, and
there were unlimited amount of stem cells available
due to its shorter expansion and doubling time than
other adult stem cells. Mechanism of stem cells in
tissue healing process is associated with the ability
of stem cells to produce growth factors and
cytokines that are necessary in healing. In vitro
condition, these metabolites are also secreted in stem
cell-conditioned medium (Rennie et al., 2012;
Skardal et al., 2012).
Prakoeswa et al (2018) reported their analytical
experimental approach study comparing the topical
hAMMSC-CM and the framycetin gauze dressing
(FGD) in ulcer healing. Ulcer healing in hAMMSC-
CM group was significantly better with significant
clinical and statistical differences (p < 0,005).
Therefore, stem cell-conditioned medium can be
used as a treatment modality because it contains
growth factors and cytokines that are essential for
cell regeneration (Rennie et al., 2012; Prakoeswa et
al, 2018).
1,296
0,9
0,576
0,432
0,333
0,222
0,2
0,185
0
0,2
0,4
0,6
0,8
1
1,2
1,4
Week1 Week2 Week3 Week4 Week5 Week6 Week7 Week8
hAMMSC‐CM
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
444

4 CONCLUSIONS
It was found clinically that there were improvements
in wound healing treated with hAMMSC-CM gel.
Its may due to the mesenchymal stem cells that
contain many growth factors. The further study to
analyze the macrophage, vascular endothelial
growth factor, fibroblast growth factor 2,
transforming growth factor β1, keratinocyte growth
factor, and epidermal growth factor is needed to
prove the hypothesis.
REFERENCES
Caplan, A.I, Correa, D., 2011. The MSC: an injury
drugstore. Cell Stem Cell, 9(1), 11-15.
Jayaraman, P., Nathan, P., Vasanthan, P., Musa, S., &
Govindasamy, V., 2013. Stem cells conditioned
medium: a new approach to skin wound healing
management. Cell biology international, 37(10), pp.
1122-1128.
Oliveira, M. P., Sousa, J. R., Araujo, R. S., Aarão, T. L.
S., & Quaresma, J. A. S., 2017. Protein profile of
leprosy patients with plantar ulcers from the Eastern
Amazon region. Infectious diseases of poverty, 6(1),
105-112.
Prakoeswa, C. S., Natallya, F. R., Harnindya, D.,
Thohiroh, A., Oktaviyanti, R. N., Pratiwi, K. D., ... &
Alinda, M. D., 2018. The efficacy of topical human
amniotic membrane-mesenchymal stem cell-
conditioned medium (hAMMSC-CM) and a mixture
of topical hAMMSC-CM+ vitamin C and hAMMSC-
CM+ vitamin E on chronic plantar ulcers in leprosy: A
randomized control trial. Journal of Dermatological
Treatment, pp. 1-6.
Puri, V., Venkateshwaran, N., & Khare, N., 2012. Trophic
ulcers-Practical management guidelines. Indian
Journal of Plastic Surgery: Official Publication of the
Association of Plastic Surgeons of India, 45(2), 340-
351.
Rennie, K., Gruslin, A., Hengstschläger, M., Pei, D., Cai,
J., Nikaido, T., & Bani-Yaghoub, M., 2012.
Applications of amniotic membrane and fluid in stem
cell biology and regenerative medicine. Stem cells
international, pp.1-13.
Rohatgi, S., Naveen, S., Salunke, P., Someshwar, S.,
Jerajani, H. R., & Joshi, R., 2016. The story of a
deformed leprous foot. Lepr Rev, 87, pp. 104-108.
Sari, D. K., Listiawan, M. Y., & Indramaya, D. M., 2017.
The Effects of Platelet Rich Plasma Topical Gel on
Chronic Plantar Ulcer Healing in Leprosy
Patient. Periodical of Dermatology and Venereology
28(3), 1-7.
Skardal, A., Mack, D., Kapetanovic, E., Atala, A.,
Jackson, J. D., Yoo, J., & Soker, S., 2012. Bioprinted
amniotic fluid-derived stem cells accelerate healing of
large skin wounds. Stem cells translational
medicine, 1(11), pp. 792-802.
The World Health Organization (WHO). Leprosy
statistics-latest data. Available at:
http://www.who.int/lep/epidemiology/en/
Walsh, D. S., De Jong, B. C., Meyers, W. M., & Portaels,
F., 2015. Leprosy and Buruli ulcer: similarities
suggest combining control and prevention of disability
strategies in countries endemic for both
diseases. Leprosy review, 86(1), pp. 1-5.
A Case Report: The Efficacy of Human Amniotic Membrane Mesenchymal Stem Cells-Conditioned Medium (hAMMSC-CM) for Treating
Plantar Pedis Trophic Ulcer in Leprosy Patients
445
