
Urethritis Chlamydiosis, Proctitis Chlamydiosis, and Anal
Condyloma Acuminata in Versatile
Icha Rachmawati Kusmayadi, Syawalika Ulya Isneny, Pati Aji Achdiat,
Rasmia Rowawi
Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran - Dr. Hasan Sadikin Hospital,
Bandung 40161 Indonesia
Keywords: chlamydiosis, urethritis, proctitis, versatile
Abstract: Versatile is a sexual role as both insertive and receptive in men who have sex with men. Versatiles are prone
to be infected to transmit sexual transmitted infections (STIs). On versatiles, we can found concomitant
STIs such as urethritis and rectal condyloma acuminata. A case of chlamydiosis urethritis, proctitis
chlamydiosis, and condyloma acuminata in 24-year old male was reported to unveil multiple STIs in genital
and anal on versatile. Physical examination showed no urethral discharge but solitary vegetative skin
colored tumor with verrucose surface on perianal. Gram staining from urethral meatus displayed 5-6
PMN/high power field (hpf) and 1-4 PMN/hpf from rectum, polymerase chain reaction (PCR) from urethra
and rectum unveiled positive result for Chlamydia trachomatis, and human papilloma virus (HPV) DNA
genotyping examination revealed type 11 HPV. Varying types genital and anal of STIs could be found on
versatiles, thorough examination should be done. High transmission in versatile can become our concern,
both genital and anal examinations should always be performed simultaneously.
1 INTRODUCTION
The increasing number of sexually transmitted
infections (STIs) has increased since 2004, allegedly
due to the increasing number of men who had sex
with men (MSM) (Mayer, 2011). In MSM, there are
sexual role such as top, bottom and versatile
(Peinado et al., 2014). Based on research in New
York in 2013, it is known that there are 63% of
versatile MSM (Tieu et al., 2013). STIs in MSM
may manifest clinically in the form of urethritis,
proctitis, and anogenital warts (Stam, 2008). The
occurrence of urethritis chlamydiosis, proctitis
chlamydiosis, and anogenital warts simultaneously
in one MSM have not been reported. Nevertheless,
in a study in Stockholm, there were 430 MSM with
17 cases (16%) of whom experienced perianal CA
and chlamydiosis at the same time (Bratt et al.,
2009). In a San Francisco study, it was found that
from 452 MSM, there were 28 (6.2%) cases of
whom had chlamydia urethritis with chlamydia
proctitis compared to those who only had infection
in one site (Kent et al., 2003).
2 CASE
A 24 year-old-male, a college student, unmarried,
came with chieft complaint of skin colored nodule
around the anus that feels itch. Patient is an MSM,
unmarried, coitarche with a boyfriend three years
ago. Risk factors in patients are having a same sex
sexual partner, multiple, sex in anus-genital manner,
as top and bottom, without condom. On
venereological examination, there was not urethral
discharge, but were perianal vegetation, solitary
lesion, irregular shape, size of 4x3x2 cm, clear
border, raised, dry, in the form of a tumor with a
skin colored verrucous surface (Fig. 1A). Anoscopic
examination found erythema rectal wall, no papules,
vesicles, ulcers or erosions, no discharge (Fig. 1B).
Kusmayadi, I., Isneny, S., Achdiat, P. and Rowawi, R.
Urethritis Chlamydiosis, Proctitis Chlamydiosis, and Anal Condyloma Acuminata in Versatile.
DOI: 10.5220/0008159204370441
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 437-441
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
437
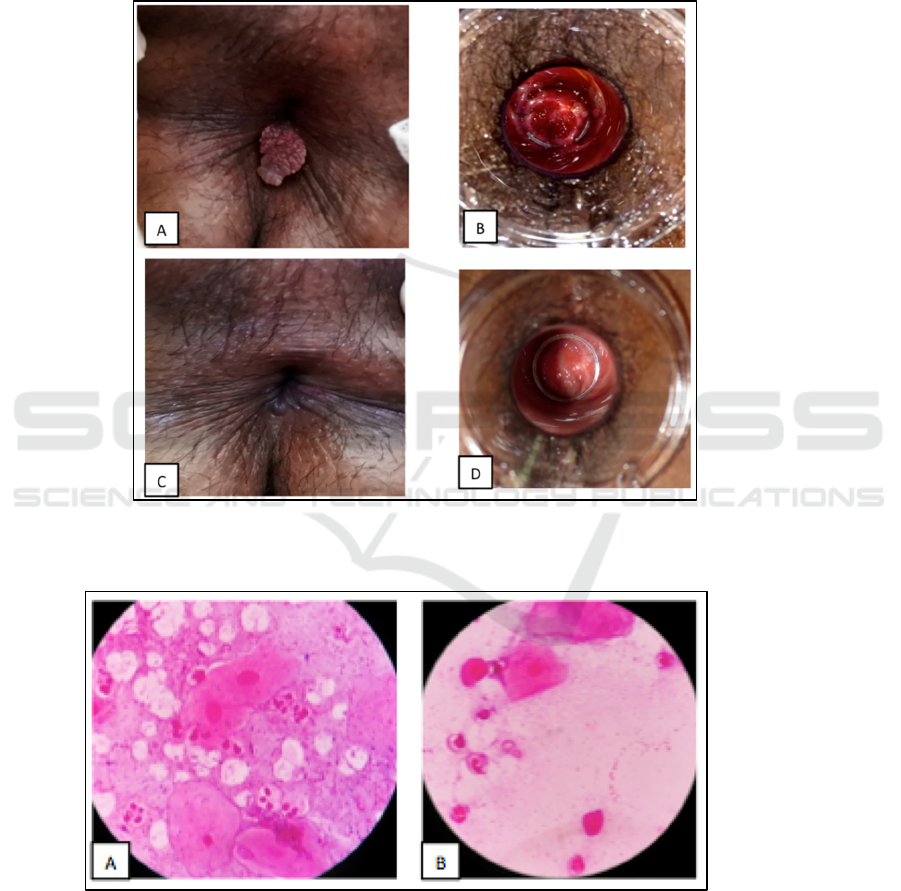
Gram stain smear examination from external
urethral meatus revealed epithelial cells in 1-2 /hpf,
PMN in 5-6 /hpf, no Gram negative bacteria, intra
and extracellular (Fig. 2A). Result of Gram stain
smear examination from rectal discharge found
epithelial cells in 3-4 /hpf, PMN cell in 1-4 /hpf, no
Gram negative bacteria, intra and extracellular (Fig.
2B). PCR on urethral and rectal positive Chlamydial
infection, HIV test negative and DNA genotyping
HPV found HPV type 11. Patients was treated with
1 gram of single doses of azithromycin followed by
doxycycline 100 mg twice daily for seven days
because infection was still present. Condyloma
acuminata therapy performed by electrocautery.
therapy gives effective results, with no infection
found and no relapse of the condyloma acuminata
.
Figure 1. A. Condyloma accuminata on perianal; B. Anoscopic examination found erythema rectal wall; C. Perianal region
2 weeks after electrocautery; D. Anoscopic examination after 2 weeks therapy, there is no erythema rectal wall.
Figure 2. A. Gram stain smear examination from external urethral meatus revealed PMN cell; B. Gram stain smear
examination from rectal discharge found PMN cell.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
438

3 DISCUSSION
Based on a study in San Francisco in 2004, STIs in
MSM are increasing (APCOM, 2008). In an
Indonesian epidemiological study in 2012, it is
estimated that there are about three million MSM in
which 60,000-80,000 of them are in Jakarta
(Anonim, 2017). Based on research in the United
States in 2011 on 21,000 MSM aged 18-24 years, it
was found that 74% of them did orogenital sexual
intercourse, 42% were anal receptive, and 30% were
anal insertive (Bratt et al., 2009). Based on these
studies, it is known that the transmission of STIs in
MSM can be an infection of the mouth, genitals, and
anus. The incidence of urethritis, proctitis, and
anogenital warts in STIs are generally transmitted
through anogenital sexual intercourse, especially on
versatile (Tieu et al., 2013). Versatile is a pattern of
sexual behavior in an MSM that acts as both
insertive and receptive (Peinado et al., 2014). In a
Dominican Republic study in 2013, it was found that
out of 100 MSM, 39 of them were versatile, of
which 22 (56%) of them had STIs, while those who
were not versatile only 19 (31%) out of a total of 61
(Brito et al., 2015). In another study, in New York in
2013, it was found that 48% versatile did not use
condom while doing sex, compared to 31.2% of
insertive sexual partners, and 19.9% had receptive
sexual intercourse without using condom (Tieu et
al., 2013). At a research in Peru in 2007, the
versatile’s occupation observed in the study is
known to be mostly an employee and only 10%
versatile are commercial sex workers (CSWs).
Characteristics of sexual behavior as versatile are
more often found in whom with higher education
(Peinado et al., 2014). The incidence of urethritis
chlamydiosis, proctitis chlamydiosis, and condyloma
acuminata of the anus occurring simultaneously in
one MSM have not been reported. Nevertheless,
based on research in Stockholm there were 430
MSM with 17 cases (16%) with rectal condyloma
acuminata and chlamydiosis occurring
simultaneously (Bratt et al., 2009). In another study,
reported from 452 MSM, there were 28 patients with
chlamydia urethritis and chlamydia proctitis
occurred simultaneously (Kent et al., 2005). Factors
that increase the risk of multiple STIs in this case
report are versatile MSM, 24 years of age, rarely use
of condom, high level of education (undergraduate
student), and history of multiple partner.
The most common causes of urethritis in MSM
are N. gonorrhoeae and C. trachomatis. Clinical
manifestation of urethritis chlamydiosis is generally
asymptomatic in about 90% (Rompalo and Quinn,
2008). Clinical manifestations may be in the form of
urethral discharge with a clear to murky mucus,
frequently in the morning/morning drops, or in the
form of spotting inside the underwear and may
accompanied with dysuria, and nocturia. Diagnosis
of urethritis is done to determine the cause of
urethritis. The easiest examination is by direct
examination. In direct microscopic examination of
urethritis chlamydiosis can be found PMN > 5/hpf.
Adjunct examination for the diagnosis of urethritis
are confirmed by polymerase chain reaction (PCR)
examination against Chlamydial DNA. Sensitivity of
PCR examination to detect urethritis is 96% and the
specificity is ≥ 99% (Takahashi et al., 2008).
Proctitis can be distinguished into ulcerative and
non-ulcerative. Non-ulcerative proctitis in MSM can
be caused by N. gonorrhoeae and C. trachomatis.
Clinical manifestations of chlamydia proctitis are
generally asymptomatic. In one study, it was found
that 91% of proctitis patients did not give any
symptoms. In symptomatic proctitis, common
symptoms found were a frequent need to defecate
(Rompalo and Quinn, 2008). Adjunct examination
on proctitis include anuscopic examination to
evaluate the presence of ulcer, inflammation,
discharge, or bleeding on the anorectal mucosa.
Based on several studies it is known that diagnosis
of proctitis can be established when PMN cells are
obtained ≥1/hpf. Adjunct examination for the
diagnosis of urethritis and proctitis chlamydiosis is
established through the examination of PCR. On
proctitis chlamydiosis PCR, the sensitivity is 92%
while the specificity is 99%. In this patient, no
symptoms of urethritis or proctitis were found. The
result of adjunct examination in this case was PMN
5-6/hpf from urethral smear and 3-4/hpf from rectal
smear, and PCR examination result on both showed
positive Chlamydia (Rompalo and Quinn, 2008;
Takahashi et al., 2008).
According to the National Guidelines for STI
Treatment in 2015, first-line treatment options for
urethritis chlamydiosis are a single dose of one gram
azithromycin per oral or doxycycline 2x100 mg/day
per oral for seven days (Takahashi et al., 2008).
First-line and second-line treatment options in
chlamydia proctitis are similar to chlamydia
urethritis. Follow-up of urethritis and proctitis are
always performed and when infection is present,
treatment may be replaced (Rompalo and Quinn,
2008). Based on a 2008 study in Japan, it is known
that in the treatment of urethritis chlamydiosis, the
cure rate of patients treated with azithromycin was
86% (Takahashi et al., 2008). In a study at
Birmingham in 2004, the cure rate of patients with
Urethritis Chlamydiosis, Proctitis Chlamydiosis, and Anal Condyloma Acuminata in Versatile
439

chlamydia proctitis treated with azithromycin was
97.5% (Habib and Fernando, 2004). Single dose of
one gram Azithromycin was administered to the
patient as an initial therapy, at the time of control on
one week later, PMN are still present as much as >
30 /hpf in the urethra and 2 /hpf in rectal, so that the
patient were given 100 mg doxycycline therapy
twice per day for seven days and gave good results.
Based on England study in 2013 it was found that
doxycycline administration had a failure rate of <
5% compared to azithromycin. Antibiotic resistance
testing of azithromycin was not done because of lack
of facility availability. Patient experiences
improvement on the observation day 16 in the form
of no PMN cells found on the Gram smears
examination in the urethra and rectal.
Anogenital type CA warts in the form of
exophytic lesion, multiple, flat or raised, skin
colored, brown or white. Site of predilection of CA
wart are on the external or internal genitalia,
perianal, anal canal, perineum, mons pubis, and
groin.
Most of CA wart patients do not complain of
skin disorders, although symptoms may include
itching, burning sensation, or bleeding (Lacey et al.,
2013). The diagnosis of anogenital warts can
generally be established based on anamnesis and
physical examination. One of the adjunct
examination for anogenital warts is genotyping
examination of HPV DNA (KalGen
). This
examination aims to determine the type of HPV
(Anonim, 2012). The diagnosis of CA type of
anogenital warts in this patient was confirmed based
on anamnesis and physical examination of a skin-
colored tumor with uneven verrucous surface, itchy,
neither pain nor bleed easily, perianal, supported by
the result of KalGen
examination which shows the
HPV DNA type 11.
The choice of treatment for anogenital warts
should pay attention to various factor such as:
patient’s choice, availability of treatment, and
experience of the health provider. Various treatment
options can be used for the treatment of warts
anogenital, divided into: the treatment applied by the
health provider (provider-administered modalities),
such as cryotherapy, surgery, electrocautery,
trichloroacetic acid (TCA) and CO
2
lasers.
Treatments that can be applied by the patient
(patient-applied modalities), such as podofilotoxins,
sinecatechin, and imiquimod. The choice of
treatment using surgery such as electrosurgery
performed when the planned visit will be in one
time, patient’s choice, and the size of the wart is
large. Based on a study, it is known that the
clearance rate of the electrosurgery use on the
anogenital warts is 95-100% with a recurrence rate
of 22% (Patel et al., 2013). In this patient, the
electrosurgery treatment is choosen based on
patient’s choice who want to quickly removed the
wart.
4 CONCLUSION
Varying types genital and anal of STIs could be
found on versatiles such as urethritis, proctitis,
and/or genital warts, thorough examination should
be done. High transmission in versatile can become
our concern, appropiate treatment shoud provide an
effective result.
REFERENCES
Bratt, G. A., Edlund, M., Cullberg, M., Hejdeman, B.,
Blaxhult, A., & Eriksson, L. E., 2009. Sexually
transmitted infections (STI) in men who have sex with
men (MSM). Open Infectious Diseases Journal, 3, pp.
118-127.
Brito, M. O., Hodge, D., Donastorg, Y., Khosla, S.,
Lerebours, L., & Pope, Z., 2015. Risk behaviours and
prevalence of sexually transmitted infections and HIV
in a group of Dominican gay men, other men who
have sex with men and transgender women. BMJ
open, 5(4), e007747.
Habib, A. R., & Fernando, R. (2004). Efficacy of
azithromycin 1g single dose in the management of
uncomplicated gonorrhoea. International journal of
STD & AIDS, 15(4), pp. 240-242.
Human papilloma virus dan kanker serviks., 2012.
http://www.kalbemed.com/Portals/6/26_189Praktis-
Human%20Papillomavirus%20dan%20kanker%20Ser
viks.pdf. (download May, 10 2017).
Kent, C. K., Chaw, J. K., Wong, W., Liska, S., Gibson, S.,
Hubbard, G., & Klausner, J. D., 2005. Prevalence of
rectal, urethral, and pharyngeal chlamydia and
gonorrhea detected in 2 clinical settings among men
who have sex with men: San Francisco, California,
2003. Clinical Infectious Diseases, 41(1), pp. 67-74.
Lacey, C.J.N., Woodhall, S.C., Wikstrom, A., Ross, J.,
2013 European guideline for the management of
anogenital warts. Journal Euro Acad Dermatology and
Venereoogy, 27, pp. 263-70.
Laki-laki suka (seks) laki-laki dalam epidemi AIDS di
Indonesia. http://aidsindonesia.com/2012/11/laki-laki-
suka-seks-laki-laki-lsl-dalam.html (diunduh tanggal 10
Mei 2017).
Mayer, K. H., 2011. Sexually transmitted diseases in men
who have sex with men. Clinical Infection Disease,
53(S3), S79-83.
MSM in Asia Pacific: critical HIV research for better
decision making., 2008. Asia Pacific Coalition on
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
440

Male Sexual Health (APCOM)..
http://www.msasia.org (diunduh tanggal 10 Mei
2017).
Patel, H., Wagner, M., Singhal, P., & Kothari, S., 2013.
Systematic review of the incidence and prevalence of
genital warts. BMC infectious diseases, 13(1), pp. 39.
Peinado, J., Goodreau, S. M., Goicochea, P., Vergara, J.,
Ojeda, N., Casapia, M., ... & Sanchez, J. R., 2007.
Role versatility among men who have sex with men in
urban Peru. Journal of sex research, 44(3), pp. 233-
239.
Rompalo, A.M., & Quinn, T.C., 2008. Sexually
transmitted intestinal syndromes. Dalam Holmes KK,
Sparling PF, Stamm WE, Piot P, Wasserheit JN,
Corey L, Cohen MS, Watts DH, penyunting. Sexually
transmitted diseases. Edisi ke-4. China: McGraw-Hill
Companies, Inc. hlm. 1277-1302.
Stam, W.E., 2008. Chlamydia trachomatis infection of the
adult. Dalam Holmes KK, Sparling PF, Stamm WE,
Piot P, Wasserheit JN, Corey L, Cohen MS, Watts
DH, penyunting. Sexually transmitted diseases. Edisi
ke-4. China: McGraw-Hill Companies, Inchlm. 575-
580.
Takahashi, S., Matsukawa, M., Kurimura, Y., Takeyama,
K., Kunishima, Y., Iwasawa, A., ... & Hirose, T.,
2008. Clinical efficacy of azithromycin for male
nongonococcal urethritis. Journal of infection and
chemotherapy, 14(6), 409-412.
Van Tieu, H., Li, X., Donnell, D., Vittinghoff, E.,
Buchbinder, S., Parente, Z. G., & Koblin, B., 2013.
Anal sex role segregation and versatility among men
who have sex with men: EXPLORE Study. Journal of
acquired immune deficiency syndromes (1999), 64(1),
pp. 121.
Urethritis Chlamydiosis, Proctitis Chlamydiosis, and Anal Condyloma Acuminata in Versatile
441
