
Serial Excisions of Three Big Tumors on the Upper Right Side of
Nose, Left Nostril, and Right Side of Chin of NF 1 under Tumescent
Surgical Anesthesia in a Woman
Sri Lestari, Fesdia Sari, Nadya Hasriningrum, Elsi Kemala Putri, Yulia Eka Suryani
Dermato-Venereology Department of Dr. M Djamil Hospital/ Medical Faculty of Andalas University, Padang, Indonesia
Keywords: Neurofibromatosis type-I, excision, flaps
Abstract: Background: Neurofibromatosis type-1 (NF1) is autosomal dominant and multi-system disorders. An
incidence 1 in 3000 live births. There are three big tumors on the face that could disturb function organs
around the tumors and she wanted to remove that tumors. Case report: A case of 32-year-old woman with
chief complaint there were brownish patches and bumps that painless and not itchy on the most part of the
body since 20 years ago. At the age of 10 year-old there were appeared multiple skin colour bumps and
growing bigger all over the body. On physical examination there were multiple skin colour tumors on most
of the body, three big tumors on upper right side of nose, left nostril, and right side of chin, caféau-lait spots,
generalized distribution, disseminated. We consulted to Ophtalmologic Departement there were Lish’s
nodules on iris of her eyes, on Neurology Departement no neurologycal focal defisits were found.
Histopathological examination is neurofibroma. We excised three big tumors on the upper right side of nose,
left nostril, and right side of chin with eliptical, subcutaneous tissue pedicle island flap and long inferiorly
melolabial transposition flap designs under tumescent surgical anesthesia and there were good cosmetic
result. Discussion: NF-1 is best cared for within a multidisciplinary approach, which has access to a wide
range of subspecialists. We excised three big tumors on upper right side of nose, left nostril, and right side
of chin every two-weeks to maintanance function of organ with good cosmetic result.
1 INTRODUCTION
Neurofibromatosis (NF) is a term that has been
applied to a variety of related syndromes,
characterized by neuroectodermal tumors arising
within multiple organs and autosomal-dominant
inheritance. At least 8 different clinical phenotypes of
neurofibromatosis have been identified and are linked
to at least two genetic disorders. Neuro-fibromatosis
type I (NF-1) is the most common type of the disease
accounting 90% of the cases, and is characterized by
multiple café-au-lait spots and the occurrence of
neurofibromas along peripheral nerves (Burton et al.,
2012; Dimitrova et al., 2008).
Von Recklinghausen’s
neurofibromatosis (NF-1) is inherited in an
autosomal-dominant and has a prevalence 1 per 3000
and 1 per 5000 live births (Dimitrova et al., 2008).
The diagnosis NF-1 was made according to the
presence of four of the seven diagnostic criteria of the
National Institute of Health Consensus Development
Conference at least two of the following criteria must
be present to make the diagnosis of NF-1 (Burton et
al., 2012; Dimitrova et al., 2008).
Five or more cafe-
au- lait spots larger than 5 mm in diameter in
prepubertal patients; six or more cafe-au-lait spots
larger than 15 mm in diameter in postpubertal
patients, two or more neurofibromas of any type, or
one plexiform neurofibroma, axillary or inguinal
freckling, optic glioma, two or more Lisch’s nodules,
a distinctive osseous lesion (pseudoarthrosis of the
tibia or sphenoid wing dysplasia), a first-degree
relative diagnosed with NF-1 in accordance with the
above criteria (Dimitrova et al., 2008; Moraes et al.,
2013; Ghalayani et al., 2012; Goldberg & Alam,
2004).
There is no medical treatment for NF-1 at this
time. Neurofibroma therapy is not required and
commonly unsuccessful with high rate of recurrences.
Discrete cutaneous neurofibromas may be removed
surgically to improve cosmetic or to prevent local
irritation (e.g., from brushing for lesions in the
hairline or from rubbing against the shoe for those on
the foot). Deeper neurofibromas may require surgical
removal when they push on vital structures, such as a
Lestari, S., Sari, F., Hasriningrum, N., Putri, E. and Suryani, Y.
Serial Excisions of Three Big Tumors on the Upper Right Side of Nose, Left Nostril, and Right Side of Chin of NF 1 under Tumescent Surgical Anesthesia in a Woman.
DOI: 10.5220/0008158604110414
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 411-414
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
411

dorsal root neurofibroma that infiltrates the neural
foramen and compresses the spinal cord.
Complications of surgery include regrowth of the
original tumor and nerve damage (Burton et al., 2012;
Dimitrova et al., 2008).
We reported three big tumors of NF1 on the upper
right side of nose, left nostril, and right side of chin of
32 year-old woman, and she wanted to remove that
tumors because of blocking of the right eye sight,
push the left of nostril and disturb the right side of
lower lip.
2 CASE
A 32 year-old woman, came to out-patient
Department of Dermato-Venereology on November
28
th
2017 with there were skin colour bumps that
painless and not itchy on the most part of the body
since twenty years ago. There were three big skin
colour bumps on the face: on the upper right side of
nose, left nostril, and right side of chin. There was
positive family history, her daughter was 6 years old
complained skin colour bumps on the back. On
physical examination we found multiple skin colour
tumors, the largest amount being on the upper right
side of nose, left nostril, and right side of chin ranging
from 1-4 cm, caféau-lait spots. On Ophtalmology
Departement there were lish nodules on her eyes and
there were no optic glioma. On Neurology
Departement there was no neurologycal focal defisits
were found. We excised three tumors on the upper
right side of nose, left nostril, and right side of chin
with eliptical, subcutaneous tissue pedicle island flap
and long inferiorly melolabial transposition flap
designs under tumescent surgical anesthesia to
maintanance the function of organ around the tumors
with good cosmetic result. Histopatological
examination is neurofibmotasosis.
2.1 Procedural Operation
First time we operated the tumor on the upper right
side of nose with eliptical design. From the area
between eyebrows, we injected local anesthesia
Pehacain® then incised with blade no.15. Using
infiltrator cannula 3 mm diameter, we delivered
surgical tumescent solution anesthesia 35 cc under the
tumor and to subcutaneous tissue around the nose and
the skin became bulging. We waited 20 minutes and
after that we injected with Pehacain® (lidocaine HCl
2% 20 mg and epinephrine 12,5ug) superficially
along the incision lines. Excised the tumor and
anastomosed the wounds in subcutaneus space with
4-0 chromic gut and epidermis with 5-0 Prolene
suture®.
Two weeks later we excised the tumor on the left
nostril with subcutaneous tissue pedicle island flap
design. From the area between eyebrows, we injected
local anesthesia Pehacain® then incised with blade
no.15. Using infiltrator cannula 3 mm diameter, we
delivered surgical tumescent solution anesthesia 40
cc under the tumor and to subcutaneous tissue around
the left nasolabial fold and left cheek and the skin
became bulging. We waited 20 minutes and we
injected local anesthesia Pehacain® superficially
along the incision lines. Excised the tumor and
anastomosed the wounds in subcutaneus space with
4-0 chromic gut and epidermis with 5-0 Prolene
suture®. Two weeks later we excised the tumor on
the right side of chin with long inferiorly melolabial
transposition flap design. From the mid right
mandibula, we injected local anesthesia Pehacain®
then incised with blade no.15. Using infiltrator
cannula 3 mm diameter, we delivered surgical
tumescent solution anesthesia 80 cc under the tumor
and to subcutaneous tissue around the chin and right
cheek, until the skin became bulging. We waited 20
minutes and we injected local anesthesia Pehacain®
superficially along the incision lines. Excised the
tumor and anastomosed the wounds in subcutaneus
space with 4-0 chromic gut and epidermis with 5-0
Prolene suture®. There were good cosmetic result
after surgery and the function of the organs became
normal.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
412
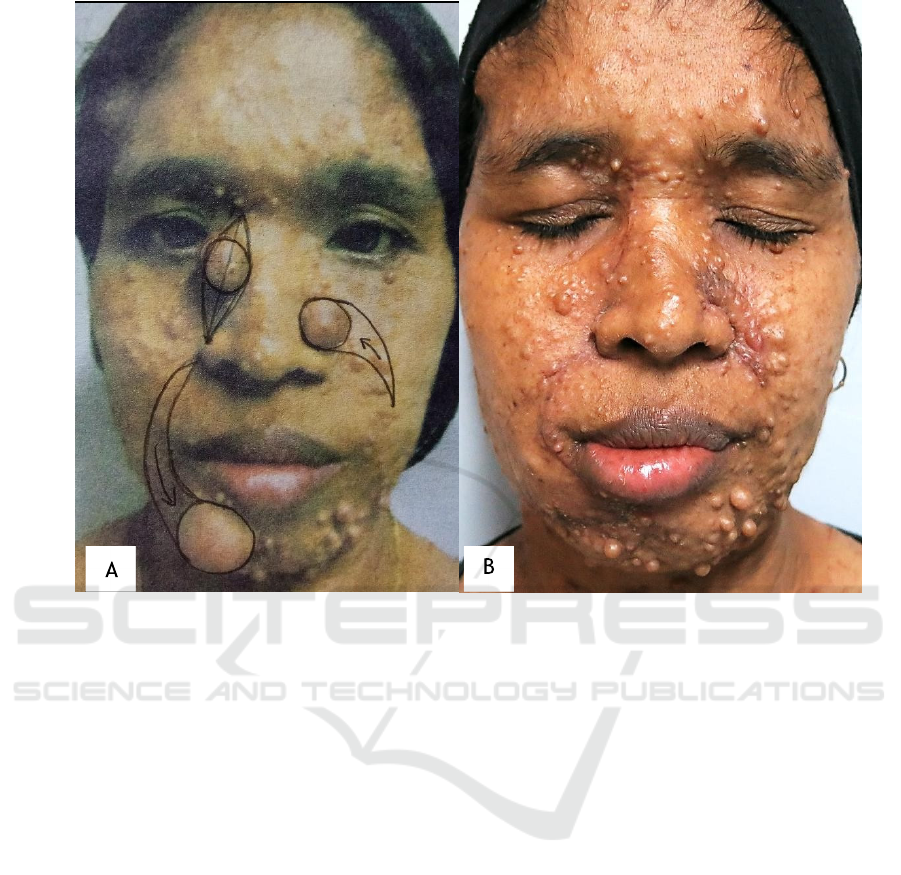
Figure 1. Design operations (A) eliptical on the upper right side of nose, subcutaneous tissue pedicle island fiap on left
nostril, and long inferiorly melolabial transposition flap on right side of chin (B) four weeks after the third operation of the
tumors.
3 DISCUSSION
The patient has done serial exicions of three big
tumors on the upper side of right nose, left nostril and
right side of chin. We excised the tumor on the upper
right side of nose with eliptical design. The elliptical
excision remains an adaptable and essential surgical
strategy. Elliptical excision are easily designed and
can be adapted to many situations. The classic ellipse
is formed by tracing 2 arcs of a circle on the skin. The
arcs, which are symmetrical with respect to the
midline axis separating them, intersect at their ends to
form a convex shape. Commonly used curvature is
variable, but typically leads to a 1:3 to 1:4 width-
length ratio between the short and long axes of the
formed ellipse. Intersection of the arcs an elliptical
angle of 30° has been traditionally assumed at the
ends (Goldberg & Alam, 2012).
The tumor on the left nostril was excised with
subcutaneous tissue pedicle island flap design from
the left cheek to the left side of the nose. The two
most commonly used local flaps for repair of
cutaneous defects of the nose and in which the donor
sites of the flaps are confined to the nose are the
subcutaneous tissue pedicle island advancement flap
and the bilobe flap. The island flap is used for repair
of defects located at the anterior aspect of the alar
groove. The bilobe flap is used to repair small
cutaneous defects of the nasal tip and caudal dorsum.
It is based on subcutaneous tissue and portion of the
transverse nasalis muscle. A triangular shaped flap
with its base making up the cephalic border of the
defect is designed with the apex of the flap positioned
laterally. The posterior border of the flap rests in the
alar groove. The anterior border extends cephalically
and slighly medially from the defect and is designed
to recruit skin of the nasal side wall. The anterior
border then arcs laterally to meet the posterior border
in the alar facial sulcus. The nasal skin is undermined
widely and the proximal and distal one-third of the
flap in undermined in the subcutaneous plane. The
central one-third of the flap remains pedicled on the
subcutaneous tissue. The flap in undermined only to
the degree that there is sufficient mobility to allow the
flap to be advanced into the recipient site. The flap is
advanced and secured at the recipient site first and
Serial Excisions of Three Big Tumors on the Upper Right Side of Nose, Left Nostril, and Right Side of Chin of NF 1 under Tumescent
Surgical Anesthesia in a Woman
413

then the donor site is closed to the repair (Baker,
2007).
The tumor on the right side of chin was excised
with long inferiorly melolabial transposition flap
design. The location and size of defect prevented
repairing the wound with a single unipedicle
advancement flap because of the inelasticity of the
chin skin. A long inferiorly melolabial transposition
flap was selected. The flap was design to recruit skin
from melolabial fold. It was slightly curved in its
linear axis to parallel the melolabial crease. This
facilitated placement of the flap donor site scar
directly with in the melolabial crease. Because the
flap was long relative to the width of the base, the
standing cutaneous deformity that formed on
transposition of the flap was not excised for fear of
compromising the vascularity of the flap (Baker,
2007).
4 CONCLUSION
NF-1 demonstrates a true proliferative process of
neuroectodermal tissue and it is need
multidisciplinary approach. There were no definitive
therapy and surgical therapy only for cosmetic and
maintain the function of organ around the tumors. We
have done operated of three tumors of NF1 of 32 year-
old woman every two weeks on the upper right side
of nose, left nostril, and right side of chin with
eliptical, subcutaneous tissue pedicle island flap and
long inferiorly melolabial transposition flap designs
under tumescent surgical anesthesia to maintain the
function of organs around the tumors with good
cosmetic result.
REFERENCES
Baker, S.R., 2007. Flap classification and design. In: Baker
SR, editor. Baker local flap in facial reconstruction.
Second editon. Philadelphia; Elsevier Inc, pp. 71-107.
Baker, S.R., 2007. Transposition flaps. In: Baker SR, editor.
Baker local flap in facial reconstruction. Second editon.
Philadelphia; Elsevier Inc, pp. 133-157.
Burton, S.C., Burkhart, C.N., Goldsmith, L.A., 2012.
Neurofibromatous. In: Freedberg IM, Eisen AZ, Wolff
AK, Austen KF, Goldsmith LA, Katz SI, editors.
Dermatology in general medicine. 8
th
ed. New York:
Mc.Graw-Hill, pp. 1679-1686.
Dimitrova, V., Yordanova, V., Pavlova, V., Valtchev, V.,
Gospodinov, D., Parashkevova, B., & Balabanov., C.,
2008. A case of neurofibromatosis type 1. Pleven,
Bulgaria. Journal of IMAB - Annual Proceeding
(Scientific Papers), 14, pp. 1-5.
Ghalayani, P., Saberi, Z., & Sardari, F., 2012.
Neurofibromatosis type I (von Recklinghausen's
disease): A family case report and literature
review. Dental research journal, 9(4), pp. 483-488.
Goldberg, L. H., & Alam, M., 2004. Elliptical excisions:
variations and the eccentric parallelogram. Archives of
dermatology, 140(2), pp. 176-180.
Moraes, F. S., Santos, W. E. D. M., & Salomão, G. H.,
2013. Neurofibromatosis type I. Revista Brasileira de
Oftalmologia, 72(2), pp. 128-131.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
414
