
The Unique Characteristic Skin Lesions of Borderline Leprosy
with Severe Reversal Reaction: The Uncommon Case
Eva Lydiawati, Febrina Dewi Pratiwi, Septiana Widyantari, Indropo Agusni
Department of Dermatology and Venereology, Faculty of Medicine, Universitas Airlangga/Dr. Soetomo General Hospital
Surabaya, Indonesia
Keywords: borderline leprosy, reversal reaction, multi drug therapy, leprosy reaction therapy
Abstract: Leprosy is a chronic granulomatous progresssive infectious disease caused by Mycobacterium leprae.
Clinical features of leprosy is dependent upon the equilibrium between bacillary multiplication and the host
cell-mediated immune response. Borderline leprosy is the immunologic intermediate of the granulomatous
spectrum and is the most unstable area. The characteristic skin changes in borderline leprosy are said to be
annular lesions with sharply marginated interior and exterior margins. It could be complicated by potential
intermittent hypersensitivity or leprosy reactions. Reversal reaction is one of leprosy reaction that most
commonly occurs in the borderline cases. We report here a case of the unique characteristic skin lesions of
borderline leprosy with reversal reaction. It was the uncommon manifestation because the lesions are
distributed in all over the body. Because of the reversal reaction, the lesions become more prominent and
have more sharply marginated borders. This case report aims to describe the characteristic of skin lesions
and clinical aspects of reversal reaction in leprosy. A 39-year-old man was diagnosed with borderline
leprosy with reversal reaction who was treated by methylprednisolone for 2 weeks adding up to the multi
drug therapy. There was clinical improvement and no side effect found during this study.
1 INTRODUCTION
Leprosy is one of a deliberately progresssive
infectious disease caused by Mycobacterium leprae.
It was complicated by potential intermittent
hypersensitivity reactions or lepra reactions. It is a
disease which primarily affects the skin and
peripheral nerve, and in highly bacillated state, any
internal organ except central nervous system can be
affected too. The damage to peripheral nerves results
in sensory and motor impairment with characteristic
dreadful abnormalities and debilities (Kumar and
Kar, 2017).
Leprosy reaction are considered as acute or
subacute episode, distinguished by cutaneous and
systemic involvement. Those are caused by changes
in the status of patient’s immune responses (Nery et
al., 2013). This immunologically mediated episodes
can be manifested as acute or subacute inflammation
affecting the skin, nerves, mucous membrane and/or
other sites which interrupt the chronic and placid
course of leprosy. It can results in deformity and
disability unless promptly and sufficiently treated.
Well-timed initiation of treatment for reaction can
reduce morbidity and prevent further deformities
(Kumar and Kar, 2017). So that, this case report
aims to describe the clinical aspects,
immunopathogenesis, and the therapy of reversal
reaction in leprosy.
2 CASE
A 39-year-old Indonesian man was referred to our
hospital in September 2017 with a 3-month history
of thickened red patches on almost all over his body.
It was also accompanied with pain sensation on the
site of lesions. Redness plaques appeared with
whitish fine scales. He was also have a slight
intermittent fever everytime he felt that the plaques
thickened. Firstly, he got red patches on his trunk
and face with thick sensation since about 8 months
befoe admission. He was diagnosed with
multibacillary leprosy for about 6 months in public
heath care and he have gotten the multidrug
treatment for lepromatous leprosy (MDTL) since th
368
Lydiawati, E., Pratiwi, F., Widyantari, S. and Agusni, I.
The Unique Characteristic Skin Lesions of Borderline Leprosy with Severe Reversal Reaction: The Uncommon Case.
DOI: 10.5220/0008157603680372
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 368-372
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
According to the patient, he felt that the macule
became thicker gradually after he took MDTL.
When the rash became thicker, he took some
medication from general practitioner (prednison) but
he forgot about the dose that he took. There were no
history of suffering from such disease before.
History of taking or applying any traditional
medicine before was denied. There were no history
of food or drug allergy. History of contact with other
persons who had leprosy was denied.
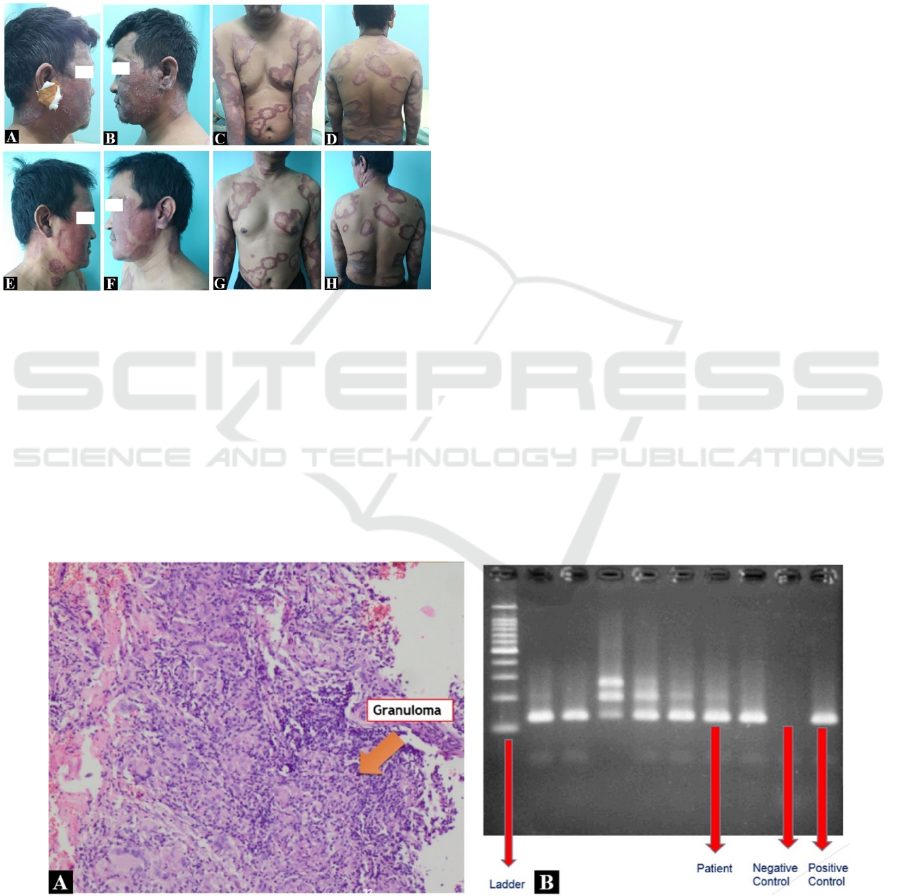
Figure 1: (A-D) The unique characteristic annular skin
lesions of borderline leprosy with severe reversal reaction
before management of leprosy reaction; (E-H) Clinical
improvement of reversal reaction after 2 weeks of oral
methylprednisolone along with MDT treatment. The
redness macules still persist but thinner than before.
Physical examination discovered slight fever and
multiple thick erythematous annular plaques that
sharply marginated, some punched out lesions, some
are covered with white fine scales and hypoaesthetic
(Fig. 1 A-D). No madarosis of the eyebrows or
eyelashes was observed. There were no saddle nose
or diffuse infiltrate on the face, and lagophthalmos.
Thickened peripheral nerves were detected on the
left and right ulnar nerves and accompanied with
tenderness on palpation. In addition, peripheral
neurological symptoms, including motoric, sensory
and autonomic nerve disturbance were not detected
based on a neurological assessment that
includedlight touch, pin – prick test, thermal sensory
test, manual muscle strength test and monofilament
test.
However, acid-fast bacilli were not detected by
the slit – skin smear test of the ear lobes and lesion
(Bacterial Index: 0; Morphological Index: 0).
Histological examination of the ear lobe skin
reveales atrophy and short-flattening of rete ridge on
the upper epidermis, there were some group of
hystiocyyte or foam cell on superficial to deep
dermis (Fig. 2 A-B). No specific microorganisms
were identified by Ziehl – Nielsen and Fite – Faraco
staining. Serologic test by detecting antiphenolic
glycolipid I (anti PGL-1) antibody was positive by
the score of IgM = 1553 (cutt off = 605 u/mL) and
IgG = 927 (cutt off = 630 u/mL). In addition, the M.
leprae deoxyribose – nucleic acid (DNA) was
detected from a skin sample by polymerase chain
reaction (PCR) (Fig. 2 C).
Based on theses findings, from physical and
laboratory examination, the diagnosis of
multibacillary, borderline (BB) leprosy was
established. The patient also had severe reversal
leprosy reaction but fortunately no disabilities was
detected at that time. The patient were observed for
Figure 2: (A) Histologic examination of ear lobe. There were atrophy and short-falttening of the rete ridge of the epidermis.
The group of histiocytes or foam cell on superficial to deep dermis and some bacteria are observed by Fite Farraco staining.
So the conclusion were borderline (BB) leprosy; (B) M. Leprae deoxyribose – nucleic acid (DNA) was detected from a skin
sample by polymerase chain reaction (PCR).
The Unique Characteristic Skin Lesions of Borderline Leprosy with Severe Reversal Reaction: The Uncommon Case
369

the period of time to observe the amendment of his
condition.
Adding up to the multi drug therapy (MDT) that
have been took by him for about 6 months, we added
methylprednisolone (32 mg/day) for a week. The
original regiment dose of MDT were rifampicin (600
mg/month), clofazimine (300 mg/month and 50
mg/day), and dapsone (100 mg/day). After that, we
found some improvement on the skin lesion,
The
redness macules still persist but thinner than before. So
we tappered off the dose of methylprednisolone
every 4-5 days to 4 mg/day. There was clinical
improvement of reaction after 2 weeks of oral
methylprednisolone along with MDT treatment (Fig.
1 E-H).
3 DISCUSSION
Leprosy is a chronic granulomatous infection caused
by M. leprae. Based on the immunological response
of the host to M. leprae, leprosy is classified into 5
major types: TT (tuberculoid), BT (borderline
tuberculoid), BB (borderline), BL (borderline
lepromatous), and LL (lepromatous) according to the
Ridley – Jopling scale (Hattori et al., 2016)
Clinical features of leprosy is dependent upon
the equilibrium between bacillary multiplication and
the host cell-mediated immune response. This can
reflect its pathology. The severity of the disease may
be different from the presence of a not worth
mentioning hypopigmented anesthetic skin patch to
widespread damage to peripheral nerves and sign
and symptoms suggestive of systemic involvement.
Leprosy is exceptional infectious disease for the
width of spectrum of signs and symptoms that it
demonstrates. (Kumar and Kar, 2017).
Borderline leprosy is the immunologic
intermediate of the granulomatous spectrum and is
the most unstable area. It means that the patients can
be quickly up- or downgrade to a more stable
granulomatous bearing with or without a clinical
reaction. Characteristic skin changes are said to be
annular lesions with sharply marginated interior and
exterior margins, large plaques with islands of
clinically normal skin within the plaque, giving a
“Swiss cheese” appearance, or the classic dimorphic
lesion. Because of its instability, the BB lesion is
short lived and such patients are rarely seen (Lee et
al., 2008). The characteristic skin lesions of
borderline leprosy can be seen in our case. It shows
us the unique annular plaque that become generalize
to all over his body. It has sharp borders in both
interior and exterior margins, it is also accompanied
with normal skin within the plaque. From the
clinical manifestation, our case simply show us the
characteristic of the diagnosis of borderline leprosy.
Leprosy reactions are periodic episodes of acute
inflammation caused by immune responses to M.
leprae or its antigen overlaid on the chronic course
of leprosy. These episodes have been classified into
two types: reversal reaction (RR) and erythema
nodosum leprosum (ENL). These are also known as
type 1 and type 2 reactions respectively. RR occurs
in the borderline cases and is a reflection of
immunological instability. It is because of increasing
in the delayed cellular hypersensitivity (DTH) or
type IV hypersensitivity which is reflected by
increase in lymphocyte transformation response
(Kumar and Kar, 2017).
Reversal reactions most commonly occur in
borderline and lepromatous forms of leprosy.
Clinically, patient display abrupt inflammatory
changes of the skin, nerves, or even both. Existing
skin lesions become erythematous and edematous
and may display ulcerative changes. Accompanying
edema is common, whereas systemic symptoms are
unusual (Kamath et al., 2014).
Reversal leprosy reaction result from the
activation of cell immunity, expressed clinically by
exacerbation of skin and pperipheral nerve
inflammation. It leads to sensory and motor
alterations. Inappropriately, the activation of
macrophages with the resulting obliteration of
bacteria that can cause irreversible nerve damage
and aggravating sensory and motor alterations.
There is predominance of the pattern of Th-1 (IL-1β,
TNF, IL-2, IFN-γ) in reversal reaction lesions. It is
more dominant over the pattern of Th-2 (IL-4, IL-5,
and IL-10), which predominates in multibacillary
leprosy (Nery et al., 2013).
The high level of TNF-α, soluble IL-2 receptor
and adhesion molecules indicate the concentration of
local inflammation. Increasing of the expression of
TNF-α mRNA in peripheral nerves and skin of
patients with the borderline form, was observed in
type 1 reactions. It seems that reversal reactions can
be facilitated through Th1 lymphocytes, and cells of
reactional lesions express the pro-inflammatory
cytokines interferon-gamma (IFN-γ), interleukin 12
(IL-12), and oxygen free radicals (Nery et al., 2013).
According to Nery et al. (2013) reversal reaction
episodes occur mainly during the first six months of
polychemotherapy. This reaction can occur at any
time but most frequently appears after starting
multiple drug therapy. This reaction may be resolved
spontaneously first, but worsen gradually. The
patient suffered from the leprosy lesions that became
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
370

4
more thick and pain in palpation. He got tenderness
on ulnar nerve as the symptom of neuritis.
Fortunately, we did not find any deformity yet.
Treatment of reversal reaction intends to supress
the cellular immune response during the reaction.
Early diagnosis and the initiation of the anti-
inflammatory therapeutic are fundamental in order
to avoid possible nerve damage. The identification
of risk factors is advantageous since it leads to a
more attentive monitoring of patients (Nery at al.,
2013). Athough, the exact events that trigger
reversal reaction are unknown. Risk factors for this
reaction include increasing age and the postpartum
period (Kamath et al., 2014). Nery at al. (2013) said
that the risk of reversal reaction was increasing due
to several factors, such as vaccination,
chemotherapy and puerperium. It can be happened
since there are factors such as improvement in cell
immunity among others, and this condition could be
happened right after pregnancy, intercurrent
infections, stress, trauma, and use of contraceptives.
Management of reversal reaction includes giving
antileprosy treatment. Multidrug therapy has to be
started or continued, if already started. This is
important since this is required for continuous
killing the M. leprae to reduce the
bacterial/antigenic load in the skin and nerves
(Kumar and Kar, 2017).
World Health Organization (WHO) recommends
corticosteroid as the drug of choice for reversal
reaction. It is because of its anti-inflammatory
effects (Andrade et al., 2015). The exact mechanism
of corticosteroid in reversal reaction has been
discussed in several studies.
Corticosteroids encourage reduction in vascular
permeability and vasodilatation through inhibition of
mediators, such as metabolites from arachidonic acid
(prostaglandins) and inhibition of the discharge of
platelet-activating factor (PAF), vasoactive amines,
neuropeptides, interleukin-1 (IL-1), tumor ecrosis
factor (TNF), and nitric oxyde. Glucocorticoid also
induce inhibition of the phagocytic capacity and
production of oxygen free radicals (burst cell) and
reduction in the number of eosinophils circulating in
peripheral blood that causes rough granulation in
polymorphonuclear neutrophils. It has a role in
inhibition of tissue migration of monocyte and
lymphocytes, with an increase in endothelial
adhesion of lymphocytes. Not only that, but it also
inhibit the vascular permeability as well as cellular
migration and activation (Nery et al., 2013).
High dose prednisone (1 mg/kg/day) provides
rapid symptomatic relief and helps reverse nerve
function impairment. The regimen must be
personalized individually based on whether nerve
tenderness and motor or sensory deficits are present.
Symptoms should be reconsidered every 2 weeks. If
nerve function improves, the dose can be decreased
by 2.5 to 5 mg; if there is no improvement or
worsening of nerve function, the dose should be
increased. Treatment may last up to 6 months or
even years for those with neuritis (Kamath et al.,
2014).
Initial dose of 40 mg prednisone was adequate to
control most of reversal reaction. The patients with
neural involvement may be need higher doses,
corresponding to 1 mg/kg/day (60 mg) and
sometimes even higher (2 mg/kg/day). The
prednisone dose should be reduced following
evidence of clinical improvement and upon reaching
the dose 20 mg/day. It should be maintained for a
long period of time until there is clinical regression
and complete recovery of neural functions (Nery et
al., 2013).
The standard dose of prednisolone schedule at
referral center uses starting dose 1 mg/kg body
weight/day to be continued until improvement of
skin lesions is visible or nerve tenderness and pain
diminishes. Then the dose should be decreased by 5
mg every 1-2 weeks. The crucial maintenance dose
should be around 15-20 mg for several weeks or
months. In the follow-up period, the dose should be
decreased by 5 mg every 2-4 months. Graded
sensory testing with monofilaments and voluntary
muscle testing can guide the tapering of
prednisolone. The duration should be long enough to
cover the period during which antigen load is able to
induce the CMI response. BT leprosy has to be 4-9
months, BB leprosy in 6-12 months, and BL leprosy
in 6-24 months (Kumar and Kar, 2017).
In acute phase the inflamed nerves must be
maintained in resting position. Appropriate splinting
and padding gives relief. When the acute phase is
over, passive and active exercises should be
initiated. Additional nonsteroidal anti-inflammatory
drugs (NSAIDs) may be required for relieveng pain
(Kumar and Kar, 2017).
In our case, we continued to give the multidrug
therapy (MDT) that have been took by him for about
6 months. We added methylprednisolone (32
mg/day) for a week. The original regiment dose of
MDT were rifampicin (600 mg/month), clofazimine
(300 mg/month and 50 mg/day), and dapsone (100
mg/day). But we did not continue to give
clofazimine treatment to the patient because of its
melanogenic side effect. After that, we found some
improvement on the skin lesion, so we tappered off
the dose of methylprednisolone every 4-5 days to 4
The Unique Characteristic Skin Lesions of Borderline Leprosy with Severe Reversal Reaction: The Uncommon Case
371

mg/day. There was clinical improvement of reaction
after 2 weeks of oral methylprednisolone along with
MDT treatment.
4 CONCLUSION
Leprosy is a chronic granulomatous progresssive
infectious disease caused by Mycobacterium leprae.
Borderline leprosy is the immunologic intermediate
of the granulomatous spectrum and is the most
unstable area. Characteristic skin changes are said to
be annular lesions with sharply marginated interior
and exterior margins, large plaques with islands of
clinically normal skin within the plaque, or the
classic dimorphic lesion. It was complicated by
potential intermittent hypersensitivity reactions or
lepra reactions. Leprosy reaction are considered as
acute or subacute episode, distinguished by
cutaneous and systemic involvement. These
episodes have been classified into two types:
reversal reaction (RR) or type 1 reaction and
erythema nodosum leprosum (ENL) or type 2
reaction. RR occurs in the borderline cases and is a
reflection of immunological instability. Management
of reversal reaction includes giving or continuing
antileprosy treatment, good rest, splinting or
padding, and analgetics. If it is accompanied by
neuritis or severe reaction we can treat the patient
with corticosteroids. If it is left untreated, surgical
decompression of nerve that is inflammed may be
useful for treating reversal reaction.
ACKNOWLEDGEMENT
The authors would like to express their genuine
thanks to the Dermatovenereology Ward and
Outpatient’s Clinic of Dr. Soetomo General Hospital
Surabaya and patient who participated in this study.
REFERENCES
Andrade PR., Pinheiro, RO., Sales, AM., Illarramendi, X.,
Barbosa, MGM., Moraes, MO., Jardim, MR., Nery,
JAC., Sampaio, EP., Sarno, EN., 2015. Tyoe 1
reaction in leprosy: a model for a better understanding
of tissue immunity under an immunopathological
condition. Expert Rev. Clin. Immunol. 11 (3): 391-407.
Hattori, M., Motegi, S., Amano, H., Ishii, N., Ishikawa,
O., 2016. Borderline lepromatous leprosy: cutaneous
manifestation and type 1 reversal reaction. Acta Derm
Venereol. 96: 422-3.
Kamath, S., Vaccaro, SA., Rea, TH., Ochoa, MT., 2014.
Recognizing and managing the immunologic reaction
in leprosy. J Am Acad Dermatol. 34: 1-9.
Kumar, B., Kar, HK., 2017. IAL Textbook of Leprosy, The
health sciences publisher. London, 2
nd
edition.
Lee, DJ., Rea, TH., Modlin, RL. Leprosy in Goldsmith,
LA., Katz, SI., Gilchrest, BA., Paller, AS., Leffell,
DJ., Wolff, K., 2008. Fitzpatrick’s dermatology in
general medicine. Mc Graw Hill. London, 8th edition.
Nery, JAC., Filho, FB., Quintanilha, J., Machado, AM.,
Oliviera, SSC., Sales, AM., 2013. Understanding the
type 1 reacional state for early diagnosis and
treatment: a way to avoid disability in leprosy. An
Bras Dermatol. 88 (5): 787-92.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
372
