
A Retrospective Study: Acne Vulgaris with Oral Antibiotic
Treatment at Dermatovenereology Outpatient Clinic Dr. Soetomo
General Hospital Surabaya
Chesia Christiani Liuwan, Evy Ervianti, Rahmadewi
Department of Dermatology and Venerology, School of Medicine, Universitas Airlangga, Dr. Soetomo General Hospital,
Surabaya, Indonesia
Keywords: Acne Vulgaris, Doxycycline, Oral Antibiotic, Lehmann, Plewig and Kligman
Abstract: Introduction: Acne vulgaris (AV) is a common skin disease, affecting more than 85% of adolescents and
often continuing into adulthood. The pathogenesis of acne involves 4 main processes: follicular
hyperproliferation, excess sebum production, inflammation, and proliferation of Propionibacterium acnes.
Although acne vulgaris is not an infection, the normal resident, Propionibacterium acnes, is the stimulus for
inflammation in acne vulgaris, and a reduction in P. acnes populations is usually accompanied by clinical
improvement. Objective: The aim of this study is to evaluate the use of oral antibiotic treatment in patients
with acne vulgaris at dermatovenereology outpatient clinic dr.Soetomo general hospital. Methods: This is a
retrospective study which analyze the data from medical records. Result: Among 475 patients, 63,37% has
been diagnosed AV moderate or AV Papulopustular grade 3-4. Doxycycline is the first choice oral
antibiotic used to treat Acne Vulgaris, used in 98,53% cases, with the duration between 4-8 weeks in
54,36% cases. There are good improvement, shown as decline severity index in diagnosis (before oral
antibiotic treatment is AV moderate at 65,37% and after treatment is AV mild at 68,90%) , after the patients
get the treatment. Conclusion: Doxycycline is effective as first line oral antibiotic to treat moderate and
severe acne vulgaris in Dr.Soetomo general hospital.
1 INTRODUCTION
Acne vulgaris is a chronic inflammatory dermatosis
notable for open or closed comedones (blackheads
and whiteheads) and inflammatory lesions, including
papules, pustules, or nodules (also known as cysts)
(Collier, et al., 2007). AV is a multifactorial
inflammatory disease affecting the pilosebaceous
follicles of the skin. The current understanding of
AV pathogenesis is continuously evolving. Key
pathogenic factors that play an important role in the
development of AV are follicular hyper
keratinization, microbial colonization with
Propionibacterium acnes, sebum production, and
complex inflammatory mechanisms involving both
innate and acquired immunity. In addition, studies
have suggested that neuroendocrine regulatory
mechanisms, diet, and genetic and nongenetic
factors all may contribute to the multifactorial
process of AV pathogenesis (Zaenglein, et al.,
2016).
AV is a common skin disease, especially in
adolescents and young adults. AV affects
approximately 85% of teenagers, but can occur in
most age groups and can persist into adulthood.
There is no mortality associated with AV, but there
is often significant physical and psychological
morbidity, such as permanent scarring, poor self-
image, depression, and anxiety (Lehman, et al.,
2002).
Antibiotic therapy is a time-honored practice
in AV treatment. Although AV is not an infection,
the normal resident, Propionibacterium acnes, is the
stimulus for inflammation in acne, and a reduction in
P. acnes populations is usually accompanied by
clinical improvement. Many AV patients is
effectively treated with the use of long-term
antibiotic regimens, and the practice is generally
considered to be safe and effective (Webster and
Graber, 2008).
The aim of this study is to evaluate
the use of oral antibiotic treatment in patients with
AV at dermatovenereology outpatient clinic
dr.Soetomo general hospital.
338
Liuwan, C., Ervianti, E. and Rahmadewi, .
A Retrospective Study: Acne Vulgaris with Oral Antibiotic Treatment at Dermatovenereology Outpatient Clinic Dr. Soetomo General Hospital Surabaya.
DOI: 10.5220/0008157003380342
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 338-342
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
2 METHODS
This study is a retrospective study that analyze the
data of AV that we get based on medical record
during January 2013 until December 2015. We only
analyze the new patients who got oral antibiotic as
one of the treatment choice in dermato-venereology
outpatient clinic.
3 RESULTS
There were 2.525 new patients who diagnosed with
AV and got treatment from Dermato-venereology
outpatient clinic in Dr.Soetomo General Hospital,
Surabaya from 2013 until 2015. There were 475
patients (18,81%) given oral antibiotic. Table 1
shown the distribution of the diagnose and therapy.
Of 475 patients, 301 patients (63,37%) has been
diagnosed AV moderate or AV Papulopustular grade
3-4. Doxycycline is the most frequent oral antibiotic
used to treat AV in Dr.Soetomo General Hospital.
From 475 patients with oral antibiotic treatment,
only 283 patients (59,75%) control to dermato-
venereology outpatient clinic. Of 283 patients, 195
patients show a good improvement during the
second visit (data not shown). The duration of the
treatment depends on the amount of visitation
recorded. Most of them, 54,36%, have the treatment
between 4-8 weeks. The detail is shown in Table 2.
Figure 1 shows the comparison diagnose before
and after oral antibiotic treatment. AV moderate was
the most diagnose made before the treatment (185
among 283 patients, 65,37%) while after the
treatment most patients was diagnosed as AV mild
(195 among 283 patients,68,90%).
4 DISSCUSSION
AV is a multifactorial, pleomorphic skin disease of
the pilosebaceous follicles characterized by a
variety of noninflamed (open and closed
comedones) and inflamed (macules, papules,
pustules and nodules) lesions. Microcomedones
(earliest subclinical lesions) are thought to be the
precursor lesions that can then develop into non-
inflamed and ∕ or inflamed lesions. Although a
common disease, the etiology of acne is not yet fully
elucidated and is thought to be a multifactorial
process. Androgens, excessive sebum production,
hyper-proliferation and abnormal differentiation of
the follicular infundibulum, changes in the microbial
flora, as well as inflammation and immunological
Table 1: Diagnose and Therapy of Acne Vulgaris.
Information Amount Percenta
g
e
(
%
)
Dia
g
nose / AV Severit
y
AVMil
d
*
/ Komedonal-Pa
p
ulo
p
ustular
g
rade 1-2
**
68 14,31
AV Moderate
*
/Pa
p
ulo
p
ustular
g
rade 3-4
**
301 63,37
AV Severe
*
53 11,16
AV Kon
g
lobata
**
53 11,16
Total 475 100
Thera
py
Dox
y
c
y
cline 468 98,53
Er
y
throm
y
cin 4 0,84
Clindam
y
cin 2 0,42
Cefixime 1 0,21
Total 475 100
*)
Lehmann Criteria
**)
Plewig and Kligman Criteria
Table 2: Durations of Treatment.
Duration of treatment Amount Precentage (%)
<4 weeks 87 30,74
4-8 weeks 140 49,48
9-12 weeks 6 2,12
13-18 weeks 6 2,12
>18 weeks 7 2,47
Without data 37 13,07
Total 283 100
A Retrospective Study: Acne Vulgaris with Oral Antibiotic Treatment at Dermatovenereology Outpatient Clinic Dr. Soetomo General
Hospital Surabaya
339
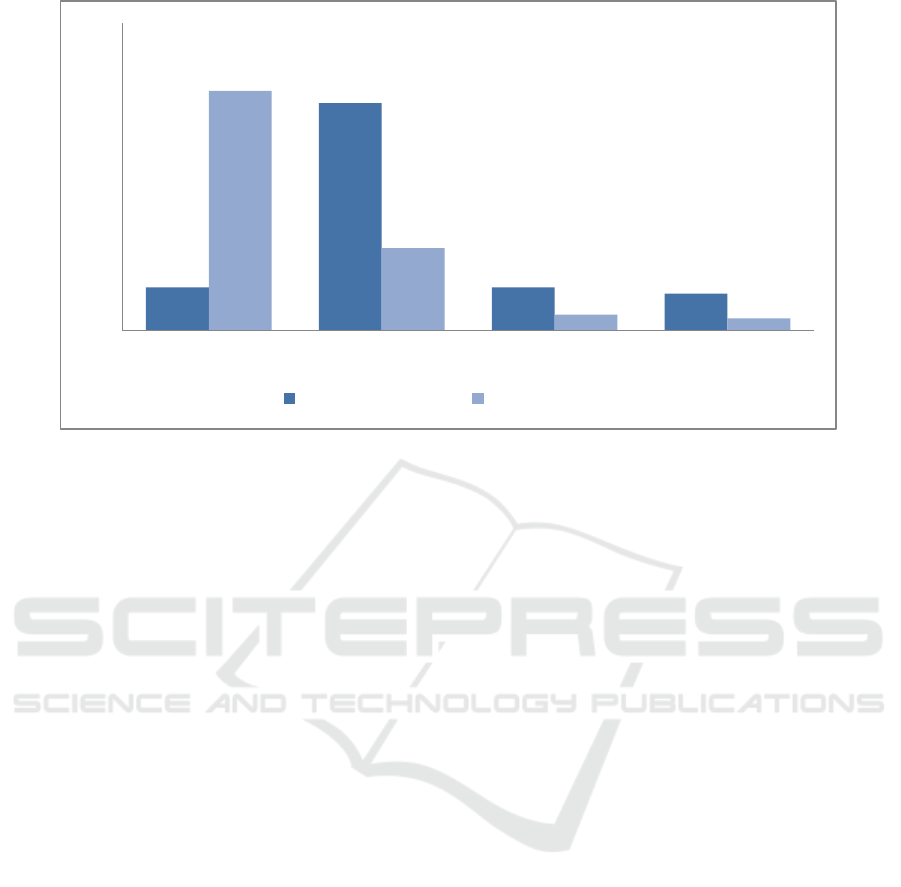
Figure 1. Distribution of AV diagnose before and after treatment.
host reactions are considered the major contributors
to acne pathogenesis (Shaheen and Gonzales, 2012).
Plewig and Kligman divide AV into three
categories, (1) comedonal acne, (2) papulopustular
acne, and (3) acne conglobata. Comedonal acne
mean that the lesions are dominantly open and
closed comedones. Some inflammatory lesions may
be, and frequently are present, but there are never
more than five on one side of the face. The severity
of comedonal acne is measured as grade I: less than
10 comedones on one side, grade II : 10-25
comedones on one side, grade III: 25-50 comedones
on one side, grade IV: above 50 on one side. Papulo-
pustular acne is by far the commonest type in mid
adolescence. Actually, it is a mixture of comedones
and inflammatory lesions which are either pustules
or papules. Assignment to this category is based
solely on the prevalence of inflammatory lesions,
regardless of the number of comedones. Grade I:
less than 10 on one side, grade II: 10-20 on one side,
grade III: 20-30 on one side, grade IV: more than 30
on one side. By definition, acne conglobate is never
mild. The disease is usually appeared with nodul and
cystic form with severe inflammation.
6
Lehmann
also divides AV into three categories, (1) mild, (2)
moderate, and (3) severe. Mild acne character is <20
comedones, or <15 inflammatory lesions, or total
lesion count <30. Moderate acne is 20-100
comedones, or 15-50 inflammatory lesions, or cyst <
5, or total lesion count 30-125. Severe acne >5
cysts, or total comedones count >100, or total
inflammatory count >50, or total lesion count > 25.
Inflammatory lesion in Lehmann categories is papul
and pustul (Lehmann, et al., 2002)
From Table 1, we can see that most of the
patients is diagnosed with AV moderate in Lehmann
categories, equivalent with papulopustular grade 3-4
in Plewig and Kligman categories. Before 2015,
Plewig and Kligman criteria was used to diagnose
acne vulgaris in Dr.Soetomo general hospital. After
Kelompok Studi Dermatologi Kosmetik Indonesia
(KSDKI) set Lehmann criteria as standard criteria to
diagnose acne vulgaris, we used Lehmann criteria at
Dr.Soetomo general hospital. This is the reason there
were some differentiations in acne vulgaris diagnose
at dermato-venereology outpatient’s medical records
during 2013-2015.
Without treatment, acne is generally expected to
spontaneously regress during the late teenaged or
early adulthood years. However, a significant
number of patients experience persistent acne or
develop new-onset adult acne after adolescence
(Collier, et al., 2007). Systemic antibiotics have
been a mainstay of acne treatment for years. They
are indicated for use in moderate to severe
inflammatory acne and should be used in
combination with a topical retinoid and Benzoyl
Peroxide. Evidence supports the efficacy of
tetracycline, doxycycline, minocycline,
erythromycin, and azithromycin to treat AV
(Zaenglein, et al., 2016).
The tetracycline class of antibiotics, including
doxycycline and minocycline as second generation
of tetracycline, should be considered first-line
therapy in moderate to severe acne, except when
contraindicated because of other circumstances (ie,
35
185
35
30
195
67
13
10
0
50
100
150
200
250
AVMild AVModerate AVSevere AVKonglobata
BeforeTreatment AfterTreatment
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
340

pregnancy, below 8 years of age, or allergy). The
antibiotics of the tetracycline class work by
inhibiting protein synthesis by binding the 30S
subunit of the bacterial ribosome. This class also has
notable anti inflammatory effects, including
inhibiting chemotaxis and metalloproteinase activity
(Zaenglein, et al., 2016). Tetracycline, often dosed
at 500 mg twice daily for acne, must be taken on an
empty stomach (1 hour before eating or 2 hours after
eating). Ingestion with food and especially dairy
products can block the absorption of tetracycline in
the gut. Tetracycline can frequently cause
gastrointestinal upset and may very rarely cause
esophagitis and pancreatitis (Webster and Graber,
2008).
Doxycycline, a second-generation member of
the tetracycline family, is often dosed at 100 mg
twice daily to give optimal antibacterial effects.
Unlike tetracycline, doxycycline may be taken with
food. However, doxycycline has more potential to
induce a phototoxic reaction than tetracycline and
extreme care should be used when prescribing
doxycycline in the summer months (Webster and
Graber, 2008). According to Kelompok Studi
Dermatologi Kosmetik Indonesia (KSDKI) and
Panduan Praktik Klinis Perhimpunan Dokter
Spesialis Kulit dan Kelamin Indonesia
(PERDOSKI), doxycycline is a first line oral
antiobiotic to treat AV moderate with the dose 50-
100 mg, 1-2 times daily (Wasitaatmaja, et al., 2016;
Anon, 2017). In Dr.Soetomo dermato-venereology
outpatients clinic, doxycycline was used as oral
antibiotic treatment in 98,53% AV patients.
Another second-generation tetracycline,
minocycline, is also commonly dosed at 100 mg
twice daily for acne, although 1 mg/kg has been
shown to be an effective dosage for the average acne
patient and one with fewer side effects. Like
doxycycline, minocycline can be taken with food.
Unlike the other tetracyclines, the minocycline
chemical structure has a large side chain that
increases its side effect profile. Because of the high
lipophilicity of minocycline, it can cross the blood–
brain barrier and may induce vestibular disturbances,
such as dizziness, vertigo, and ataxia. A blue– gray
discoloration of the skin may be seen with long-term
minocycline use. Rarely, minocycline may induce a
serum sickness-like reaction characterized by
arthralgias, urticaria, fever, and lymphadenopathy.
When this occurs, it typically starts just days to
weeks after beginning minocycline. Other less
common side effects of minocycline include drug
induced lupus-like disease, vasculitis and hepatic
failure (Webster and Graber, 2008).
Erythromycin
and azithromycin have also been used in the
treatment of acne. The mechanism of action for the
macrolide class of antibiotics is to bind the 50S
subunit of the bacterial ribosome. Again, there are
some antiinflammatory properties for these
medications, but the mechanisms are not well
understood. Azithromycin has been primarily
studied in the treatment of acne in open label studies
with different pulse dosing regimens ranging from 3
times a week to 4 days a month, with azithromycin
being an effective treatment in the time span
evaluated usually 2 to 3 months. A recent
randomized controlled trial comparing 3 days per
month of azithromycin to daily doxycycline did
show superiority of doxycycline (Zaenglein, et al.,
2016). Beside the high used of doxycycline in
dermato-venereology outpatients clinic, there were 7
patients (1,47%) using other classes of oral
antibiotics, such as erythromycin, clindamycin, and
cefixime. The consideration of using different class
of oral antibiotic usually depends on the history of
doxycycline allergy, pregnancy and lactation.
Unfortunately, there were not enough documentation
in these 7 patient’s medical record.
The intensity of doxycycline penetration is
excellent in the pilosebacea unit, and it takes 6-7
days to reach the pilosebasea gland. Doxycycline
works long-term with a half-life of 18-22 hours.
Therefore, the duration of oral antibiotic therapy for
AV cases is a minimum of 6-8 weeks, a maximum
of 12-18 weeks. The expected clinical effects take 4-
8 weeks. If an individual does not respond to
antibiotics or stops responding, there is no evidence
that increasing the frequency or dose is helpful. Such
strategies increase selective pressure without
increasing efficacy. Antibiotics should be stopped if
no further improvement is evident. Antibiotics
should not be routinely used for maintenance.
Global Alliance to Improve Outcomes in acne
(2003) recommends that if antibiotics must be used
for longer than 2 months, benzoyl peroxide should
be used for a minimum of 5–7 days between
antibiotic courses to reduce resistant organisms from
the skin (Williams, et al., 2012). The used of
doxycycline in AV management at Dr.Soetomo
general hospital is already appropriate with the
guideline. The dose and duration is correct to treat
AV moderate or worse. From Figure 1, it is
concluded that using doxycycline is giving a good
result in AV patient because there are a significant
decrease in AV severity (before treatment: AV
moderate 65,37% and after treatment AV moderate:
23.68%, AV mild: 68,90%).
The choice of antibiotic should therefore be
based on the patient’s preference, the side-effect
A Retrospective Study: Acne Vulgaris with Oral Antibiotic Treatment at Dermatovenereology Outpatient Clinic Dr. Soetomo General
Hospital Surabaya
341

profile, and cost. Clinicians also should pay attention
to pharmacokinetic factors that influence the
absorption and tissue distribution for individual
antibiotic agents to better inform on rational dosing
considerations of oral antibiotics for the treatment of
acne vulgaris (Leyden and Rosso, 2011). A general
problem with the tetracycline derivate is the
potential for photosensitivity. Doxycycline was
believed to impair the effectiveness of many types of
hormonal contraception due to CYP450 induction.
Recent research has shown no significant loss of
effectiveness in oral contraceptives while using most
tetracycline antibiotics (including doxycycline),
although many physicians still recommend the use
of barrier contraception for people taking the drug to
prevent unwanted pregnancy. Doxycycline is
categorized by the FDA as a class D drug in
pregnancy. As with all tetracycline antibiotics, it is
contraindicated in pregnancy through infancy and
childhood below eight years of age, due to the
potential for disrupting bone and tooth development.
Doxycycline crosses into breast milk. Although the
dose an infant would receive through breastfeeding
would likely be minimal, it is better to not give
doxycycline to breastfeeding mothers (Zaenglein, et
al., 2016). Although the tetracycline can function in
many ways to be beneficial, the physician should be
well versed in the potential side effects of these
drugs. This detail side effect, interaction, and
pregnancy and lactation status were not well
recorded in dermato-venereology outpatients clinic
so that we could not evaluate any further to this
condition.
5 CONCLUSIONS
The used of doxycycline as first line oral antibiotic
at dermato-venereology outpatient clinic,
Dr.Soetomo general hospital is already appropriate
the guideline and effective to treat acne vulgaris.
The suitable dose and duration also play an
important role of the successful treatment. We
recommend to continue using doxycycline as the
first line oral antibiotic treatment for acne vulgaris.
REFERENCES
Collier, C.N., Haerper, J.C., Camtrell, W.C., Wang, W.,
Foster, K.W., Elewski, B.E., 2007. The prevalence of
acne in adults 20 years and older. J Am Acad
Dermatol,58, pp.56-59..
Zaenglein, A.L., Pathy, A.L., Schlosser, B.J., Alikhan, A.,
Baldwin, H.E., Berson, D.S., et al., 2016. Guideline of
care for management of acne vulgaris. Am Acad
Dermatol, pp.1-64.
Lehmann, H.P., Robinson, K.A., Andrews, J.S., Holloway,
V., Goodman, S.N., 2002. Acne therapy. A
methodologic review. J Am Acad Dermatol, 47,
pp.231-240.
Webster, G.F., Graber, E.M., 2008. Antibiotic treatment
for acne vulgaris. Semin Cutan Med Surg,27, pp.183-
187.
Shaheen, B., Gonzalez, M., 2012. Acne sans P. acnes. J
Eur Acad Dermatol Venereol, 27(1), pp.1-10.
Plewig, G., Kligman, A.M., 1975. Acne: Classification of
Acne Vulgaris. Berlin: Spinger-Verlag, pp.162-167.
Wasitaatmadja, S.M., Arimuko, A., Norawati, L.,
Bernadette, I., Legiawati, L., 2016. Kelompok Studi
Dermatologi Kosmetik Indonesia. Pedoman Tata
Laksana Akne di Indonesia. 2
nd
ed. Jakarta: Centra
Communication;. pp.1-16.
Anon, 2017. Akne Vulgaris. Panduan Praktik Klinis bagi
dokter spesialis kulit dan kelamin di Indonesia.
Perhimpunan Dokter Spesialis Kulit dan Kelamin
Indonesia.
Williams, H.C., Dellavalle, R.P., Garner, S., 2012. Acne
Vulgaris. Lancet, 379, pp. 361–72.
Leyden, J., Rosso, J., 2011. Oral antibiotic therapy for
acne vulgaris pharmacokinetic and
pharmacodynamics perspectives. Nevada, 4.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
342
