
Clinico-epidemiological Profile of Cutaneous Tuberculosis in
Dr. M. Djamil Hospital Padang Period of 2015 – 2017
Indah Indria Sari and Tutty Ariani
Dermato-Venereology Department of Dr. M. Djamil Hospital, Padang, Indonesia
Keywords: Cutaneous tuberculosis, epidemiology, clinical profile
Abstract: Cutaneous tuberculosis (CTB) is a relatively rare manifestation with a wide spectrum of clinical profiles
depending on the source of infection and the immune status of the host that is influenced by co morbidity
diseases. The study was conducted to assess the epidemiology and clinical profile of patient with CTB in Dr.
M. Djamil Hospital Padang. A retrospective study had been done by collecting data from the medical records
of patients with diagnosis of CTB at Dr. M. Djamil Hospital Padang between January 2015 and December
2017. A total of 17 cases are included in the final analysis. There were 9 males and 8 females with ratio males
: females was 1.3:1 and generally occurs in young adults (64.7%). All of patients had no family history of
tuberculosis infection. Among these patients, 76.48% was scrofuloderma, 11.76% was lupus vulgaris and
11.76% was tuberculosis verrucosa cutis. Neck was the most common site of involvement. Regional
lymphadenopathy was found in 82.35%. Pulmonary tuberculosis was found in 76.47% patients. There were
3 patients had acquired immune deficiency syndrome (AIDS), 2 patients had diabetes mellitus, 1 patient had
chronic kidney disease and 1 patient had malnutrition. Combination of scrofuloderma and morbus hansen was
noted in one patient. CTB had wide variation with most of cases having co morbidity diseases. More multi-
department studies should be carried out to obtain clinic-epidemiological profile of cutaneous tuberculosis in
Dr. M. Djamil Hospital, Padang, Indonesia.
1 INTRODUCTION
Globally in 2016 there were an estimated 10,4 million
incident cases of TB (range 8.8 million to 12.2
million), equivalent to 140 cases per 100 000
population. The 30 high TB burden countries
accounted for 87% of all estimated incident cases
worldwide. The five countries that stood out as
having the largest number of incident cases in 2016
were India, Indonesia, China, the Philippines and
Pakistan, which together accounted for 56% of the
global total. Of these, China, India and Indonesia
alone accounted for 45% of global cases in 2016.
Nigeria and South Africa each accounted for 4% of
the global total (WHO, 2017).
CTB is relatively
uncommon and not a well-defined disease,
comprising only 1-1.5% of all extra-pulmonary
manifestations (Zyl et al., 2015). The problem is now
further complicated by relentless spread of HIV
which causes AIDS pandemic and the emergence of
multidrug resistant strains (Verma and Mahajan,
2007).
Infection can occur through exogenous routes,
i.e., cutaneous inoculation takes place directly on the
skin (tuberculous chancre, tuberculosis verrucosa
cutis and some cases of lupus vulgaris) or endogenous
ones, with cutaneous involvement occurring
secondarily, through hematogenous route from a
distant tuberculosis focus or by contiguity from an
already established focus (most cases of lupus
vulgaris, scrofuloderma, miliary tuberculosis and
orificial tuberculosis) (Dias et al., 2014).
The development of clinical manifestations in
CTB should be understood as the outcome of
interactions between the environment, the agent and
the host. The factors are infected person’s cellular
immunity state, infection route, bacilli resistance,
virulence factors, individual’s inherent factors (age,
sex, race), factors that lead to immunosuppression
such as malnutrition, alcoholism, silicosis, diabetes
mellitus, gastrectomy, and immunosuppressive
conditions caused by disease or drugs are also
important and environmental factors (Santos et al.,
2014).
This study was conducted to assess the
epidemiology and clinical profile of patient with CTB
Sari, I. and Ariani, T.
Clinico-epidemiological Profile of Cutaneous Tuberculosis in Dr. M. Djamil Hospital Padang Period of 2015 - 2017.
DOI: 10.5220/0008155402670271
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 267-271
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
267

in Dr. M. Djamil Hospital Padang period between
January 2015 and December 2017.
2 METHODS
The present study is retrospective study using medical
records patients with CTB in Dr. M. Djamil Hospital
Padang between January 2015 and December 2017,
which were diagnosed on the basis of clinical
presentation and histopathology finding. These cases
were classified by year. The medical records consist
of age, sex, family history of tuberculosis infection,
duration of disease, distribution of lesions, regional
lymphadenopathy, x-ray chest, co-morbidity disease
and type of cutaneous tuberculosis.
3 RESULT
A total of 17 patients with CTB were identified during
the period, which represents 0.48% of the total 3508
cases of tuberculosis. Of the various patterns of CTB
seen. The most common was scrofuloderma seen in
76.48% patient. Followed by tuberculosis cutis
verrucosa and lupus vulgaris in 11.76% patient. There
were 9 males and 8 females with ratio males : females
was 1.3:1. The age of the patients ranged from 7 to 67
years. The most commonly affected was young adult
with the age group was 18-40 years (64.7%).
Followed by adult, the age group 41-65 years was
23.5%, childhood the age group 2-10 years and
elderly the age group more than 65 years were 5.9%.
The duration of the lesion ranged from 1 month to 24
months with a mean 5.31 months. There were 70.59%
patient had CTB for less than 6 months duration. All
of patient had no family history of pulmonary
tuberculosis.
Neck was the most common site of involvement
seen in 64.71% cases. The others site was face, back,
arm, hand, inguinal and leg. There were 82.35%
patients had lymphadenopathy and the most common
was cervical region. Pulmonary tuberculosis was
found in 13 patients. Beside that, there were 3 patients
had acquired immune deficiency syndrome (AIDS), 2
patients had diabetes mellitus, 1 patient had chronic
kidney injury and 1 patient had malnutrition. Five
patients had more than 1 co-morbidity disease.
Combination of scrofuloderma and morbus hansen
was noted in one patient.
4 DISCUSSION
CTB is relatively uncommon comprising only 1-1.5%
of all extra-pulmonary manifestations.
2
During the
period, a total of 17 patients with CTB were
identified, which represents 0.48% of the total 3508
cases of tuberculosis in Dr. M. Djamil Hospital. There
is an increase in cases of CTB each year during this
period. Compare with study from Nepal by Mathur M
et al in 2014 reported incidence of cutaneous
tuberculosis in Nepal was 0,1% (Mathur and Pandey
et al., 2014). Thus, the incidence of CTB in Dr. M.
Djamil Hospital is still higher than other area.
Of the 17 patients, there were 9 males and 8
females. It means ratio males : females was 1.3:1. The
most commonly affected was young adult with the
age group was 18-40 years (64.7%). Punia RS et al
reported in 2015, 54% of patients were in 2
nd
and 3
rd
decade of life (Punia et al., 2015). Preponderance for
the younger age has also been in the other studies
from India. Males : females ratio was almost equal.
Young adult is productive periods, which allows
frequent contact with tuberculosis-infected patients
thus increasing the risk of transmission. Beside that,
skin trauma due to increased physical activity during
younger age as well as contact with active
tuberculosis cases at an early age may be the
underlying factors for younger age predilection
(Gopinathan et al., 2001).
All of patient had no family
history of tuberculosis infection.
Scrofuloderma was the commonest type of CTB
in this study. Followed by tuberculosis verrucosa
cutis, lupus vulgaris and tuberculosis caseosa cutis.
Similar with cases in Cipto Mangunkusumo hospital
Jakarta at 2010, scrofuloderma was the most common
type of CTB, followed by tuberculosis verrocusa
cutis. Scrofuloderma and tuberculosis verrucosa cutis
commonly found in developing countries, especially
low socioeconomic groups and generally in children
and young adult (Djuanda, 2016).
The duration of the lesion ranged from 1 month to
24 months with a mean 5.31 months. There were
70.59% patient had CTB for less than 6 months
duration. It means that most of patients can be
diagnosed and treated at an early stage. Neck was the
most common site of involvement observed (64.6%)
in comparison to other sites such as arm, back, axilla,
hand and leg, which is similar to other studies
reported. Sharma S et al reported in 2015, neck and
axilla being the most common in scrofuloderma
(Sharma et al., 2015).
Regional lymphadenopathy was seen in 13
patients (82.35%) and cervical lymph nodes were
commonly affected in scrofuloderma. The similar
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
268
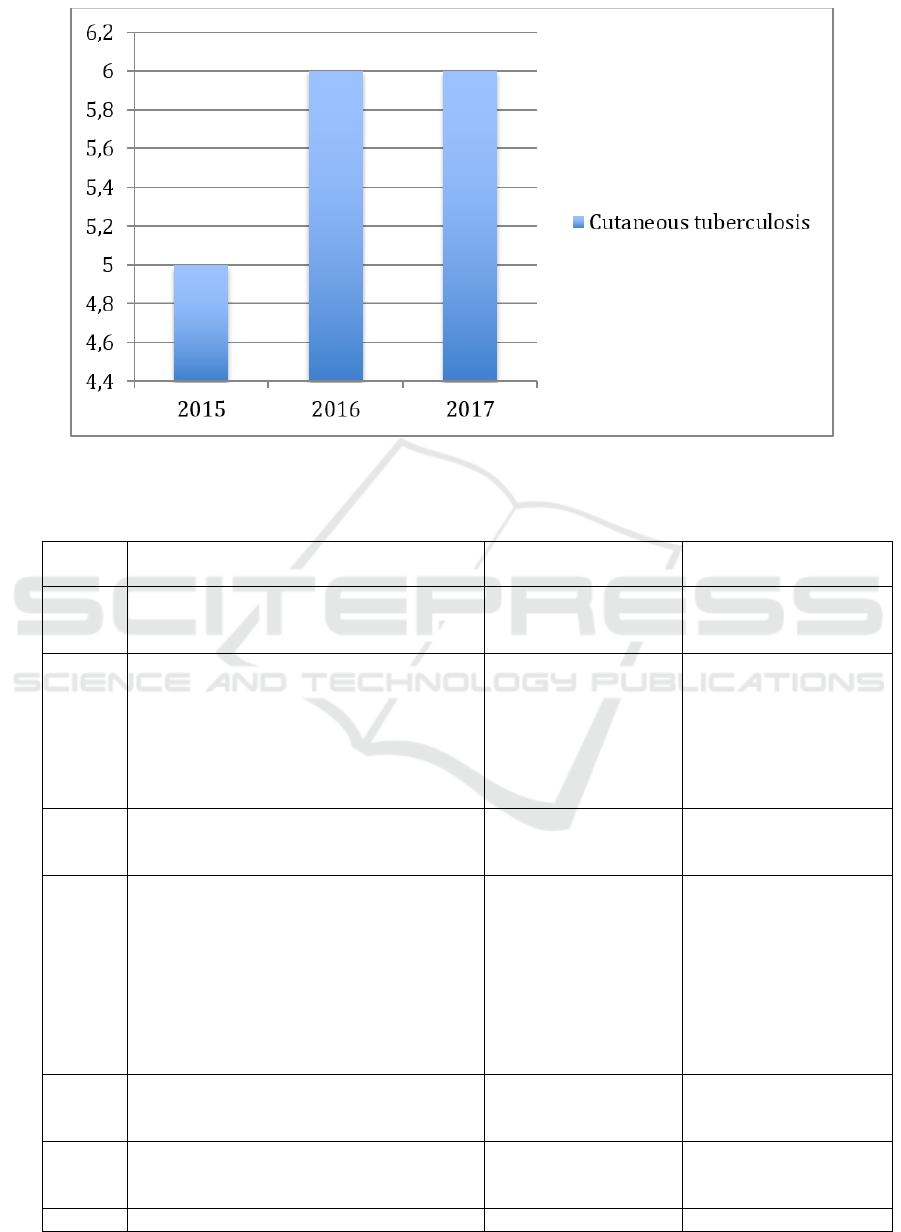
Figure 1. Incidence of cutaneous tuberculosis in Dr. M. Djamil Hospital Padang (2015-2017)
Table 1. Clinico-epidemiological profile of cutaneous tuberculosis at Dr. M. Djamil Hospital Padang period of 2015-2017
No. Epidemiology and Clinical Profile
Case Number
(n=16)
Percentage of Total
Cases (%)
1. Sex
Male
Female
9
8
52.94
47.06
2. Age (year)
Infant : 0 – <2
Childhood : 2 – 10
Adolescence : 11 – 17
Young adult : 18 – 40
Adult : 41 – 65
Elderly : >65
0
1
0
11
4
1
0
5.9
0
64.7
23.5
5.9
3. Duration of disease
< 6 months
≥ 6 months
12
5
70.59
29.41
4. Distribution of lesions
Face
Neck
Axilla
Trunk
Inguinal
Arm
Leg
Other
1
11
1
1
1
1
1
0
5.9
64.6
5.9
5.9
5.9
5.9
5.9
5.9
4. Family history
Yes
No
0
17
0
100
5. Regional lymphadenopaty
Yes
No
14
3
82.35
17.65
6. X-ray chest : Pulmonary tuberculosis
Clinico-epidemiological Profile of Cutaneous Tuberculosis in Dr. M. Djamil Hospital Padang Period of 2015 - 2017
269
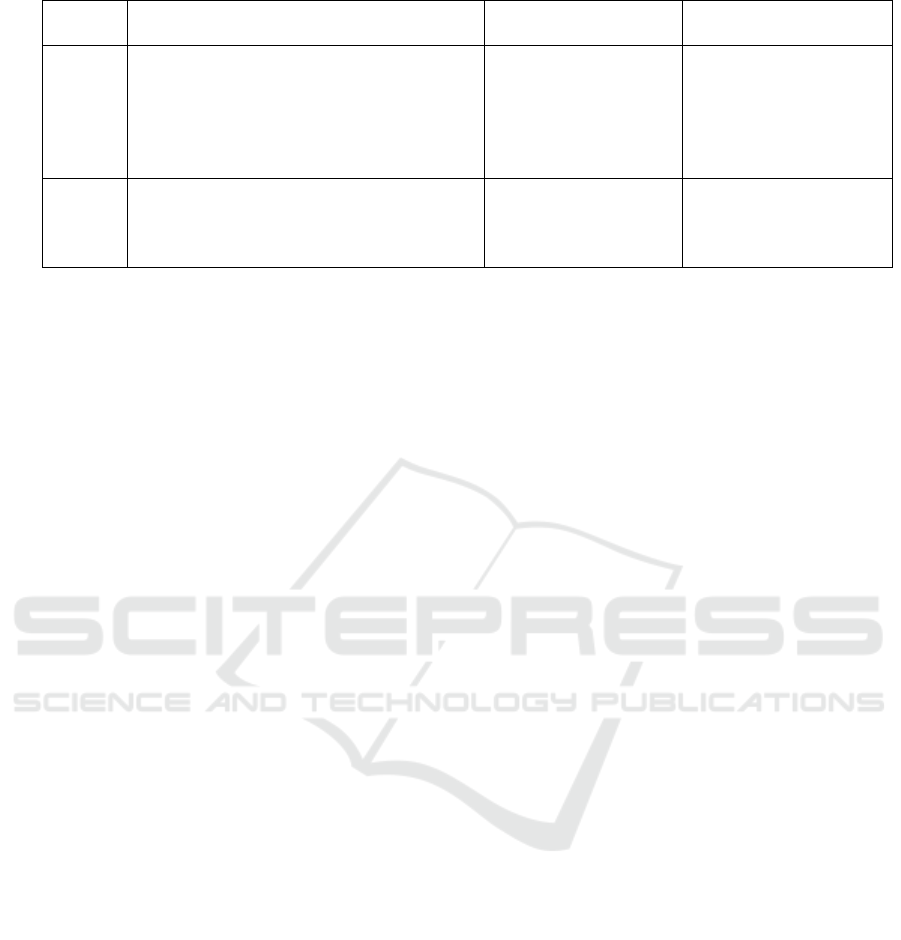
Yes
No
13
4
76,47
23.53
7. Co-morbidity
No co-morbidity
AIDS
Diabetes mellitus
Chronic kidney injury
Malnutrition
4
3
2
1
1
23.53
17.65
11.76
5.9
5.9
8. Clinical diagnosis
Scrofuloderma
Lupus vulgaris
Tuberculosis verrucosa cutis
13
2
2
76.48
11.76
11.76
case had been reported by Shresta SB et al in 2015
(Shrestha et al., 2015).
The pulmonary tuberculosis
was found in 12 patients (75%). Based on theory,
infection of CTB can occur through exogenous
routes, i.e., cutaneous inoculation takes place directly
on the skin (tuberculous chancre, tuberculosis
verrucosa cutis and some cases of lupus vulgaris) or
endogenous ones, with cutaneous involvement
occurring secondarily, through hematogenous route
from a distant tuberculosis focus or by contiguity
from an already established focus (most cases of
lupus vulgaris, scrofuloderma, miliary tuberculosis
and orificial tuberculosis) (Dias et al., 2014; Santos et
al., 2014).
There are many other co-morbidity for CTB such
as HIV infection (AIDS), transplantation,
malnutrition, diabetes, renal failure, liver failure,
cancers, immunosuppressive drugs and
corticosteroids (Shrestha et al., 2015). There were 3
patients had acquired immune deficiency syndrome
(AIDS). In recent years, the epidemiology of
tuberculosis has been adversely affected by the
human immunodeficiency virus (HIV) pandemic. In
fact, HIV infection is now the most important
predisposing factor to the development of active
tuberculosis. Moreover, tuberculosis and HIV
infection pose the two greatest global public health
threats owing to their high morbidity and mortality
rates (Bonamonte et al., 2017). There were 2 patients
had diabetes mellitus, 1 patient had chronic kidney
injury and 1 patient had malnutrition. Four patients
had more than 1 co morbidity disease. All these
condition play an important role in CTB.
Combination of scrofuloderma and morbus
hansen was noted in one patient. Tuberculosis (TB)
and leprosy, the 2 major mycobacterial infections of
humans, are classic granulomatous diseases that still
affect millions of people. Both infections are now
curable, but no highly effective vaccine is yet
available for either of them. Both are ancient scourges
with a wide range of cutaneous manifestations, and
both are infamous for their ability to mimic other
diseases and sometimes fool even the most skilled
diagnostician (Scollard et al., 2015).
5 CONCLUSION
The incidence of CTB in Dr. M. Djamil Hospital
increased during the period and the most commonly
affected was young adult. Scrofuloderma was the
most common type. Majority of patients were
accompanied by pulmonary tuberculosis and others
disease like acquired immune deficiency syndrome
(AIDS), diabetes mellitus, chronic kidney disease and
malnutrition. More multi-centered studies should be
carried out to obtain epidemiological data of
cutaneous tuberculosis in Dr. M. Djamil Hospital,
Padang, Indonesia.
REFERENCES
Bonamonte, D., Filoni, A., Verni, P., Angelini, G., 2017.
Cutaneous tuberculosis. Bari: Springer International
Publishing.
Dias, MFRG., Quaresma, MV., Azulay, DR., Filho, FB.,
Nery, JADC., 2014. Update on cutaneous tuberculosis.
Anais brasileiros de dermatologia, 89, 925-938.
Djuanda, A. 1981. Tuberkulosis kutis. In: Djuanda A,
Hamzah M, Aisah S, editor. Ilmu Penyakit Kulit dan
Kelamin. Jakarta: Fakultas Kedokteran Universitas
Indonesia, 7, 64–72.
Gopinathan, R., Pandit, D., Joshi, J., Jerajani, H., Mathur,
M., 2001. Clinical and morphological variants of
cutaneous tuberculosis and its relation to
Mycobacterium species. Indian Journal Medicine
Microbiology, 19, 193-196.
Mathur, M., Pandey, SN., 2014. Clinicohistological Profile
of Cutaneous Tuberculosis in Central Nepal.
Kathmandu University Medicine Journal, 48(4), 238-
241.
Punia, RS., Aggarwal, P., Kundu, R., Mohan, H., Bhalla,
M., Aggarwal, D., 2015. Cutaneous tuberculosis: a
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
270

clinicopathological study of 50 cases from a tertiary
care referral hospital. Applied Medical Research, 1,
104-108.
S, Verma., V, Mahajan., 2007. HIV-tuberculosis co-
infection. The Internet Journal of Pulmonary Medicine,
10(1), 1-5.
Santos, JB., Oliveira, MH., Figueiredo, AR., Silva, PG.,
Ferraz, CE., Medeiros, VLS., 2014. Cutaneous
tuberculosis: epidemiologic, etiopathogenic and
clinical aspects. Anais brasileiros de dermatologia,
89(2), 219-228.
Scollard, DM., Dasco, MM., Venida, MLA., 2015.
Tuberculosis and leprosy: classical granulomatous
diseases in the twenty-first century. Dermatology
clinics, 33, 541–562.
Sharma, S., Sehgal, VN., Bhattacharya, SN., Mahajan, G.,
Gupta, R, 2015. Clinicopathologic spectrum of
cutaneous tuberculosis: a retrospective analysis of 165
Indians. The American Journal of Dermatopathology,
37(6), 444-450.
Shrestha, SB., Pokhrel, GP., Pradhan, SB., 2015. Clinico-
epidemiological profile of childhood cutaneous
tuberculosis. Nepal Journal of Dermatology,
Venereology & Leprology, 13(1), 45-51.
World Health Organization. 2017. Global tuberculosis
report 2017, 28.
Zyl, LV., Plessis, JD., Viljoen, J., 2015. Cutaneous
tuberculosis overview and current treatment regimens.
Tuberculosis, 95:629-638.
Clinico-epidemiological Profile of Cutaneous Tuberculosis in Dr. M. Djamil Hospital Padang Period of 2015 - 2017
271
