
Common Dermatoses and Predisposing Factors in Food Handlers in a
University Campus: A Cross-sectional Study
Alexis Paula D. Ibañez, Patricia Anne Nicole O. Ramirez, Ma. Angela M. Lavadia
Department of Dermatology, East Avenue Medical Center, Quezon City, Philippines
Keywords: food handlers, occupational skin disease.
Abstract: Behind food industries are the food handlers that thoroughly prepare the meals we consume on a daily basis.
Food and food preparation activities are noted to be a cause of skin conditions. Since dermatoses are often
multifactorial in origin, the various contributing factors to disease can be difficult to determine. The
objectives of this study are to describe the demographic characteristics of food handlers, identify the
common dermatoses seen and possible inherent individual factors, work-related events and external triggers
in the workplace that contribute to the common skin conditions. A prospective cross-sectional study was
done. 160 food handlers participated in this study. All went to the UP Health Service and underwent a
complete dermatologic history and physical examination, and managed accordingly. The most common
diagnoses of food handlers are xerosis, post-inflammatory hyperpigmentation (PIH) secondary to burn,
melasma, chronic hand dermatitis and verruca plana, atopic dermatitis and dermatophytoses. Melasma, solar
lentigenes, dermatosis papulosa nigra and compound nevus were significantly associated to sun exposure.
Exposure to cleaning agents was significantly associated with xerosis, chronic hand dermatitis and acne
vulgaris. Food handlers exposed to heat were significantly associated with PIH secondary to burn. Skin
disease has a large number of factors instrumental in the development and progression of disease. All food
handlers should be encouraged to report all potential work-related dermatoses and seek consult for full
evaluation by a physician. Further research on occupational skin disease is vital towards improving
environmental and occupational research in the Philippines.
1 INTRODUCTION
Food is a basic necessity. With this, the food service
industry is and will always remain in high demand.
Behind the various food industries in our country are
the food handlers that thoroughly prepare and
deliver the meals we consume on a daily basis and
they play a paramount role in ensuring food safety
and prevention of food poisoning. Food handlers in
the University of the Philippines Diliman (UPD) are
present in basically every building in the university.
They can be seen in various food establishments,
restaurants, cafeterias, indoor and outdoor food
stalls, and even on the streets pushing food carts or
carrying baskets of their products. And due to the
number of students they cater to, efforts have been
established to ensure food safety management
procedures. Hence, it is imperative to examine them
for any sign of disease that could predispose to the
spread of infection, as contamination of food may
progress into an outbreak.
A significant proportion of occupational disease
is accounted for by occupational contact dermatitis.
Several studies have stressed the frequency of these
dermatologic conditions in food handlers. However,
the National Institute of Occupational Safety and
Health still emphasized that there has been relatively
scarce occupational studies to establish a clear
connection between the occupational setting and the
cutaneous presentation. This is important as
measures could be done to be able to assist workers
who have developed skin conditions that commonly
afflict them for the rest of their lives. Therefore,
there continues to be a need to further research on
this subject as local studies have not been made.
2 METHODS
A prospective cross-sectional study on the common
skin conditions in food handlers was conducted at
the University of the Philippines Diliman Health
Service (UPHS). 160 food handlers working at the
262
Ibañez, A., Ramirez, P. and Lavadia, M.
Common Dermatoses and Predisposing Factors in Food Handlers in a University Campus: A Cross-sectional Study.
DOI: 10.5220/0008155302620266
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 262-266
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

UPD participated. The participants went to the
UPHS for assessment by a Primary Care Physician
for their annual medical examination. All
participants were directed to the dermatology clinic
for a full cutaneous assessment by dermatologists.
The participants were briefed on the purpose of the
study, assured confidentiality and were asked to sign
an informed consent form if willing to participate in
the study. Those who have agreed to participate and
who have signed an informed consent form were
included and were assigned case numbers. All
subjects underwent a complete dermatologic history
and physical examination by the investigators and
were managed accordingly.
All valid data from evaluable subjects were
included in the analysis. Input and descriptive
analyses of data was performed using Microsoft
Excel. Mann Whitney U test was used to compare
averages. Chi-square test, Fisher’s exact test or
Yates’ chi-square test was used to compare
proportions. Statistical significance was based on p-
values ≤ 0.05. STATA v13 was used in data
processing and analysis.
3 RESULTS
A total of 160 food handlers participated in the
study, with no noted refusals to participate nor
dropouts. 95.6% (153) of the study participants were
assessed to have dermatoses. Of the patients with
dermatoses, majority of them were females (87,
56.9%). Age of study participants ranged from 19-
79 years old, wherein the average age of those with
dermatoses was 38 years. The types of work were
food serving (79.7%), food preparation (68%),
cleaning (64.1%), and cooking (62.7%). It was
found that the food handlers with dermatoses had
longer length of service (p=0.049).
3.1 History of Atopy
A few of the food handlers with dermatoses had a
personal history of asthma (17, 11.1%), allergies
(21, 13.7%), atopic dermatitis (AD) (4, 2.6%), and
allergic rhinitis (AR) (9, 5.9%). Some also had a
family history of asthma (28, 18.3%), allergies (8,
5.2%), AD (2, 1.3%) and AR (7, 4.6%). About
37.3% (57) had a history of previous skin conditions.
However, there was insufficient evidence to show
significant association between personal and family
history of atopy and the presence of dermatoses.
History of present skin condition was significantly
associated with dermatoses (p<0.0001).
3.2 External (Occupational and
Environmental) and Inherent
Factors
About 86.9% (133) food handlers with dermatoses
had contact with food such as vegetables (98,
73.7%), fruits (56, 42.1%), meat (112, 84.2%) and
dairy (28, 21.1%). About 64.7% (99) had contact
with cleaning agents like soap or detergent (98,
99%) and solutions (45, 45.5%). About 79.7% (122)
had contact with pans. Of the 72.5% (111) food
handlers with common dermatoses, 89.2% (99) had
contact with hot containers and 10.8% (12) with cold
containers. Out of those with outdoor food
establishments, food kiosks/stalls comprised of
62.5% (35) while ambulant vendors made up 37.5%
(21). Cafeterias were the majority of the indoor food
establishments at 48.5% (47), followed by food
kiosks/stalls (28, 28.9%) and restaurants (22,
22.7%).
3.3 Common Diagnoses
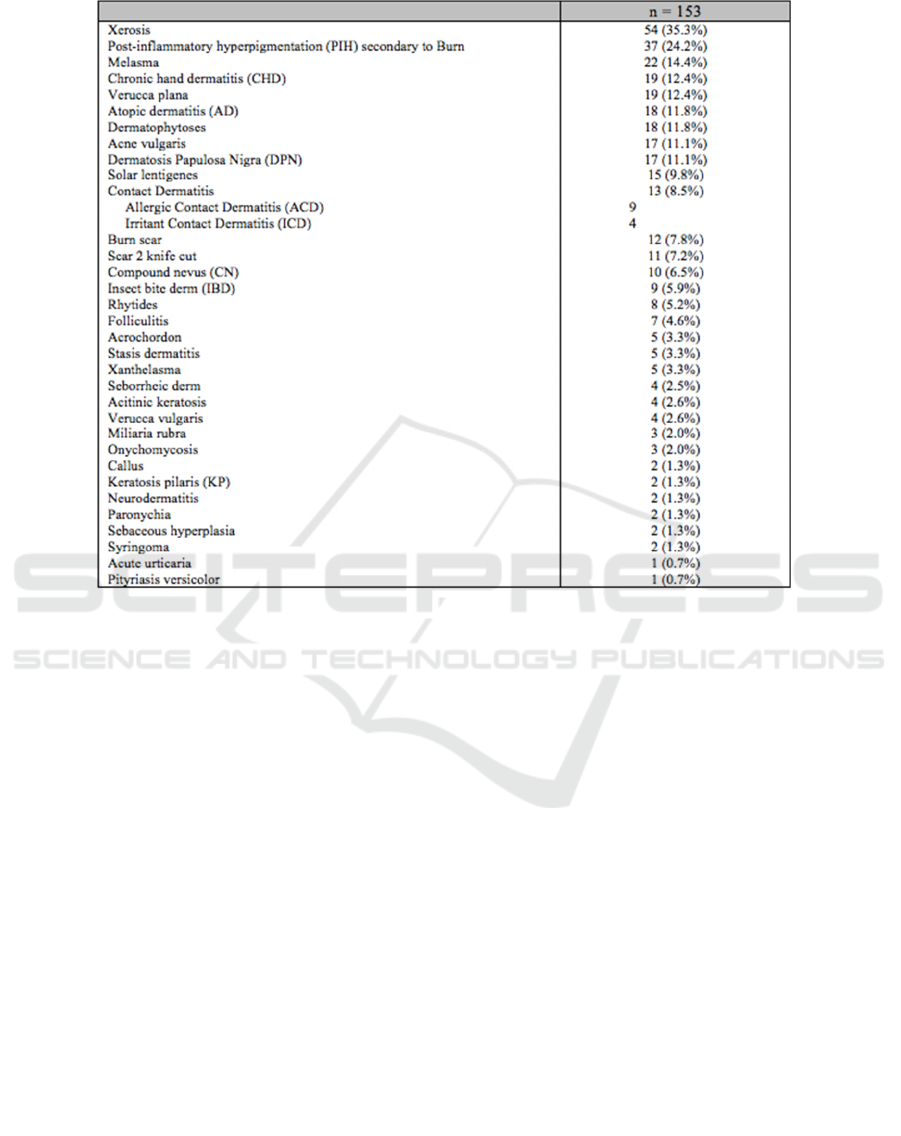
The top 10 most common diagnoses of food handlers
in the study are as follows: xerosis (54, 35.3%),
post-inflammatory hyperpigmentation (PIH)
secondary to burn (37, 24.2%), melasma (22,
14.4%), chronic hand dermatitis (CHD) and verruca
plana (VP) (19, 12.4%), atopic dermatitis (AD) and
dermatophytoses (18, 11.8%), acne vulgaris and
dermatosis papulosa nigra (DPN) (17, 11.1%), solar
lentigenes (15, 9.8%), contact dermatitis (13, 8.5%),
burn scar (12, 7.8%) and scar secondary to knife cut
(11, 7.2%) (Table 1).
Common Dermatoses and Predisposing Factors in Food Handlers in a University Campus: A Cross-sectional Study
263
3.4 Environmental Factors
Exposure to outdoor environmental factors was
significantly associated with the following
diagnoses: 28.6% (16) had melasma (p<0.0001),
23.2% (13) had solar lentigenes (p<0.0001), 25%
(14) had DPN (p<0.0001), and 12.5% (7) had
compound nevus (p=0.038).
3.5 Exposure to Cleaning Agents
Exposure to cleaning agents was significantly
associated with the following diagnoses: 43.4% (43)
xerosis (p=0.005), 17.2% (17) chronic hand
dermatitis (CHD) (p=0.019) and 15.2% (15) acne
vulgaris (p=0.033).
3.6 Exposure to Extreme Temperature
About 28.8% (32) of food handlers exposed to
extreme temperature were diagnosed with post-
inflammatory hyperpigmentation (PIH) secondary to
burn (p=0.034), which was noted to be significant.
4 DISCUSSION
Food handlers are at high-risk for developing
occupational skin disease (OSD) as they habitually
come into contact with a wide range of hazards
potentially responsible for causing skin disease. A
review of several articles discussed the influence of
age, gender, endogenous conditions associated with
atopic constitution, or exogenous triggers such as
environmental factors and specific occupational
risks, on the occurrence of occupational dermatitis
(Iston et al., 2007, Warshat et al., 2007).
4.1 Demographic Data
In our study, most of the participants with
dermatoses were female. This is consistent with a
study by Kibret in 2012, who reported that majority
(73.4%) of the food handlers were females while
(26.6%) were males (Kibret, 2012). Another study
by Warshaw et al also mentioned that women were
found to have a higher prevalence of hand dermatitis
compared to men primarily because females washed
Table 1: Diagnoses of food handlers with dermatosis
n: count; Data presented as n (%). * Significant at 5% level.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
264

their hands more than males (Warshaw et al., 2007;
Williams, 2009; Kibret, 2012). Age of our study
participants ranged from 19-79 years old, wherein
the average age of those with dermatoses was 38
years. According to the The European Agency for
Occupational Safety and Health at Work (EU-
OSHA), workers between 15–44 years old have a
slightly higher risk of being affected by skin diseases
than workers over 45 (Warshaw et al., 2007). It
could be presumed that those among the older age
group have been employed for a longer amount of
time, which is consistent in our study that the food
handlers with dermatoses had significantly longer
length of service.
4.2 History of Atopy
There was insufficient evidence to show a
significant association between a personal and
family history of atopy and the resulting common
dermatoses. Previous studies have showed that a
history of atopy and pre-existing skin disease are
influential factors for the development of the work-
related skin conditions, and that these workers were
also observed to fare worse in severity and are more
likely to have persistent disease than non-atopic
workers (Belsito, 2005; Saary et al., 2005). This
finding was not evident in our study probably
because only a small portion of our participants had
a history of atopy (36 out of 153). However, among
the 36 people noted with atopy, all presented with a
skin condition: 18 (50%) were noted to have AD, 13
(36%) had xerosis, 10 (27.8%) had CHD, 3 (8.3%)
ACD, 2 (5.5%) with ICD and KP were noted.
4.3 Common Dermatoses
The statistics on occupational skin diseases (OSD)
are different for each country because of the
different definitions used to classify occupational
diseases (Lee et al., 2017). Based on literature, those
dermatoses we expect to see in association with food
preparation, cooking, serving and cleaning would be
xerosis, PIH secondary to burn, CHD, contact
dermatitis, burn scar, and scar secondary to knife
cut. These were all significant in our study. For our
setting, we have noted the numerous various food
establishments in the university as well as the
multitude of food handlers seen in practically every
corner. Given that our food handlers are subject to
various environmental factors, such as exposure to
sunlight and humidity, the presence of the other
noted dermatoses in our study may be justified.
4.4 Exposure to Environmental Factors
There is a different impact depending on the
geographic region, being worse in places where the
weather is always warm, and the skin becomes more
exposed (Warshaw et al., 2007). Consequently, the
Philippine weather and environment is very different
from that in Western and first-world countries where
majority of studies were conducted. This could
probably explain the significance of why most of
those diagnosed with melasma, dermatosis papulosa
nigra, solar lentigenes and compound nevus were
noted to have been observed mostly in food handlers
who worked outdoors as these diseases are all
associated with sun exposure.
4.5 Exposure to Cleaning Agents
Another environmental risk factor is “wet work,”
wherein the cumulative effects of water, soaps and
detergents induces maceration of the skin, leading to
increased penetration of irritants and allergens
(Jones & Horn, 2014). This is consistent with the
significant finding that those with xerosis and
chronic hand dermatitis mostly had cleaning as part
of their job. Acne was also found to be significantly
associated to exposure to cleaning agents. We could
probably attribute this to wearing of protective
clothing such as caps and masks, which could trigger
acne mechanica. We also note that the food handlers
with acne are in the 19-30 year old age range, which
we can all deduce that they must have gotten acne
due to more common factors- increase in sebum
production and proliferation of P. acnes.
4.6 Exposure to Extreme Temperature
PIH is characterized by increased pigmentation
acquired after a cutaneous inflammatory process.
People with higher skin phototypes such as
Filipinos, are more prone to this skin condition,
because they already have a higher basal amount of
epidermal melanin (Cestari et al., 2014). Frequent
contact with hot containers such as pans while
cooking predisposes one to burns, with subsequent
post-inflammatory hyperpigmentation after the burn
has healed on the area of contact. With that, we have
found an association between exposure to hot
containers and burn post-inflammatory
hyperpigmentation. There was no association
evident between cold containers (ice cream vendors
mostly) and dermatoses.
Common Dermatoses and Predisposing Factors in Food Handlers in a University Campus: A Cross-sectional Study
265

5 CONCLUSION
It could not be emphasized more that skin disease
has a large number of occupational and non-
occupational predisposing factors that are
instrumental in the development and progression of
disease. Several factors were identified throughout
the course of the study that may differentiate our
study population from those in foreign studies, thus
affecting the results of the study. In summation, it
was found that food handlers with dermatoses had
significantly longer length in service. Our study also
shows that the common dermatoses found in the
food handlers in UP Diliman are more dependent on
occupational and environmental factors and not so
much on inherent factors or atopy. The location of
the food establishment, as well as their type of work
proved to be major contributing factors to the skin
conditions noted. Food handlers who worked
outdoors and had considerable sun exposure were
significantly associated with solar-induced
dermatoses such as melasma, dermatosis papulosa
nigra, solar lentigenes and compound nevus. Those
that had daily exposure to cleaning agents were
mostly found with xerosis, chronic hand dermatitis
and acne vulgaris. Lastly, food handlers who are in
constant contact with hot containers had a significant
association with post-inflammatory
hyperpigmentation secondary to burn. Studies on the
prognosis of occupational dermatoses point out that
primary prevention is very important. Hence, further
research on OSDs is indeed vital towards improving
environmental and occupational research in the
Philippines.
ACKNOWLEDGEMENTS
Ethel M. Estanislao, MoS – statistician for this
study; Ma. Angela M. Lavadia, MD, FPDS –
research adviser; Alexis Paula D. Ibanez, MD – co-
investigator; Deejay B. Arcega, MD, FPDS –
research coordinator; Ma. Cecilia Onjoco, MD,
FPDS – research coordinator.
REFERENCES
Belsito, D. V., 2005. Occupational contact dermatitis:
Etiology, prevalence, and resultant
impairment/disability. J. Am. Acad. Dermatol.
https://doi.org/10.1016/j.jaad.2005.02.045
Cestari, T.F., Dantas, L.P., Boza, J.C., 2014. Acquired
hyperpigmentations. An. Bras. Dermatol. 89, 11–25.
https://doi.org/10.1590/abd1806-4841.20142353
Elston, D.M., Ahmed, D.D.F., Watsky, K.L., &
Schwarzenberger, K. 2002. Hand dermatitis. Journal
of American Academy of Dermatology, 47(2), 291-
299.
Jones, R., Horn, H.M., 2014. Identifying the causes of
contact dermatitis. Practitioner 258, 27–31.
Kibret, M., Abera, B., 2012. The sanitary conditions of
food service establishments and food safety
knowledge and practices of food handlers in bahir dar
town. Ethiop. J. Health Sci. 22, 27–35.
Lee, H.K., Abdul Halim, H., Thong, K.L., Chai, L.C.,
2017. Assessment of food safety knowledge, attitude,
self-reported practices, and microbiological hand
hygiene of food handlers. Int. J. Environ. Res. Public
Health 14. https://doi.org/10.3390/ijerph14010055
Saary, J., Qureshi, R., Palda, V., DeKoven, J., Pratt, M.,
Skotnicki-Grant, S., Holness, L., 2005. A systematic
review of contact dermatitis treatment and prevention.
J. Am. Acad. Dermatol.
https://doi.org/10.1016/j.jaad.2005.04.075
Warshaw, E.M., Ahmed, R.L., Belsito, D. V., DeLeo,
V.A., Fowler, J.F., Maibach, H.I., Marks, J.G., Toby
Mathias, C.G., Pratt, M.D., Rietschel, R.L., Sasseville,
D., Storrs, F.J., Taylor, J.S., Zug, K.A., 2007. Contact
dermatitis of the hands: Cross-sectional analyses of
North American Contact Dermatitis Group Data,
1994-2004. J. Am. Acad. Dermatol. 57, 301–314.
https://doi.org/10.1016/j.jaad.2007.04.016
Williams, J. 2009. Final Report to the British Occupational
Health and Research Foundation. 1-50.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
266
