
Correlation between Density of House Dust Mites and Relapse Rate
of Atopic Dermatitis: A Cross Sectional Study
Gardenia Akhyar
1*
1
Department of Dermatology-Venereology, Head of Allergo-Immunology Division, Dr. M. Djamil Hospital, Medical
Faculty of Andalas University, Padang, West Sumatera, Indonesia
Keywords: house dust mites, atopic dermatitis, skin prick test
Abstract: Background: Inhaled allergens especially house dust mites (HDM) greatly contribute to the occurrence of
atopic dermatitis (AD). It is supported by research conducted by Collof (1992) that measured the density of
HDM on mattresses of AD and mattresses of non atopic healthy people and the result of HDM density on
mattresses of patients with AD is higher than non atopic healthy controls. Teplitsky et al (Jerussalem, 2008)
reported that patients with AD showed a higher prevalence of mites on their skin than did healthy individuals,
which could be involved in allergic sensitization and disease exacerbation. The present study aims to
investigate the correlation between density of HDM and relapse rate of AD, confirmed with skin prick test
(SPT) of HDM. Methods: In present study 30 participants were included. Dust from each bedroom was
collected. The density of HDM was calculated while the participants were checked their sensitivity of HDM
by SPT. Establishing the diagnosis of AD based on Hanifin-Radjka criteria. Each participant was asked about
recurrence of AD in the last three months. Results: Seven (23.3%) samples had moderate density of HDM
while 23 (76.7%) had low density of HDM. From anamnesis, 10 (33.3%) participants were diagnosed with
AD and SPT showed that 50% samples were sensitive against HDM. Out of 10 AD participants, 8 (80%)
were positive with HDM allergens. All 10 participants with AD had relapse within three months. Conclusion:
Out of 10 participants with atopic dermatitis, two (20%) had moderate density of HDM in bedroom (p>0.05).
Also, from seven samples with moderate density of HDM, three (20%) were sensitive against HDM (p>0.05).
About 80% of AD showed sensitivity against HDM while all 10 AD participants had relapse within last three
months indicated that HDM allergen could induce exacerbation of disease in AD, but the correlation between
HDM density and the relapse rate could not be proven yet. This present study suggests further investigation
with larger samples size.
1 INTRODUCTION
Atopic dermatitis (AD) is a chronically relapsing skin
disease that occurs most commonly during early
infancy and childhood (Leung et al., 2012). This
disease usually begins in the early life and is often
seen in the people with the personal or family
background of asthma or swelling of the mucous
membranes. Forty five percent of children experience
the early onset in the first 6 months of their life, 60%
during their first year and 85% before the age of 5.
This disease can assist with asthma and allergic
rhinitis. This disease can cause sleep, educational,
and social disorders in patients (Leung e tal., 2012;
Norris et al., 1998).
AD is a highly pruritic inflammatory skin disease
that results from complex interactions between
genetic susceptibility genes resulting in a defective
skin barrier, defects in the innate immune system, and
heightened immunologic responses to allergens and
microbial antigens (Leung et al., 2012). Sensitization
to inhalant allergens such as house dust mite (HDM)
allergens, detectable with specific IgE tests, is very
common in adolescent and adult patients suffering
from AD (Werfel et al., 2006; Gavino et al., 2008). A
T-cell-mediated reaction is critical in the worsening
of eczema, which can be triggered by the
epicutaneous application of HDM allergens in
sensitized patients. HDM allergens penetrate the skin
where they are trapped via specific IgE on high-
affinity Fc-receptors on Langerhans cells.
Langerhans cells may subsequently present the
allergens to T lymphocytes, leading to specific T-cell
proliferation and eczema (Werfel et al., 2006; Gavino
et al., 2008; Leung et al., 2012).
To cause transdermal sensitization, HDM
Akhyar, G.
Correlation between Density of House Dust Mites and Relapse Rate of Atopic Dermatitis: A Cross Sectional Study.
DOI: 10.5220/0008155102530256
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 253-256
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
253

allergens must be absorbed through the skin,
processed by dendritic cells, and presented to T-
helper lymphocytes. For efficient absorption, close
and prolonged contact between the skin and HDM
allergens is probably necessary, for example, via
HDM-contaminated clothes and bedding (Plattsmills
& Chapman, 1993). Accordingly, several studies
have reported that the homes of patients with AD
contain large amounts of HDM and their antigens,
compared with controls, and that clothes and bedding
are an important source of HDM (Teplitsky, 2008).
The aim of the present study was to determine the
number of HDM and to correlate its density with
incidence of atopic dermatitis, also comparing with
skin sensitivity towards HDM by conducting skin
prick test (SPT).
2 METHODS
The study samples were 30 children and
adolescent of Al Falah and Aisyiyah
Reformatory in
Padang, with aged range 8 to 23
year old. Ethical approval was obtained and all
participants were explained about the purpose of the
study and also were informed about the procedure of
SPT and the informed consent was obtained from
each of the participant. The following data were
collected: demographic data for age, sex, personal
and family history of atopy. Diagnosis of atopic
dermatitis was established based on Hanifin-Radjka
criteria.
2.1 Dust Collecting and Counting
Dust was sucked with a vacuum cleaner. At the end
of the vacuum cleaner was installed a chiffon cloth to
catch the inhaled dust. Suction was done for 3 minutes
on each mattress in the reformatory. Dust inserted to
plastic containers. The container was labeled
according to where the dust was taken. The dust
samples were then taken to the Parasitology
Laboratory of the Faculty of Medicine, Andalas
University for examination.
Dust in a plastic container that had been labeled
was filtered using a sieve. Strained dust was put in a
petri dish that has been previously weighed to
determine the weight of an empty petri dish. Dust was
weighted and noted each weight. Weighted dust was
put into a container containing 100 ml of 5% sodium
chloride solution. The solution was put into a reaction
tube. This solution was centrifuged for 4 min at 600
rpm for separating mites from debris. A saturated
NaCl solution is added to the reaction tube until it was
full and the surface of the convex solution appears.
Then covered with cover glass (deck glass) and left
for 30 minutes. Cover glass was taken and placed on
the object glass. Samples were examined using a 40x
light magnification microscope. The number of HDM
found was calculated.
2.2 Skin Prick Testing
The medial aspect of the forearms and the upper arms
were cleaned and test sites for placing the allergens
were marked using a marker 2-3 cm away from the
wrist and ante cubital fossae. Distance between two
allergens was kept at 2 cm to avoid false positives
either due to direct contamination or due to axon
reflex. A drop of each allergen was placed on the skin
and was pricked with a lancet to introduce the
allergen. Equal pressure was applied for all the
allergens. Histamine dichloride (10 ng/ml or 0.1%)
was used as a positive control and saline as negative
control. Results were read after 20 minutes. Wheals
at the test site were compared with the wheal
produced at the positive control site. Largest diameter
of the wheal was measured using a plastic scale
provided along with the test kit. A wheal of 50% of
diameter positive control or bigger was considered as
positive. Negative control was used to rule out any
dermographism.
2.3 Statistical Analysis
Data obtained was analyzed using SPSS vr.15.0.
3 RESULTS
We conducted 30 participants which 1o of them have
met the Hanifin-Radjka criteria. Seven dust samples
had moderate density of HDM and other 23 samples
with low density of HDM. From seven samples of
moderate density of HDM, only one that have a
history of urticarial (p>0.05). 15 participants were
sensitive to HDM (positive SPT), and three of them
had moderate density of HDM (p>0.05).
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
254
From anamnesis, we found that all 10 AD participants
had relapse in the last three months. And out of 10
AD participants, eight samples (80%) were sensitive
against HDM allergen.
4 DISCUSSION
The house dust mites are the most common
environmental allergens. Mites sensitize and induce
allergic disorders such as perennial rhinitis and
asthma in predisposed individuals. In addition, house
dust mites are important deteriorating factors in
patients with atopic dermatitis (Tupker et al., 1998).
Although definite causality has yet to be
determined, it has been alleged that HDMs play a role
in the immunopathogenesis of AD. Not only do AD
patients have elevated levels of serum IgE antibodies
specific to HDM allergens, biopsy specimens of AD
lesional skin have also been shown to be infiltrated
with T lymphocytes that recognize HDM. It has been
shown that HDM may facilitate its entry into AD skin
by enzymatically breaking down the epidermal
barrier. Mite allergens are able to activate
keratinocytes and induce them to produce and secrete
proinflammatory cytokines (Gavino et al., 2008).
Briefly, the prevalence of allergic diseases due to
household arthropods have significantly increased in
the recent last decades, because people spend most of
their time in their home environment and according
to the modern lifestyle, houses are warmer and filled
with a lot of furniture and not enough air-regulation
is provided (Ziyaei et al., 2017). In this study, we
determined the correlation between density of HDM
with the incidence of atopic dermatitis.
Out of 10 participants with atopic dermatitis, two
(20%) had moderate density of HDM in bedroom
(p>0.05). Also, from seven samples with moderate
density of HDM, three (20%) were sensitive against
HDM (p>0.05). There was no evidence to support the
first assumption, as no difference in incidence of
atopic dermatitis with HDM density that was counted
from patients’ clothes and bedding, although an
earlier study had reported there were larger numbers
of HDMs in the mattresses of patients with AD when
compared with controls.
8
However, all AD
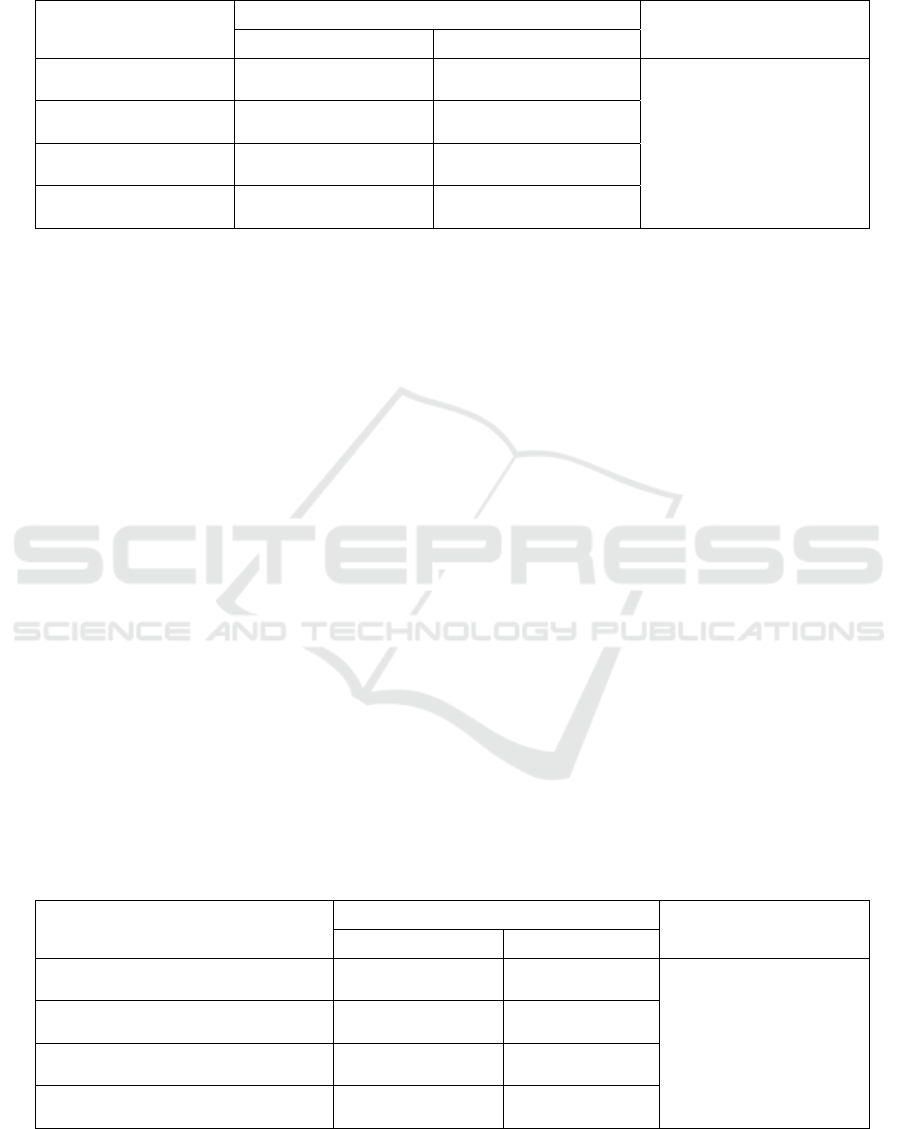
Table 1. Correlation between HDM density with incidence of atopic dermatitis
HDM DENSITY
INCIDENCE OF ATOPIC DERMATITIS
P value
YES NO
HIGH
0
(
0%
)
0
(
0%
)
p 1.000
MODERATE
2
(20.0%)
5
(25.0%)
LOW
8
(80.0%)
15
(75.0%)
TOTAL
12
(
100%
)
18
(
100%
)
Table 2. Correlation between HDM density with sensitivity of HDM
HDM DENSITY
SKIN PRICK TEST
P value
POSITIVE NEGATIVE
HIGH
0
(
0%
)
0
(
0%
)
p 1.000
MODERATE
3
(20%)
4
(26.7)
LOW
12
(80%)
11
(73.3%)
TOTAL
15
(
100%
)
15
(
100%
)
Correlation between Density of House Dust Mites and Relapse Rate of Atopic Dermatitis: A Cross Sectional Study
255

participant had relapse within three months while
80% of them positive to SPT indicates that HDM
allergen might induce the recurrence of disease.
5 CONCLUSION
Even though recent evidence supports a role for HDM
in atopic dermatitis, the correlation of its density with
prevalence of occurrence of atopic dermatitis still
needs further research with bigger sample size.
ACKNOWLEDGMENT
This research is not sponsored and there is no
conflict of interests.
REFERENCES
Casimir, G.J., Duchateau, J., Gossart, B., Cuvelier, P.,
Vandaele, F., Vis, H.L., 1993. Atopic dermatitis: role of
food and house dust mite allergens. Pediatrics 92, 252–
256.
Gavino, A.C., Needham, G.R., High, W.A., 2008. Atopic
dermatitis, patch testing, and house dust mites: a brief
review. Dermatitis 19, 121–128.
Leung, D.Y.M., Eichenfield, L.F., Boguniewicz, M. 2012.
Atopic Dermatitis (Atopic Eczema). In: Wolff, K.,
Goldsmith, L.A., Katz, S.I., Gilchrest, B.A., Paller,
A.S., Leffell, D.J., editors. Fitzpatrick’s dermatology in
general medicine. 8
th
ed: vol.1. New York: McGraw-
Hill, p.165-82.
Norris, P., Schofield, O., Camp, R. 1988. A study of the role
of house dust mite in atopic dermatitis. British Journal
of Dermatology. 118(3), 435-440.
Platts-Mills, T.A.E., Chapman, M.D., 1987. Dust mites:
Immunology, allergic disease, and environmental
control. J. Allergy Clin. Immunol. 80, 755–775.
https://doi.org/10.1016/S0091-6749(87)80261-0
Teplitsky, V., Mumcuoglu, K.Y., Babai, I., Dalal, I., Cohen,
R., Tanay, A., 2008. House dust mites on skin, clothes,
and bedding of atopic dermatitis patients. Int. J.
Dermatol. 47, 790–795. https://doi.org/10.1111/j.1365-
4632.2008.03657.x
Tupker, R. a, de Monchy, J.G., Coenraads, P.J., 1998.
House-dust mite hypersensitivity, eczema, and other
nonpulmonary manifestations of allergy. Allergy 53,
92–6.
Werfel, T., Breuer, K., Ruéff, F., Przybilla, B., Worm, M.,
Grewe, M., Ruzicka, T., Brehler, R., Wolf, H.,
Schnitker, J., Kapp, a, 2006. Usefulness of specific
immunotherapy in patients with atopic dermatitis and
allergic sensitization to house dust mites: a multi-
centre, randomized, dose-response study. Allergy 61,
202–205. https://doi.org/10.1111/j.1398-
9995.2006.00974.x
Ziyaei, T., Berenji, F., Jabbari-Azad, F., Fata, A., Jarahi, L.,
Fereidouni, M., 2017. House dust mite prevalence in the
house of patients with atopic dermatitis in Mashhad,
Iran. J. Arthropod. Borne. Dis. 11, 299–304.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
256
