
Clinical and Life Quality Improvement, and IL-17 Serum Level in
Psoriasis Patients Treated with Metothrexate Injection: A Pilot Study
in 15 Severe Psoriasis Cases
Prasta Bayu Putra
1*
, Kusnindita Noria Rahmawati
1
, Adissa Tiara Yulinvia
1
, Sunardi Radiono
2
, Dyah
Ayu Mira Oktarina
3
1
Department of Dermatology and Venereology, Gadjah Mada University/Sardjito General Hospital, Yogyakarta-Indonesia
2
Department of Dermatology and Venereology, Erythrosquamous Disease and Phototherapy Subdivision, Gadjah Mada
University/Sardjito General Hospital, Yogyakarta-Indonesia
3
Department of Dermatology and Venereology, Dermatopathology Subdivision, Gadjah Mada University/Sardjito General
Hospital, Yogyakarta-Indonesia
Keywords: Severe Psoriasis, Methotrexate Injection, Clinical Improvement, Life Quality Improvement, IL-17 serum
level
Abstract: Psoriasis is an autoimmune T cell mediated chronic skin disorder which is difficult to treat. Conventional
therapy using oral methotrexate in severe cases often showed unsatisfying result. Our department was
developing methotrexate injection protocol for severe cases to improve patient treatment and life quality and
for achieving quick remission. Objective: This pilot study was aimed to observe efficacy of methotrexate
injection 50mg/week for 6 consecutive weeks. Method: Study subjects were severe psoriasis patients that
unresponsive to any conventional therapies. PASI score and DLQI score improvement and serum IL-17 level
at the end of study were measured. Result: PASI-100 was achieved by 12 subjects (80%) at the end of sixth
weeks. DLQI score were significantly different (p<0.001) after sixth injection and subjects serum IL-17 level
were not significantly different with healthy peoples at the end of study. Conclusion: Methotrexate injection
50mg/week for 6 consecutive weeks initiation can be considered as an effective treatment for severe psoriasis.
Further studies with larger samples and longer observation period are needed to determine long term efficacy,
side effects, and protocol guideline policy.
1 INTRODUCTION
Psoriasis is an autoimmune T cell mediated chronic
skin disorder with polygenic predisposition and
clinical manifestation such as papule and
erythematous plaque with thick scale, pustular, or
erythroderma (Gudjonsson et al., 2012). Psoriasis
pathogenesis is run by IL-23/Th17 axis, in which IL-
23 is Th17 cell activator, and IL-17 is the prime
secreted cytokine. Recent study also reported that IL-
23 and IL-17 can be used to assess psoriasis remission
(Chiricozzi, 2014; Karczewski et al., 2016).
Psoriasis often need long term therapy and
difficult to treat. Conventional therapeutic modalities
that can be used for psoriasis treatment consist of
topical agent, systemic, and phototherapy. Topical
corticosteroid, vitamin D analogues, tazaroten, and
calcineurin inhibitor can be used as topical therapy.
Cyclosporine, methotrexate, acitretin, fumaric acid
esther, hydroxyurea, mychophenolate mofetil, and
sulfasalazine can be used as systemic therapy.
Phototherapy modality consist of Narrowband
Ultraviolet B (NB-UVB), Broadband Ultraviolet B
(BB-UVB), and Psoralen with Ultraviolet A (PUVA)
(Gudjonsson et al., 2012).
Methotrexate is the prime choice for systemic
conventional therapy in psoriasis treatment that has
anti-proliferative effect by inhibition of DNA
synthesis giving anti-inflammatory and
immunosuppression effect (Puig, 2014; Yélamos &
Puig, 2015)
Mild to severe psoriasis and psoriasis that
unresponsive to topical therapy and phototherapy are
the indications of methotrexate administration.
Methotrexate as single psoriasis drug need 1-8 weeks
to achieve therapeutic effects. High dose
methotrexate (15-25 mg/week) is more effective than
176
Putra, P., Rahmawati, K., Yulinvia, A., Radiono, S. and Oktarina, D.
Clinical and Life Quality Improvement, and IL-17 Serum Level in Psoriasis Patients Treated with Metothrexate Injection: A Pilot Study in 15 Severe Psoriasis Cases.
DOI: 10.5220/0008153401760180
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 176-180
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

low dose (7,5-15 mg/week) (Dogra & Mahajan,
2013).
The usual adverse effects of methotrexate such
as nausea, vomitus, bone marrow depression, folic
acid deficiency, and hepatotoxicity have been
reported. Cumulative dose more than 3 gram
increasing the hepatotoxicity risk (Pathirana et al.,
2009).
In severe psoriasis cases, the conventional therapy
using oral metothrexate often showed unsatisfying
results with low clinical and life quality improvement
(Gudjonsson et al., 2012). Due to the the disease
severity and socio-economic limitation, our
department tried to develop methotrexate injection
protocol. The protocol is using methrotrexate
injection 50mg/week for 6 consecutive weeks in
phase I, followed by two 50mg methotrexate injection
per two weeks in phase II and two 50mg methotrexate
injection per month for phase III. This is the pilot
study that observe efficacy of methotrexate injection
50mg/week for 6 consecutive weeks (phase I) in the
treatment of severe psoriasis from the clinical and life
quality improvement and serum IL-17. The result of
this study can be used as baseline data for further
study for determining efficacy, side effects, and
protocol guideline policy in severe psoriasis cases.
2 METHODS
The study was conducted in Dermatology and
Venereology Clinic and Ward Dr. Sardjito General
Hospital, and Dermatology and Venereology
Department Faculty of Medicine Gadjah Mada
University. All procedures were performed after
ethical clearance gained from Medical and Health
Research Ethics Committee of Faculty of Medicine,
Gadjah Mada University. Our study subjects
population were severe psoriasis patients that treated
regularly in Dr. Sardjito Hospital Yogyakarta during
September to December 2017 period and previously
unresponsive to any conventional psoriais therapies.
Selected subjects in this study were erythroderma
psoriatica or psoriasis vulgaris patients with PASI
score more than 25, who previously unresponsive to
conventional therapies. Patients with other
autoimmune disease, immunodeficiency, pregnancy
and lactation, obesity with BMI>30kg/m
2
, severe
anemia, in combination therapy with other
immunosuppressive drugs, renal failure, elevated
lived transaminase enzyme, hepatitis, or cirrhosis
were excluded from this study. Patients were
informed about the protocol, asked for consent and
recruited as study subjects if they signed the informed
consent form. Methotrexate 50 mg/week for 6
consecutive weeks was administered via
intramuscular injection.
Psoriasis disease severity and remission were
assessed using Psoriasis Area and Severity Index
(PASI) score at the beginning of the therapy
(baseline) and one week after each of methotrexate
injection until 6
th
injection. Patient’s life quality was
assessed using Dermatological Life Quality Index
(DLQI) score at the beginning of the therapy
(baseline) and one week after 6
th
methotrexate
injection. Blood samples from the subjects were taken
at one week after the 6
th
injection and from healthy
peoples without autoimmune disease or systemic
infection, to measure IL-17A serum level using
Komabiotech
®
human IL-17A ELISA kit. The data
were analyzed using IBM SPSS
®
version 24
comparative and correlation test, with the p value
<0.05 was considered as significant result.
3 RESULT
During September to December 2017 there were 15
severe psoriasis patients that undergo methotrexate
injection therapy in Dermatology and Venereology
Clinic and Ward unit Dr. Sardjito General Hospital
Yogyakarta. Mean subject’s age was 46 ± 3,98 years
old, which is range from 18 to 66 years old and consist
of 12 men and 3 women. From the occupation, most
of the subjects were farmer and labor (Table 1). The
baseline PASI score and DLQI score were
significantly decreased after 6
th
injection, and there
was no significant serum IL-17 level difference found
between subjects and healthy peoples at the end of
therapy (Table 2).
In this study 87% subjects achieved PASI-75 at
the end of therapy, which was achieved mostly after
the third injection. The PASI-100 was achieved
mostly after the fourth injection and at the end of
therapy was achieved by 80% subjects. There were
13% and 20% non responsive subjects that improved
clinically, but didn’t achieved PASI-75 and PASI-
100 respectively at the end of study (Chart 1). From
statistic analysis test result, there was significant
linear correlation between PASI score improvement
(ΔPASI score) and DLQI score improvement
(ΔDLQI score) with strong correlation power (r=
0.641, p= 0.01) (Chart 2).
Clinical and Life Quality Improvement, and IL-17 Serum Level in Psoriasis Patients Treated with Metothrexate Injection: A Pilot Study in
15 Severe Psoriasis Cases
177
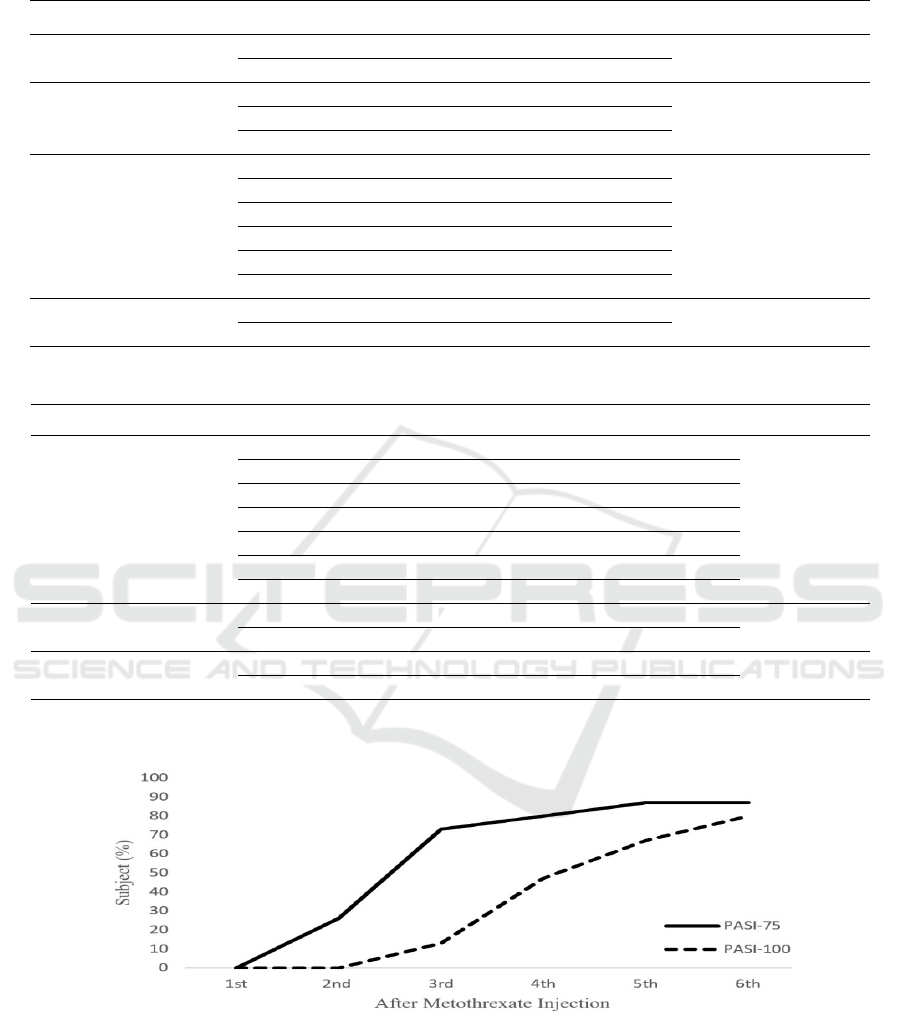
Table 1. Subject characteristics
Characteristics Total (%) Mean
Sex Male 12 (80%)
Female 3 (20%)
Age <40
y
ears ol
d
4 (27%) 46 ± 3,98
40-60
y
ears ol
d
8 (53%)
>60
y
ears ol
d
3 (20%)
Job Farme
r
5 (33%)
Labo
r
4 (27%)
Studen
t
2 (13%)
Housewife 2 (13%)
Office wor
k
1 (6,7%)
Teache
r
1 (6,7%)
Diagnosis Er
y
throderma Psoriatica 9 (60%)
Psoriasis Vul
g
aris 6 (40%)
Table 2. PASI scores, DLQI scores, & serum IL-17 levels data
Measurement Period Mean p Value
PASI Score Baseline 51,56 ± 4,41 0.001
1
Post 1
st
In
j
ection 32,1 ±3,04
Post 2
nd
In
j
ection 18,52 ± 2,38
Post 3
rd
In
j
ection 9,6 ± 1,8
Post 4
th
In
j
ection 3,92 ± 1,56
Post 5
th
In
j
ection 2,14 ± 1,27
Post 6
th
In
j
ection 1,36 ± 1,08
DLQI Score Baseline 27.6 ± 0,66 0.001
1
Post 6
th
In
j
ection 5,27 ± 0,78
Serum IL-17 Level Health
y
Peoples 7,75 ± 0,41 0.070
2
Sub
j
ects (Post 6
th
In
j
ection) 9,68 ± 0,79
1
p value is obtained from Wilcoxon comparative test
2
p value is obtained from Mann Whitney comparative test
Chart 1. Subject PASI-75, PASI-100
(ΔPASI score) and DLQI score improvement (ΔDLQI score) with strong correlation power (r= 0.641, p= 0.01)
(Chart 2).
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
178
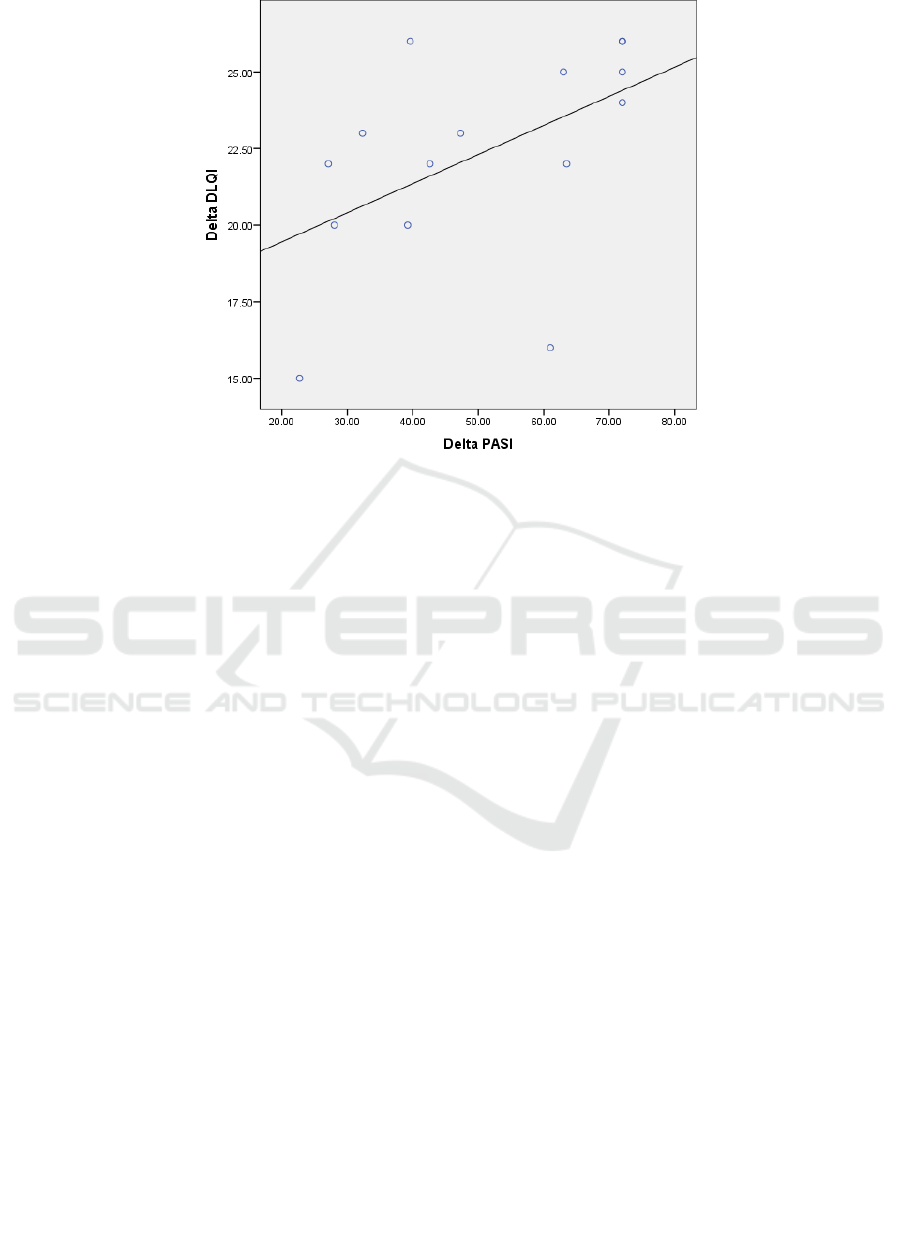
Chart 2. ΔPASI score & ΔDLQI score correlation
1
p value is obtained from Spearman correlation test
2
correlation coefficient (r) is obtained from Spearman correlation test
*ΔPASI & ΔDLQI Score obtained from difference between baseline and post 6
th
injection score
4 DISCUSSION
Methotrexate is the prime choice for systemic
conventional therapy in patient with extensive,
refractory, or severe psoriasis. Methotrexate
monotherapy in psoriasis treatment show various
responses depend on the administered dose (Dogra &
Mahajan, 2013). When low dose is used (7,5-
15mg/week), PASI-75 response is achieved by 24%
patients at 12
th
week. When higher dose is used (15-
25mg/week), PASI-75 response is achieved by 42-
60% patients at 16
th
week (Cabello et al., 2017). In
this study the earliest PASI-75 and PASI-100
responses was achieved at 2
nd
week by 26% subjects
and at 3
rd
week by 13% subjects respectively by using
50mg/week methotrexate dose. These findings are in
line with previous studies that higher dose of
methotrexate could induce quicker remission in study
subjects.
IL-17 is a cytokine that has role in psoriasis
pathogenesis and host defence against pathogens such
as bacteria and fungal. IL-17 cytokine has 6 subunits
that consist of IL-17 (A-F) and 5 receptor subunits
that consist of IL-17R (A-E). IL-17A cytokine
subunit and IL-17RA and IL-17RC receptor subunits
are the subunits that have major role in psoriasis
pathogenesis (AbuHilal et al., 2016)
The importance of IL-17 in the pathogenesis can
be used to assess psoriasis remission (Karczewski et
al., 2016). In this study we found that the subject’s
serum IL-17 level after 6
th
injection had no significant
difference with the healthy peoples and we assumed
the remission was achieved. However, IL-17 serum
level in study subjects was still higher than in healthy
peoples.
Dermatological life quality index score is the most
often used tool for assessing patient life quality due
to its reliability and applicability. Revicki et al (2008)
study on moderate to severe plaque psoriasis reported
that PASI score improvement had correlation with
DLQI score improvement (Revicki et al., 2008). The
same results had been found in this study, in which
the PASI score and DLQI score improvement
significantly correlated. Significant difference also
can be found between baseline and after 6
th
injection
in DLQI score and PASI score as well.
In this study we also found that the earliest PASI-
75 and PASI-100 responses were achieved by all <40
years and >60 years old subjects and some of 40-60
years old subjects. All of non responsive subjects
derived from 40-60 years old subjects showed PASI
score improvement, however they did not achieved
PASI-75 and PASI-100 responses after 6 consecutive
weeks of 50mg/week methotrexate injection. Daily
Clinical and Life Quality Improvement, and IL-17 Serum Level in Psoriasis Patients Treated with Metothrexate Injection: A Pilot Study in
15 Severe Psoriasis Cases
179

activity, job, and environmental exposure might have
role in this condition, as the subject’s job majority are
farmers and labors that usually work without
protective equipment, which can triggering new
lesions formation or aggravating the old lesions
(Mahler et al., 2014).
5 CONCLUSION
This study reported that methotrexate injection
protocol 50mg/week for 6 consecutive weeks
initiation can be considered as an effective treatment
for severe psoriasis. Most of the subjects had
achieved full remission and significantly improved
quality of life at the end of protocol. Both clinical and
life quality improvement were significantly
correlated each other in this study. Further studies
with larger samples and longer observation period are
needed to determine long term efficacy, side effects,
and protocol guideline policy.
ACKNOWLEDGEMENT
This study was self funded by the authors without
using any research grant, scholarship, or sponsorship.
REFERENCES
AbuHilal, M., Walsh, S., Shear, N., 2016. The Role of IL-
17 in the Pathogenesis of Psoriasis and Update on IL-
17 Inhibitors for the Treatment of Plaque Psoriasis.
Journal of Cutaneous Medicine and Surgery, 20, 509–
516. doi:10.1177/1203475416651605
Cabello Zurita, C., Grau Pérez, M., Hernández Fernández,
C.P., González Quesada, A., Valerón Almazán, P.,
Vilar Alejo, J., Carretero Hernández, G., 2017.
Effectiveness and safety of Methotrexate in psoriasis:
an eight-year experience with 218 patients. Journal of
Dermatological Treatment, 28, 401–405.
doi:10.1080/09546634.2016.1273469
Chiricozzi, A., 2014. Pathogenic role of IL-17 in psoriasis
and psoriatic arthritis. Actas dermo-sifiliograficas, 105,
Suppl, 9–20. doi:10.1016/S0001-7310(14)70014-6
Dogra, S., Mahajan, R., 2013. Systemic methotrexate
therapy for psoriasis: Past, present and future. Clinical
and Experimental Dermatology,
doi:10.1111/ced.12062
Gudjonsson JE, Elder JT. Psoriasis. In: Wolff K, Goldsmith
LA, Katz SI, Gilchrest BA, Paller AS, Leffel DJ, eds.
Fitzpatrick’s Dermatology in General Medicine 8th ed.
New York: McGraw-Hill;. 2012:197-231.
Karczewski, J., Dobrowolska, A., Rychlewska-
Hańczewska, A., Adamski, Z., 2016. New insights into
the role of T cells in pathogenesis of psoriasis and
psoriatic arthritis. Autoimmunity.
doi:10.3109/08916934.2016.1166214
Mahler, V., Diepgen, T., Skudlik, C., Becker, D., Dickel,
H., Fartasch, M., Geier, J., Häberle, M., Hillen, U.,
Krohn, S., John, S.M. alte, Weisshaar, E., Werfel, T.,
Zagrodnik, F., 2014. Psoriasis predisposition and
occupational triggering factors in the appraisal of
occupational medical expertises. Journal der Deutschen
Dermatologischen Gesellschaft = Journal of the
German Society of Dermatology : JDDG, 12, 519–529.
doi:10.1111/ddg.12262
Pathirana, D., Ormerod, a D., Saiag, P., Smith, C., Spuls,
P.I., Nast, a, Barker, J., Bos, J.D., Burmester, G.-R.,
Chimenti, S., Dubertret, L., Eberlein, B., Erdmann, R.,
Ferguson, J., Girolomoni, G., Gisondi, P., Giunta, a,
Griffiths, C., Hönigsmann, H., Hussain, M., Jobling, R.,
Karvonen, S.-L., Kemeny, L., Kopp, I., Leonardi, C.,
Maccarone, M., Menter, a, Mrowietz, U., Naldi, L.,
Nijsten, T., Ortonne, J.-P., Orzechowski, H.-D.,
Rantanen, T., Reich, K., Reytan, N., Richards, H., Thio,
H.B., van de Kerkhof, P., Rzany, B., 2009. European
S3-guidelines on the systemic treatment of psoriasis
vulgaris. Journal of the European Academy of
Dermatology and Venereology : JEADV 23 Suppl 2, 1–
70. doi:10.1111/j.1468-3083.2009.03389.x
Puig, L., 2014. Methotrexate: New Therapeutic
Approaches. Actas Dermo-Sifiliográficas (English
Edition) 105, 583–589.
doi:10.1016/j.adengl.2014.05.011
Revicki, D. a, Willian, M.K., Menter, A., Saurat, J.-H.,
Harnam, N., Kaul, M., 2008. Relationship between
clinical response to therapy and health-related quality
of life outcomes in patients with moderate to severe
plaque psoriasis. Dermatology (Basel, Switzerland)
216, 260–70. doi:10.1159/000113150
Yélamos, O., Puig, L., 2015. Systemic methotrexate for the
treatment of psoriasis. Expert Review of Clinical
Immunology, 11, 553–563.
doi:10.1586/1744666X.2015.1026894
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
180
