
The Correlation of Contraception with Sexually Transmitted
Infection and HIV Infections on Female Sex Workers in Surakarta
Ambar Aliwardani, Putti Fatiharani Dewi, Rini Hastuti, Mardiana, Endra Yustin Ellistasari
Dermatovenereology Departement, Dr. Moewardi General Hospital/Faculty of Medicine
Sebelas Maret University, Surakarta, Indonesia
Keywords: Sexually Transmitted Infections, HIV Infections, contraception
Abstract: The control and prevention of Sexually Transmitted Infections (STIs) and Human Immunodeficiency Virus
(HIV) infections still a major challenge especially in developing countries. One of the high risk groups that
can spread STIs and HIV infection are female sex workers (FSWs). Condom as one of contraception can be
used as a way in preventing transmission of STIs and HIV infection. However the other method, especially
hormonal contraception such as Oral contraception pills (OCPs) and Injection can increase the risk of STIs
and HIV infection. The purpose of this study was to determine the correlation between the use of contraception
with the occurrence of STIs and HIV infection in FSWs in Surakarta. A cross sectional study was conducted
FSWs in several areas in Surakarta. A total 75 female sex workers completed a questionnaire and provided
blood samples for HIV and syphilis testing, endocervical and vaginal swab were performed for STIs
examination. Chi Square Test was used for the statistical analysis. There was a significant correlation between
the use of hormonal contraceptive especially in implant with HIV incident.
1 INTRODUCTION
Sexually Transmitted Infections (STIs) are still a
major public health problem for developed and
developing countries, despite the availability of
therapies and effective preventive measures.More
than 1 millions STIs are occurred everyday
worldwide. Each year, it is estimated 357 millions new
infections have 1 of 4 STIs such as chlamydia (131
milion), gonorrhoeae (78 million), syphilis (5.5
million) and trichomoniasis (143 million) (WHO,
2016).The association between STIs and Human
Immunodeficiency Virus (HIV) infection has been
widely reported whereas STIs can increase the risk of
HIV transmission. Untreated STIs can increase the
risk of transmitting HIV infection up to 3 times higher
than people without STIs (Gyawale and Pokhrel,
2014).
The global HIV prevalence in the world is
increasing especially in the female population. By
2012 in the world 35.3 million people infected with
HIV and 1.6 million people died from acquired
immunodeficiency syndrome (AIDS) (Mabey,
2014).The regions with the highest mortality rates are
Sub Saharan Africa, the Caribbean, and South and
Southeast Asia in Asia, Indonesia ranks in the top five
highest in the number of people living with HIV
whereas in 2012 there were 370 thousands new cases
of HIV infection and HIV epidemic in the region has
been concentrated in key populations at higher risk of
HIV exposure, including commercial sex worker
(Dokubo et al., 2013).In Central Java, particularly in
Surakarta, based on the data from the Surakarta AIDS
Commission (KPA) in 2015 in the FSWs group there
were 263 new STIs cases and 77 new HIV infections
(Komisi Penanggulangan AIDS, 2016).
Contraception can be used as a way of preventing
transmission of STIs and HIV infection in sex
workers. Using contraception has several benefits i.e
prevention of unplanned pregnancies and protection
against STIs, reduction in the risk of Pelvic
Inflammatory Diseases (PID) and also protection from
HIV infection especially in high risk group like FSWs.
There are many methods of contraception such as
the barrier method of male and female condoms,
hormonal methods of contraception, including oral
contraception pills (OCPs), combination of estrogen
and progestin injectable, progestin-only injectable
such as depo-medroxyprogesterone acetate (DMPA),
and hormone containing technologies i.eimplants,
intrauterine devices (IUD), patches, and rings
(Morrison and Cates, 2008;Baeten and Heffron,
2015).
136
Aliwardani, A., Dewi, P., Hastuti, R., Mardiana, . and Ellistasari, E.
The Corelation of Contraception with Sexually Transmitted Infection and HIV Infections on Female Sex Workers in Surakarta.
DOI: 10.5220/0008152501360140
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 136-140
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

There have been many literatures reviewing the
effect of different contraception on the risk of STIs
and HIV. In general, they all come to the same
conclusion that male condoms used correctly and
consistenly provide good protection against mostSTIs,
both bacterial and viral (Steiner et al., 2008).
Several
studies have suggested a possibble link between
hormonal contraception use and enhanced HIV-1
suspectibility, although other studies have found no
such link. Study by Grabowski et all suggested that
hormonal contraception especially DMPA might
increase HIV risk.They reported that DMPA injection
could increased genital inflammation and increased
cervical DNA shedding (expressed either as
detectability or quantity) (Baeten and Heffron, 2015).
It is still debatable whether contraception use is
related to STIs and HIV. Therefore we conducted this
cross sectional study to investigate the correlation of
contraception with STIs and HIV among FSWs in
Surakarta.
2 METHODS
Cross sectional study was conducted in FSWs in
Surakarta. Female sex workers (FSWs) who were still
actively working willing to be interviewed and fill in
questionnaires, undergo endocervical and vaginal
swab examinations were performed at the sites.
Laboratory examinations were performed at dr.
Moewardi Hospital using Gram examination for Non-
Specific Genital Infection (NSGI), Neisseria
gonorhoea and Bacterial Vaginosis (BV), NaCl for
Trichomonas Vaginalis (TV), KOH for
Vulvovaginalis Candidiasis (VVC), Acetowhite test
for Condiloma Acuminata (CA) and Rapid Test for
Syphilis and HIV . All data were analyzed with
SPSSversion 17, Chi Square Test was used for the
stastitical analysis, p<0.05 was considered
significant.
3 RESULT
The total subjects were 75 FSWs. Most of FSWs aged
between 26-49, with the longest time being FSWs
was <5 years. Most of these FSWs had more than
twice sexual intercourse in a week (71%).
Contraception with 3 month injection was the most
preferable contraception used by FSWs. The
incidence of STIs in this study was 53.33%. STIs
were found in 40 WPS, consisting of Bacterial
Vaginosis 18.67%, Syphilis 14.67%, Vulvo vaginalis
Candidiosis 9.3%, Trichomoniasis 5.3%, Non-
Specific Genital Infection (2.6%), Cervicitis
Gonorrhoeae (1.33%) and Condyloma Acuminata
(1.33%).
Based on table 2 , there were no significant
correlation between contraceptive use with STIs and
HIV. However implant contraception had a
significant correlation with HIV infection (P value <
0.002, Contingency Coeficient (CC) 44.7%).
4 DISCUSSION
The use of contraception is closely relatedto
prevention efforts of STIs and HIV. Given the
different cultures and contraceptive practices, several
methods of providing protection from unintended
pregnancy, STIs and HIV infection should ideally be
available.
Globally more than 100 million women use
hormonal contraception in which it is associated with
potential effects of HIV infection. The association of
the effects of hormonal contraception with the risk of
HIV infection remains a matter of debate.Hormonal
contraception could act through a number of
biological. There are multiple mechanisms by which
the use of hormonal contaception might increase a
woman’s suspectibility to HIV infection. The
possible mechanism include the ability of oral
contraception to increase cervical ectopy which then
increases the susceptibility to STIs including HIV,
increased cervical chlamydial infection, a
hypoestrogenic effect associated with DMPA
injection use resulting in thining of the vaginal
epitelium, reduction in hydrogen peroxide producing
lactobacilli (and thereby decreased vaginal acidity)
and irregular uterine bleeding, suppression of the
local (cell-mediated) immune response and increased
recruitment of inflammatory and other target cells to
the genital tract or through a direct effect on the
infecting virus inoculum by upregulating HIV gene
expression and associated viral replication (Morrison
and Cates, 2008;Baeten and Heffron, 2015).
A prospective study revealed an increased
incidence of STIs in women using hormonal
contraception.Study by Borgdorff H in Rwandan
female sex workers reported that oral contraception
(OCPs) use was associated with increased Chlamydia
trachomatis incidence and injectable use significantly
associated with candidiasis incidence (H Borgdoff et
al., 2015).
A systematic review and meta analysis by
LAVodstrcilreported that hormonal contraception use
was associated with a significant reduced risk of
Bacterial Vaginosis (Vodstrcil et al., 2013).However,
The Corelation of Contraception with Sexually Transmitted Infection and HIV Infections on Female Sex Workers in Surakarta
137
in our study the oral contraception group had high rate
of BV infection (2.67%) followed by Cervicitis
gonorrhoeae infection (1.33%) while in the
contraceptive injection group
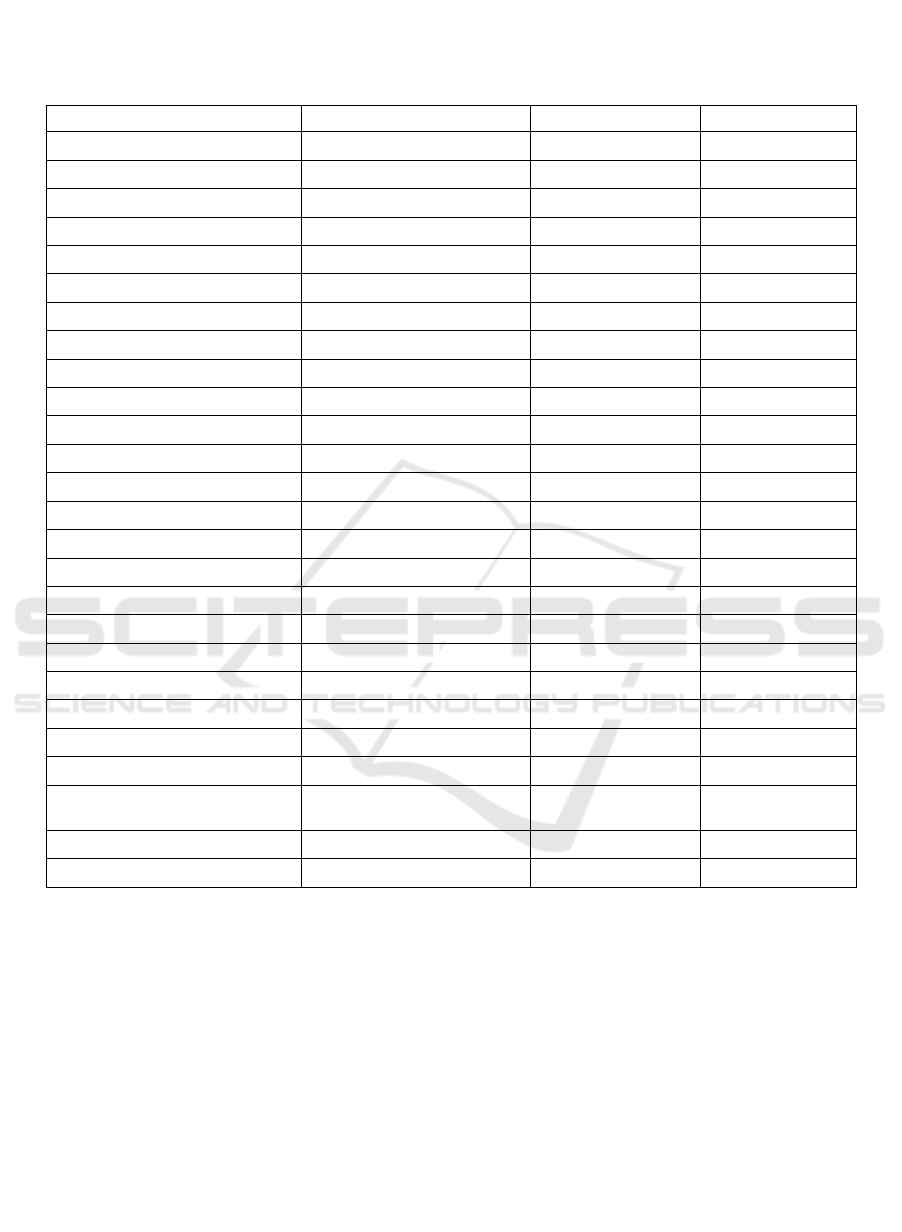
Table 1. Demographic characteristics of Female Sex Workers in Surakarta.
Characteristic Frequency (n=75) Percent (%)
Current Age <25 years of age 2 2.6
26-49years of age 69 92
>50 years of age 4 5.3
Length of work <5 years 39 52
5-10 years 20 26.67
>10 years 16 21.33
Sex Frequency>2x/week Yes 71 94.6
No 4 5.3
Condom use Always 42 56
Occasionally 33 44
Contraceptive Method No 25 33.33
Injectionof 3 months 22 2.3
Injectionof 1 month 10 13.3
Pill 11 14.6
Implant 5 6.67
IUD 2 2.67
HIV Yes 3 4
No 72 96
STIs No 35 46.67
Bacterial Vaginosis 14 18.67
Syphilis 11 14.67
Vulvovaginalis Candidiasis 7 9.3
Trichomoniasis 4 5.3
Non Specific Genital
Infection
2 2.6
Cervicitis Gonorrhoeae 1 1.33
CondilomaAcuminata 1 1.33
the incidence of STIs including BV (6.67%), NSGI
(1.33%) and Trichomoniasis ( 2.67%). There was no
significant correlation between the length
contraception use with the incidence of STIs or HIV
infection.
Some cross sectional studies reported that
hormonal contraception was use significantly
associated with increased amount of HIV-1 DNA in
genital tract. The only prospective study by Wang
measured HIV-1DNA levels before and after
initiation of hormonal contraception confirmed the
findings that 2 months after the initiation of hormonal
contraception, endocervical HIV-1 DNA increased
(Blish and Baeten, 2011).Study by CB Polis et all
assessed genital viral shedding comparing the
levonorgestrel implant reported no change in cervical
or vaginal tract (CB Polis et al., 2013).In our study
revealed a significant correlation between the use of
hormonal contraception (the implant group) and the
incidence of HIV infection (P value < 0.002,
Contingency Coeficient (CC) 44.7%).
Mechanical barriers contraception, such as
condom, may provide some protection against
bacterial STIs, their impact on HIV prevention is
currently under study. One analysis by AN Turner et
all compared findings from case crossover design
with a traditional cohort analysis found that condoms
were significantly protective against STIs especially
chlamydial and gonococcal infection
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
138
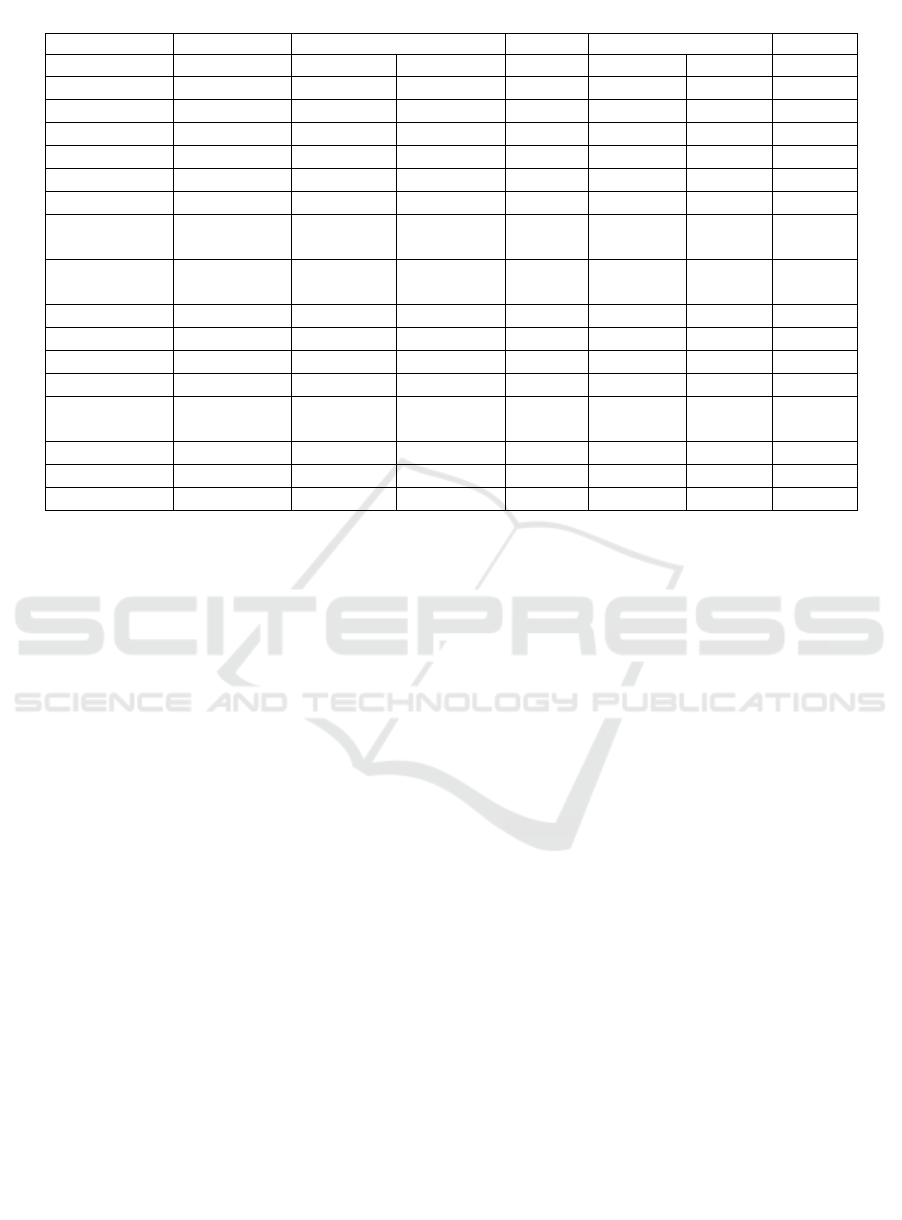
Table 2. The correlation between contraception, STIs and HIV.
STIs P Value HIV P Value
No Yes
No Yes
Contraceptive Yes
30 (40%) 20(26.7%) 0.509 48 (64%) 2 (2.7%) 1.000
No
13(17.3%) 12 (16%) 24 (32%) 1 (1.3%)
Total 33(57.3%) 32(42.7%) 72 (96%) 3 (4%)
Condom Always 24(32%) 18(24%) 0.970 40(53.3%) 2(2.7%) 0.704
Occasionally 19(25.3%) 14(18.7%) 32(42.7%) 11.3%)
Total 43(57.3) 32(42.6%) 72(96%) 3(4%)
Contraceptive
Types
Injection 3
month
13(17.3%) 9 (12%) 0.875 22(29,3%) 0 (0%)
Injection 1
month
7 (9.3%) 3 (4%) 10(13.3%) 0 (0%)
Pill 7 (9.3%) 4 (5.3%) 11(14.6%) 0 (0%)
Implant* 2 (2.7%) 3 (4%) 3 (4%) 2 (2,7%) 0.002*
IUD 1 (1.3%) 1 (1.3%) 2 (2.7%) 0 (0%)
Total 30(39.9%) 20(26.6%) 48(63.9%) 2(2,7%)
Contraceptive
Use
< 1 year 4 (18.2%) 2 (9.1%) 0.469 6 (27.3%) 0 (0%) 0.592
2-5 years 2 (9.1%) 3 (13.1%) 5 (22.7%) 0 (0%)
>5 years 4 (18.2%) 7 (31.8%) 10(45.5%) 1 (4.5%)
Total 10(45.5%) 12(54,5%) 21(95.5%) 1(4.5%)
*Significant statistically
(Turner et al., 2011). The study in Surakarta revealed
a significant relation between condom use and the
incidence of STIs and HIV among FSWs in surakarta
(Yuliarto et al., 2017).
our study revealed that the use
of either condom and iud contraception had no
correlation with stis and hiv infection
5 CONCLUSION
The use of implant contraception is significantly
correlated with HIV infection. However the use
contraception including condom and the length of
contraception use have no significant correlation with
STIs and HIV infection among FSWs. Further study
with larger sample size is needed in order to
generalized these findings.
REFEREENCES
Baeten, JM., Heffron, R., 2015. Contraception and sexually
transmitted infections : risks and benefits, hypotheses
and evidence. The Lancet Global Health, Lancetgh, 3,
430-431.
Blish, CA., Baeten, JM., 2011. Hormonal contraception and
HIV-1 transmission. American Journal of Reproductive
Immunology, Mar 65 (3), 302-7.
Borgdorff, H., Verwijs, M. C., Wit, F. W., Tsivtsivadze, E.,
Ndayisaba, G. F., Verhelst, R., Schuren, F. H. & Van De
Wijgert, J. H., 2015. The Impact of Hormonal
Contraception and Pregnancy on Sexually Transmitted
Infections and on Cervicovaginal Microbiota in African
Sex Workers. Sexually transmitted diseases Pubmed.
March, 42 (3), 143-152.
Dokubo, EK., Kim, AA., Le, LV., Nadol, PJ., Prybylski, D.,
Wolve, MI., 2013. HIV Incidence in Asia : A Review of
Available Data and Assessment of the Epidemic. AIDS
Rev, 15, 67-76.
Gyawalee, M., Pokhrel. D., 2014. Pattern of Sexually
Transmitted Infections and Sexual Behavior in Patients
with Genital Symptomps. Nepal Journal of
Dermatology, Venereology & Leprology, 12(1), 20-27.
Komisi Penanggulangan AIDS. 2016. Target dan Capaian
KPA Kota Surakarta, Surakarta.
Mabey, D., 2014. Epidemiology of Sexually Transmitted
Infections. Medicine Journal, 1-4.
Morrison, CS., Cates, W Jr., 2008. Contraception,
Contraceptive Technology and STDs. In : Holmes KK,
Sparling PF, Stamm WE, Piot P, Wasserheit JN, Corey
L, et all. Sexually Transmitted Diseases. New York:
McGraw Hill, 1493–1506.
Polis, CB., Phillips, SJ., Curtis, KM., 2013. Hormonal
Contraceptive Use and Female to male HIV
Transmission : a systematic review of the
epidemiologic evidence. Aids Pubmed, 27, 493-505.
Steiner, Markus J., Warner, Lee., Stone, Katherine M.,
Cates, W Jr., 2008. Condoms and Other Barrier
Methods for Prevention of STD/HIV Infection and
Pregnancy. In : Holmes KK, Sparling PF, Stamm WE,
Piot P, Wasserheit JN, Corey L, et all. Sexually
Transmitted Diseases. New York: McGraw Hill, 1821–
18266.
The Corelation of Contraception with Sexually Transmitted Infection and HIV Infections on Female Sex Workers in Surakarta
139

Turner, AN., Feldblum, P., Hoke, TH., 2011. Condom use
and Sexually Transmitted Infections among Malagasy
Sex Workers. International Journal of STDs and AIDS,
22(10), 552-557.
Vodstrcil, LA., Hocking, JS., Law, M., Walker, S., Tabrizi,
SN., Fairley, CK., et all., 2013. Hormonal
Contraception Is Associated with a Reduced Risk of
Bacterial Vaginosis: A Systematic Review and Meta-
Analysis. Plos One, 8 (9), 1-16.
World Health Organisation., 2016. Sexually Transmitted
Infectons (STIs).
www.who.int/mediacentre/factsheets/fs110/en/.
Yuliarto, D., Ellistasari, EY., Hastuti, R., Dewi, W., Hartaty,
AT., 2017. Hubungan Frekuensi Pemakaian Kondom
dengan Infeksi Menular Seksual dan Human
Immunodeficiency Virus pada Wanita Pekerja Seks di
Surakarta. In : Proceeding Book Konas XV Perdoski.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
140
