
The Relation of Comorbidities with Psoriasis Patients Treated in
Ermatovenereology Outpatient Clinic of Dr. Moewardi General
Hospital Surakarta January 2013-December 2017
Tutik Rahayu, Eka Putra Wirawan, Marsita Endy Dhamayanti, Rina Diana, Danu Yuliarto, Arie
Kusumawardhani
Dermatovenerology Departement Dr.Moewardi General Hospital/Faculty of Medicine Sebelas Maret University,
Surakarta, Indonesia
Keywords: comorbidities, relation, psoriasis.
Abstract: Psoriasis is a chronic inflammatory disease with typically lesions and especially concerning on the body that
are often affected trauma. The onset of psoriasis is primarily 15-35 years of age, the prevalence various with
age, geography and environment. Immunopathogenic psoriasis involves Th1 and Th 17 cells that can cause
the formation of inflammatory mediators that can trigger other comorbidities physically, psychologically and
socially. This Cross sectional study assesed the relation of comorbidities with psoriasis in dermatovenerology
outpatient clinic of Dr. Moewardi Hospital Surakarta between January 2013-December 2017. Psoriasis
patients visited dermatovenereology outpatient clinic during January 2013-December 2017 were included in
our study. There were 97 psoriasis patients, of these 51 were males and 46 females. All study subjects were
under 80 years old. The data were analyzed statistically by using SPSS and Chi-Square test with P<0.05 was
considered significant. Various comorbidities were found including hypertension (28.6%), diabetic militus
(20.4%), hyperuricemia (4.1%), dyslipidemia (16.3%), nerve disease (6.1%), dermatophyte (12.2%), kidney
disease (14.3%), malignancy (6.1%), gastropathy (24.5%), obesity (4.1%), heart disease (26.5%), lung disease
(22.4%), arthritis psoriasis (10.2%), depression (12.2%), systemic lupus erytematosus/SLE (4.1%) and
vitiligo (2%). Chi-Square test showed that age and occupation are significantly relation with all
commorbidities with P=0.011 and P=0.000 respectively. Our study revealed that age and occupation are
related to comorbidities occured in psoriasis patients. The older the age and the lower the income the greater
the momorbidity affect psoriasis patients
1 INTRODUCTION
Psoriasis is a chronic inflammatory skin disease
associated with genetic. It is characterized by
complex changes in the epidermal growth,
differentiation, multiple biochemistry, immunology
and vascular abnormalities with an unknown
association of nervous system function. This chronic
disease is triggered by environment, trauma, infection
and medication, typical clinical features of psoriasis
is well defined erythematous plaque with thick
squama coated in white silvery layer, occuring on
elbow, knees, scalps, trunk and umbilicus which often
get trauma injury (Johan, 2012). Psoriasis has various
forms of clinical manifestations and the most
common variant is psoriasis vulgaris (Johan, 2012;
Factor, 2017).
The prevalence of psoriasis affected by several
factors such as age, geography and environment,
affecting for about 2%-3% of the overall population
with onset of patients ranging between the ages of 15-
35 years (Johan, 2012), (WHO, 2016). The incidence
of psoriasis in Asia is 0.4% and more common in
male patients and study by Eka et all in
RSUD.Dr.Moewardi Solo reported that the
prevalence rate is about 4.5% with male patients were
more dominant than females and age dominant in the
second and third decades (Johan, 2012; Putra, 2016).
The severity of this disease is assessed by
calculating psoriasis area and severity index (PASI)
and classified into 3 parts: mild, moderate and severe
( Bozek, 2017). The severity of PASI scores is often
associated with increased comorbidity in patients
with moderate to severe (WHO, 2016).
44
Rahayu, T., Wirawan, E., Dhamayanti, M., Diana, R., Yuliarto, D. and Kusumawardhani, A.
The Relation of Comorbidities with Psoriasis Patients Treated in Ermatovenereology Outpatient Clinic of Dr. Moewardi General Hospital Surakarta January 2013-December 2017.
DOI: 10.5220/0008150400440047
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 44-47
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
Psoriasis is a chronic disease that can cause
various comorbidities physically, psychologically
and socially (WHO, 2016). Immunopathogenesis of
psoriasis involves Th1, Th17 and proinflammatory
lymphocytes such as tumor necrosis factor-alpha
(TNF-α), interferon-γ and interleukin-2 predisposing
factors to comorbidities such as arteriosclerosis, skin
disorders and metabolism, psoriasis arthritis,
malignancies and other autoimmune diseases (factor,
2017), (Mazlin, 2012), (Tsai, 2011).
Pradyumma et
all study on psoriasis patients in Europe in 2013 found
that psoriasis had some comorbidities such as
hypertension, diabetis militus, obesity, dyslipidemia,
heart disease, metabolic syndrome, cardiovascular
disease, psoriasis arthritis, crohn's disease, lung
disease, mental disorders and malignancies
(Bhandary, 2016).
Soorya et al also studied in
patients with psoriasis in India in 2017 and found
some skin comorbidities in these patients (Factor,
2017). Thus we investigated the relation of
comorbidities with psoriasis in patients who visited
dermatovenerology outpatient clinic of Dr. Moewardi
General Hospital Surakarta in period
of January
2013-December 2017.
2 METHODS AND RESULTS
This Cross sectional study was performed in psoriasis
patients visited of dermatovenerology outpatient
clinic of Dr. Moewardi Hospital Surakarta during
January 2013-December 2017. The data were taken
from medical record data of patients. The data were
then analyzed with SPSS and Chi-Square test, with
the significant value of P<0.05.
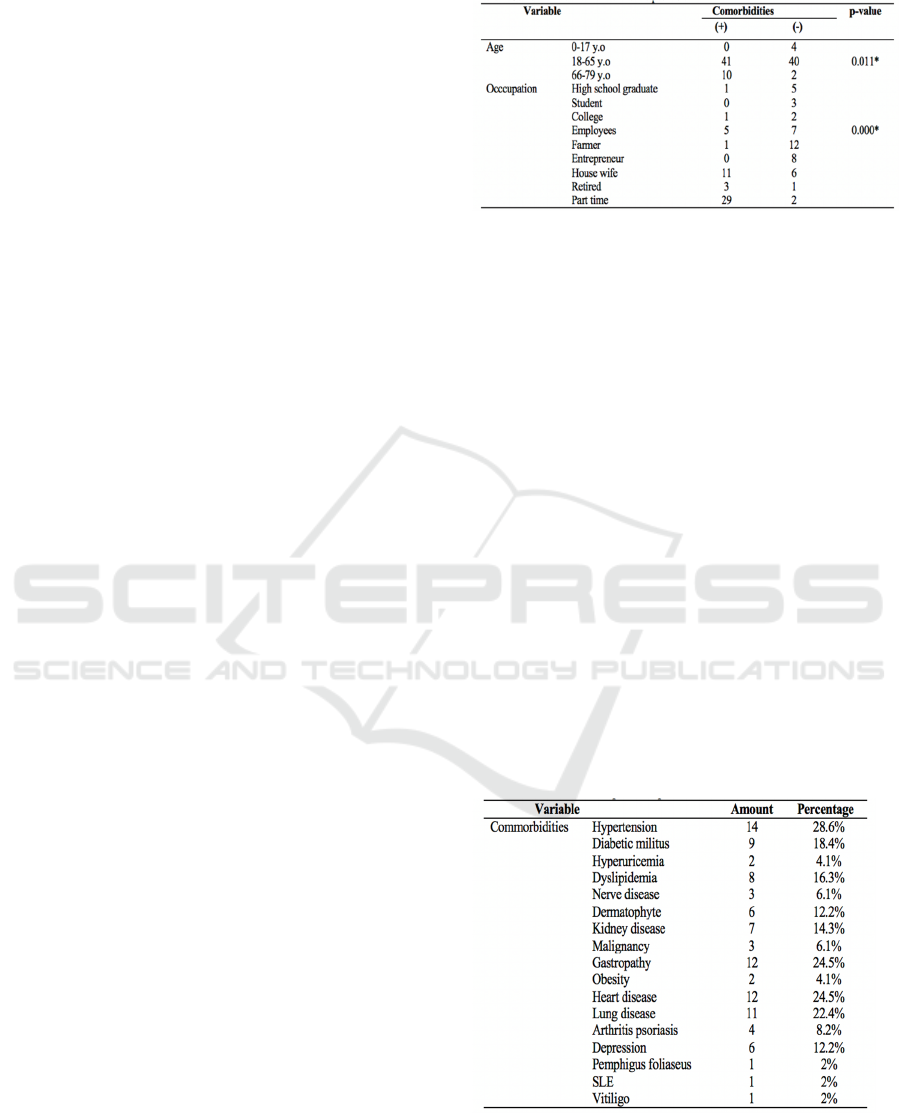
The study sample of these subject the age ranged
from 0-17 years, 18-65 years, 66-79 years were 4.1%,
83.5% and 12.4% respectively. Males were more
dominant than females (52.6% vs 47.4%). The study
subjects were comprised of part time (31.9%). All
psoriasis patients in our study had been suffering
from this disease for more than 3 months. Psoriasis
area and severity index score revealed mild (26.8%),
medium (52.6%) and severe (20.6%). The most
common comorbidity was hypertension (28.6%),
followed by heart disease (24.5%), gastropathy
(24.5%) and lung disease (22.5%).(Table 1).
Table 1. Comorbidities of psoriasis patients
Chi-Square test showed that age and occupation are
significantly relation with all commorbidities with
value of P=0.011 and P=0.011.
3 DISCUSSION
Psoriasis is a skin disease of the erythrosquamous
dermatoses, characterized by autoimmune and
chronic residif with typical are macula erythema,
covered by thick, layered squama and clear white as
mica, accompanied by droplets of wax phenomenon
and an Auspitz sign. Psoriasis can occur at any age
but rarely in the age of under 10 years old, usually
appears at the age of 15-35 years (Johan, 2012),
(WHO, 2016). In our study it appeared at the age of
18-65 years old. It is consistent with previous study
by Alexander et all, in which the dominant age in
psoriasis is in the second and third decades (Egeberg,
2017). This probably due to the onset of this disease
is at the age of 15-35 years old and the disease tends
to be residual and lasts for a lifetime (WHO, 2016).
Table 2. Comorbidities and their relation to psoriasis
According to the National Health Council the
definition of chronic disease is a disease lasts more
than 3 months (National Health Council, 2014). This
study found that all respondents (100%) suffered for
The Relation of Comorbidities with Psoriasis Patients Treated in Ermatovenereology Outpatient Clinic of Dr. Moewardi General Hospital
Surakarta January 2013-December 2017
45

more than 3 months. This is because psoriasis is a
long-term chronic disease (WHO, 2016).
Psoriasis may occur in both men and women, but
more likely in men (WHO, 2016). This study found
that the number of male respondents were more
dominant. Similar results were also reported by Tsen-
Fang Tsai et al. that psoriasis sufferers were more
common in men than women (Ogdie, 2013). These
conditions are not due to phenotypic differences but
because men were more frequently exposed to
precipitating factors due to their physical activity
(Johan, 2012;WHO, 2016;Griffits, 2010).
The most common clinical variant of psoriasis is
the type of vulgaris psoriasis, which affects about
58%-97% of all patients with psoriasis (WHO, 2016).
The number of vulgaris psoriasis patients in this study
was 74.2% and it is the most common type of
psoriasis compared with other psoriasis types as
another previous study by Kurniasari et al. reported
that the most dominant type of psoriasis is psoriasis
vulgaris (Boham, 2016). However, to date there has
not been any study which definitively report the
reason for this type to be the most dominant. psoriasis
vulgaris (Boham, 2016). However, to date there has
not been any study which definitively report the
reason for this type to be the most dominant. Most of
psoriasis patients in our study are part timers with low
income. This finding is similar to that of study by
Carlson et all. Perhaps this is due to the patients
perception that psoriasis gives negative impact on
their life causing problems with work, daily activities
and socialization (Carlson, 2016).
In this study obtained PASI score of mild 26.8%,
moderate 52.6% and severe 20.6%. The severity of
the PASI score is associated with increased
comorbidity in patients, where comorbidity is
obtained primarily in patients with moderate to severe
(WHO, 2016). In this study, the majority of patients
had a moderate PASI score of 52.2% and the number
of psoriasis patients who had comorbidities 51.5%.
Research with similar results was previously reported
by Pradyumna et al (Bhandary, 2016). The condition
is presumed because the majority of respondents in
this study worked part timers/low income so the
ability of patients to seek medical attention also
decreased and caused less controlled the disease
(Carlson, 2016).
Psoriasis is a chronic disease that affects the nails,
skin and can cause various comorbidities physically,
psychologically and socially (WHO, 2016). This
study reported that 50.5% of these patients had
comorbidities of disease including hypertension
(28.6%), diabetic militus (20.4%), hyperuricemia
(4.1%), dyslipidemia (16.3%), nerve disease (6.1%),
dermatophyte (12.2%), kidney disease (14.3%),
malignancy (6.1%), gastropathy (24.5%), obesity
(4.1%), heart disease (26.5%), lung disease (22.4%),
arthritis psoriasis (10.2%), depression (12.2%), SLE
(4.1%) and vitiligo (2%). This is similar with
previous study by Bergamo et all and Howa yeung et
all (Factor, 2017), (Rota, 2010). The comorbidities in
psoriasis are due to psoriasis is an immune disease
involving Th1, Th17 and proinflammatory
lymphocytes suspected to be predisposing factors for
various comorbidities including arteriosclerosis, skin
disorders and metabolism as well as trigger the
emergence of symptoms of other autoimmune
diseases (Factor, 2017;Mazlin, 2016;Tsai, 2011). In
this chronic disease where the increase of T cell
activation, both Th1 and Th17 cells to produce
proinflammatory cytokines. These inflammatory
cells can affect the function of cells, other tissues and
trigger the comorbidities (Factor, 2017;Mazlin,
2016;Tsai, 2011).
Our study revealed that age and occupation are
related to comorbidities occured in psoriasis patients.
The older the age the greater the momorbidity affect
psoriasis patients. This is similar to previous study by
Pradyumna et all. who reported that the older the age
the greater the momorbidity affect psoriasis patients
(Bhandary, 2016). While the relation between
occupation status and comorbidities is also similar
with study by Carlson et all. It is due to the patients
perception that psoriasis gives negative impact on
their life causing problems with work, daily activities
socialization and that economic level the majority in
low treatment (Carlson, 2016).
4 CONCLUSION
There is a relation between comorbidity with
psoriasis particularly age and occupation. The older
the psoriasis sufferer the greater the comorbidities,
and the lower the income, the greater the
comorbidities too. Thus routine screening is required
in patients with psoriasis and need cooperation with
other clinical divisions is necessary to prevent and
manage accompany it.
REFERENCES
Bhandary, P. R., Sanath, P. K., Shetty, N. J., Girish, P. N.,
& Lathika, K. Clinico-epidemiological study of
Psoriasis and associated co-morbidities. IAIM, 3(3), pp.
116-122.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
46

Boham, M.P., & Suling, P., 2016. Profil Psoriasis
diPoliklinik Kulit dan Kelamin RSUP Prof. Dr. R. D.
Kandou Manado 2013-2015. Jurnal e-clinic, (4), pp. 1-
6.
Bożek, A, A., & Reich, A, A., 2017. The reliability of three
psoriasis assessment tools: Psoriasis area and severity
index, body surface area and physician global
assessment. Advances in clinical and experimental
medicine: official organ Wroclaw Medical
University, 26(5), pp. 851-856.
Carlson, A., 2016. Interventions to improve quality of life
for patients with psoriasis and psoriatic arthritis. Drug
topics, 1, pp. 51-63.
Egeberg, A., Skov, L., Gislason, G. H., Thyssen, J. P., &
Mallbris, L., 2017. Incidence and prevalence of
psoriasis in denmark. Acta dermato-
venereologica, 97(6-7), pp. 808-812.
Factor, S.I., Baskaran, S., Thomas, J., Sneha, K., 2017. A
study on dermatological comorbidities in psoriasis.
World Journal Pharmacology Research, 3(9), pp. 157–
159.
Griffits, C., Barker, J., 2010. Psoriasis. Dalam: Rook’s
Textsbook of Dermatology.edisi ke 8. Inggris: Willey-
Blackwell, p. 1-60
Johan, E. Gudjonsson., & James, T. Elder., 2012.
Psoriasis. Dalam: Goldsmith LA, Katz SI, Gilchrest
BA, dkk. editors. Fitzpatrick's Dermatology in General
Medicine. Edisi ke-8. New York: McGraw Hill, pp.
197-222.
Mazlin, M. B., Chang, C. C., & Baba, R., 2012.
Comorbidities associated with psoriasis-data from the
malaysian psoriasis registry. The Medical journal of
Malaysia, 67(5), pp. 518-521.
National Health Council., 2014. About chronic disease.
h.10–1. Tersedia pada :
www.nationalhealthcouncil.org.
Ogdie, A., Margolis, D.J., Shin, D.B., Attor, R., Troxel,
A.B., Gelfand, J.M., 2013. Psoriasis Severity and the
Prevalence of Major Medical Comorbidity A
Population-Based Study. Journal of American
Medicine Association, 19104(10), pp. 1173–1179.
Putra, E. W., & Dharmawan, N., 2017. Profile of psoriasis
patients in patients who visited dermatovenerology
outpatient clinic of Dr. Moewardi General Hospital
Surakarta Januari 2012-desember 2016, pp. 1-8.
unpublissed.
Rota, O.M., Riuniti, O., Raffaele, S.S., 2010.
Epidemiology of comorbidities. Dermatology Therapy,
23, pp. 114–118.
Tsai, T. F., Wang, T. S., Hung, S. T., Phiona, I., Tsai, C.,
Schenkel, B., ... & Tang, C. H., 2011. Epidemiology
and comorbidities of psoriasis patients in a national
database in Taiwan. Journal of dermatological
science, 63(1), pp. 40-46.
World Health Organization., 2016. Global Report on
Psoriasis. h.1-8.
The Relation of Comorbidities with Psoriasis Patients Treated in Ermatovenereology Outpatient Clinic of Dr. Moewardi General Hospital
Surakarta January 2013-December 2017
47
