
The Effect of Macrophage Addition to Interleukin 10 (IL-10) in
Tuberculosis Granuloma Model In Vitro
Dini Puspodewi
1,2,3
, Agung Dwi Wahyu W
3
and Jusak Nugraha
4
1
Post Graduate Student of Master of Immunology, Faculty of Pasca Sarjana, Universitas Airlangga,Indonesia
2
Department of Stem Cell Institute of Tropical Disease, Universitas Airlangga, Indonesia
3
Department of Microbiology Clinic, Faculty of Medicine, Dr. Soetomo Hospital, Indonesia
4
Department of Patology Clinic, Faculty of Medicine, Dr.Soetomo Hospital, Indonesia
Keywords: Mycobacterium tuberculosis, Granuloma, IL-10
Abstract: Tuberculosis (TB) caused by the bacterium Mycobacterium tuberculosis has caused more deaths than other
infectious diseases over the past 200 years. Granulomas are characteristic of mycobacterial infection.
Doubling of Mycobacterium tuberculosis bacilli in any place will cause specific inflammation to form
characteristic granulomas. Granulomas contains of different types of cells, but the main cellular component
of the structure is macrophages. Macrophages are cells for the formation of granulomas and major cell types
in most granulomas. One function of macrophages in granulomas is the production of anti-inflammatory
cytokines IL-10. IL-10 can reduce inflammation and maintain homeostasis. This study aims to determine
the effect of the addition of macrophages to levels of interleukin-10 (IL-10) in granuloma model in vitro.
This type of research is true experimental with the object of research in the form of PBMC which comes
from 1 healthy volunteer. Analysis using twoway ANNOVA with P <0.05, and tukey comparing for
comparison. The results showed that without macrophage group with 1x10
5
, 2x10
5
, and 3x10
5
macrophage
groups, the value of p = 0.3197 was greater than 0.05 (p> 0.05), so there was no significant difference.
While the variation day in the treatment group obtained p = 0.2407 which showed no effect of macrophage
addition to interleukin-10 (IL-10) level on granuloma model in vitro, with IL-10 concentration on the 1
st
day
until the 5
th
day are low. There is no effect of adding macrophages to IL-10 levels in tuberculosis granuloma
models in vitro.
1 INTRODUCTION
Tuberculosis (TB) has caused more deaths compared
to other infectious diseases over the past 200 years
(Heemskerk et al., 2015). This disease is caused by
Mycobacterium tuberculosis mostly attacks people
living in low-income and middle-income countries
where it reaches 9.4 million people a year
worldwide. Most individuals who are exposed do
not develop the disease because it can produce an
immune response to resist or eliminate bacteria (Fox
and Menzies, 2013).
Tuberculosis granuloma is a hallmark of
mycobacterial infection (Heemskerk et al., 2015).
Characteristic granuloma formation originates from
the presence of specific inflammation caused by
multiplication of Mycobacterium tuberculosis bacilli
in any place (Elorriaga et al., 2015). Granulomas
have a dynamic process in which the structure of the
size will increase as more cells move in (Orme and
Basaraba, 2014).
Mycobacterium tuberculosis infection causes
granuloma formation where bacteria enter in an
inactive state and can live for decades before
reactivation to develop active disease when the
host's immune system is weakened (Kapoor et al.,
2013). Bacteria will become latent when trapped in
granulomas and are under hypoxic conditions, lack
of nutrition, and pressure from adaptive immunity
(Orme and Basaraba, 2014). A person infected with
latent TB can store a small amount of inactive
Mycobacterium tuberculosis bacilli contained in
microgranuloma. This organism can continue to live
but is not active (Kapoor et al., 2013).
IL-10 is called an anti-inflammatory cytokine, an
inhibiting cytokine for a balance between
inflammatory and immunopathological responses
(Cyktor et al., 2013). IL-10 plays an important role
386
Puspodewi, D., W, A. and Nugraha, J.
The Effect of Macrophage Addition to Interleukin 10 (IL-10) in Tuberculosis Granuloma Model In Vitro.
DOI: 10.5220/0007543503860391
In Proceedings of the 2nd International Conference Postgraduate School (ICPS 2018), pages 386-391
ISBN: 978-989-758-348-3
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

in Mtb infection, where cytokines have been shown
to reduce immunity (Cavalcanti et al., 2012; Cyktor
et al., 2013; Adrian et al., 2015).Immunosuppressive
cytokines IL-10 have been associated with
susceptibility to TB in both humans and animals
(Cyktor et al., 2013). IL-10 plays an early inhibitory
role in preventing the development of protective
immunity associated with the containment of Mtb
infection (Cyktor et al., 2013).
This study aims to detect whether there is an
effect of the addition of macrophages on IL-10
levels in tuberculosis granuloma models in vitro.
2 MATERIALS AND METHODES
2.1 RPMI
The growth media used in this study was the
Roswell Park Memorial Institute (RPMI) 1640
which was obtained already in the form of ready-to-
use solution. RPMI 1640 media is a medium used
for cell and tissue culture, usually used for the
growth of human lymphoid cells. This medium
contains a large amount of phosphate and is
formulated for use in air with a 5% CO
2
atmosphere.
RPMI 1640 uses the bicarbonate buffer system so
that it enables the growth of several types of cells,
especially T lymphocytes, hybridomas. There are
several series of RPMI most often used is RPMI
1640.
2.2 PBMCs
Peripheral Blood Mononuclear Cells = PBMCs are
cells made from human blood which are then
processed for the PBMC cell capture. Sample
criteria are adult blood, the blood used should be
new blood taken, it can not be blood that has been
stored for too long, blood comes from healthy
people and does not suffer from tuberculosis
infection, there is no specific provision for sex either
male or female. Suggestions from the blood
researcher used should come from one person only,
because the immune response of each individual is
different so if coming from more than one person in
worry affects the outcome. The number of PBMC
used in this study was 10
5
in each well.
2.3 Mycobacterium tuberculosis
This study used bacterial isolates Mycobacterium
tuberculosis H37Rv obtained from the Laboratory of
Microbiology, Institute of Tropical Disease,
Airlangga University Surabaya with concentration
10
5
in each well.
2.4 Macrophage
Taken buffy-coat about 60 ml. Then prepare 50 ml
conical tubes with histopags each 15 ml. Prepared
one tube every 10 ml of buffy-coat. Histopags are
used at room temperature. Plate at 10 cm culture
dishes (10 ml / dish) incubated at 1-2 hours at 37ºC
5% CO
2
. Observe macrophage cells under a
microscope and then make doses 1,2 and 3x10
5
.
2.5 Procedure
There are four groups on this procedure. Group I
was given PBMC and Mycobacterium tuberculosis
bacteria on RPMI media as control. Group II was
given PBMC, Mycobacterium tuberculosis and
1x10
5
macrophages on RPMI media. Group III was
given PBMC, Mycobacterium tuberculosis and
2x10
5
macrophages on RPMI media. Group IV was
given PBMC, Mycobacterium tuberculosis and
3x10
5
macrophages on RPMI media. Prepared well
plates that already contain RPMI media. Enter
1x10
5
PBMC cells into all wells. Inoculated with
1x10
5
M. tuberculosis strain H37Rv bacterial
isolates into all wells. Added macrophages as much
as 1x10
5
, 2x10
5
and 3x10
5
cells into each well of
group II, III, and IV. Plate was incubated at 37°C
with 5% CO
2
condition. Observed on days 1,2, 3, 4
and 5. Every day 100 uL of supernatant was taken
to test IL-10 levels using the ELISA test at 450 nm
wavelength.
3 RESULTS
3.1
Direct Granuloma Observation
Results from observations under an inverted
microscope with 400x magnification of PBMC
samples from 1 healthy volunteer were added with
1x10
5
, 2x10
5
, 3x10
5
and Mtb macrophages showing
the difference from day one to fifth day. On the first
day there has not been a good aggregate on culture
without macrophages with a culture plus
macrophages (Figure 1). The second day has already
begun to form aggregate on both treatments i.e.,
without the addition of macrophages and the added
macrophages (Figure 2). On the third day (Figure 3)
and the fourth day (Figure 4) is still aggregate, while
on the fifth day the aggregate has begun to decrease
(Figure 5).
The Effect of Macrophage Addition to Interleukin 10 (IL-10) in Tuberculosis Granuloma Model In Vitro
387
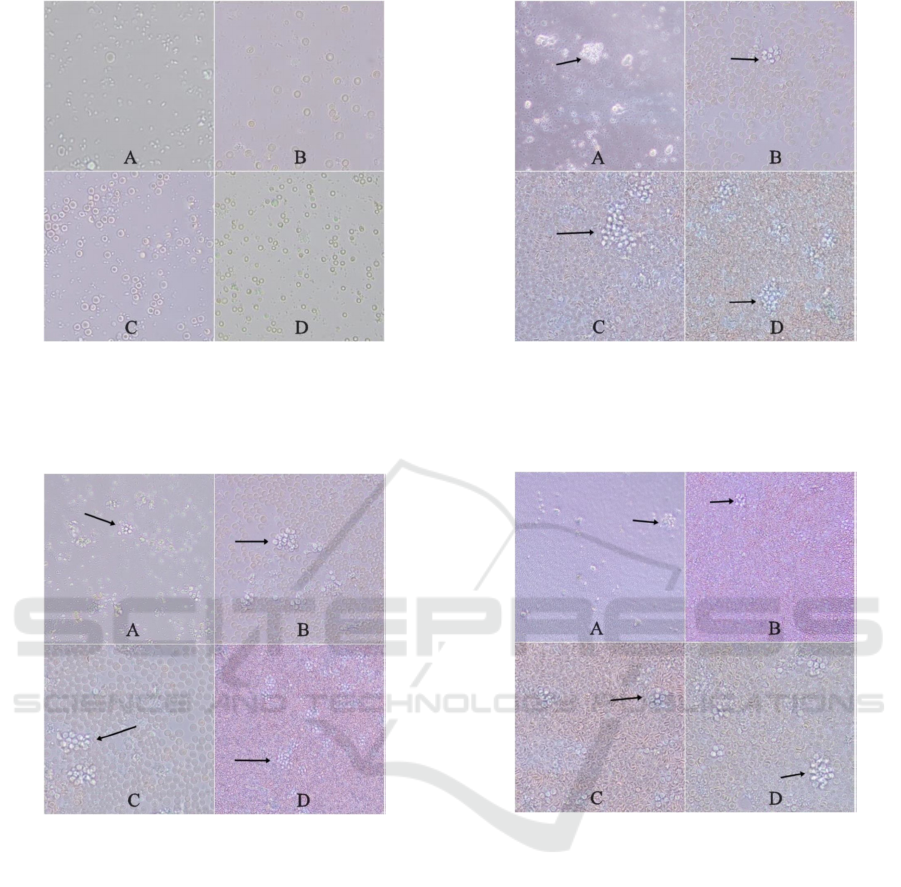
Figure 1. First Day Culture. A. Without Macrophages, B.
Addition of macrophages 1x10
5
,
C. Addition of macrophages 2x10
5
, D. Addition of
macrophages 3x10
5
.
Figure 2. Culture Second day. A. Without Macrophages,
B. Addition of macrophages 1x10
5
,
C. Addition of macrophages 2x10
5
, D. Addition of
macrophages 3x10
5
.
Figure 3. Third Day Culture. A. Without Macrophages, B.
Addition of macrophages 1x10
5
,
C. Addition of macrophages 2x10
5
, D. Addition of
macrophages 3x10
5
.
Figure 4. Fourth Day Culture. A. Without Macrophages,
B. Addition of macrophages 1x10
5
,
C. Addition of macrophages 2x10
5
, D. Addition of
macrophages 3x10
5
.
ICPS 2018 - 2nd International Conference Postgraduate School
388
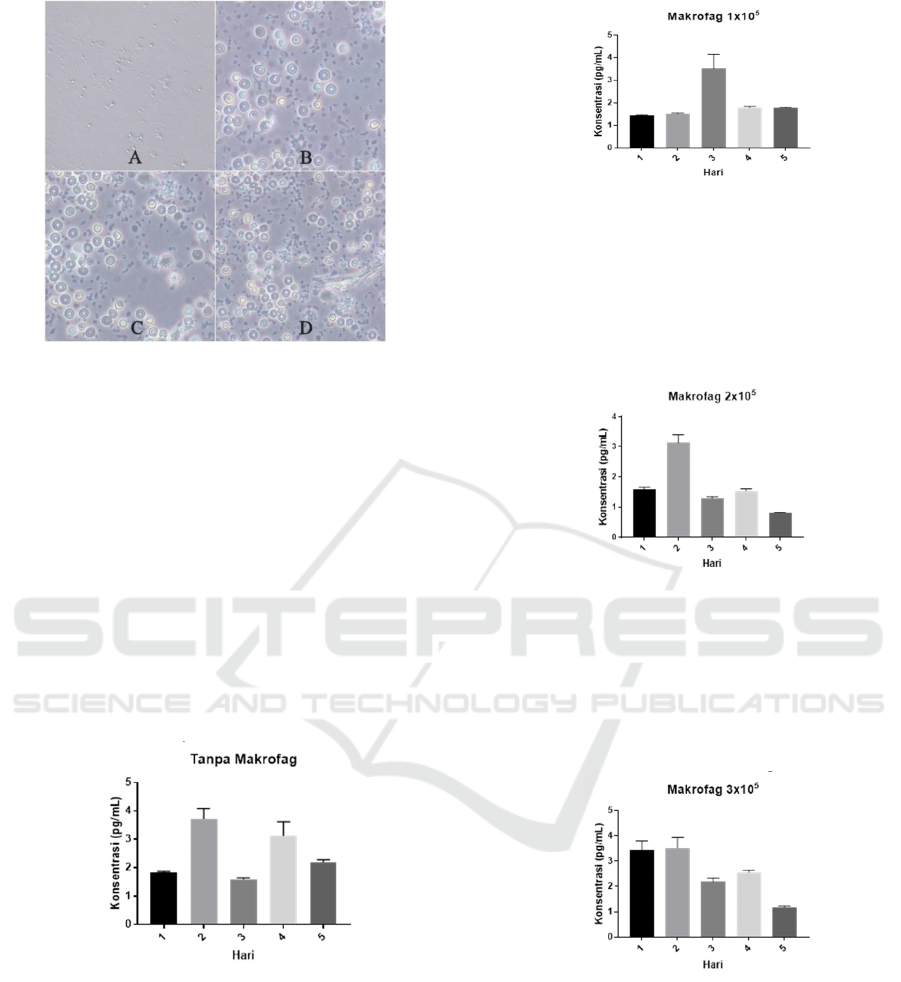
Figure 5. 5th Day Culture. A. Without Macrophages, B.
Addition of macrophages 1x10
5
,
C. Addition of macrophages 2x10
5
, D. Addition of
macrophages 3x10
5
.
3.2 Examination the levels of IL-10
Result of examination of level of IL-10 with elisa
method from 4 group that is without the addition of
macrophages, with the addition of 1x10
5
, 2x10
5
,
3x10
5
macrophages were analyzed by day variation.
From the research, it was found that the levels of
IL-10 without addition the highest value of
macrophages occurred on the 2nd day with an
average of 3,733 and the lowest average value
occurred on the 3rd day of 1,595 shown on figure 6.
Figure 6. Levels of IL-10 without the addition of
macrophages
The level of IL-10 with the addition of 1x10
5
macrophage the lowest value occurred on the 1st day
with an average of 1.435 and the highest average
value occurred on the 3rd day ie 3,506 shown in
Figure 7.
Figure 7. Levels of IL-10 with the addition of 1x10
5
macrophages
The level of IL-10 with the addition of 2x10
5
macrophage the highest value occurred on the 2nd
day with an average of 3.135 and the lowest average
value occurred on the 5th day that is 0.804 shown in
figure 8.
Figure 8. Levels of IL-10 with the addition of 2x10
5
macrophages
It was found that the level of IL-10 with the
addition of 3x105 macrophage of the lowest value
occurred on the 5th day with an average of 1,191
and the highest average value occurred on the
second day that is 3,521 shown in Figure 9.
Figure 9. Levels of IL-10 with the addition of 3x10
5
macrophages
The results of IL-10 examination with elisa
method of 4 groups, i.e., without the addition of
macrophages with the addition of macrophages
1x10
5
, 2x10
5
, 3x10
5
showed low levels of IL-10.
All groups experienced increased concentrations
on the second day. On the third day, the fourth and
fifth groups of 1x105 macrophages were different
from the other groups, i.e., the third and fifth day
The Effect of Macrophage Addition to Interleukin 10 (IL-10) in Tuberculosis Granuloma Model In Vitro
389

increases and the decrease on the fourth day, while
the group without macrophages, the 2x105 and
3x105 macrophages decreased the concentration on
the third and fifth days and increased the fourth day
(Figure 10).
Figure 10. IL-10 levels on day variations
The data obtained are then analyzed by two-way
ANOVA which aims to determine the significance
of the price of the proportion (p). In groups without
macrophages with a group of 1x105, 2x105, and
3x105 macrophages, the value p = 0.3197 was
greater than 0.05 (p> 0.05). Likewise with day
variations of groups without macrophages with
groups of macrophages added 1x105, 2x105, and
3x105 obtained value p = 0.2407 value is greater
than 0.05 (p> 0.05) so it shows no difference.
3.3 Discussion
Tuberculosis granuloma is a hallmark of
mycobacterial infection (Heemskerk et al., 2015).
Characteristic granuloma formation originates from
the presence of inflammation Specifically caused by
doubling the Mycobacterium tuberculosis bacilli in
any place (Elorriaga et al., 2015). Granuloma is a
pathological sign host response to Mycobacterium
tuberculosis infection. Development Granuloma is a
defense tool designed as a wall and contains
pathogens (Orme and Basaraba, 2014). Granuloma
formation facilitates host in accommodating
Mycobacterium tuberculosis bacilli and prevent
spread of bacteria, but can also be used by bacteria
for breed (Heemskerk et al., 2015). Granulomas
have a dynamic process because the more cells
move in, the size structure will increase (Orme and
Basaraba, 2014).
M. tuberculosis IL-10 is an immunoregulatory
cytokine with activity immunosuppressive is potent
against APC and Th1 cells. IL-10 production level
by Macrophages and dendritic cells are infected,
although promoted by Th1 ability, IL-10 is secreted
more by dendritic cells than macrophages. IFN-γ
decreases IL-10 production from macrophages
infected with M. tuberculosis. In this
microenvironment, IFN-γ secreted by activated T
cells can synergize with M. tuberculosis to reduce
IL-10 production (Hickman et al, 2002).
IL-10 is not always produced by T cells that
make other pro-inflammatory cytokines, although
checking granulomas in a small subset, there is a
small population of T cells (1.2%) that make IL-10
and IL-17. T cells with this phenotype have been
associated with control of several bacterial
infections rather than with autoimmune diseases
(Gideon et al., 2015).
4 CONCLUSIONS
There w no effect of adding macrophages to IL-10
levels in tuberculosis granuloma models in vitro.
ACKNOWLEDGEMENTS
The authors would like to thank the technicians of
the Stem cell Research Centre and Tuberculosis and
Leprosi Laboratory of Tropical Diseases (ITD) of
Airlangga University and all those who have assisted
in the completion of this research.
REFERENCES
Adrian, T. B. R., J. L. Montiel, G. Fernandez and A.
Valecillo. 2015. Role of Cytokines and other
Factors Involved in the Mycobacterium
tuberculosis infection. World Journal of
Immunology. 5(1): 16 – 50.
Cavalcanti, Y. V. N. M. C. A. Brelaz, J. K. D. A. L.
Neves, J. C. Ferraz and V. R. A. Pereira. 2012.
Role of TNF-alpha, IFN-gamma, and IL-10 in the
development of pulmonary tuberculosis.
Pulmonary Medicine 2012. doi:
10.1155/2012/745483.
Cyktor, J. C., B. Carruthers, R. A. Kominsky, G. L.
Beamer, P. Stromberg and J. Turner. 2013.
Interleukin-10 Inhibits Mature Fibrotic Granuloma
Formation During Mycobacterium Tuberculosis
Infection. The Journal of Immunology. 190: 2778
– 2790.
Elorriaga, G. G. et al. 2015. Practical and Laboratory
Diagnosis of Tuberculosis From Sputum Smear to
Molecular Biology. Springer, Switzerland. Doi
10.1007/978-3-319-20478-9_1.
Fox, G. J. and D. Menzies. 2013. The New Paradigm of
Immunity to Tuberculosis. Advances in
Experimental Medicine and Biology 783.
Springer, New York.
Gideon, H. P., J. Y. Phuah, A. J. Myers, B. D. Bryson, M.
A. Rodgers, M. T. Coleman, P. Maiello, T.
ICPS 2018 - 2nd International Conference Postgraduate School
390

Rutledge, S. Marino, S. M. Fortune, D. E.
Kirschner, P. L. Lin and J. L. Flynn. 2015.
Variability in Tuberculosis Granuloma T Cell
Responses Exists, but a Balance of Pro- and
Antiinflammatory Cytokines Is Associated with
Sterilization. PLOS Pathogens.
doi:10.1371/journal.ppat.1004603.
Heemskerk, D. et al. 2015. Tuberculosis in Adults and
Children, Tuberculosis in Adults and Children.
doi: 10.1007/978-3-319-19132-4.
Hickman, S. P., J. Chan and P. Salgame. 2002.
Mycobacterium tuberculosis Induces Differential
Cytokine Production from Dendritic Cells and
Macrophages with Divergent Effects on Naive T
Cell Polarization. Journal of Immunology. 168:
4636 – 4642.
Kapoor, N., S. Pawar, T. D. Sirakova, C. Deb, W. L.
Warren and P. E. Kolattukudy. 2013. Human
Granuloma In Vitro Model, for TB Dormancy and
Resuscitation. Plos one. 8(1).
Orme, I. M. and R. J. Basaraba. 2014. The formation of
the granuloma in tuberculosis infection. Seminars
in Immunology 26: 601 – 609.
The Effect of Macrophage Addition to Interleukin 10 (IL-10) in Tuberculosis Granuloma Model In Vitro
391
