
Factors Affecting Healthcare Costs in Indonesia: What the Hospitals
and Doctors Said
Noorlailie Soewarno and Bambang Tjahjadi
Department of Accounting, Universitas Airlangga, Surabaya, Indonesia
noorlailie@gmail.com, bambang.tjahjadi@feb.unair.ac.id
Keywords:
Business Ethic, Good Governance, Healthcare Providers, Strategic Cost-Driversa.
Abstract: This study focuses on exploring and identifying the cost drivers behind healthcare cost in Indonesia, and
particularly the role of the healthcare provider.
A value chain analysis is used to identify strategic
activities, strategic cost-drivers, and the behavior of hospitals and doctors. This study uses an exploratory
case-study method, particularly focusing on the contribution of healthcare providers to the expensive cost
of healthcare in Indonesia. Both secondary data and primary data have been used in this study. The main
contribution of this study is to highlight strategic cost-drivers as well as business ethics and governance
issues. This study demonstrates important findings relating to high hospital costs and the high cost of
doctors.
1 INTRODUCTION
Healthcare has become a main concern of every
nation in the world. To be healthy, everyone needs
affordable healthcare. Compared to the OECD
standard healthcare costs, which stand at 12% of
GDP (Lock, 2013), the average healthcare cost in
most ASEAN countries is still low (below 4%). In
Indonesia, healthcare is the second-most important
issue after education. Healthcare costs in Indonesia
are also small compared to other ASEAN countries,
standing at around 3% of GDP in 2013. This is the
smallest percentage compared to Malaysia (3.9%),
Thailand (3.9%), Philippines (4.6%) and Singapore
(4.7%).
Health is a very important aspect with which to
determine a nation’s productivity. People with good
health (both physically and spiritually) are able to
contribute to Indonesia’s productivity. In order to
provide good-quality, cheap, and evenly distributed
healthcare services, the government (as a regulator)
and all of the healthcare provider players must come
up with an affordable and efficient healthcare
service. The main players in the healthcare industry
consist of: (1) healthcare providers (hospitals,
laboratories and pharmacies); (2) healthcare
professionals (doctors and other medical services);
(3) pharmaceutical companies; (4) suppliers of
healthcare facilities and infrastructure; (5) insurance
providers (both government and private) and (6) the
government as the regulator of healthcare facilities
and infrastructure. Unfortunately, current healthcare
costs are still high, and therefore not every citizen is
able to have access to proper healthcare services.
The contribution this study makes is to provide
strategic information about the strategic cost-drivers
causing healthcare cost inefficiencies from the
perspective of hospitals and doctors as healthcare
providers in Indonesia.
This study also contributes to the field of
management and accounting. It confirms how
agency theory describes the importance of a
congruent relationship between the principal (the
community) and agents (players in the healthcare
industry). Agents should act in accordance with the
expectations of the principal. Otherwise, the agents
may incur costs that harm the principal.
The practical benefit of this study is to clearly
illustrate the unique pattern in the relationship
between the players in the healthcare industry;
especially that of the healthcare providers (hospitals
and doctors) with the Indonesian community.
330
Soewarno, N. and Tjahjadi, B.
Factors Affecting Healthcare Costs in Indonesia: What the Hospitals and Doctors Said.
In Proceedings of the Journal of Contemporary Accounting and Economics Symposium 2018 on Special Session for Indonesian Study (JCAE 2018) - Contemporary Accounting Studies in
Indonesia, pages 330-337
ISBN: 978-989-758-339-1
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

2 LITERATURE REVIEW
2.1 Agency Theory and Good
Governance
Agency theory, proposed by Jensen and Meckling
(1976), refers to the relationship between agent and
principal. An agent is a party who does not have
resources but who has the skills to manage those
resources, while the principal is the party who has
resources but who submits the management of those
resources to the agent. The relationship between
agent and principal is called the agency relationship.
The relationship between agent and principal
does not always go well. In many cases, there are
problems or conflict between the two parties. The
conflict is mostly due to differences in objectives.
What the agent wants is sometimes incompatible
with what the principal wants. Conflict is also driven
by different views of risk; as a result, the actions
taken by each party also differ. The cost of this
conflict is called agency cost, which includes all
monitoring costs, bonding costs and residual loss
(Fama & Jensen, 1983).
Agency theory is the foundation of the need for
good corporate governance in modern organizations
(Keasey & Wright, 1993). In the healthcare industry
there are a variety of relationship patterns that can be
viewed from the perspective of agency theory. In
macro terms, the relationship between the
community as the owner of resources (the principal)
and the managers of healthcare resources (the agent)
is clearly an agency relationship. Distorted behavior
by agents in the healthcare industry clearly creates a
loss (agency costs) to society as the principal. This is
the time when good governance is needed within
healthcare management.
2.2 Strategic Cost-Drivers
Value-chain management plays a strategic role in
creating a competitive advantage. Value-chain
analysis provides management with strategic
information regarding the sources of cost leadership
or differentiation. Furthermore, managers need to
know what factors are driving costs in each strategic
activity. Riley states that cost drivers can be divided
into two categories, namely: (1) structural cost-
drivers, and (2) executional cost-drivers.
Structural cost-drivers are those cost drivers that
are associated with economic structure, including:
(1) scale, (2) scope, (3) experience, (4) technology,
and (5) complexity. Executive cost-drivers are
associated with factors affecting the organization’s
ability to execute a strategy, including: (1)
workforce involvement, (2) total quality
management, (3) capacity utilization, (4) plant
layout efficiency, (5) product configuration, and (6)
linkage exploitations (Shank & Govindarajan, 1993).
3 RESEARCH METHODS
3.1 Design of the Study
This study is designed as a qualitative case-
study. The unit of analysis is the cost of healthcare
in Indonesia. The informants in this study are actors
in the healthcare industry, namely: (1) doctors, and
(2) hospital directors. Because this study is
exploratory in nature, no proposition has been
formulated. Primary data is obtained by conducting
in-depth interviews and secondary data is generated
from the internet. The macro healthcare cost is
reviewed from the perspective of the relationship
pattern between actors or players in the healthcare
industry and an analysis of how this relationship can
trigger healthcare costs. Each pattern within the
relationship between players is explored using
theories that have been previously discussed.
3.2 Research Questions
This study focuses on the relationship between the
pharmaceutical industry and healthcare providers in
Indonesia, as expressed in the following research
questions:
(1) Are healthcare costs in Indonesia inefficient?
(2) What are the factors and strategic drivers
affecting healthcare costs in Indonesia, especially
those that come within the scope of doctors and
hospitals in their role as healthcare providers?
3.3 Analysis Technique
The analysis techniques used in this study include
data reduction, data presentation, data analysis,
conclusion and verification, as stated by Miles and
Huberman (1992) and Neumann (2006). The results
of this study are expected to produce
recommendations for policymakers in regards to
healthcare management in Indonesia.
3.4 Data collection
Data was collected from two main sources, namely:
(1) informants, and (2) archival data. The informants
of this study have more than 10 years of experience
Factors Affecting Healthcare Costs in Indonesia: What the Hospitals and Doctors Said
331
in their fields; as such, they were considered to have
sufficient knowledge to provide information about
the main issues of the study. Archival data was also
obtained from documents originating from both print
and online media. The data was analyzed and
summarized in order to address the major research
issues.
4 RESULTS AND DISCUSSIONS
4.1 Research Question 1: Are Healthcare
Costs in Indonesia Inefficient?
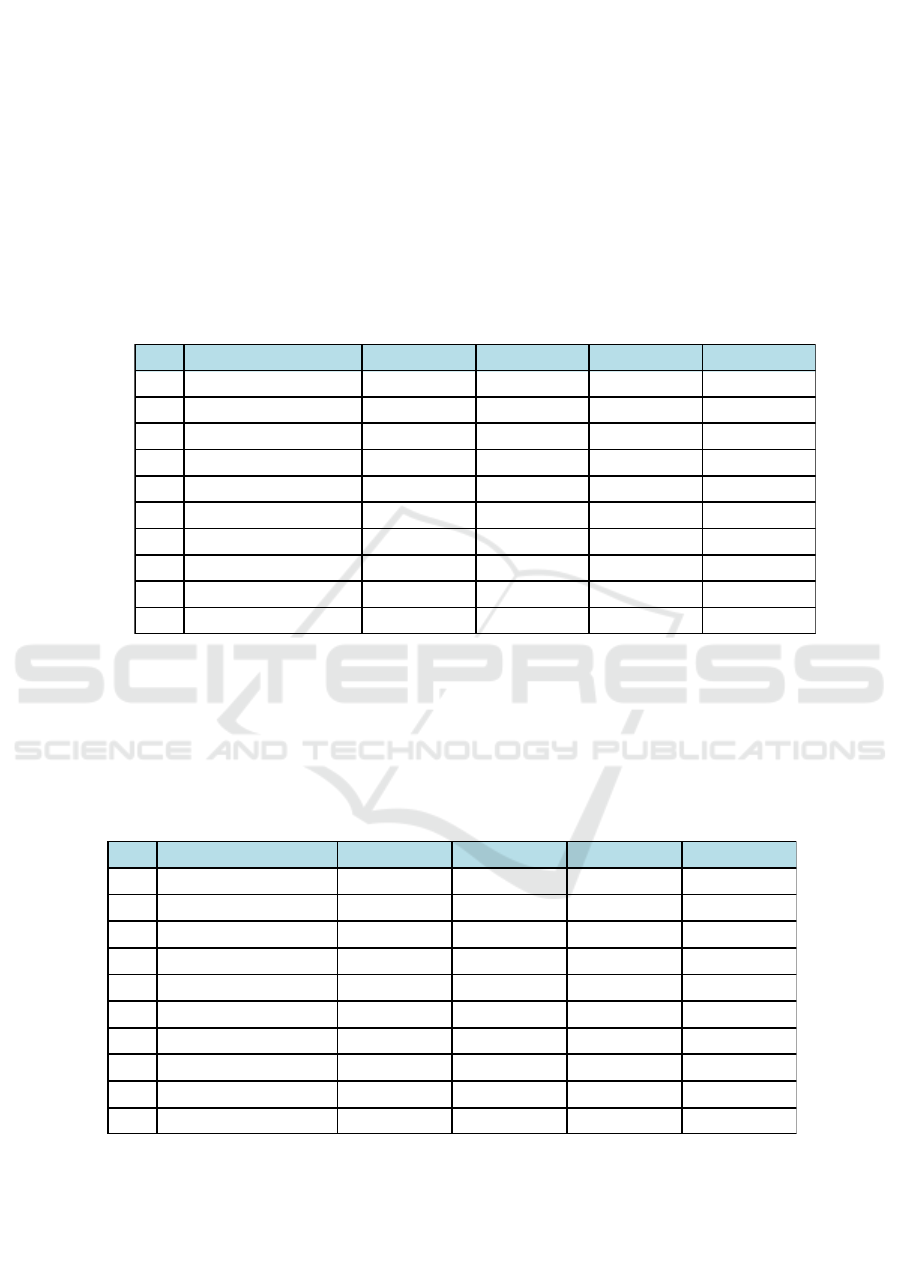
The World Bank data in Table 1 shows that the
healthcare costs per capita in Asia from 2011 to
2013 vary significantly by country. Singapore leads
in the first position, while Indonesia’s spending is
stagnant and, by 2012, is only higher than India’s
Table 1: Healthcare Cost per Capita (USD) in Asia
Source: The World Bank.
The World Bank data in Table 2 shows that the
percentage of healthcare costs in relation to GDP in
Asia from 2011 to 2013 also varies significantly.
Korea leads in the first position, while Indonesia is
also stagnant at around 2.9 percent of GDP.
Table 2: Healthcare Costs in Asia as a percentage of GDP (%)
Source: The World Bank.
According to the Indonesian Central Bureau of
Statistics, the average monthly spending on
healthcare costs per capita in Indonesia is 27,777
rupiahs for urban citizens and 14,895 rupiahs for
rural citizens (or an average of 21,392 rupiahs per
capita per month for both urban and rural). This
No. Country 2011 2012 2013 2014
1 BruneiDarussalam 2.2 2.3 2.6 2.6
2 China 5 5.3 5.4 5.5
3
India 4.3 4.4 4.5 4.7
4 Indonesia 2.7 2.9 2.9 2.8
5 Malaysia 3.9 4 4 4.2
6 Philippines 4.3 4.5 4.6 4.7
7 Singapore 3.9 4.2 4.5 4.9
8 Korea,Rep 6.8 7 7.2 7.4
9 Thailand 4.1 4.2 4 4.1
10 Vietnam 6.2 7 7.2 7.1
No. Country 2011 2012 2013 2014
1 BruneiDarussalam 938.5 961.9 1,022.90 957.6
2 China 279.5 328.7 375.1 419.7
3
India 65.7 64.9 68.5 75
4 Indonesia 99 107.2 106 99.4
5 Malaysia 393.7 421.5 427 455.8
6 Philippines 101.8 116.2 127.1 135.2
7 Singapore 2,086.10 2,310.40 2,531.50 2,752.30
8 Korea,Rep 1,650.50 1,714.90 1,870.10 2,060.20
9 Thailand 212.9 227.2 229.9 227.5
10 Vietnam 94.1 120.1 134.3 142.4
JCAE Symposium 2018 – Journal of Contemporary Accounting and Economics Symposium 2018 on Special Session for Indonesian Study
332
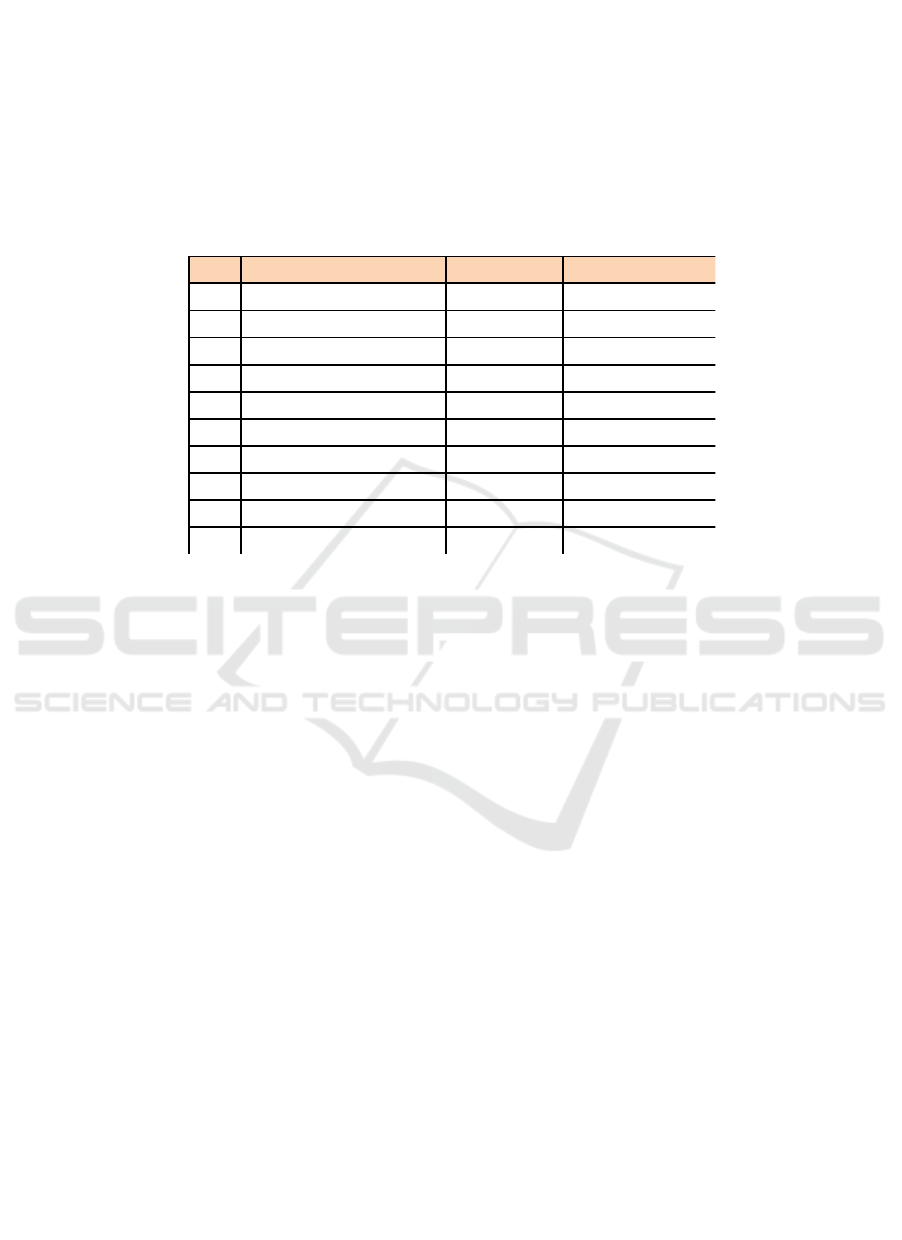
figure is considered to be low in the field of
healthcare spending.
Table 3 shows the result of a study conducted by
Tandon et al. (2000). It shows Indonesia’s position
in terms of healthcare efficiency. Indonesia ranks
92nd of 191 countries. Compared to other ASEAN
countries (Singapore, Brunei Darussalam, Thailand,
Malaysia and Philippines), Indonesia ranks 6th with
an efficiency score of 0.66 (score 1 = more
efficient). This means that the management of
healthcare in Indonesia is still inefficient. The best
healthcare management is found in Singapore. In
addition, Bloomberg has released information about
50 countries with the best health management costs
in the world, and Indonesia is not included.
Table 3: Healthcare Efficiency Score 2000
Source: World Health Organization.
From the previous discussions, it can be
concluded that healthcare costs in Indonesia are still
inefficient. Various factors may trigger good or bad
performance within healthcare management in
Indonesia. Those factors are interconnected in a
complex way and include both macro- and micro-
environment factors.
The influence of the macro environment on
healthcare costs in Indonesia may include political,
economic, socio-cultural, technological,
environmental, and legal environments. The
influence of the micro environment may relate to the
parties operating in the healthcare industry in
Indonesia and may include factors such as
management expertise, the standard of equipment,
utilization of information and communication
technology, human resources, leadership,
organizational culture, and others.
4.2 Research Question 2: What are the
factors and strategic drivers
affecting healthcare costs in
Indonesia, especially those that
come within the scope of doctors
and hospitals in their role as
healthcare providers?
4.2.1 The Role of the Hospital
The high healthcare costs in Indonesia are also
contributed to by hospitals. The cost of
inefficiencies in hospitals are contributed to by both
external and internal factors, as follows.
4.2.1.1 Marketing fees
Medicine is a high-cost component in a hospital,
especially patent medicines. Marketing costs are an
external factor that makes patent medicines so
expensive. One informant stated that:
“The cost of medicine includes
swallowed medicine and injected medical
materials, such as infusions, and other
disposable materials, such as gloves, etc.
Patent medicine is so expensive because
of high marketing costs (promotions) and
No.
Country Rank EfficiencyScore
1 Singapore 6 0.973
2 BruneiDarussalam 40 0.829
3 Thailand 47 0.807
4 Malaysia 49 0.802
5 RepublicofKorea 58 0.759
6 Philippines 60 0.755
7 Indonesia 92 0.66
8 India 112 0.617
9
China 144 0.485
10 VietNam 160 0.393
Factors Affecting Healthcare Costs in Indonesia: What the Hospitals and Doctors Said
333

R&D costs. If a patent has expired, a
medicine turns into a generic product and
its price will be cheaper. Producers should
be efficient in internal business processes
and in their business relationships with
doctors. The production cost for
manufacturers is around 30%, while the
remaining 70% of costs are promotional
costs. Meanwhile discounts for hospitals
are only about 20%."
4.2.1.2 Excessive Inventory
Inventory is costly, and excessive inventory is even
more costly. At the end, these inventory costs will be
charged to patients. Excessive inventory can be
associated with a doctor’s preference for a certain
brand of medicine, which is caused by their
arrogance, their confidence in the brand, as well as
their close relationship with manufacturers. One
informant stated that:
“Doctors have full authority to give a
certain medicine to their patients.
Periodically, manufacturers send doctors
to attend domestic or overseas workshops
for free. Doctors also sign agreements
stating that these facilities will not affect
their prescriptions, but in fact, this does
not always happen. So, there is a tendency
that even patients with similar diseases
will be prescribed a different medicine to
that prescribed by previous doctors, even
though it has the same content. In a
symposium organized by manufacturers,
doctors will be informed about product
knowledge, including contents, benefits,
etc. This is why doctors will have the
confidence to prescribe that medicine to
patients. This doctor's confidence is
expensive. This explains why different
doctors give different medicines for
similar diseases.”
Purchasing decisions related to medicines,
medical devices, and other medical support for
hospitals are mostly determined by doctors. Often,
they do not understand or consider economies of
scale, resulting in excessive inventory or under-
utilized medical equipment or drug supplies. Of
course, this inefficiency is then charged to patients.
"Doctors have full power to determine the
types of medicine in hospital. The
medicine control function should be done
by pharmacists. However, in many cases,
pharmacists are positioned as stock
controllers only.”
4.2.1.3 Out of Stock at the Manufacturers
As a business, medicine manufacturers are always
profit-oriented and follow economic principles.
There are fast-moving and slow-moving products.
Products also have expired dates. In order to manage
their own risks, manufacturers will often reduce
production or even stop producing slow-moving
products to reduce losses. At the same time, from the
perspective of hospital management, a medicine
must be available when the hospital faces a certain
disease that needs that medicine, no matter what.
Fast-moving products can also go out of stock
as well. Fast-moving products make manufacturers
panic because of an imbalance between high demand
and limited supply. It needs a strong government
commitment and assertiveness to force
manufacturers to continue producing slow-moving
products even though the profit margin on these is
thin. The concept of price regulation using an e-
catalog must be reviewed and the GOI is encouraged
not to cut prices in a way that makes manufacturers
limit the amount of a certain medicine they produce
due to it being economically unprofitable.
"Manufacturers use their capacity to
produce products with higher margins
before producing [those with] smaller
margins. That is why the government has
to force SOEs in the pharmaceutical
industry to produce generic products, then
make an e-catalog. Then, when hospitals
want to buy [a medicine], it is in the list
of the e-catalog. However, slow-moving
or fast-moving products are often out of
stock or there are only a few in the
market. So, even though there is an e-
catalog, slow- or fast-moving products
cannot be ordered, and the price of these
products remains high."
4.2.1.4 The role of ICT in Prescriptions
Receiving the correct medication is one of the key
elements leading to the success of medical
treatment; this is true both for patients receiving
prescribed medication and those who are self-
medicating.
Medicine has very complex attributes. The use
of information communication technology (ICT) in
hospitals will provide benefits in terms of medical
safety and of accuracy when prescribing. ICT will
JCAE Symposium 2018 – Journal of Contemporary Accounting and Economics Symposium 2018 on Special Session for Indonesian Study
334

encourage efficiencies in hospitals. One informant
stated that:
"ICT infrastructure also affects hospital
productivity. In terms of prescriptions, a
hospital that has good ICT will generate a
notification that this medicine has been
prescribed by other doctors before.
However, once again, it depends on the
arrogance of doctors."
4.2.2 The Role Played by Doctors
As the main actor in a hospital, a doctor contributes
to healthcare costs. Doctors’ contributions to high
healthcare costs can be traced to their level of
education or rank or competencies, their prescription
decisions, medical equipment decisions, medical
treatment decisions, and unclear medical fees. The
following statement by an informant confirms these
issues:
"A hospital classifies a doctor’s service
fee based on [certain] criteria: whether a
doctor is a general, specialist, and/or
consultant. A higher education or rank,
such as Ph.D. or “professor” matters.
Doctors’ fees are calculated based on the
number of visits [they make] over the
length of the patient’s stay. Often, length
of stay for patients is longer only because
the doctor has not finished with their
diagnosis.”
4.2.3. Role of Non-Doctor Medical Personnel
The capacity of the hospital also contributes to
healthcare costs. Government regulations stipulate
the terms of service, human resources, hospital
equipment and buildings, as well as hospital
infrastructure. To meet these standards, hospitals
must pay relatively large operating expenses,
especially those incurred by non-doctor medical
personnel. This is revealed by an informant, who
stated:
"A hospital must follow the requirements
of regulations and standards. A hospital is
a labor-intensive organization. A
minimum standard for nurses follows the
number of beds. Not to mention that
hemodialysis units also have standards.
Then, there are standards for pharmacies
and a minimum standard for pharmacists.
But this standard is sometimes not fully
implemented by the hospital in order to
save human resource costs. In terms of
competence, ICU requires an advanced
nursing competence. The hospital must
provide a training fund of about 15-20
million rupiahs, with a training period of
six months. It’s a similar situation for
hemodialysis nurses. Operating rooms
require anesthetic nurses, general nurses,
surgical nurses and nurses to wash
surgical instruments. The cost of training
an anesthesia nurse is quite expensive and
takes about a year. A hospital must
prepare for retirement pension provision,
accreditation fees, etc.”
5. CONCLUSIONS AND
RECOMMENDATIONS
5.1 Conclusions
From previous discussions, the following
conclusions can be made:
(1) Healthcare costs in Indonesia are still
inefficient.
(2) Strategic cost-drivers affecting healthcare costs
in Indonesia, from doctors’ and hospitals’
perceptions, are: (a) high hospital costs
(marketing fees, excessive inventory, out-of-
stock medicine at the manufacturers, need for
ICT implementation and the cost of non-doctor
medical personnel); (b) the high costs incurred
or charged by doctors (their level of education,
rank or competency, their prescription
decisions and their medical equipment
decisions, as well as their medical treatment
decisions and unclear medical fees).
REFERENCES
Chakraborty, Samyadip and David D. Dobrzkowski. 2013.
Supply Chain Practices for Complexity in Healthcare:
A Srevice-Dominant Logic View. The IUP Journal of
Supply Chain Management, Vol. X, No., 3, pp. 53 –
75.
Choi, T and Y. Hong. 2002. Unveiling the Structure of
Supply Networks: case Studies in Honda, Acura, and
Daimler Chrysler. Journal of Operation Management,
Vol. 20, No. 5, pp. 469 – 493.
David, F.R., 2011. Strategic Management: Concepts and
Cases. Thirteenth Edition. Upper Saddle River, New
Jersey: Pearson Education Inc.
Factors Affecting Healthcare Costs in Indonesia: What the Hospitals and Doctors Said
335

Fama. E.F. & M.C. Jensen. 1983. Separation of
Ownership and Control. Journal of Law and
Economics, Vol. 26, 2: pp.301-325.
Ireland R.D., R.E. Hoskisson & M.A. Hitt. 2011. The
Management of Strategy: Concepts and Cases , 9
Edition. Canada: South-Western.
Keasy, K. & M. Wright. 1993. Issues in corporate
accountability and governance: An editorial.
Accounting and Business Research, 23 (91A): pp. 291-
303.
Leong, Lesly. 2008. Value Chain Management In Online
Reverse Auction: Towards Strategic and Operational
Excellence. Academy of Information and Management
Sciences Journal, Vol. 11, No. 1, pp. 13 - 28.
Lock, S. 2013. The State of Healthcare in Southeast Asia.
Terdapat di: http://www. edelman.com/ post/the-state-
of-healthcare-in-south-east-asia/.
Pathak, S.D., J.M. Day, A. Nair, W. J. Sawaya, and M.M.
Kristal. 2007. Complexity and Adaptivity in Supply
Networks: Building Supply Network Theory Using a
Complex Adaptive Systems Perspective. Decision
Sciences, Vol. 38, No. 4, pp. 547 – 580.
Porter, M.E. 1985. Competitive Advantage. The Free
Press. New York.
Porter, M.E. 2008. The Five Competitive Forces That
Shape Strategy, The Magazine. Terdapat di
http://hbr.org/2008/01/the-five-competitive-forces-
that-shape-strategy/ar/1
Shank, JK dan V Govindarajan. 1993. Strategic Cost
Management: The New Tool for Competitive
Advantage. New York: The Free Press.
Wieser, Philippe. 2011. From Health Logistics to Health
Supply Chain Management. Supply Chain Forum, An
International Journal. Vo 12, No 1, pp. 4 – 13.
World Bank, 2013. Health Expenditure, Total of GDP.
Terdapat dihttp://data.worldbank.org/
indicator/SH.XPD.TOTL.ZS.
http://kebunhadi.blogspot.co.id/2012/11/pembiayan-
kesehatan.html,
https://delfistefani.wordpress.com/2013/06/19/makalah-
pembiayaan-kesehatan/
http://afrinataika.blogspot.co.id/2014/06/demand-dan-
supply-pelayanan-kesehatan.html,
http://repository.usu.ac.id/bitstream/handle/123456789/19
856/Chapter%20II.pdf;jsessionid=332BC9C8AA043D
98DC5EA71CC91B3EB0?sequence=4
https://www.researchgate.net/profile/ronny_mustamu/publ
ication/50434713_manajemen_rantai_pasokan_industr
i_farmasi_di_indonesia/links/560d711f08ae96742010
cc65/manajemen-rantai-pasokan-industri-farmasi-di-
indonesia.pdf?origin=publication_detail
http://heldaupik.blogspot.co.id/2011/11/pembiayaan-
kesehatan.html?m=1
http://fk.uns.ac.id/static/materi/Ekonomi_Kesehatan_-
_Prof_Bhisma_Murti.pdf
http://www.kompasiana.com/yantigobel/kebijakan-
pembiayaan-kesehatan_550ee41ca33311b92dba8544
https://yantigobel.wordpress.com/2011/10/01/kebijakan-
pembiayaan-kesehatan/
http://sakinahkreatif.blogspot.co.id/2014/08/konsep-dasar-
ekonomi-kesehatan.html
https://www.imshealth.com/files/web/IMSH%20Institute/
Healthcare%20Briefs/Understanding_Pharmaceutical_
Value_Chain.pdf
http://www.ispiritsolutions.com/blog-should-you-be-
investing-in-chinese-pharma-sector/,
http://cmuscm.blogspot.co.id/2014/09/healthcare-mass-
customization-and.html -→ gambar player in the
hospital system,
http://marketrealist.com/2014/11/5-major-entities-
hospital-industry-value-chain/ -→ gambar 5 major
entities of the hospital industry
https://www.pomsmeetings.org/confproceedings/043/fullp
apers/fullpaper_files/043-0259.pdf,
http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.
836.6170&rep=rep1&type=pdf
https://courses.edx.org/asset-
v1:MITx+CTL.SC2x+3T2015+type@asset+block/thes
es_2005_Singh_Thesis.pdf, diakses tanggal 10 April
2017 pukul 14:27
http://www.nahu.org/legislative/policydocuments/NAHU
WhitePaperCost.pdf
http://www.pbs.org/newshour/rundown/seven-factors-
driving-your-health-care-costs/
http://www.physiciansfoundation.org/uploads/default/Driv
ers_of_Health_Care_Costs_-_November_2012.pdf,
diakses tanggal 19 April 2017 pukul 11:08
http://www.gfoa.org/sites/default/files/GFR081626.pdf
http://www.allhealth.org/wp-
content/uploads/2017/03/Cost_Drivers_in_Health_Car
e_109.pdf
http://www.beckershospitalreview.com/finance/9-drivers-
of-high-healthcare-costs-in-the-u-s.html
http://www.calhealthplans.org/pdfs/FactSheetHealthCareC
ostDrivers071013.pdf
http://www.who.int/healthinfo/paper30.pdf, diakses
tanggal 11 Mei 2017 pukul 19:22
https://www.bloomberg.com/news/articles/2016-09-29/u-
s-health-care-system-ranks-as-one-of-the-least-
efficient
http://www.who.int/healthsystems/topics/financing/healthr
eport/28UCefficiency.pdf
https://indonesiana.tempo.co/read/53241/2015/11/02/gend
ursudarsono/suap-dokter-40-harga-obat-tiga-hal-yang-
mengejutkan,
http://bisnis.liputan6.com/read/2628482/kenaikan-biaya-
berobat-di-indonesia-tertinggi-ketiga-di-asia,
http://www.pikiran-
rakyat.com/ekonomi/2017/02/22/biaya-kesehatan-
bisa-melebihi-pendapatan-394193
http://indonesia-
pharmacommunity.blogspot.co.id/2010/11/merintis-
industri-bahan-baku-obat-di.html
http://economy.okezone.com/read/2015/11/19/320/125246
3/impor-bahan-baku-diduga-sebabkan-kartel-obat-ri
JCAE Symposium 2018 – Journal of Contemporary Accounting and Economics Symposium 2018 on Special Session for Indonesian Study
336

https://finance.detik.com/berita-ekonomi-
bisnis/3076041/kppu-juga-endus-ada-kartel-obat-
impor
https://www.merdeka.com/uang/bahan-baku-impor-
dinilai-bikin-harga-obat-di-indonesia-mahal.html
http://nasional.kompas.com/read/2010/01/11/03551250/an
tisipasi.serbuan.obat.impor.china,
http://www.mashani77.net/2016/04/10/extra-ordinary-
problem-program-jkn-obat/
http://www.neraca.co.id/article/10876/permintaan-obat-
generik-meningkat-bangun-pabrik-indofarma-
terbitkan-obligasi-rp-300-miliar
https://bisnisfarmasi.wordpress.com/2008/03/16/strategi-
marketing-obat-a-little-bit-of-writer%E2%80%99s-
stupid-talk/
http://teknologi-profesional.blogspot.co.id/2012/02/peran-
teknologi-informasi-ict-dalam.html
http://setiawanbudi.blogspot.co.id/2006/09/tanya-tentang-
apotik.html
http://www.idionline.org/wp-
content/uploads/2015/01/Acuan-Tarif-Jasa-Medik.pdf
http://www.wajibbaca.com/2016/10/tarif-jasa-dokter-
dinilai-tak-lagi.html
https://www.merdeka.com/khas/dilema-tarif-dokter-
penghasilan-dokter.html
https://finance.detik.com/bursa-valas/2844145/bisnis-
rumah-sakit-mitra-keluarga-punya-omzet-hingga-rp-
17-triliun
http://market.bisnis.com/read/20160303/191/524802/jasa-
kesehatan-membedah-prospek-bisnis-rumah-sakit
http://data.worldbank.org/indicator/SH.XPD.TOTL.ZS
https://en.wikipedia.org/wiki/List_of_countries_by_total_
health_expenditure_per_capita
http://www.bi.go.id/id/statistik/metadata/seki/Documents/
12.%20Inflasi-
Indeks%20Harga%20Konsumen%20(IHK-
IND)%202016.pdf
Factors Affecting Healthcare Costs in Indonesia: What the Hospitals and Doctors Said
337
