
Ocular Abnormalities in Correlation with Multi-transfused in
Children with Beta Thalassemia Major
B. Lubis
1
and S. M. Lubis
2
1
Pediatric Hematology-Oncology Division, Department of Child Health, Medical School, Universitas Sumatera Utara,
Medan, Sumatera Utara, Indonesia
2
Pediatric Endocrinology Division, Department of Child Health, Medical School, Universitas Sumatera Utara, Medan,
Sumatera Utara, Indonesia
Keyword: Ocular Abnormalities, Children, Beta Thalassemia Major.
Abstract: Thalassemia is the commonest haemoglobinopathies worldwide. Repeated blood transfusion lead to
hemosiderosis which affects all the organ in the body including eyes. The aim of this study was to evaluate
ocular abnormalities in children with beta thalassemia major who have received multiple blood transfusions.
A cross-sectional study was conducted in the Thalassemia day-care centre of a tertiary care at H. Adam
Malik Hospital Medan, Indonesia. Visual aquity, anterior segment, fundus, and retina were evaluated to
screen ocular abnormalities. There were 37 patients with beta thalassemia major, male and female were 20
(51.3%) and 17 (48.7%), respectively, age 3 to 18 years. All patients received regular blood transfusions,
but only 28 patients (78.4%) received iron chelation therapy. Opthalmologic examinations showed ocular
abnormalities in 15 subjects (40.4%), cataract in 3 patients (8.1%), papil edema in 10 patients (27%), and
papil atrophy in 2 patients (5.4%). Decreased visual acuity was observed in 8 patient (21.6%).
Hyperpigmentation in bulbar conjunctiva were seen in 12 patients (32.4%). There was no significant
correlation between ocular abnormalities and multiple transfusions. Regular ophthalmologic evaluations
was needed to detect retinopathy and early changes in their ocular system for a better quality of life in
thalassemic patients.
1 INTRODUCTION
Thalassemia is a severe genetic blood disorders
caused by a mutation in the globin gene. Abnormal
globin chains lead to the excessive destruction of red
blood (Vichinsky EP, 2005). Beta thalassemia major
is one of the most common hemoglobinopathy.
Management of thalassemia major consist of regular
blood transfusions therapy throughout the life,
getting natural development and growth, reducing
hyperplasia of erythroid tissue and deformities of
skeleton (Cao A, 2010; Langhi D et al., 2016).
Although transfusions can prevent death and decease
mortality, iron accumulated from repeated blood
transfusion and enhanced iron absorption by
gastrointestinal tract can lead to organ damage such
as heart, liver, endocrine gland, and skeletal system
(Propper RD, 1980).
Mechanism of ocular manifestations in
thalassemia is multifactorial such as regular blood
transfusion therapy which causes iron overload. Iron
chelating agents chelate other metals suchs as
Copper, zinc, nickel, and cobalt essential for normal
retinal function causing several ocular abnormalities.
Deficiency micronutrients like zinc, vitamins like
vitamin B
12
can also lead to ocular manifestations.
Iron deposition in eye can lead to several ocular
abnormalities as a result of the disease itself or as
side effects of iron chelators and include ocular
surface disorders, cataract, angioid streak, retinal
venous tortuosity, retinal pigment epithelium (RPE)
degeneration and mottling, optic neuropathy, and
decreased visual acuity (Taher A et al., 2006; Arden
GB et al., 1984; Gartaganis S et al., 1989).
This study was conducted to assess the
prevalence of ocular abnormalities in multi-
transfused beta-thalassemia patients and to
determine their relationship with serum ferritin level.
2 METHODS
A cross-sectional study was conducted in the
Thalassemia day-care centre of a tertiary care H.
898
Lubis, B. and Lubis, S.
Ocular Abnormalities in Correlation with Multi-transfused in Children with Beta Thalassemia Major.
DOI: 10.5220/0010099508980903
In Proceedings of the International Conference of Science, Technology, Engineering, Environmental and Ramification Researches (ICOSTEERR 2018) - Research in Industry 4.0, pages
898-903
ISBN: 978-989-758-449-7
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
Adam Malik Hospital Medan, Indonesia. Thirty
seven children were included in this study. Inclusion
criteria were children with beta thalassemia major
with the age less than 18 years with regarding two
years blood transfusion. Subjects have received
packed red cell transfusions with a dosage of 15 ml/
Kg BW to maintain haemoglobin concentration after
transfusion at levels greater than 11 g/dL for at least
2 years were enrolled in the study. Haemoglobin was
measured before each transfusion and the serum
ferritin levels was measured in all patients at 6-
monthly intervals. The records were kept at the
thalassemia day-care centre.
Ophthalmological assessment was assessed by
Pediatric Ophthalmologist, included a detailed
history of visual problems and visual aquity
screening. Anterior segment was examined by using
slit lamp and posterior segment screening was
evaluated by using multimodal imaging in
ophthalmology like indirect retinoscopy, optical
coherence tomography (OCT) or fundus photo.
Subjects who had history of corneal disease, using
contact lens, ocular trauma, previous ocular surgery,
and those taking topical medications were excluded
in this study.
2.1 Statistical Analysis
The relationship between serum ferritin level and
ocular abnormalities was analysed using Chi square
test. Spearman test was used to determine the
correlation between frequency and volume of
transfusion with serum ferritin level. Statistical
calculation was done using Statistical Package for
Social Science (SPSS) version 24.0 at 95%
confidence interval and P-value of <0.05 was
considered as statistically significant.
3 RESULTS
There were thirty seven thalassemia subjects with
the age 3–18 years were included in this study, there
were 20 subjects (51.3%) were male and 17 subjects
(48.7%) were female. Baseline characteristics of
subjects were shown in Table 1. The dominant
ethnic in this study was Javanese (59.8%). All
subjects received regular blood transfusion, but only
28 patients (78.4%) received iron chelation therapy,
and others (21.6%) without iron chelation
treatments. Median age at diagnosis was 31.0 (3.0-
180.0) months. Only 5 (13.5%) subjects had serum
ferritin levels was less than 1000 ng/mL, and 32
subjects (86.5%) was more than 1000 ng/
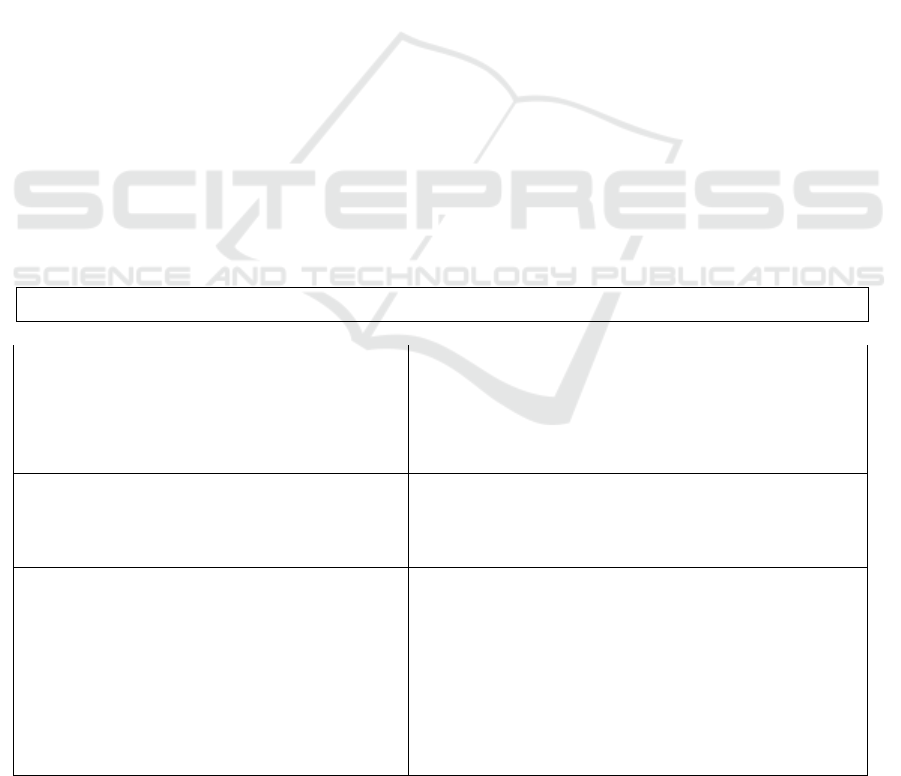
Table 1. Baseline characteristics of subjects
n (%)
Age, year
<5
5-10
>10
Gender
Male
Female
20 (51.3)
17 (48.7)
Ethnicity
Acehnese
Javanese
Karonese
Melayunese
Padangnese
Sundanese
Chinese
2 (5.4)
22 (59.8)
3 (8)
2 (5.4)
6 (16)
1 (2.7)
1 (2.7)
Ocular Abnormalities in Correlation with Multi-transfused in Children with Beta Thalassemia Major
899
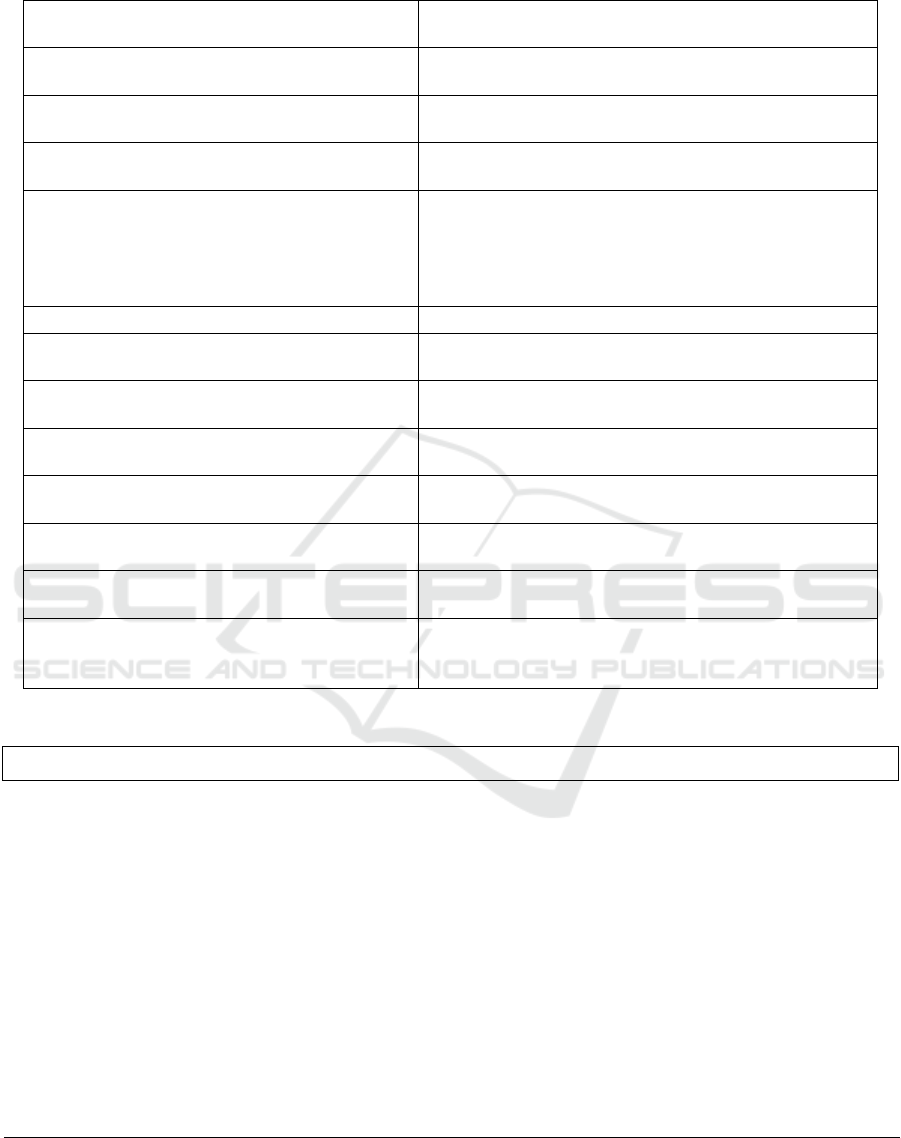
Table 1: Baseline characteristics of subjects
Table 2: Ocular abnormalities findings
n (%)
Characteristics of bulbar conjunctiva
Normal 25 (67.6)
Hyperpigmentation 12 (32.4)
Characteristics of camera oculi anterior
Normal 30 (81.1)
Hyperpigemtation 7 (18.9)
Visual acuity
Normal 29 (78.4)
Decrease 8 (21.6)
Ocular abnormalities
None 22 (59.5)
Papil edema 10 (27)
Complicated cataract 3 (8.1)
Papil atrophy 2 (5.4)
Mean body weight, kg (mean ±SD)
24.5 (8.8)
Mean body height, cm (mean ±SD) 123.6 (18.9)
Mean BMI, kg/m
2
(mean ±SD)
15.4 (2.2)
Median age at diagnosis, month (min-max) 31.0 (3.0-180.0)
Iron chelating agent
Exjade
Ferriprox
None
13 (35.1)
16 (43.3)
8 (21.6)
Serum ferritin level
< 1000 ng/mL
5 (13.5)
1000-5000 ng/mL 20 (54.1)
5000-10000 ng/mL
8 (21.6)
>10.000 ng/mL 4 (10.8)
Median serum ferritin level, ng/mL ((Min –
max)
2842.0 (430.8-31285.4)
Median transfusion volume, mL (min-max)
175.0 (10.0-525.0)
Median transfusion frequency, time (min-
max)
12.0 (3.0-48.0)
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
900
The association between serum ferritin levels and
ocular abnormalities has been shown in Table 3.
The prevalence of hyperpigmentation in bulbar
conjunctiva and camera oculi anterior were 8
(66.7%) and 3 (42.9%), respectively, in subjects who
had serum ferritin levels between 1000-5000 ng/ml.
Visual acquity decreased in 8 (21.6%) in subjects,
we also found 3 subjetcs with cataract, but there
were no significant association between serum
ferritin levels and hyperpigmentation, vivisual
acquity, and cataract in our subjects.
Table 4 showed the correlation between
frequency and volume of transfusion with serum
ferritin level. There was significant association
between blood volume of transfussion and serum
ferritin levels (p<0. 05), but there was no significant
association between frequency of transfussion with
serum ferritin levels.
Table 3. Association between serum ferritin level and ocular abnormalities
Category of serum
ferritin level
Bulbar conjunctiva p
Normal (%) Hyperpigmentation (%)
<1000 3 (12.0) 2 (16.7) 0.428
1000-5000 12 (48.0) 8 (66.7)
5000-10000 6 (24.0) 2 (16.7)
>10000 4 (16.0) 0 (0.0)
Camera oculi anterior
Normal (%) Hyperpigmentation (%)
<1000 4 (13.3) 1 (14.3) 0.920
1000-5000 17 (56.7) 3 (42.9)
5000-10000 6 (20.0) 2 (28.6)
>10000 3 (10.0) 1 (14.3)
Visual acuity
Normal (%) Decreased (%)
<1000 3 (10.3) 2 (25.0) 0.283
1000-5000 17 (58.6) 3 (37.5)
5000-10000
>10000
5 (17.2)
4 (13.8)
3 (37.5)
0 (0.0)
Ocular abnor
m
alities
None (%) Oedema of
papilla (%)
Complicated
cataract (%)
Atrophy of
papilla (%)
<1000 3 (10.3) 2 (25.0) 0 (0.0) 0 (0.0) 0.632
1000-5000 17(58.6) 3 (37.5) 1 (33.3) 2 (100.0)
5000-10000 5 (17.2) 3 (37.5) 1 (33.3) 2 (100.0)
>10000 4 (13.8) 0 (0.0) 1 (33.3) 0 (0.0)
Ocular abnormalities
Complicated cataract (%) No cataract (%)
<1000 0 (0.0) 1 (8.3) 0.541
1000-5000 1 (33.3) 8 (66.7)
5000-10000 1 (33.3) 2 (16.7)
>10000 1 (33.3) 2 (16.7)
*Chi square test
Table 4. Correlation between frequency and volume of transfusion with serum ferritin level
Mean
r
p
Frequency of transfusion, time
Serum ferritin level, n
g
/mL
17.6
5033.2
0.199 0.239
Volume of blood transfusion, mL
Serum ferritin level, n
g
/mL
188.7
5033.2
0.544 <0.001
*Spearman test
Ocular Abnormalities in Correlation with Multi-transfused in Children with Beta Thalassemia Major
901

4 DISCUSSION
Thalassemic patients are on lifelong blood
transfusion therapy. Multiple or repeated blood
transfusions lead to siderosis and adverse ocular
changes may occur as a result of the disease or due
to iron overload and chelation therapy. Adverse
retinal effects may occur as a result of the iron
chelators or the disease itself and include the
following: Retinal pigment epithelium (RPE)
degeneration, RPE mottling, retinal venous
tortuosity and vitrretinal hemorrhages. Thalassemic
patients may present with decresed visual acuity,
color vision anomalies, hyperpigmentasi, papil
edema, papil athrophy, thinning and tortuosity of
retinal vessels, vitreo-retinal hemorrhages, night
blindness, cataracts, visual field defect and optic
neuropathy. Thalassemia major may also be
associated with a nonproliferative pigmentary
retinopathy due to liberation of free iron as a result
of hemolysis (Gartaganis S et al., 1989; Wong RW
et al., 2001).
This study was conducted to detect various
ocular changes in patients who were on regular
transfusion and iron chelating agent. We evaluated
37 thalasemic children with ocular abnormalities in
15 patients (40.5%), such as visual acquity
decreased in 8 patients (21.6%). There was no
significant correlation between serum ferritin levels
and edema and athropy papil, and cataract. Other
studies reported ocular abnormalities were found in
41.3%, 36%, and 38% (Gartaganis S et al., 1989;
Dewan P et al.2011; Soecinelli R et al., 1990).
Difference results of ocular abnormalities that had
been reported in previous studies may be due to
differences in parameters used to evaluate ocular
abnormalities, it is difficult to make an accurate
comparison. Ocular changes were seen more in
children above 10 years of age and was less in
children below 5 years of age. This clearly shows
that longer the duration of the illness more are the
eye changes.
Decreased visual aquity was observed in 8
patients (21.6%), this result was almost same with
other studies that reported the insidence of decreased
visual acquity was about 15.5–30% in thalassemic
patients (Taher A et al., 2006; Gartaganis S et al.,
1989). The presence of ocular abnormalities was
correlated with serum ferrin levels and multiple
transfusion. This study reported ocular abnormalities
were found in 16 (84%) subjects with the serum
ferritin levels were more than 1000, and less than
1000 ng/mL in 3 subjects (16%). Iron causes
oxidative damage to protein, lipids, and DNA
through the generation of free radicals in the Fenton
reaction and it has been shown to disrupt the blood-
retinal barrier. Iron may play a role in the
pathogenesis of retinal degeneration as a source of
free radical damage. Iron toxicity from multiple
blood transfusions may contribute to beta-
thalassemia retinopathy. Iron is important
component of many metabolic processes, but
appropriate regulation is necessary to prevent
toxicity (Liaska A et al., 2016; Song D et al., 2013).
The limitations in our study were that very few
children with thalassemia use iron chelating therapy
due to low their low socio-economic level, and we
could not evaluate the effect of chelation therapy on
the ocular abnormality especially on the retina in
thalassemic children. We did not correlate the ocular
abnormalities with frequency and volume of blood
transfusion in our subjects. Our study has same
limitations, we did not compare the ocular
abnormalities with frequency and volume blood
transfusion therapy for thalassemic patients,
differences between iron chelation regimen and
there is a possibility that their ocular abnormalities
could have occurred before first time blood
transfusion treatment. Overall, the correlation
between ocular abnormality and frequency and
volume blood transfusion has not been established in
present study, hence, further prospective
investigations with a large sample of thalassemia
patients are suggested.
5 CONCLUSION
The ocular abnormalities in our subjects were
asymptomatic, but 15 subjects (40.4%) was revealed
ocular abnormalities. We did not find any significant
correlation between ocular abnormalities with serum
ferritin levels and multiple transfusion, but a
significant association was found between volume of
blood transfussion and serum ferritin levels. Since
life expectancy in patients with beta thalassemia
major increases, it is necessary to screen for ocular
abnormalities in all children with thalassemia to
improve the quality of life of thalassemic patients.
ACKNOWLEDGMENT
The authors wish to thank the children and parents
of thalassemia patients in one day care center (ODC)
- H. Adam Malik Hospital Medan and dr Balqis D
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
902

Sulistyowati Pediatric Ophthalmologist - for their
cooperation.
This study has been granted by TALENTA 2018
University of Sumatera Utara.The authors declare
not having any proprietary interest in the materials
described in the article. There are no conflicts of
interest.
All procedures performed in studies involving
human participants were in accordance with the
ethical standards of the institutional and national
research committee and with the 1964 Helsinki
declaration and its later amendments or comparable
ethical standards.
Informed consent was obtained from all
individual participants included in the study.
REFERENCES
Vichinsky EP. Changing patterns of thalassemia
worldwide. Ann N Y Acad Sci. 2005; 1054: 18-24.
Cao A, Galanello R. Beta-thalassemia. Genet Med. 2010;
12: 61-76.
Langhi D, Ubiali EMA, Marques JFC, et al. Guidelines on
Beta-thalassemia major-regular blood transfusion
therapy. Revista Brasileira de Hematologia e
hemoterapia. 2016; 38(4): 341-5.
Propper RD, Button LN, Nathan DG. New approaches to
the transfusion management of thalassemia. Blood
1980; 55: 55-60.
Taher A, Bashshur Z, Shamseddeen WA, et al. Ocular
findings among thalassemia patients. Am J
Ophthalmol. 2006; 142: 704-5.
Arden GB, Wonke B, Kennedy C, Huehns ER. Ocular
changes in patients undergoing long term
desferrioxamine treatment. Br J Ophthalmol. 1984; 68:
873-7.
Gartaganis S, Ismiridis K, Papageorgion O, Beratis NG,
Papanastatasiou D. Ocular abnormalities in patients
with beta thalassemia. Am J Ophthalmol. 1989; 108:
699-705.
Wong RW, Richa DC, Hahn P, Green WR, Dunaief JL.
Iron toxicity as a potential factor, in AMD. Retina
.2007; 27: 997-1003.
Dewan P, Chawla H, Rohatgi J. Ocular changes in multi-
transfused children with β-thalassaemia receiving
desferrioxamine: A case-control study. SA J Child
Health. 2011; 5: 11-4.
Soecinelli R, Sitzia A, Figus A, Lai ME. Ocular findings
in beta-thalassemia. Metab Syst Ophthalmol. 1990;
13: 23-5.
Liaska A, Petrou P, Geogakopoulos CD, Diarmanti R, et
al. β-Thalassemia and ocular implications: A systemic
review. BMC Ophthalmol. 2016; 16: 102.
Song D, Dunaief JL. Retinal iron homeostasis in health
and disease. Front Aging Neurosci. 2013; 5: 24 (PubMed:
23825457).
Ocular Abnormalities in Correlation with Multi-transfused in Children with Beta Thalassemia Major
903
