
Relationship between Short Stature and Serum Ferritin in Children
with Beta Thalassemia Major
S. M. Lubis
1
and B. Lubis
2
1
Pediatric Endocrinology Division, Department of Child Health, Medical
School, Universitas Sumatera Utara, Medan, Sumatera Utara, Indonesia
2
Pediatric Hematology-Oncology Division, Department of Child Health,
Medical School, Universitas Sumatera Utara, Medan, Indonesia
Keyword: Short Stature, Serum Ferritin, Children, Beta Thalassemia.
Abstract: Short stature has been recognized in thalassemia major patients for many years and continue to be common
problems despite regular transfusion and chelation therapy. The aim of this study was to determine the
relationship between short stature and serum ferritin in children with beta thalassemia major. A cross sectional
study was carried out in children with beta thalassemia major who met the inclusion criteria and selected
based on consecutive sampling, aged less than 18 years, and regularly visited Thalassemia Day-Care Centre
at H. Adam Malik and Universitas Sumatera Utara General Hospital. This study was conducted in March to
May 2018. Data was collected through the questionnaire, anthropometric measurements, and blood test
analysis. Descriptive statistics and chi-square test were performed, p<0.05 was considered as significant level.
There were 56 children were recruited in this study, females and males comprised 27 (48.2%) and 29 (51.8%)
respectively, 60.2% of subjects had short stature and 14.3% had severe thinness. The mean serum ferritin
levels were 5081.41±4503.65 ng/mL. Age at diagnosis was 40±33.61 months. This study found there was no
significant association between serum ferritin levels with short stature but significant association was
identified between age at diagnosis and short stature.
1 INTRODUCTION
Thalassemia as the most common genetic disorder
worldwide is regarded as a serious problem in public
health issues especially in Asia region (Ansari Sh et
al., 2014).Almost 100,000 patients with major
thalassemia need regular transfusions. Regular red
blood cell (RBC) expansion, permit normal
development throughout childhood, and extend
survival (Hashemi A et al., 2011). Transfusions
result in iron overload, which is fatal without
treatment in the second decade of life. Iron-chelating
therapy for iron overload is one important part of
major thalassemia treatment in last 20 years
(Hashemi A et al., 2011).Although morbidity and
mortality of the thalassemia major has been
significantly in the light of modern medical
treatment, however, it could influence various
aspects of patients’ life (Ansari Sh et al., 2014).
Many complications of beta thalassemia major
are the result of increased iron deposition from
repeated blood transfusion. The accumulation of iron
in different tissues causes organ damage affecting
mainly endocrine glands, heart, and liver. The most
prominent endocrine complication is growth
retardation and failure of normal pubertal
development. Growth failure has been attributed to
growth hormone (GH) hypothalamic and/or
pituitary, insulin-like growth factor 1 (IGF-1),
insulin-like growth factor binding protein 3
(IGFBP3) deficiency, hypothyroidism, delayed
sexual maturation and to bone disorders caused by
iron-chelating toxicity. Short stature in children with
beta thalassemia major could be due to GH-IGF-1
axis dysfunction and iron-chelating induced bone
dysplasia (Nasr MR., 2012).
Malnutrition is a significant cause of growth
retardation in thalassemic children living in poor
countries. In these children, inadequate nutrient
intake (zinc, folic acid, vitamin D, carotenoids, and
retinol binding proteins) contribute significantly to
their growth impairment (De Sanctis V et al., 2014).
The aim of this paper was to determine the
relationship between short stature and serum ferritin
in children with beta thalassemia major.
Lubis, S. and Lubis, B.
Relationship between Short Stature and Serum Ferritin in Children with Beta Thalassemia Major.
DOI: 10.5220/0010098908910897
In Proceedings of the International Conference of Science, Technology, Engineering, Environmental and Ramification Researches (ICOSTEERR 2018) - Research in Industry 4.0, pages
891-897
ISBN: 978-989-758-449-7
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
891
2 METHODS
This cross sectional study was conducted in March
to May 2018. Subjects were selected by using
consecutive sampling that met the inclusion criteria
and regularly visited Thalassemia Day-Care Centre
at H. Adam Malik and Universitas Sumatera Utara
General Hospital. The inclusion criteria were
children with beta thalassemia major aged less than
18 years with regarding two years blood transfusion
and received blood transfusion regularly, and
exclusion criteria were having genetic disease such
as Down syndrome and chronic illness (malignancy,
tuberculosis, chronic hepatitis, congenital heart
disease, chronic renal failure, primary skeletal
disorders, diabetes mellitus). Serum ferritin level
was measured using the
chemiluminescentmicroparticle immunoassay
(CMIA).
The study included a questionnaire for parents or
guardians and anthropometric measurements. The
questionnaires requested information about the age
at diagnosis, history of thalassemia in family, get
iron chelating agent, frequency of blood transfusion
in a year, and social- economic data. Anthropometric
measurements included body weight (in Kg), was
measured to the nearest 0.1 Kg by digital machine.
Height (in cm) was measured to the nearest 0.1cm by
using stadiometer. All instruments were validated
following the manufacturer’s protocol. Body mass
index (BMI) was calculated as weight (kg) /height
(meter) (Ogden CL et al., 2010).Then, the subjects
were categorized based on World Health
Organization (WHO) reference of Children Growth
Chart which is recognized as z- scores (standard
deviation scores). Short stature was assessed by
using Growth Chart Center for Disease Control
(CDC) 2000 for boys and girls.
This study was approved by The Ethics
Committee of The Medical School, Universitas
Sumatera Utara, Medan, Sumatera Utara, Indonesia.
All parents or guardians gave written informed
consent that the results of this study would be used
for scientific research purposes.
2.1 Statistical Analysis
Data were analyzed using SPSS software version 24
(SPSS Inc., Chicago, IL, USA). Quantitative
variables were expressed as mean±standard
deviation (SD). The descriptive statistics were used
to analyze socio demographic characteristics of the
subjects. The relationship between short stature and
serum ferritin level was used chi-square test, p<0.05
was considered as significant level.
3 RESULTS
There were 56 children were recruited in this study,
females was 27 (48.2%) and male was 29 (51.8%),
respectively. Characteristics of children in this study
are given in Table 1. Short stature was found in 34
(60.7%) and normal stature was in 22 (39.3%)
subjects. Most thalassemia children had normal
nutritional status, but 14,3% subjects were thinness
(BMI <-2 SD) and 14.3% are severe thinness (BMI
<-3 SD). Family history of thalassemia was found
only in 12 (21.4%) subjects, but it is possible that the
number of subjects who had a family history of
thalassemia is actually more than that reported by
parents in the questionnaire, because some are not
diagnosed or have not screened. Most subjects were
diagnosed with beta thalassemia major at over 2
years of age. Around 87.5% of subjects had parental
income of 5-10 million rupiah in a month.
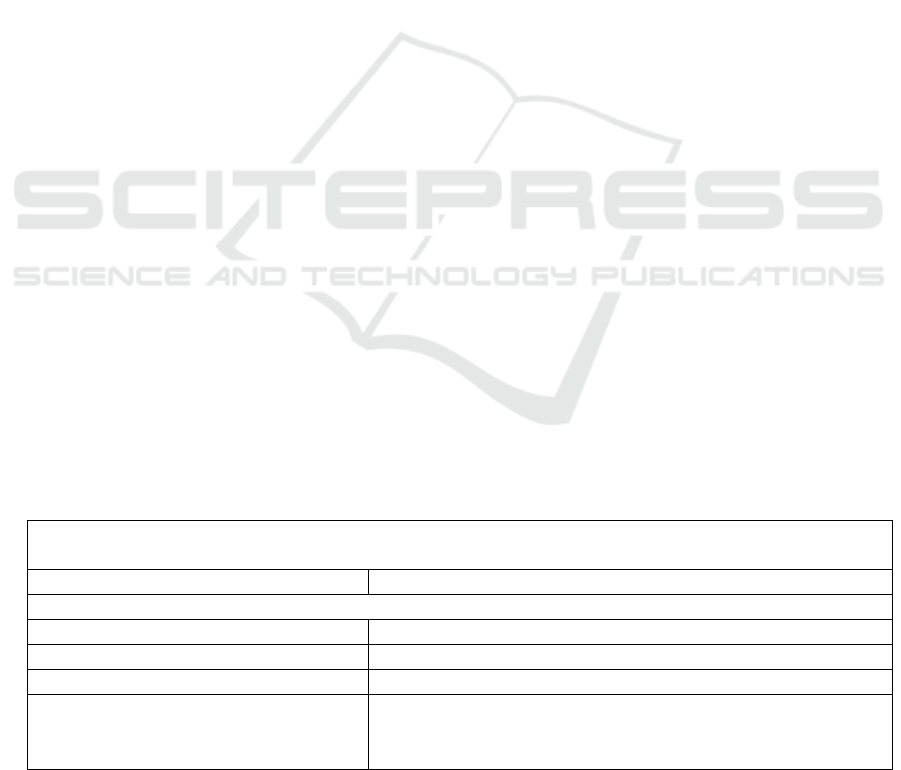
Table 1. Characteristics of Children in this Study
n (%)
Age (years) 9.46±4.44
Age at diagnosis
< 6 months 7 (12.5)
6 months to 2 years 12 (21.4)
>2 years 37 (66.1)
Sex:
Male
27 (48.2)
Female 29 (51.8)
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
892
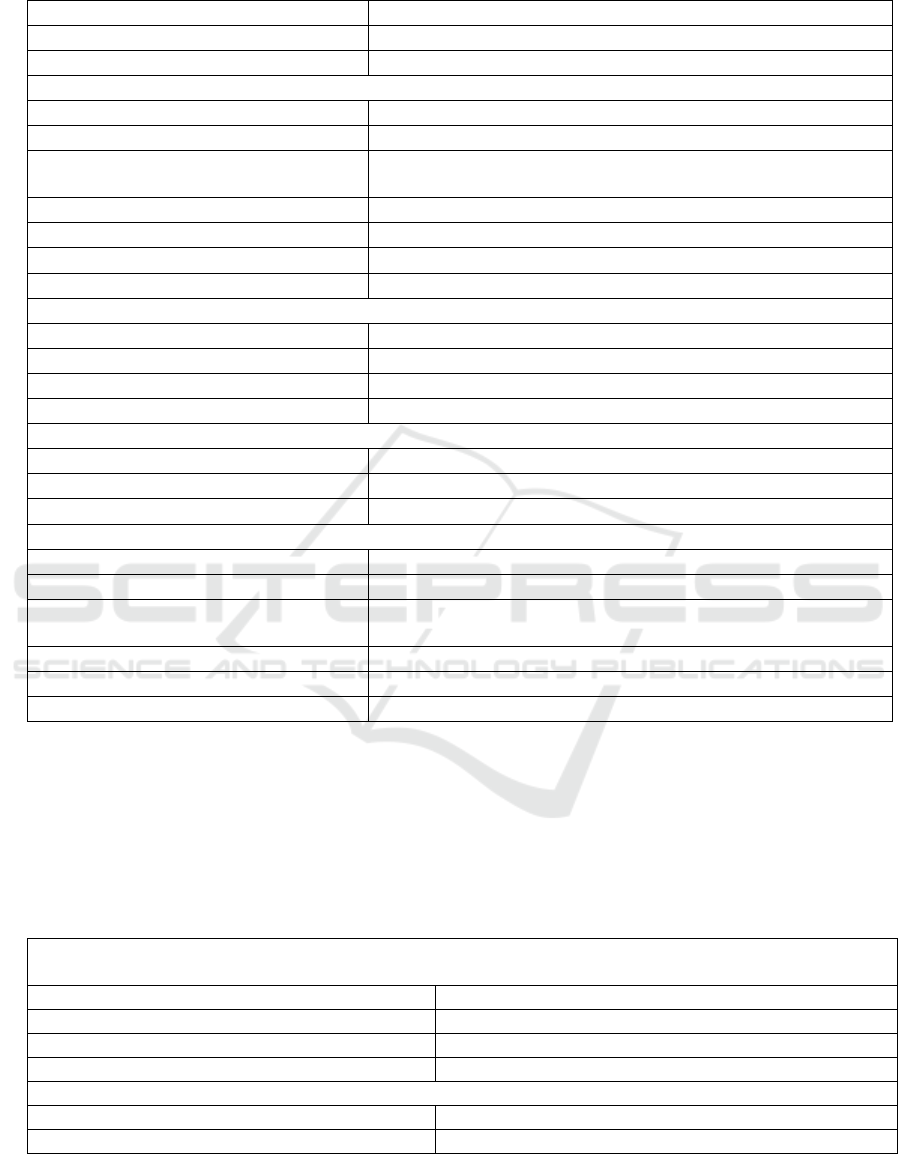
Table 1. Characteristics of Children in this Study (cont.)
Body weight (Kg) 23.63±8.77
Body height (cm) 121.41±19.07
BMI (kg/m
2
) 15.50±2.16
Family history of thalassemia
Yes 12(21.4%)
No 44(78.6%)
Father’sEducation
level
Elementaryschool 9 (16.1)
Middle school 11 (19.6)
Seniorhighschool 31 (55.4)
University 5 (8.9)
Mother’s education level
Elementaryschool 9 (16.1)
Middle school 14 (25.0)
Seniorhighschool 27 (48.2)
University 6 (10.7)
Parental income (Rupiah)
< 5 million 49 (87.5)
5-10million 6 (10.7)
> 10million 1 (1.8)
Nutritional status (body mass index)
Normal 40 (71.4)
Thinness (<-2 SD) 8 (14.3)
Severethinness (<-3
SD)
8 (14.3)
Stature
Normal 22 (39.3)
Short stature 34 (60.7)
BMI: Body mass index. Data are means ± SD, or percentages.
Table 2 showed serum ferritin levels in most subjects
were above 2000 ng/mL, hemoglobin levels before
transfusion of most children between 5-7 g/dL, most
subjects received blood transfussions every month,
and 17 (30.4%) subjects did not use iron chelating
therapy.
Table 2. Variables Characteristics
n(%)
Ferritin Level (ng/mL)
<1000 7 (12.5)
1000-2000 12 (21.4)
>2000 37 (66.1)
Haemoglobin level before transfussion (g/dL)
<5 6 (10.7)
5-7 44 (78.6)
Relationship between Short Stature and Serum Ferritin in Children with Beta Thalassemia Major
893
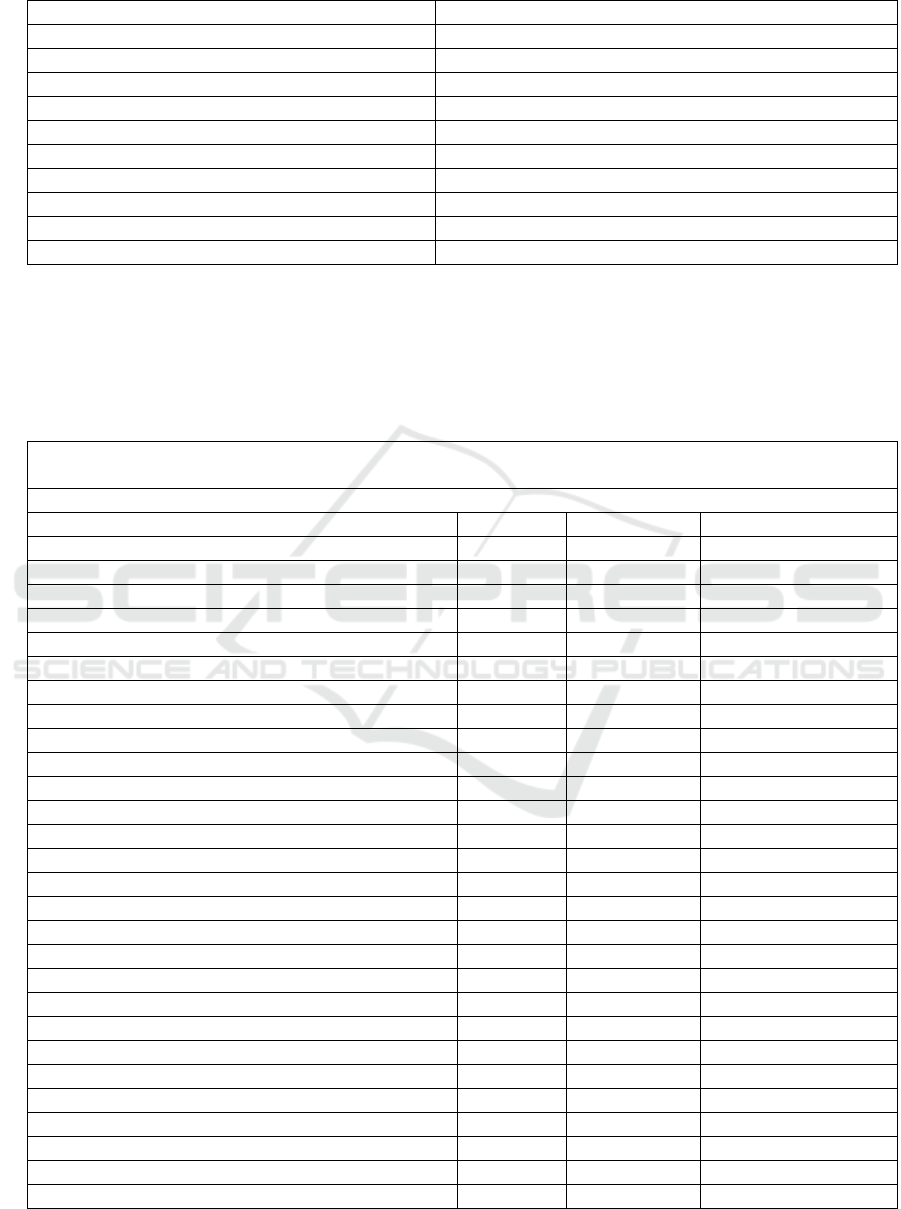
Table 2. Variables Characteristics (cont.)
>7 6 (10.7)
Transfussion frequency
Every week 2 (3.6)
Every 2 weeks 19 (33.9)
Every 3 weeks 6 (10.7)
Every month 24 (42.9)
More than 1 month 5 (8.9)
Iron-chelating agent
Deferiprone 21 (37.5)
Deferasirox 18 (32.1)
Without therapy 17 (30.4)
The relationship between short stature and serum
ferritin levels and other variables characteristics can
be seen in Table 3. There was no significant
relationship between short stature and serum ferritin
levels and with other characteristic variables, but this
study reported a significant relationship between
short stature and age at diagnosis.
Table 3. Association between short stature with serum ferritin and other characteristics
Normal Short stature p
Age
<5 4 5 0.328
5-10 12 13
>10 6 16
Age at diagnosis
< 6 months 6 1
0.003
6 months to 2 years 7 5
>2 years 9 28
Sex: Male 11 16 0.830
Female 11 18
Family history of thalassemia
Yes 18 26 0.634
No 4 8
Parental income (Rupiah)
< 5 million 19 30 0.440
5-10 million 2 4
> 10 million 1 0
Nutritional status (body mass index)
Normal 15 25 0.799
Thinness (<-2 SD) 4 4
Severe thinness (<-3 SD) 3 5
Ferritin Level (ng/mL)
<1000 1 6 0.296
1000-2000 6 6
>2000 15 22
Haemoglobin level before transfussion (mg/dL)
<5 2 4 0.893
5-7 18 26
>7 2 4
Transfussion frequency
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
894
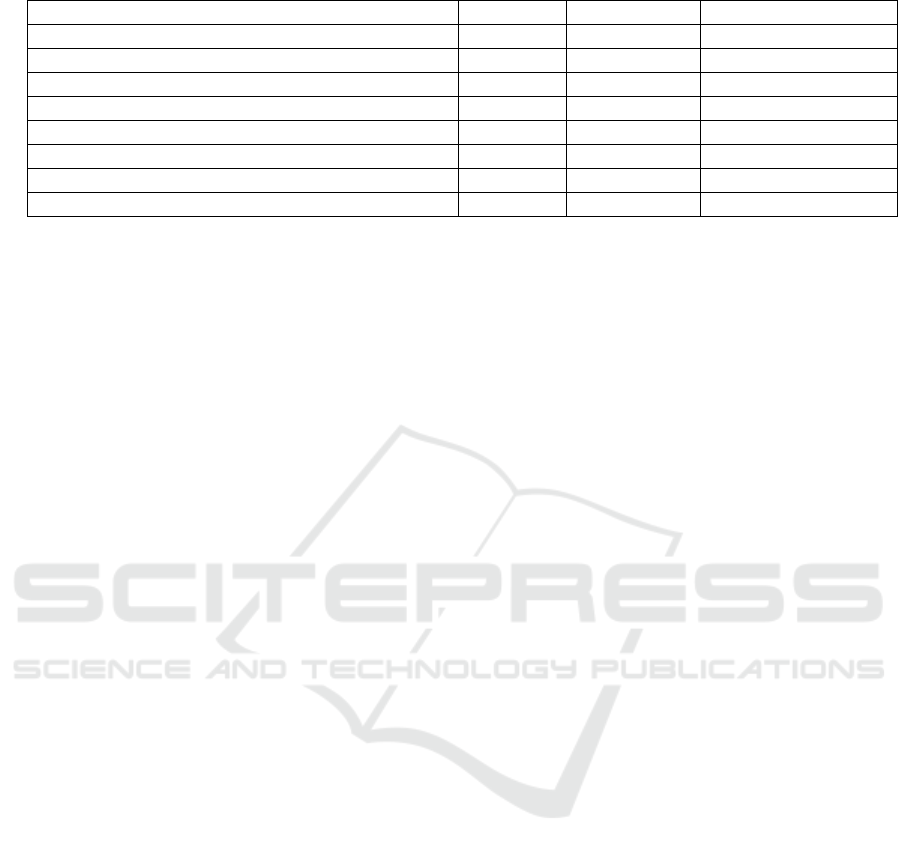
Table 3. Association between short stature with serum ferritin and other characteristics (cont.)
Every week 1 1 0.062
Every 2 weeks 5 14
Every 3 weeks 0 6
Every month 14 10
More than 1 month 2 3
Iron-chelating agent
Deferiprone 8 13 0.849
Deferasirox 8 10
Without therapy 6 11
Associations are considered significant when p< 0.05.
4 DISCUSSION
Beta thalassemia major is a severe early-onset form
of beta-thalassemia characterized by severe anemia
requiring regular red blood cell transfusions, it
usually cause severe anemia with several health
problems like enlarged spleen, bone deformities,
short stature, diabetes, hepatitis infection, and
requires regular life-long transfusion, therapy, and
medical supervision. Thalassemia affects the growth
of the thalassemic patients (Al-saleheQAA et al.,
2015). Other risk factors that might affect growth
disorders in thalassemia children are low hemoglobin
level pre-transfusion, high ferritin level, not optimal
used iron chelating agent, low social- economic level
and increasing age of thalassemia children. Long-
term blood transfusion and chelating agent
administrations can improve quality of life of the
thalassemic children and decrease deaths due to heart
failure. Growth characteristics in children with
thalassemia major commonly show normal condition
in the first 10 years but growth retardation may occur
after 10 years (Al-salehe QAA et al., 2015; Fadlyana
E et al., 2017).
A total of 56 subjects who met the inclusion
criteria were involved in this study. The results
showed that 60.7% subjects were reported short
stature. The proportion of short stature in this study
was similar to the previous studies that found the
incidence of short stature,as in study that was
conducted on Iranian thalassemic patients the
incidence of short stature were 52.3% (Badfar G et
al., 2017),and other countries reported the prevalence
of short stature to be 30-60% (HamidahA et al., 2001;
Shlomit et al., 2005; Borgna-Pignatti C et al., 1985;
Gomber S, 2006). Butlower incidence was found in a
study by Shamshirsaz et al that reported the incidence
of short stature in thalassemic children was 39.3%
(Shamshirsaz AA et al., 2003).Difference in
prevalence of short stature in patients living in
various countries could be due to genetic
susceptibility to the toxic effects of iron overload in
endocrine gland and serum ferritin. It may also
indicate differences in quality of care, follow-up and
treatment, quality of blood transfusion, chelation
therapy type (regular or irregular) and beginning of
iron chelating therapy.
Normal growth in thalassemic children in the first
10 years depend on hemoglobin levels which are
maintained at above 10–11 g/dL. This condition can
be caused by hypoxia as a major growth disorder
factor (Al-(Wataify AS, 2014). In this study, most
subjects showed average hemoglobin levels before
transfusion was 5–7 g/dLthat foundin 78.6% subjects,
this study also reported that there was no association
between hemoglobin levels before transfusion and the
incidence of short stature (p>0.05). However, a study
that was conducted in Iraq revealed different results
that the hemoglobin levels before transfusion was <9
g/dLwas statistically increase the incidences of short
stature in thalassemic children (Wataify AS,
2014).Differences in results can be caused by a lack
of compliance to attend regular blood transfusion.
Low family income becomes a major factor that
affect the compliance.
Ferritin is an iron storage form in the body, which
releases the required iron when needed. All
thalassemic patients using iron chelator should be
monitored and evaluated regarding serum ferritin
levels (Nesheli HM et al., 2016).Moayeri et al
reported that short stature in thalassemic children was
found with serum ferritin levels more than 2000
ng/mL.It can be caused by not optimal and delayed
iron chelating treatment (Moayeri H et al.,
2006).Another study reported that short stature was
foundwith serum ferritin levels more than 3000
ng/mL (Shalitin S et al., 2005).While other study
reported that high serum ferritin levels in puberty may
cause growth retardation (Jahargidar R et al.,
2017).Causes of growth retardation that usually
becomes remarkable in puberty are chronic anemia-
Relationship between Short Stature and Serum Ferritin in Children with Beta Thalassemia Major
895

related chronic hypoxemia, increased calorie need
due to increased erythropoiesis, growth hormone
deficiency that may develop as a result of toxicity on
hypotalamo-hypophysial level caused by increased
iron load, hypothyroidism, inability to make the
growing spurt because of delayed puberty and
hypogonadism, and psychosocial factors (Yaman A
et al., 2013).
Unlike previous studies, in this study we did not
find significant association between serum ferritin
levels and short stature in our subjects.This can occur
due to a small sample size, measurement errors, or
chelating therapy type. Another possible reason to
explaining the lack of significant association between
serum ferritin levels and short stature is the possible
serum ferritin tolerance. In this study, serum ferritin
levels were measured at a given moment, and its
changes at different times were not determined.
However, short stature was seen in most our subjects
with the serum ferritin levels more than 2000 ng/mL.
Some factors considered as risk factors for having
complication in thalassemia patients were as follows:
Sex, age at diagnosis, age at start of transfusions, age
at start of chelation therapy, intensive and/or early
chelation with desferrioxamine, use of oral chelators,
chronic hepatitis C, and iron-related complications
(Origa R et al., 2016).This study reported a significant
association between age at diagnosis and short stature
(p<0.05), it showed us that the rate of complications
was increased in older patients. This phenomenon
may be a result of early hypothalamic/ pituitary
damage induced by iron overload, and/or by the toxic
effects of iron deposition in tissues. As reported by a
study conducted by Aydinok et al, although the risk
of developing short stature was lower among children
receiving the oral chelator, they reported decreased of
stature in adolescent receive iron chelators after age
10 years for 3 years, therefore, an eventual positive
effect of oral chelators on growth does not seem to be
sufficient when started after age 10 years (Aydinok Y
et al., 2012).Some of our subjects (30.4%) were
without therapy of iron chelator treatment and maybe
it may be caused by lack of parental or children
compliance to protocol treatments that have been
made to patients. Therefore, all thalassemia patients
should be adherence to all treatments such as
regularly transfusion and use iron chelation agents,
and avoidance of iron chelator overdosage clearly
reduced the risk for short stature and other
thalassemia complications.
5
CONCLUSION
The results of this study demonstrated that there was
nosignificant association between serum ferritin
levels and short stature, but this result showed
significant association between age at diagnosis and
short stature, it means that they are suffering from
growth disorder since the beginning of their life.
Therefore, new planning and policies seem to be
necessary to minimize the complications in patients
with beta thalassemia major. Some of the
recommended plans include improvement of blood
transfusion protocols, chelation therapy, informing
the parents and patients about the complications of
iron overload in the endocrine glands. We suggest
that all patients be examined at an early age in terms
of growth every six months.
ACKNOWLEDGMENTS
The authors gratefully acknowledge that the present
research is supported by Ministry of Research and
Technology and Higher Education Republic of
Indonesia. The support is under the research grant
TALENTA USU of year 2018, contract number
139/UN5.2.3.1/PPM/KP-TALENTA USU/2018.
REFERENCES
Ansari Sh, Baghersalimi A, Azarkeivan A, Nojomi M,
Hassanzadeh Rad A. Quality of life in patients with
thalassemia major. Iran J PediatrHematoOncol. 2014;
4: 57-63.
Hashemi A, Ghilian R, Golestan M, Akhavan GM, Zare Z,
Dehghani MA. The study of growth in thalassemic
patients and its correlation with serum ferritin level.
Iran J PediatrHematoOncol. 2011; 1: 147-51.
Nasr MR, Ebrahim NA, Ramadan MS, Salahedin O.
Growth pattern in children with beta-thalassemia major
and its relation with serum ferritin, IGF1 dan IGF BP3.
J ClinExp Invest. 2012; 3: 157-63.
De Sanctis V, Soliman AT, Elsedfy H, Skordis N, Kattamis
C, Angastiniotis M, et al. Growth and endocrine
disorders in thalassemia: The international network on
endocrine complications in thalassemia (I-CET)
position statement and guidelines. Indian J
EndocrinolMetab. 2013; 17: 8-18.
Ogden CL, Flegal KM. Changes in terminology for
childhood overweight and obesity. U.S Department of
Health and Human Services, Centers for Disease
Control and Prevention, National Center for Health
Statistics. Natl Health Stat Report. 2010; 25: 1-6.
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
896

Al-salehe QAA, Al-Awady MS, Abbas SK. Growth
retardation inβ-thalassemia major. Iraqi Postgrad Med
J. 2015; 14: 267-73.
Fadlyana E, Ma’ani F, Elizabeth M, Reniarti L. Correlation
between serum ferritin level and growth disorders in
children with thalassemia. Am J Clin Med Res. 2017;
5: 31-5.
Badfar G, Nasirkandy MP, Shohani M, Mansouri A,
Shabani E, Rahmati S, et al. Prevalence of short stature,
underweight, and delayed puberty in Iranian patients
with thalassemia major: A systematic review and meta
analysis. Iran J PedHematolOncol. 2017; 7: 245-59.
Hamidah A, Rahmah R, Azmi T, Aziz J, Jamal R. Short
stature and truncal shortening in transfusion dependent
thalassemia patients: Results from a thalassemia center
in Malaysia. Southeast Asian J Trop Med Public
Health. 2001; 32: 625-30.
Shlomit, Doron C, Naomi W. Serum ferritin level as a
predictor of impaired growth and puberty in
thalassemia major patients. Eur J Haematol. 2005; 74:
93-100.
Borgna-Pignatti C, De Stevano P, Zonta L, Vullo C, De
Sanctis V, Melevendi C, et al. Growth and sexual
maturation in thalassemia major. J Pediatr. 1985; 106:
150-5.
Gomber S, Dewan P. Physical growth patterns and dental
cares in thalassemia. IndPediatr. 2006; 43: 1064-9.
Shamshirsaz AA, Bekheirnia MR, Kamgar M,
Porzahedgilani N, Bouzari N, Habibzadeh M, et al.
Metabolic and endocrinologic complications in beta-
thalassemia major: A multicenter Study in Tehran.
BMC Endocrine Disorders. 2003; 3: 1-6.
Al-Wataify AS. Growth retardation among multi-
transfused thalassemia center in Babylon Governorate.
Med J Babylon. 2012; 4: 815-23.
Nesheli HM, Farahanian E. Relation between bone mineral
density and serum ferritin levels in patients with
thalassemia major. Caspian J Pediatr. 2016;2: 158-63.
Moayeri H, Oloomi Z. Prevalence of growth and puberty
failure with respect to growth hormone and
gonadotrophins secretion in beta-thalassemia major.
Arch Iranian Med. 2006; 9: 329-34.
Shalitin S, Carmi D, Weintrob N, Philip M, Miskin H,
Kornreich L, et al. Serum ferritin level as a predictor of
impaired growth and puberty in thalassemia major
patients. Eur J Haem. 2005; 74: 93-100.
Jahargidar R, Parikh S, Deshpande R, Lalwani. Growth
profile of children with thalassemia major. Indian J
Appl Res. 2017; 7: 724-6.
Yaman A, Isik P, Yarali N, Karademir S, Cetinkaya S, Bay
A, et al. Common complications in Beta-Thalassemia
Patients. Int J HematolOncol. 2013; 23: 193-9.
Origa R, Danjou F, Orecchia V, Zappu A, Dessi C, Foschini
ML, et al. Current growth patterns in children and
adolescents with thalassemia major. Blood. 2016; 128:
2580-2.
Aydinok Y, Unal S, Oymak Y, et al. Observational study
comparing long-term safety and efficacy of deferasirox
with desferrioxamine therapy in chelation naïve
children with transfusional iron overload. Eur J
Haematol. 2012; 88: 431-43
Relationship between Short Stature and Serum Ferritin in Children with Beta Thalassemia Major
897
