
Platelet Profile Distribution in Critically Ill Children
Gema Nazri Yanni
1
, Rina Amalia C. Saragih
1
1
Department of Child Health, Faculty of Medicine, Universitas Sumatera Utara, Haji Adam Malik General Hospital,
Medan, Indonesia
Keywords: Platelet, Critically Ill.
Abstract: Thrombocytopenia occurring in a critically ill patient is the result of hemodilution, increased platelet
consumption, an immune mechanism (increased platelet destruction), and increased platelet sequestration.
Previous studies showed that platelet indices might be a more useful prognostic indicator, but a study on
critically ill children is still limited. We report the platelet profile of critically ill children admitted in the
pediatric intensive care unit. This report is part of an ongoing study of the prognostic marker in critically ill
children that consist of septic and non-septic patients. All patients admitted to the pediatric intensive care
unit Haji Adam Malik Hospital and Universitas Sumatera Utara Hospital were recruited. We examined the
platelet profile (platelet count, Plateletcrit/PCT, Mean Platelet Volume /MPV and Platelet Distribution
Width/PDW) on the first day of admission. Of 53 samples, 29 were boys with an average age of 7.62
(+6.43) years old. Severe malnutrition was found in 12 cases (22.6%). We found platelet count median
value was 316000 (23000-828000). Median value of PCT, MPV, and PDW were 0.32 (0.08-1.40), 9.4 (7.9-
13.5), 9.7 (7.0-17.5), respectively. As the conclusion of this ongoing study, it is shown that there were
changes of platelet profile in critically ill children. Further studies studying its usefulness as a prognostic
indicator are still needed.
1 INTRODUCTION
Inflammation, regardless of its causes, is very
common during critical illness (Kellum et al, 1996).
One of the inflammation’s hallmarks is endothelial
dysfunction, which has an important role in the
pathogenesis of organ dysfunction and may be
associated with platelet activation and consumption
(Aird et al, 2003; Warkentin et al, 2003).
Studies had indicated that inflammation
associated endothelial dysfunction is one of the
causes of organ failure which is related to platelet
activation and consumption. According to these
findings, changes in platelet count are closely
associated with the prognosis of critically ill patients
(Aird et al, 2003; Vanderschueren et al, 2000;
Moreau et al, 2007).
Mean platelet volume (MPV) is defined as a ratio
of plateletcrit to platelet count and measured in
femtolitres. Larger platelets have more rapid respond
than smaller platelets, they can release chemical
mediators more readily in response either to
endogenous or exogenous stimuli (Becchi et al,
2006; Oncel et al, 2012; Gasparyan et al, 2011). The
association between changes of MPV level and
patient’s morbidity and mortality in various diseases
have been reported in several studies (Chu et al,
2010; Cho et al, 2013; Altintoprak et al, 2013;
Kandis et al, 2011; Aydemir et al, 2015; Vizioli et
al, 2009). However, studies in child population are
still limited. Only a few studies that had revealed the
association between MPV and early diagnosis
(O’Connor et al, 1993; Guida et al, 2003; Akarsu et
al, 2005; Oncel et al, 2012; Aksoy et al, 2012; Aydin
et al, 2014; Yao et al, 2015; Kim et al, 2015) or
mortality (Ahmad et al, 2014; Catal et al, 2014;
Zhao et al, 2015) of sepsis. , all of these studies were
performed in the neonatal period.
2 METHODS
This report is part of an ongoing study of a
prognostic marker in critically ill children. In this
paper, we describe the platelet profile specifically
platelet count, Plateletcrit /PCT, Mean Platelet
Volume /MPV and Platelet Distribution
Yanni, G. and Saragih, R.
Platelet Profile Distribution in Critically Ill Children.
DOI: 10.5220/0010098808870890
In Proceedings of the International Conference of Science, Technology, Engineering, Environmental and Ramification Researches (ICOSTEERR 2018) - Research in Industry 4.0, pages
887-890
ISBN: 978-989-758-449-7
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
887
Width/PDW) in critically ill children between Mei –
July 2018.
Inclusion criteria were all patients admitted to the
pediatric intensive care unit Haji Adam Malik
Hospital and Universitas Sumatera Utara Hospital
from one month until 18 years old. Patients with
malignancy, idiopathic thrombocytopenic purpura,
immunodeficiency, history of using chemotherapy
agent and refused for laboratory test were excluded.
Subjects were taken consecutively. The blood
sample was taken on the first day of admission .
Data were analyzed using SPSS version 20.
3 RESULT
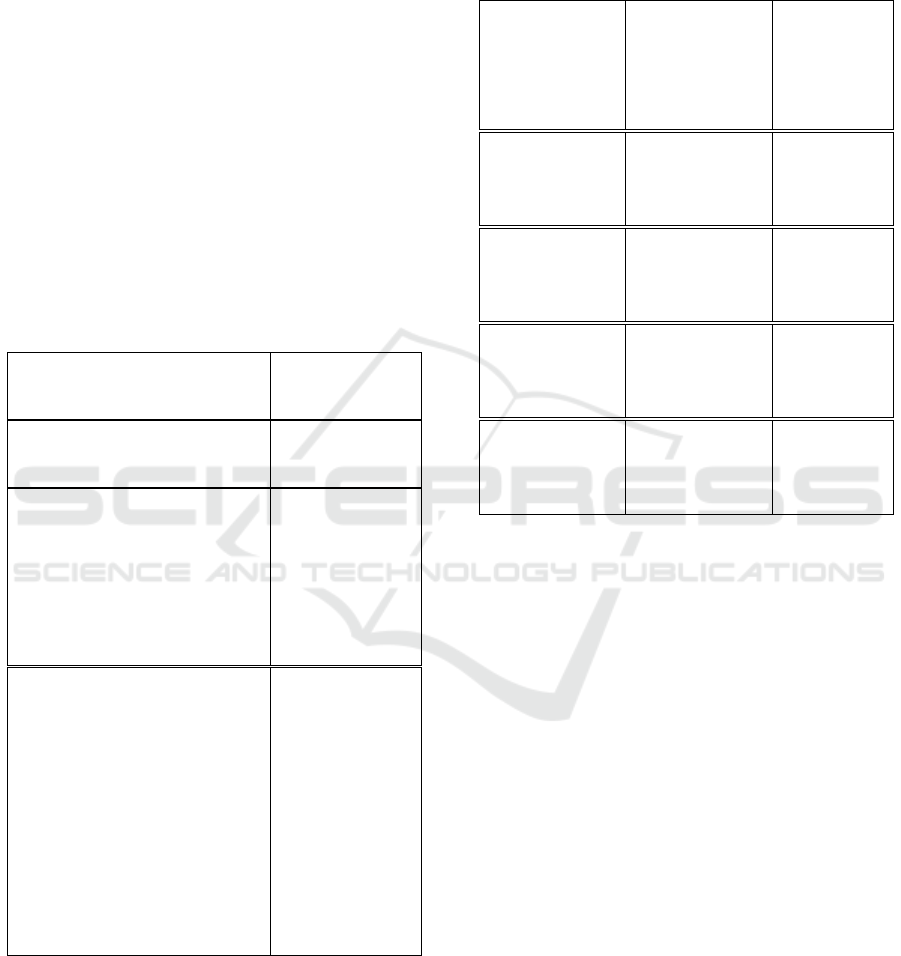
The characteristics of all patients are presented in
Table
Table 1: Subjects Characteristics
Characteristic n = 53
Age (months), mean ± SD 7,6 (± 6,43)
Gender (n, %)
Boy
Girl
29 (54,7)
24 (45,3)
Nutritional Status (n, %)
Severe
Moderate
Normal
Overweight
12 (22,6)
7 (13,21)
33 (62,26)
1 (1,89)
n = total number of subject
Table 2 shows the platelet profile’s values. We
found that platelet count have a wide range. The
minimum level was 23000/ µL
(thrombocytopenia), and the maximum level was
828000/ µL (thrombocytosis). We also found the
minimum and maximum level of PCT were out of
normal range. The maximum level of MPV was
higher than the average value. The minimum level of
PDW was lower than average value.
Table 2: Platelet Profile
Platelet profile n = 53 Normal value
(population
mean)
Platelet count
(/µL), median
(min-max)
316000
(23000–828000)
150000-
450000
PCT (%),
median
(min-max)
0,3
(0,08–1,4)
(0,1-0,5)
MPV (fl),
median
(min-max)
9,4
(7,9–13,5)
(6,5-9,5)
PDW (%),
median
(min-max)
9,7
(7,0–17,5)
(10-18)
4 DISCUSSION
Our study found that platelet profile in critically ill
children on day one of admission had abnormal
value. In this study, we found subjects with
thrombocytopenia (<15000/ µL) and also
thrombocytosis (>450000/µL). Thrombocytopenia
was found on day one of admission , and it might be
because of varies underlying disease in critically ill
children.
Thrombocytopenia is one of the most frequent
laboratory abnormalities encountered in ICU, and
the reported incidence varies from 13 to 58% in
various studies (Strauss et al, 2002; Crowther et al,
2005; Aissaoui et al, 2007; Guida et al, 2003).
Various conditions have been identified as
underlying cause of thrombocytopenia, such as
disseminated intravascular coagulation, immune
mechanisms, reduced production, increased
consumption or irregular sequestration of platelets o
r a combination of these (Bogdonof et al, 1990;
Housinger et al, 1993). PCT reflects not only the
platelet count but also platelet size. In this study, we
found that minimum and maximum level of PCT
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
888

were out of laboratory normal range that reflect the
platelet count level.
MPV level was increased in this study. Mean
platelet volume (MPV) is one of the platelet indices
which is frequently used and routinely measured in
the complete blood count test with automatic
analyzer. MPV is defined as a ratio of plateletcrit to
platelet count and is measured in femtoliters (Zhang
et al, 2014). Van Der Leile et al have shown an
increase in MPV in septicemic patients (Van der
lelie et al, 1983), he postulated that with sepsis there
is increased thrombocytosis and this result in
increased megakaryocyte ploidy and an increase in
MPV.
PDW level in this study decreased. This result
was contradict with Patrick et al who studied PDW
level in neonates with late onset sepsis. He found
that PDW increased in sepsis (Patrick et al, 1990).
Based on this result, our ongoing study will
investigate the role of the platelet profile as
prognosic factors in critically ill children.
5 CONCLUSIONS
There were changes in platelet profile distribution in
critically ill children. Further studies studying its
usefulness as a prognostic indicator are still needed.
REFERENCES
Ahmad, MS, Waheed, A., 2014. Platelet counts, MPV and
PDW in culture proven and probable neonatal sepsis
and association of platelet counts with mortality rate. J
Coll Physicians Surg Pak. 24: 340-4.
Aird, WC., 2003. The role of the endothelium in severe
sepsis and multiple organ dysfunction syndrome.
Blood. 101(10):3765–3777.
Aissaoui, Y, Benkabbou, A, Alilou, M, Moussaoui, R, El,
Hijri, A, Abouqal, R., 2007. Thrombocytopenia ina
surgical intensive care unit, incidence, risk factors and
effects on outcome. Presse Med. 36:43–9.
Akarsu, S, Taskin, E, Kilic, M., 2005. The effects of
different infectious organisms on platelet counts and
platelet indices in neonates with sepsis: is there an
organism-specific response? J Trop Pediatr. 51:388-
91.
Aksoy, HT, Eras, Z, Guzoglu, N, Canpolat, FE, Dilmen,
U., 2013. Mean platelet volume is not associated with
bacterial sepsis in newborns. Int J Infect Dis. 17:
e1263.
Altintoprak, F, Arslan, Y, Yalkin, O, Uzunoglu, Y, Ozkan,
OV., 2013. Mean platelet volume as a potential
prognostic marker in patients with acute mesenteric
ischemia-retrospective study. World J Emerg Surg. 8:
49.
Aydemir, H, Piskin, N, Akduman, D, Kokturk, F, Aktas,
E., 2015. Platelet and mean platelet volume kinetics in
adult patients with sepsis. Platelets. 26: 331-335.
Aydın, B, Dilli, D, Zenciroğlu, A, Karadağ, N, Beken, S,
Okumuş, N., 2014. Mean platelet volume and uric acid
levels in neonatal sepsis. Indian J Pediatr. 81: 1342-6.
Becchi, C, Al, Malyan, M, Fabbri, LP, Marsili, M, Boddi,
V, Boncinelli, S., 2006. Mean platelet volume trend in
sepsis: is it a useful parameter? Minerva Anestesiol.
72(9):749–56.
Bogdonoff, D, Williams, M, Stone, D., 1990
Thrombocytopenia in critically ill patient. J Crit Care.
3:186–205.
Catal, F, Tayman, C, Tonbul, A., 2014. Mean platelet
volume (MPV) may simply predict the severity of
sepsis in preterm infants. Clin Lab. 60: 1193-1200.
Chu, SG, Becker, RC, Berger, PB., 2010. Mean platelet
volume as a predictor of cardiovascular risk: a
systematic review and meta-analysis. J Thromb
Haemost. 8:148-56.
Cho, SY, Jeon, YL, Choi, SK, Suh, JT, Lee, HJ, Park, TS.,
2013. Mean platelet volume in Korean patients with
acute ischemic stroke: a gender difference. Platelets.
24:75-6.
Crowther, MA, Cook, DJ, Meade, MO, Griffith, LE,
Guyatt, GH, Arnold, DM., 2005. Thrombocytopenia in
a medical-surgical critically ill patients: Prevalence,
incidence and risk factors. J Crit Care. 20:348–53.
Gasparyan, AY, Ayvazyan, L, Mikhailidis, DP, Kitas,
GD., 2011. Mean platelet volume:a link between
thrombosis and inflammation? Curr Pharm Des.
17(1):47–58.
Guida, JD, Kunig, AM, Leef, KH, McKenzie, SE, Paul,
DA., 2003. Platelet count and sepsis in very low birth
weight neonates: is there an organism-specific
response? Pediatrics. 111: 1411-5.
Housinger, T, Brinkerhoff, C, Warden, G., 1993. The
relationship between platelet count, sepsis and survival
in pediatric burn patients. Arch Surg. 128:65–7.
Kandis, H, Ozhan, H, Ordu, S., 2011. The prognostic
value of mean platelet volume in decompensated heart
failure. Emerg Med J. 28: 575-578.
Kellum, JA, Decker, JM., 1996. The immune system:
relation to sepsis and multiple organ failure. AACN
Clin Issues. 7(3):339–50. quiz 459–360.
Kim, JY, Yoon, J, Lim, CS, Choi, BM, Yoon, SY., 2015.
Clinical significance of platelet-associated
hematological parameters as an early supplementary
diagnostic tool for sepsis in thrombocytopenic very-
low-birth-weight infants. Platelets. 26: 620-6.
Moreau, D, Timsit, JF, Vesin, A., 2007. Platelet count
decline: an early prognostic marker in critically ill
patients with prolonged ICU stays. Chest. 131: 1735-
41.
O’Connor, TA, Ringer, KM, Gaddis, ML., 1993. Mean
platelet volume during coagulase-negative
staphylococcal sepsis in neonates. Am J Clin Pathol.
99: 69-71.
Platelet Profile Distribution in Critically Ill Children
889

Oncel, MY, Ozdemir, R, Yurttutan, S., 2012. Mean
platelet volume in neonatal sepsis. J Clin Lab Anal.
26(6): 493-6.
Patrick, CH, Lazarchick, J. The effect of bacteremia on
automated platelet measurements in neonates. Am. J.
Clin. Pathol. 93(3):391–4.
Strauss, R, Wehler, M, Mehler, K, Kreitzer, D,
Koebnick, C, Hahn, E., 2002. Thrombocytopenia in
patients in the Medical Intensive Care Unit:
Bleeding prevalence, transfusion requirement and
outcome. Crit Care Med. 30:1765–71.
Van, der, Lelie, J, Von, dem, Borne, AK., 1983.
Increased mean platelet volume in septicaemia. J.
Clin. Pathol. 36(6):693–6.
Vanderschueren, S, De, Weerdt, A, Malbrain, M., 2000.
Thrombocytopenia and prognosis in intensive care.
Crit Care Med. 28: 1871-6.
Vizioli, L, Muscari, S, Muscari, A., 2009. The
relationship of mean platelet volume with the risk
and prognosis of cardiovascular diseases. Int J Clin
Pract. 63: 1509-15.
Warkentin, TE, Aird, WC, Rand, JH., 2003. Platelet-
endothelial interactions: sepsis,HIT, and
antiphospholipid syndrome. Hematology Am Soc
Hematol Educ Program. 2003(1):497–519.
Yao, Y, Tu, Y, Lu, Q., 2015. Values of C-reactive
protein, percentage of neutrophils and mean platelet
volume in early diagnosis of neonatal sepsis.
Zhongguo Dang Dai Er Ke Za Zhi. 17: 425-9.
Zhang, Z, Xu, X, Ni, H, Deng, H., 2014. Platelet indices
are novel predictors of hospital mortality in intensive
care unit patients. J Crit Care. 29: 885.e1-6.
Zhao, D, Qiu, G, Luo, Z, Zhang, Y., 2015. Platelet
parameters and (1,3)-β-D-glucan as a diagnostic and
prognostic marker of invasive fungal disease in
preterm infants. PLoS One. 10: e0123907.
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
890
