
Characteristic Description of Multiparous Women
with
Mycoplasma hominis
and
Ureaplasma urealyticum
Infection
at Outpatient Clinic in Medan
L. Feriyawati
1
, D. R. Anggraini
1
and T. A. Nasution
2
1
Anatomic Department, Medical Faculty, Universitas Sumatera Utara, Medan,
Indonesia
2
Microbiology Department,Medical Faculty, Universitas Sumatera Utara, Medan,Indonesia
Keywords: Mycoplasma hominis, Ureaplasma urealyticum, Multiparous Women.
Abstract:
Among the organisms that cause genital infection are
Mycoplasma hominis
and
Ureaplasma urealyticum
which
are commensally in women
urogenital
but may become pathogens and were associated as a cause of
complications of genital tract infection in pregnant women, such as ascending chorioamnionitis, premature
rupture of membranes, preterm birth, miscarriage, weight and neonatal birth low and newborn deaths..The
objective of this study was to describe the characteristic of multiparous women with
Mycoplasma hominis
and
Ureaplasma urealyticum
infection. Design of the study
was
a descriptive study with cross-sectional approach
by
collecting cervical swab of 50 multiparous women
from
outpatient clinic in Medan. Duplex PCR assay was
perfomed using two primers: RNAH1 and RNAH2 that amplify the 16sRNA
M. Hominis
gene at 334bp;
UMS125 and UMA226 amplifying serovar3 genes multiple banded antigen which can amplify biovar1 that
appeared at 403bp and biovar2 appeared at 448bp. The result of this study showed
Mh-Uu
duplex PCR results
revealed that 3(6.0%) respondents were positive Mycoplasma infection and 9(18%) respondents were positive
Ureaplasma infection and 5(10.0%) from infected respondents had abortion history.
1 INTRODUCTION
Mycoplasma hominis and Ureaplasma spp. is a
commensal organism that found in 30-80% women’s
urogenital tract, thus causing urogenital tract
infection. In pregnant woman, these organisms could
stay in utero and then transmission by placenta to the
fetus, causing several infections and trigger
premature labor (Otgonjargala, 2017). In rare cases
these microorganisms may infect the central nervous
system in healthy neonates and present a risk of
severe complications and poor prognosis
(Wildenbeest, 2016). The role of these pathogens in
women with chronic urinary tract symptoms remains
a problem due to difficult to detect and its
intracellular nature makes conventional antibiotics
ineffective (Nasution, 2007).
Polymerase Chain Protein (PCR) analysis of
these bacteria should be performed if symptomatic
sterile leukocytosis is present, chronic urethritis
and bladder hyperactivity or interstitial cystitis/
painful bladder syndrome, recurrent infections or if
microbiological culture is negative (Combaz-
Söhnchen, 2017). The difficulty of detecting M.
hominis on persistent neonatal CNS infections with
unknown causes requires diagnostic protocols using
a specific real-time PCR. Physicians should be
aware of the pathogens as possible causes of
neonatal meningoencephalitis if corrective failure is
found in empirical antibiotic treatment
(Wildenbeest, 2016).
A study by Manhart et al, 2003, found that from
719 young women Mycoplasma genitalium was
detected as much as 50 (7%) in a sample previously
negative for bacterial vaginosis. Nasution et al, 2007,
in 40 Malaysia women, used duplex PCR Mh / Uu
method (Mycoplasma hominis/ Ureaplasma
urealyticum) and showed that Ureaplasma is the most
commonly discovered pathogen (positive in 90.5% of
women and 47.5% of newborns), followed by
Mycoplasma (32.5% and 7.5%), and the rest are
chlamydia, trichomonas and gonococcus.
The purpose of this study is to describe the
characteristic of multiparous women with
Feriyawati, L., Anggraini, D. and Nasution, T.
Characteristic Description of Multiparous Women with Mycoplasma hominis and Ureaplasma urealyticum Infection at Outpatient Clinic in Medan.
DOI: 10.5220/0010093108370840
In Proceedings of the International Conference of Science, Technology, Engineering, Environmental and Ramification Researches (ICOSTEERR 2018) - Research in Industry 4.0, pages
837-840
ISBN: 978-989-758-449-7
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
837

Mycoplasma hominis and Ureaplasma urealyticum
infection detected by using duplex PCR method.
2 METHOD
2.1 Study Design
The study design is cross sectional with observational
approach.
2.2 Study Area
This study was conducted at an outpatient clinic in
Medan North Sumatera in 2018.
2.3 Sampling
Protocol of this study has been approved by Medical
Ethics Committee Universitas Sumatera Utara
(No.375/TGL/KEPK FK USU-RSUP HAM/2018)
2.2.1 Respondents Characteristics
Respondents were 50 female adolescents,
multiparity, age above 18 years and signed the
informed consent.
3 DATA COLLECTION
3.1 Socio-demographics Background
A questionnaire consist of social demographics, using
contraception, first age of sexual intercourse and
history of abortion was administered by self-reports
of the participants,
3.2 Sample Collection and Laboratory
Processing
3.2.1 DNA Extraction
Cervical swabs from 50 respondents on the micro
tube contained 0.9% NaCl firstly centrifuged at a
speed of 14,000rpm for 4 minutes. The precipitated
portion is added to 1.5 ml of the PBS (phosphate
buffer salin). After that tube were repeating
centrifuged at a speed of 14.000 rpm for 4 minutes.
Furthermore, a DNA isolation procedure is performed
based on the protocol of the Invitrogen® kit. There
are 200 µL sample inserted into another micro tube.
Moreover, inside the tube was added 20 µL of
proteinase K and 200 µL of lysis buffer, then vortexed
for a few minutes. After that, the tube was incubated
at 55°C for 10 minutes. Followed step is the tube were
added 250 µL ethanol 96%, then vortexes for 15
seconds and move the fluid into the column spin.
Then the column was centrifuged at 10.000 rpm for 2
minutes. After that, replace the collection tube, then
washed with 500 µL wash buffer 1. Centrifuged at
10.000rpm for 2 minutes. Next step was replacing the
collection tube then washed again with 500 µL wash
buffer 2, centrifuge with maximum speed
(14.000rpm) for 3 minutes. Finally, replaced the
collection tube again and added 50 µL delution
buffer, then tube was centrifuged at 14.000rpm for 1.5
minutes.
3.2.2 Mycoplasma hominis and Ureaplasma
urealyticum Detection
M. hominis and U.urealyticum duplex PCR (Mh-Uu
duplex PCR), using 2 primers: RNAH1 and RNAH2
that amplify the 16sRNA M. hominisgene at 334 bp;
UMS125 and UMA226 amplifying serovar 3
genes multiple banded antigen which can amplify
biovar1 that appeared at 403 bp and biovar 2 appeared
at 448 bp. The amplification mixture was carried out
in 12,5l master mix PCR which consists of Taq
polymerase enzyme, MgSO
4
, and dNTP (Go Taq®
PCR Core System, Promega); 7,5 l nuclease-free
water and 4l DNA template. PCR was performed in
a thermocycler (Verity 96-well Thermal Cycler,
AppliedBiosystems) with an initial denaturation
94
o
C for 1 minute 30 seconds, annealing in 55
o
C for
2 minutes, extension for 1 minute 30 seconds and
ending with a final extension step at 72
o
C (Nasution
2007).
4 RESULTS AND DISCUSSION
4.1 Socio-demographics Background
In this study, respondents mostly women between 35-
40 years old (66%), followed by women above 45
years old (22%) and the least under 35 years old
(12%). Most respondents were housewife (58%)
Respondents whose using contraception accounted
for 26%. The first age of sexual intercourse was found
mostly women between 26-30 years old (56%),
following women between 20-25 years old (40%) and
the least were under 20 years old (4%). The
respondents whose having abortion history accounted
for 23%.
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
838
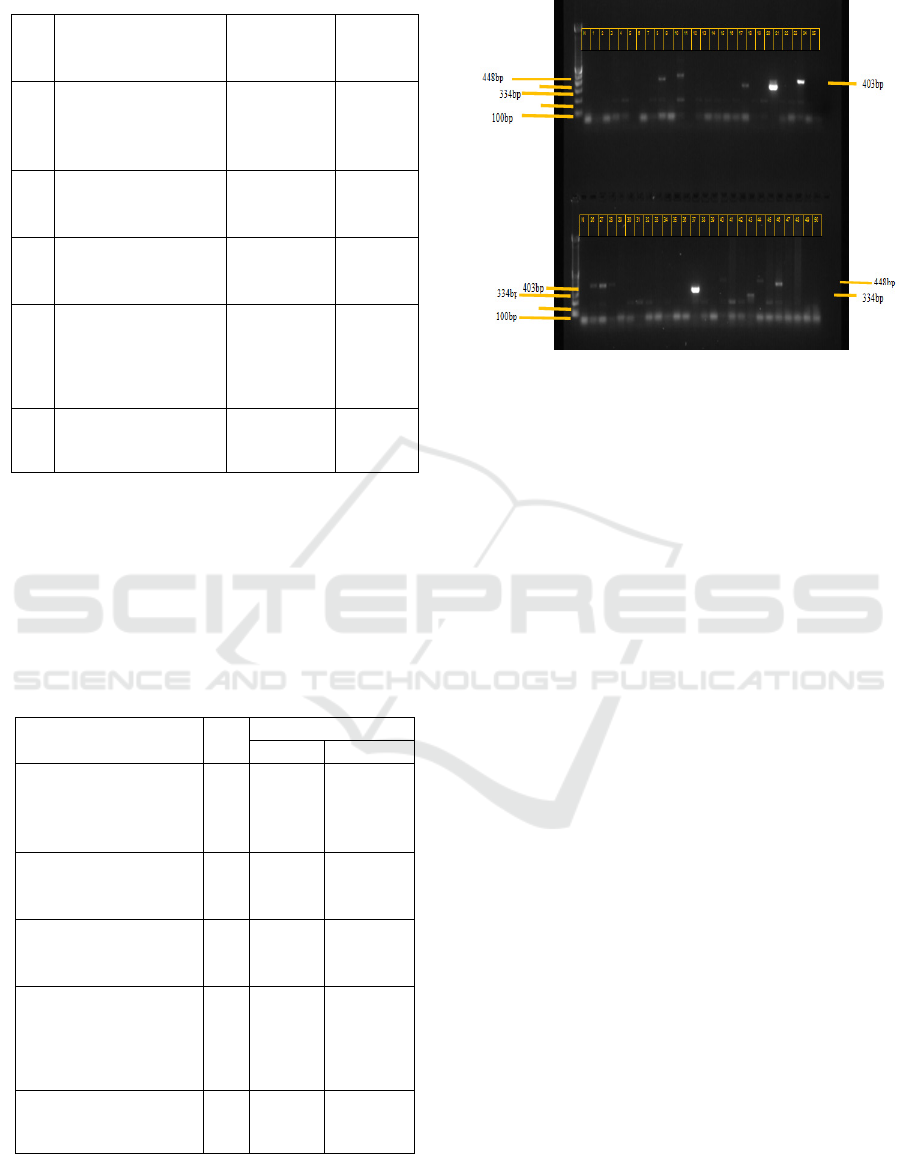
Table 1: Socio-demographics characteristic
No Socio-demographics
characteristic
Number of
Respondent
(n=50)
%
1 Age
< 35 years
35-40 years
> 45 years
6
33
11
12.0
66.0
22.0
2 Occupation
Working woman
Housewife
21
29
58.0
42.0
3 Use of contraception
Yes
No
13
37
26.0
74.0
4
First age of sexual
intercourse
< 20 years old
20 – 25 years old
26 – 30 years old
2
20
28
4.0
40.0
56.0
5
History of abortion
Yes
No
23
27
46.0
54.0
4.2 Polymerase Chain Protein
Mh-Uu duplex PCR results revealed that 3(6.0%)
respondents were M. hominis positive and 9(18.0%)
respondents were U. urealyticum positive (Figure. 1)
Table 2: Distribution of detection Mycoplasma hominis
(Mh) and Ureaplasma urealyticum (Uu) using Duplex PCR
n No (%) Detection
Mh Uu
Age
< 35 years
35-40 years
> 45 years
6
33
11
1(16.0)
2(6.06)
0
2(33.0)
4(12.1)
3(27.2)
Occupation
Working woman
Housewife
21
29
0
3(10.3)
4(19.0)
5(17.2)
Use of contraception
Yes
No
13
37
0
3(8.1)
2(15.4)
7(0.2)
First age of sexual
intercourse
< 20 years old
20 – 25 years old
26 – 30 years old
2
20
28
0
1(5.0)
2(7.1)
0
6(30.0)
3(10.7)
History of abortion
Yes
No
23
27
3(13.0)
0
2(8.7)
7(25.9)
Figure 1: Mh-Uu duplex PCR results of 50 respondents
This study found that the respondents who had
Mycoplasma infection were all housewives with the
most 35-40 years old range. It is interesting that
almost all respondents have had abortion; even one of
the respondents had experienced abortion twice.
While respondents who have Ureaplasma infection
were most are housewives with the most age range
35-40 years old. Abortion history is also found in this
group who was 2 respondents ever aborts 1 time.
This study was consistent with another previous
study conducted in a cohort of females with bacterial
vaginosi (BV) or asymptomatic, in which U.
urealyticum infection was detected significantly more
often than M. Hominis (Verteramo, 2013 and Padang,
2015)
The high prevalence of Ureaplasma spp. infection
was also found according to previous study in Brazil
with 6,810 patients with the age range of 11 to 80
years who in gynecological routine examination,
found that M. hominis (n = 79), Ureaplasma spp. (n =
2,026) and the co-colonization of both (n = 199)
which extract from cytological sample and detect by
PCR (Milanezi, 2016). Another study in Iran using
multiplex PCR to urine and genital samples from
symptomatic females (20-54 years old), found that
the highest incidence of M. hominis and U.
urealyticum and were highly associated with habitual
abortion in symptomatic females (Maleki, 2013). The
inconsistent result found in case control study in Iran
which conclude that no association between
mycoplasma infection and spontaneous abortion
(Ramazanzadeh, 2016).
Characteristic Description of Multiparous Women with Mycoplasma hominis and Ureaplasma urealyticum Infection at Outpatient Clinic in
Medan
839

5 CONCLUSION
This study has revealed that from 50 multiparous
women, 3(6.0%) were positive Mycoplasma infection
and 9(18.0%) were positive Ureaplasma infection and
had abortion history. Further research is needed to
explore whether the cause of their previous abortion
was associated with this bacterial infection. Early
screening is needed to detect bacterial infection of M.
hominis and U. urealyticum in pregnant women with
a history of preterm and premature rupture of
membranes, thus decreasing the complication of this
infection to newborns’ morbidity and mortality
ACKNOWLEDGMENTS
The authors would like to thank the funding support
from the Universitas Sumatera Utara.
REFERENCES
Combaz-Söhnchen, N., Kuhn, A., 2017. A systematic
review of Mycoplasma and Ureaplasma in
urogynaecology. Geburtshilfe Frauenheilkd; 77(12):
1299–1303
Maleki, S., Motamedi, H., Moosavian, S.M., Shahbaziyan,
N., 2013. Frequency of Mycoplasma hominis and
Ureaplasma urealyticum in females with urogenital
infections and habitual abortion history in Ahvaz, Iran;
using multiplex PCR. Jundishapur Journal of
Microbiology. 6(6); Aug; e10088.
Manhart, L.,E., Dutro, S.M., Holmes, K.K., 2001.
Mycoplasma genitalium is associated with
mucopurulent cervicitis. Int J STD AIDS; 12(Suppl
2):69
Milanezi, F., Falconi, A., Schnabel, B., Ricardi, L.R.,
Monfredini, P.M., Ziliotto, A.T., Lopes, V.F.,
Machado, S.A., Oliveira, M.J., Centrone, C.C., Nakano,
V., 2016. Prevalence of Mycoplasma hominis and
Ureaplasma spp. in routine gynecological care in Sao
Paulo City, Brazil. Arch Clin Infect Dis.; 11(3):e36668.
Nasution, T.A., Cheong, S.F., Lim, C.T., Leong, E.,
Ngeow, Y.F., 2007. Multiplex PCR for the detection of
urogenital pathogens in mothers and newborns.
Malaysian J Pathol; 29(1): 19 – 24
Otgonjargala, B., Becker, K., Batbaatar, G., Tsogtsaikhan,
S., Enkhtsetseg, J., Enkhjargal, A., Pfeffer K., Adams
O., Battogtokh C., Henrich B., 2017. Effect of
Mycoplasma hominisand Cytomegalovirus infection on
pregnancy outcome: A prospective study of 200
Mongolian women and their newborns. PLoS ONE
12(3): e0173283
Padang, C., Jacob, T.N.A., Nilasari, H., Daili, S.F., 2015.
Prevalence of Mycoplasma hominis and Ureaplasma
urealyticum infection in female sex workers and its
association with douching: a study in East Jakarta,
Indonesia using Mycoplasma System Plus. J Gen Pro
DVI;1(1):1–8.
Ramazanzadeh R., Khodabandehloo, M., Farhadifar, F.,
Rouhi, S., Ahmadi, A., Menbari, S., Fallahi, F.,
Mirnejad, R., 2016. A case control study on the
relationship between Mycoplasma genitalium infection
in women with normal pregnancy and spontaneous
abortion using Polymerase Chain Reaction. Osong
Public Health Res Perspect; 7(5), 334e338
Verteramo, R., Patella, A., Calzolari, E., Recine, N.,
Marcone, V., Osborn, J., 2013. An epidemiological
survey of Mycoplasma hominis and Ureaplasma
urealyticum in gynaecological outpatients, Rome, Italy
Epidemiol Infect;141(12):2650–7
Wildenbeest, J.G., Said, I., Jaeger, B., van Hest,R.M., Van
de Beek, D., Pajkrt, D., 2016. Neonate with
Mycoplasma hominis meningoencephalitis given
moxifloxacin. Lancet Infect Dis;16: e261–66
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
840
