
Advances in Endovascular Neurosurgery Techniques: Toyama
Hospital Experience
Steven Tandean
1
1
Department of Neurosurgery, Universitas Sumatera Utara, Medan, North Sumatera, Indonesia
Keywords: Endovascular, Angiography, Anastomosis, Moya-Moya Disease.
Abstract: Advance developing technologies of neurosurgery field in the world especially endovascular treatment and
vascular surgery. Endovascular treatment has new technique in internal carotid stenosis, basilar tip aneurysm,
and carotid cavernous aneurysm. Effectiveness and safety of endovascular treatment not inferior compare to
open surgery and for some cases more superior. The only management for moyamoya disease is surgical
revascularization by direct bypass, indirect bypass, and combined bypass. Most of the previous procedures
were aimed on MCA territory so EDMAPS was developed to revascularize ACA territory by using frontal
pericranial flap for additional indirect bypass through medial frontal craniotomy. Studies demonstrates STA-
MCA anastomosis and EDMAPS is safe and effective to improve long term prognosis in moyamoya disease.
1 INTRODUCTION
Vascular neurosurgery has remarkable of
neurosurgical advances that require decision making,
critical care support, microsurgical skill, and
advanced technology. This field has evolved for this
past several decades and changed the nature of this
subspecialty of neurosurgery. In 1937 the first
aneurysm clipping procedure was performed by
Walter Dandy and evolved progression of devices
and techniques. Aneurysm sac obliteration by
endovascular insertion of silver wire was reported in
1941. Evolution of endovascular treatment was
continue by development of detachable device,
balloon and stent-assisted coiling, and recently flow
diverter. Vascular neurosurgery should be a field
oriented on disease and not procedure. At present,
vascular neurosurgery requires extraluminal and
endoluminal approach. The extraluminal approach is
an open cranial microsurgical technique involves
clipping, cortical mapping, and anastomosis. The
endoluminal approach is a technique requires
microcatheter, coils, balloon systems, embolic
materials, and stent technology
(Tjoumakaris et al,
2011; Crocker, 2007).
2 ENDOVASCULAR
NEUROSURGERY
2.1 Internal Carotid Artery Stenosis
Many clinical trials have been done to compare
carotid endarterectomy with carotid artery stenting
(CAS) in regard to their effectiveness and safety.
Most studies show that CAS is not inferior compare
to carotid endarterectomy. Currently there are three
types of cerebral embolic protection devices (EPD):
Flow preservation devices with distal filters, distal
occlusion devices, and proximal protection device by
flow stasis or flow reversal. Neurosurgery department
of Toyama University hospital has policy that
asymptomatic carotid artery >80% treat by CAS
(Gahremanpour, 2012).
Carotid stenosis cases will be analyzed by
magnetic resonance imaging (MRI) and diagnostic
digital subtraction angiography (DSA). DSA will be
performed with addition of three-dimensional
rotational angiography and 3D shaded surface
displays (SSDs). Two imaging modalities will
improve accuracy of the diagnosis and plan for
treatment. DSA can evaluate the entire carotid artery
system about tandem atherosclerotic disease, plaque
morphology, collateral circulation, and lesion
associated with atherosclerotic disease can be done
Tandean, S.
Advances in Endovascular Neurosurgery Techniques: Toyama Hospital Experience.
DOI: 10.5220/0010087607550759
In Proceedings of the International Conference of Science, Technology, Engineering, Environmental and Ramification Researches (ICOSTEERR 2018) - Research in Industry 4.0, pages
755-759
ISBN: 978-989-758-449-7
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
755

by DSA. MRI was used to evaluate consistency of the
plaque by T1 and TOF (Adla, 2015).
Figure 1: A. Plaque in T1 sagittal MRI image (arrow). B.
Plaque in TOF axial MRI image (arrow). C. ICA stenosis
showed by 3D angiography (arrow). D. Lateral unsbtracted
angiographic view during angioplasty using du protection
with flow reversal: CCA (arrowhead) and ECA (small
arrow) occluded with balloon and distal filter (big arrow).
E. CCA angiography after stenting.
Carotid stenosis with large and soft plaque
(unstable plaque) was treated using dual protection
device (simultaneous flow reversal and distal filter)
and blood aspiration. Using EPD with only distal
filter or proximal balloon protection by flow stagnant
or flow reversal might not be sufficient to prevent
debris migrating to intracranial artery because
potential distal embolization by large and soft plaques
is high. Dual protection during CAS can cause debris
floating between the distal filter and the proximal end
of the stent so blood aspiration was performed after
post-dilation stent (Sakamoto, 2015).
Figure 2: A. A 9 Fr occlusion balloon-guiding catheter in
femoral artery connected to 4 Fr sheath in femoral vein via
filter and line for manual blood aspiration (asterisk). B.
Visible debris captured by the filter from AV shunt line.
(Image used with permission from Akioka N. (2016).
Textbook of JSNET educational seminar, Kobe).
All CAS procedures were performed under local
anesthesia and using heparin to maintain activated
clotting time between 250-300 seconds. Purpose of
using local anesthesia is to enable neurologic
examination during procedure. A 4 Fr sheath was
placed into the left femoral vein and 9 Fr occlusion
balloon-guiding catheter (OPTIMO; Tokai Medical
Products, Aichi, Japan) was introduced into the
common carotid artery (CCA) via right femoral
artery. An external arteriovenous (AV) shunt line was
created by connecting 9 Fr occlusion balloon-guiding
catheter with 4 Fr sheath via the blood filter to capture
debris. The line from AV shunt line was made for
manual blood aspiration. The balloon wire system
(GuardWire; Medtronic, Minneapolis, MN, USA)
was introduced into the external carotid artery (ECA)
and continuously inflated during procedure. Blood
flowed to venous circulation through AV shunt line
was confirmed after occlusion in the CCA and ECA
because of difference pressure of arterial and venous
(flow reversal). Distal filter using FilterWire EZ
(Boston Scientific, Natick, MA, USA) passed
through stenotic lesion and deployed into distal
internal carotid artery (ICA). After dual protection
was created with simultaneous flow reversal, stenotic
lesion was pre-dilated then performed blood
aspiration manually through AV shunt line about 30
cc using 50 cc syringe. Balloon in CCA was deflated
after aspiration to reduce duration of brain ischemia.
After inflation of CCA balloon, self-expanding stent
(Carotid Wallstent; Boston Scientific or PRECISE;
Johnson & Johnson, Miami Lakes, FL, USA) was
deployed from distal stenotic lesion to the CCA and
post-dilatation was performed. Manual blood
aspiration through AV shunt line about 30 cc using 50
cc syringe was performed repeatedly until absence of
debris from aspirated blood then CCA and ECA
balloon deflated. EC balloon and distal filter was
retrieved and the CAS procedure was completed.
2.2 Basilar Tip Aneurysm
Aneurysms in posterior circulation are considered as
the most hazardous location and also been long
considered as the most difficult lesion to treat by
surgery. Treatment of posterior circulation aneurysms
has shifted from microsurgery to endovascular during
past decade. Microsurgical clipping in this region
need aggressive cranial base resection and has high
risk of perforator infarction and cranial nerves
neuropathy. While endovascular treatments using
coils with stent or balloon assistance are considered
easier and more benign. Microsurgical clipping is
considered as secondary alternative when
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
756

endovascular treatment is not possible especially for
both ruptured and unruptured aneurysms at basilar
trunk, proximal anterior inferior cerebellar artery, or
vertebrobasilar junction region (Sanai, 2008).
Important issue for endovascular treatment is
aneurysm recanalization, with approximately 20%
recanalized and 10% need retreatment. Quality of
aneurysm occlusion was mostly depended on the
neck size. Wide-neck aneurysm was treated with stent
assisted coiling and study show significantly decrease
need to retreatment and increase long-term
anatomical stability. For recent years, wide-necked
aneurysm on bifurcation artery like basilar tip was
treated using Y-stenting technique. Y-stenting
technique is Y-configuration double stent using
combination of open-open, open-closed, or closed-
closed stent with preserving parent artery circulation.
This technique shown good outcomes with low
complications but it’s technically complex and has
various challenges. Invention of braided stent with
compliant and flexible closed-cell design enable to
perform single stent assisted coiling at the wide-neck
bifurcation aneurysm (Alghamdi, 2016; Du, 2016).
At neurosurgery department of Toyama
University hospital, unruptured basilar tip aneurysms
are treated with single stent assisted-coil jailed-
catheter technique using Low-profile Visualized
Intraluminal Support Junior device (LVIS Jr;
MicroVention-Terumo, Tustin, California, USA) that
are dedicated for small parent artery from 2 to 3.5
mm. Single stent assisted coiling using LVIS Jr can
be obtained by placing from one of the branch arteries
to the parent artery with pull and push technique. All
procedure was performed in general anesthesia and
by using heparin to maintain activated clotting time
between 250-300 seconds. Procedures were using
standard 6 Fr guiding catheter from one or both
femoral arteries depend on the vertebral artery
diameter, for small size vertebral artery both femoral
artery will be used.
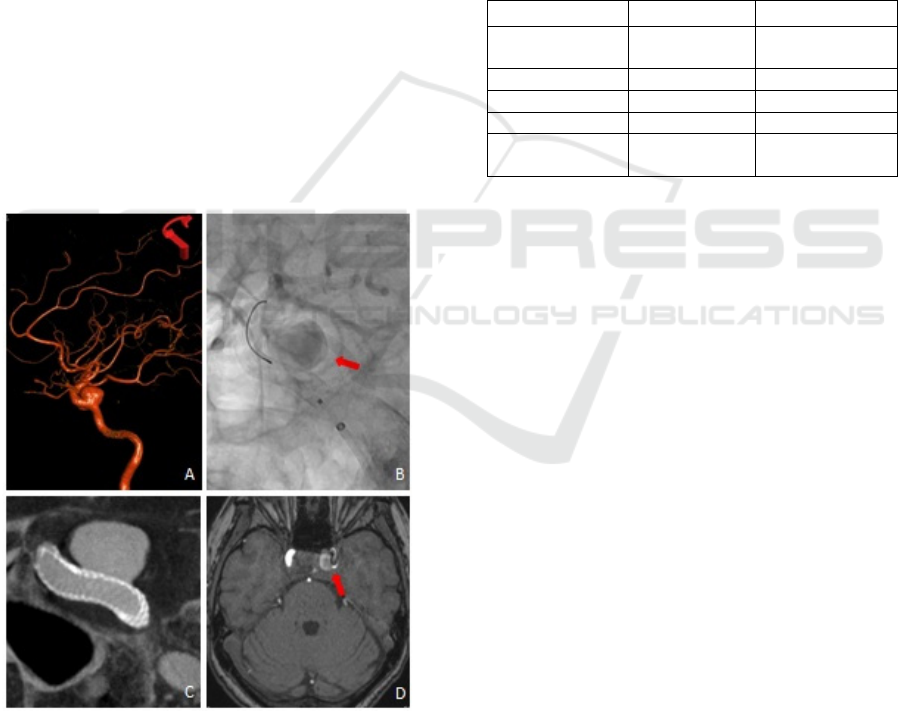
Figure 3: A. Wide-necked basilar tip aneurysm showed by
3D angiography (arrow). B. Coil (arrowhead) was partially
inserted to the sac and stent (arrow) was deployed use ‘push
and pull’ technique until cover all the neck. C. Stent (arrow)
was fully deployed and embolizing with coils (arrowhead).
D. Complete occlusion of Aneurysm (arrowhead).
Headway 21 microcatheter (Microvention-
Terumo) will be used for LVIS Jr stent. First,
Headway 21 microcatheter will be accessed to one of
distal arteries. After that, other microcatheter that
used to coil will be place in the aneurysm sac. Once
both microcatheters were placed, the coil was
partially inserted to aneurysm sac and stent was
deployed three quarters until cover all aneurysm
orifice. Unsheathing first centimeter of the stent by
withdraw the microcatheter. After that, deployment
of stent was by pushing on the pusher wire of the stent
and pulling the microcatheter. The stent deployed 1
mm at a time and continued until the stent pooch at
the neck of aneurysm and form a shape like shelf.
After the stent was considered shape satisfactory, the
rest of the stent was deployed three quarters using
standard technique. Then by using dyna-CT, the stent
was checked for the opening and absence of twisting.
Now, the microcatheter containing coil was
constrained between deployed stent and parent artery
wall. Coils continued to deploy until aneurysm sac
was completely packed, then stent can also be
deployed completely. After aneurysm sac was
completely occluded, microcatheter for coil was
pulled slowly with microguidewire. Packed coils
have been encaged between the aneurysm sac and
stent to prevent migration out of the sac.
2.3 Carotid Cavernous Aneurysm
Natural history of aneurysms from cavernous
segment was thought to be more benign and low
tendency to rupture than other vascular territories.
Due to dysplastic nature and anatomical morphology,
treatment options including surgical clipping, parent
artery occlusion with or without bypass, and
endovascular coiling was difficult to achieve
complete occlusion and have varying risk of
morbidity and mortality. Treatment was only
indicated for carotid cavernous aneurysm (CCA) that
symptomatic (opthalmoplegia or intractable retro-
orbital neuralgia), large size, and evidence of growth.
Because of endovascular technology advances, new
treatment option by using endoluminal device was
offered with a promising clinical outcome and also
low morbidity and mortality (Tanweer, 2014).
Endoluminal device or flow diversion is use to
exclude aneurysm segment of the parent artery by
implanting a metal scaffolding of low porosity (small
pore size) across the aneurysm neck. The idea of flow
diversion is to reduce intra-aneurysmal flow by
redirect blood flow along the parent artery. Reduction
of inflow jet velocity and level of shear stress on
aneurysm wall will initiate thrombosis in the
aneurysm sac. Ultimately, endothelization process
will begin with neointima and endothelium
Advances in Endovascular Neurosurgery Techniques: Toyama Hospital Experience
757
overgrowth of the stent that covered the aneurysm
neck. Adjacent branch vessel with uninterrupted
perfusion will not be affected. Thrombus in aneurysm
sac will be resorbed gradually via scavenger-cell-
mediated process and aneurysm mass will collapse.
This process begins immediate after stent deployment
and evolves over weeks to months. Currently, flow
diversion that approved by FDA is Pipeline
Embolization Device (PED; ev3-Covidien, Irvine,
CA) (Krishna, 2014).
PED is cylindrically shaped, self-expanding, and
made of 75% cobalt chromium alloy and 25%
platinum filament to impart greater radiopacity. PED
has low porosity (65-70%) and available in 10-35 mm
lengths and 2.5-5 mm diameters. Multiple PEDs can
be telescoped within each other to increase length or
to augment stent porosity over the aneurysm neck.
PEDs are supplied loaded within a removable sheath
an mounted on delivery microwire. The PED is
delivered through 0.027inch inner diameter
microcatheters so PED can be reconstructed to any
location that can be accessed with a 0.027inch inner
diameter microcatheter. Microcatheter can be
advanced to either capture delivery wire or relocated
distally for additional of PED deployment in a
telescoping fashion (Krishna, 2014).
Figure 4: A. Cavernous carotid aneurysm showed by 3D
angiography. B. Immediate angiography post flow diverter
placement showed stasis of contrast within aneurysm sac.
C. CT showed good position of device. D. Axial TOF MRI
after oneweek treatment showed trombosis in aneurysm
sac.
3 COMPARISON APPROACH
Endovascular therapy in 3 months at Toyama hospital
was 33 cases compare to vascular surgery only 12
cases. For vascular lesion, there are great swift from
vascular surgeries to endovascular therapies. So,
endovascular therapies 2.75 times more than vascular
surgeries. This is caused by improvement in
endovascular technology that made endovascular
therapies were effective and safe. Endovascular
therapies need a lot of cost depend on how
complicated the case and device that needed.
Sometimes endovascular therapies more expensive
than vascular surgeries.
Table 1: Approach list for vascular lesion.
Procedure Sum Type
Carotid angioplasty
Stentin
g
14 Endovascular
Coiling 12 Endovascula
r
Embolization 7 Endovascula
r
Clipping 8 Vascula
r
Vascular
Anstomosis
4 Vascular
4 CONCLUSION
Training with a different work culture at Toyama
University Hospital was an excellent experience. It
gave a broad perspective of different ways of to
approach similar conditions. This training also made
me more familiar with state-of-the-art neurosurgical
equipment and procedures in endovascular and
vascular neurosurgery.
ACKNOWLEDGEMENTS
I would like to acknowledge Prof Kuroda and Prof
Kuwayama for the opportunity to study endovascular
and vascular neurosurgery in Toyama University
Hospital and constant help during my training.
REFERENCES
Adla, T., Adlova, R., 2015. Multimodality imaging of
carotid stenosis. Int J angiol, 24, pp. 179-184.
Alghamdi, F., Mine, B., Morais, R., Scillia, P., Lubicz, B.,
2016. Stent-assisted coiling of intracranial aneurysms
located on small vessels: midterm results with the LVIS
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
758

junior stent in 40 patients with 43 aneurysms.
Neuroradiology, 58, pp. 665-671.
Crocker, M., Tolias, C., 2007. What future for vascular
neurosurgery? Vascular Health and Risk Management,
3(3), pp. 234-244.
Du, E. H. Y., Shankar, J. J. S., 2016. LVIS Jr ‘shelf’
technique: an alternative to Y stent assisted aneurysm
coiling. J NeuroInterv Surg,8(12), pp: 1256-1259.
Gahremanpour, A., Perin, E. C., Silva, G., 2012. Carotid
artery stenting versus endarterectomy.
Tex Heart Inst J, 39(4), pp: 474-487.
Krishna, C., Sonig, A., Natarajan, S. K., Siddiqui, A. H.,
2014. The expanding realm of endovascular
neurosurgery: Flow diversion for cerebral aneurysm
management. MDCVJ, X(4), pp: 214-219.
Sakamoto, S., Kiura, Y., Okazaki, T., Shinagawa, K.,
Ichinose, N., Shibukawa, M., et al, 2015. Usefulness of
dual protection combined with blood aspiration for
distal embolic protection during carotid artery stenting.
Acta Neurochir, 157, pp: 371-377.
Sanai, N., Tarapore, P., Lee, A. C., Lawton, M. T., 2008.
The current role of microsurgery for posterior
circulation aneurysms: A selective approach in
endovascular era. Neurosurgery, 62(6), pp: 1236-1253.
Tanweer, O., Raz, E., Brunswick, A., Zumofen, D.,
Shapiro, M., Riina, H. A., et al, 2014. Cavernous
carotid aneurysms in the era of low diversion: A need
to revisit treatment paradigms. AJNR Am J
Neuroradiol, 35, pp: 2334-2340.
Tjoumakaris, S. I., Jabbour, P. M., Gonzales, L. F.,
Dumont, A. S., Randazzo, C. G., Rosenwasser, R. H.,
2011. The evolution of future directions of
neuroendovascular therapy: From clips to coils to?
Clinical Neurosurgery, 58, pp: 42-50.
Advances in Endovascular Neurosurgery Techniques: Toyama Hospital Experience
759
