
Biomoleculer Screening on Women\Risked Servical Cancers in
Medan North Sumatera
Fatwa Imelda
1
, Nurbaiti
1
1
Faculty of Nursing, Universitas Sumatera Utara, Medan, Indonesia
Keywords : Servical cancers, Pap smears, Immunohistochemistry
Abstract: Cervical cancer is a women's health problem in Indonesia with the first order with high mortality. Effective
screening that can be used is Papanicolau Tests (Papsmears) to detect precancerous lesions and
immunohistochemistry techniques to identify the image of cervical cancer gene triggers in women at risk of
cervical cancer.This study aims to see biomolecular screening on women risked cervical cancers in Medan
North Sumatera.This study used cross sectional design. Samples were taken by consecutive sampling
technique. The number of samples taken as many as 80 samples, divided into 2 groups of 40 samples were
examined papsmears and 40 samples were examined immunohistochemistry technique.Pap smears from risk
factors such as 72.5% of respondents were age group more than 35 years and 37.5% the results of papsmears
not normal, 97.5%married respondents with abnormal 47.8% papsmears results, 67.5% were unemployed
with abnormal 35% pap smears results, 62.5% of respondents with regular women's menstrual cycles with an
abnormal 30% papsmears, 75% of respondents with a history of not using contraception with a majority of
abnormal papsmears of 37.5%. immunohistochemistry technique from risk factors such as age of over 35
years had IHC +1 (7.5%) and IHC +3 (2.5%), married status (87.5%) with HC +1 (7.5%) and IHC +1 (2.5%)
result IHC +1 have high school education (5%), Diploma (2.5%) and IHC +3 (2.5%), with status not working
with IHC +1 (5%), and IHC +3 (2.5%), history parity has the same distribution of ≤ 2 and 2 with 45% sample
with female parity status with IHC intensity 0 and parity ≤ 2 with IHC intensity +1 (2.5%) and IHC intensity
+3 (2.5%), with regular menstrual cycle with IHC +1 result (5%), and irregular menstrual cycle with IHC +3
(2.5%), non-FP (30%) result, with FP Mantap of IHC +1 (5%) and FP Hormonal with IHC +3 (2.5%).
1 INTRODUCTION
Cervical cancer in developed countries ranks fourth
after breast cancer, colorectal and endometrium,
while in developing countries ranks first (Kemenkes
RI, 2015). Various risk factors have been identified to
increase the risk of cervical cancer, namely; sexual
intercourse, patner characteristics, gynecological
history, diethylstilbesterol (DES), infectious agents,
Human Papilloma Virus (HPV), Herpes Simplex
Virus, smoking. Some other predicted risk factors
increase the risk of cervical cancer, namely: oral
contraceptives, diet, ethnic and social and
occupational factors (Imam, 2009). Human
Papilloma virus as the cause of cervical cancer is
found in 99.7% of cases of cervical cancer. It is the
WHO reason to set HPV 16 and 18 to be a carcinogen
agent in humans.
Cancer cells are the accumulation of a number
of genetic changes that contribute to the incidence of
tumorigenesis, tumor progression and resistance to
chemotherapy. Most of these genetic changes result
in cell cycle regulation. Loss of some molecular
checkpoints, found in the development of some
tumors, is because of cell cycle progression that
becomes dysregulated. The accumulation of genetic
changes contributes to the onset of chemoresistance
resulting in the ability of DNA to respond to damage.
Detectable DNA damage is regulated by a 53 p
Suppressor tumor, when the DNA damage is severe
enough p53 to initiate a cell death program
(apoptosis) (Calvagna, 2007).
534
Imelda, F. and Nurbaiti, .
Biomoleculer Screening on WomenServical Cancers in Medan North Sumatera.
DOI: 10.5220/0010077405340541
In Proceedings of the International Conference of Science, Technology, Engineering, Environmental and Ramification Researches (ICOSTEERR 2018) - Research in Industry 4.0, pages
534-541
ISBN: 978-989-758-449-7
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
2 METHOD
This study used a cross sectional research design with
research design by measuring or observing research
subjects simultaneously or once. The population of
this study women at risk of cervical cancers. The
sample was taken by consecutive sampling technique
that is the sample selection by setting the subject
according to the inclusion criteria in the research until
the sample quantity is fulfilled. The research was
conducted at Bhayangkara Hospital Medan, the
location of this study was taken because the general
hospital in the city of Medan and have women at high
risk of cervical cancer both in terms of age, hormone
contraceptive use. The study duration is one year.The
number of samples taken as many as 80 samples,
divided into 2 groups of 40 samples were examined
papsmear and 40 samples were examined
Immunohistochemical technique.
After getting permission from the hospital, the
researcher collected the data. The first stage of data
collection of prospective respondents are classified
as: married and sexually active women,
gynecological history of more than two children, use
of diethylstilbesterol (DES), smokers or passive
smokers, body weight, use of oral
contraceptives.Then the cotton biopsy sample was
taken for pap smear and IHC examination. After the
data of all actions done finished then continued by
comparing the data of pap smear and IHC
examination results.
The Research Ethics Committee from the
Commission of Health Research Ethics Faculty of
Nursing University of Sumatera Utara No.
1154/IV/SP/2017. The data was analyzed using
univariat so that just gotten the frequency
distributions.
3 RESULT
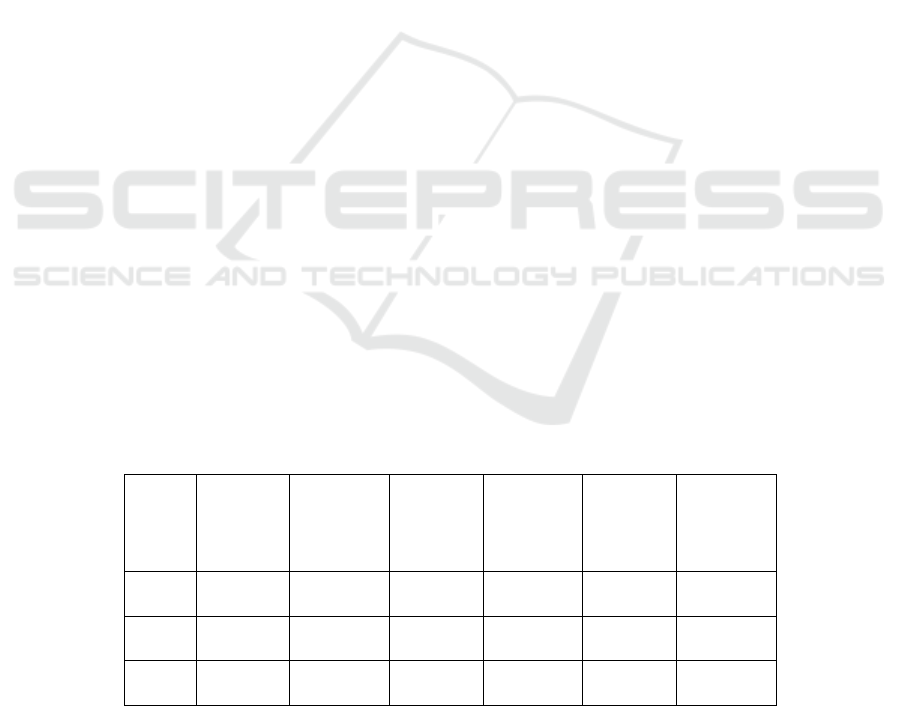
Table 1 shows that most (72.5%) of the samples are
age group over 35 year old and the majority of normal
and abnormal papsmears at age >35 year old is
37.5%. Table 2 shows that most (70%) of the samples
are age group over 35 year old having negative
intensity 0 (negative p53) and 7.5% intensity +1 (p53
negative) and 2.5% intensity +3 (P53 positive or
protein expression p 53 over expression). Table 3
shows that most (97.5%) of samples with marital
status married with a majority result of abnormal pap
smear 47.5%. Table 4 shows that most of the samples
with married marriage status (87.5%) with the
majority of IHC results with intenistas 0 (negative
P53) and 7.5% IHC +1 results (negative p53) and
2.5% with IHC +3 results (P53 positive or protein
expression p 53 over expression). Table 5 shows that
most (50%) women with senior high school education
degree with a majority of pap smear are abnormal at
25%. Table 6 shows that most of the samples (90%)
with IHC results of intensity 0 (negative P53) have
senior high school (42.5%), Diploma (15%),
Bachelor (32.5%) and IHC results of intensity +1
(negative p53) (5%), Diploma (2.5%) and IHC +3
results (positive p53 / over p53 expression) of (2.5%).
Table 7 shows that most (67.5%) with status not
working with abnormal Paps Smear results of 35%.
Table 1. Frequency distribution by age of women with Pap Smear
age
(years)
frequency
sample
percentage
sample
frequency
abnormal
pap
smear
percentage
normal
pap smear
frequency
abnormal
pap
smear
percentage
abnormal
pap smear
<20
0
0
0
0
0
0
20-35
8
20
5
12.5
5
12.5
>35
32
80
15
37.5
15
37.5
Biomoleculer Screening on WomenServical Cancers in Medan North Sumatera
535
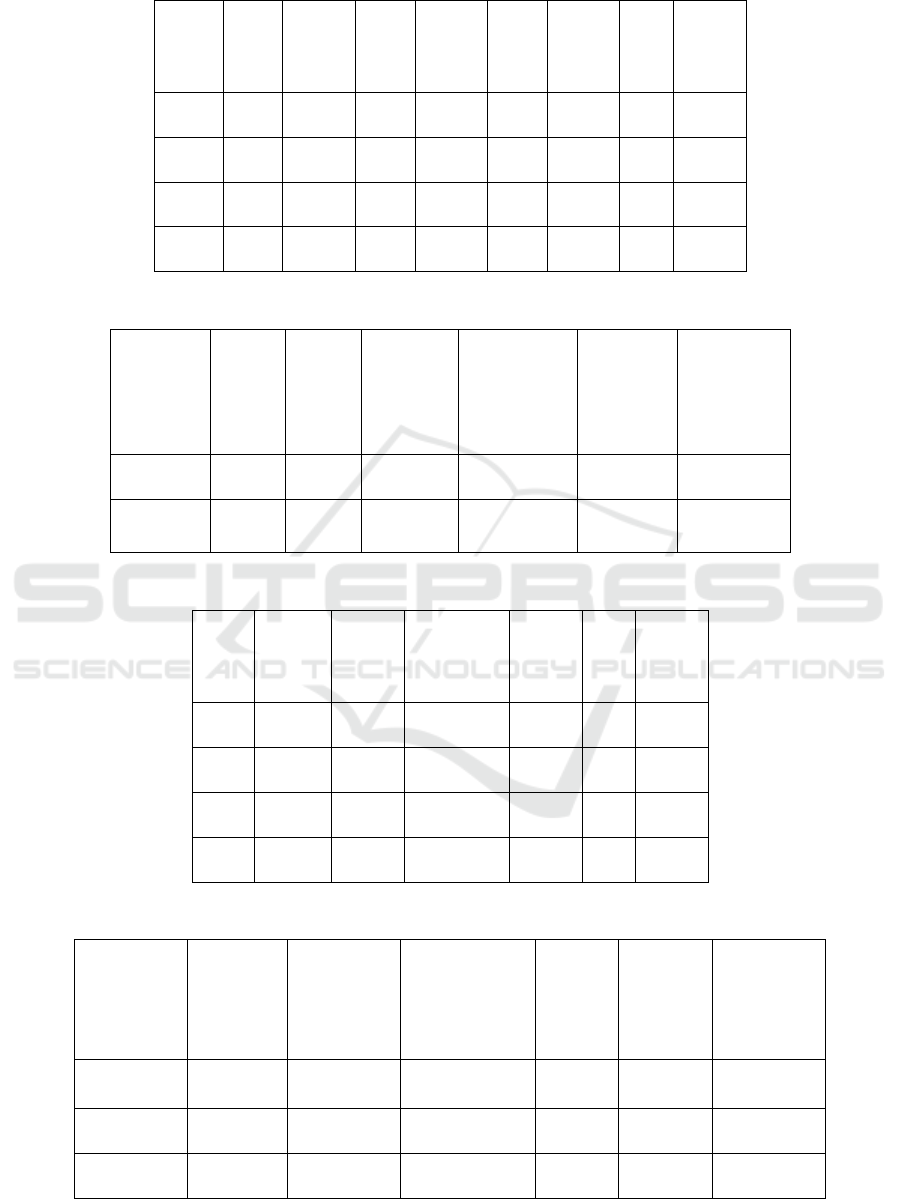
Table 2. Frequency distribution by age of woman with IHC
IHC
results
<20
years
%
sample
20-
35
years
%
sample
>35
years
%
sample
total
total
%
sample
0
0
0%
8
20 %
28
70%
36
90%
+1
0
0%
0
0%
3
7.5%
3
7.5%
+2
0
0%
0
0%
0
0%
0
0
+3
0
0%
0
0%
1
2.5%
1
2.5%
Table 3. Frequency distribution by marriage status of women with PapSmear results
marital
status
freque
ncy
sample
percent
age
sample
frequency
abnormal
pap smear
percentage
normal pap
smear
frequency
abnormal
pap smear
percentage
abnormal
pap smear
Married
39
97.5
20
50
19
47.5
divorced/
widowed
1
2.5
0
0
1
2.5
Table 4. Frequency distribution by marriage status of women with IHC results
IHC
result
merried
%
sample
Divorced/
widow
%
sample
total
total
%
sample
0
35
87.5%
1
2.5 %
36
90%
+1
3
7.5%
0
0%
3
7.5%
+2
0
0%
0
0%
0
0%
+3
1
2.5%
0
0%
1
2.5%
Table 5. Frequency distribution by marriage status of women with IHC results
educational
degree
frequency
sample
percentage
sample
frequency
abnormal pap
smear
percent
age
normal
pap
smear
frequency
abnormal
pap
smear
percentage
abnormal
pap smear
senior high
school
20
50
10
25
10
25
diploma
7
17.5
2
5
5
12.5
bachelor
13
32.5
8
20
5
12.5
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
536
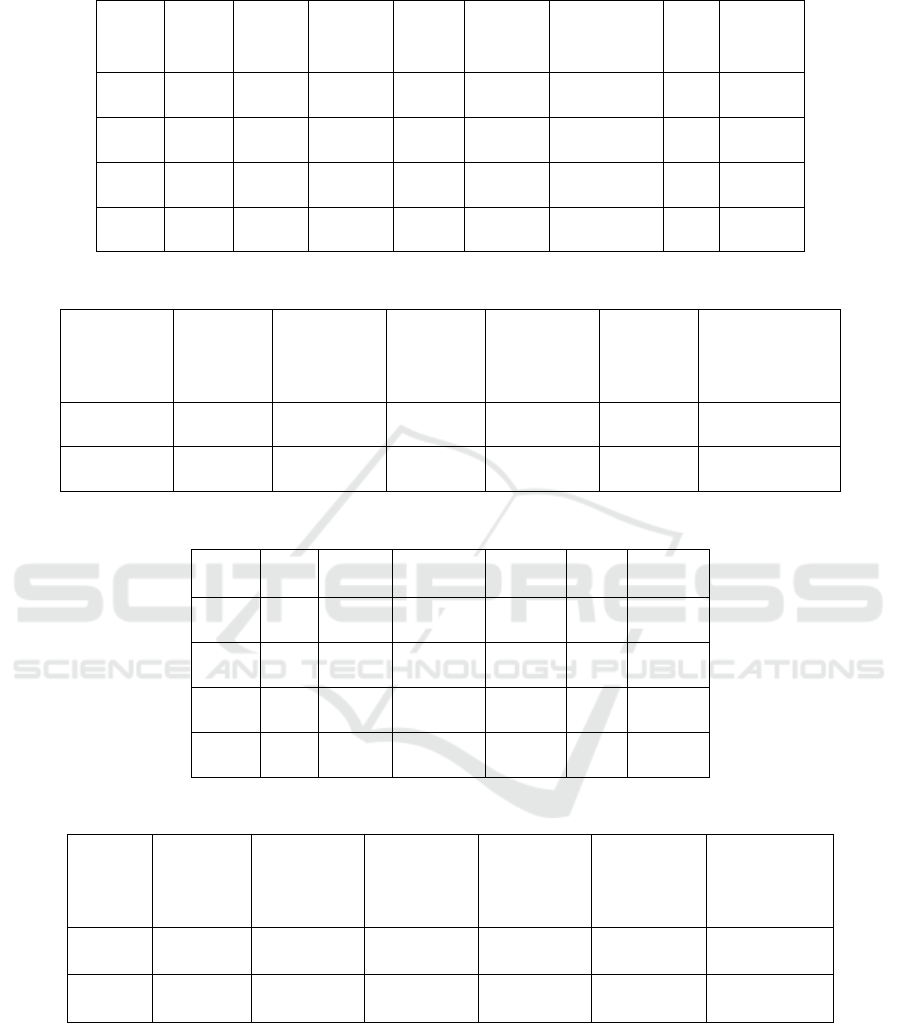
Table 6. Frequency distribution by status of education of women of reproductive age with IHC results
IHC
results
senior
high
school
%
sample
diploma
%
sampl
e
bachelor
percentage
sample
total
total %
sample
0
17
42.5 %
6
15%
13
32.5%
36
90%
+1
2
5%
1
2.5%
0
0%
3
7.5%
+2
0
0
0
0%
0
0%
0
0%
+3
1
2.5%
0
0%
0
0%
1
2.5%
Table 7. Frequency distribution based on women employment status with Pap Smear results
employment
status
frequency
sample
percentage
sample
frequency
abnormal
pap smear
percentage
normal pap
smear
frequency
abnormal
pap smear
percentage
abnormal pap
smear
working
13
22.5
7
17.5
6
15
not working
27
67.5
13
32.5
14
35
Table 8. Frequency distribution based on women employment status with IHC results
IHC
results
labor
%
sample
not
working
%
sample
total
total %
sample
0
12
30%
24
60%
36
90 %
+1
1
2.5 %
2
5 %
3
7.5 %
+2
0
0 %
0
0 %
0
0 %
+3
0
0 %
1
2.5 %
1
2.5 %
Table 9. Frequency distribution by women Parity with Papsmear results
Parities
history
frequency
sample
percentage
sample
frequency
abnormal
pap smear
percentage
normal pap
smear
frequency
abnormal
pap smear
percentage
abnormal pap
smear
≤ 2
20
50
7
17.5
13
32.5
>2
20
50
13
32.5
7
17.5
Biomoleculer Screening on WomenServical Cancers in Medan North Sumatera
537
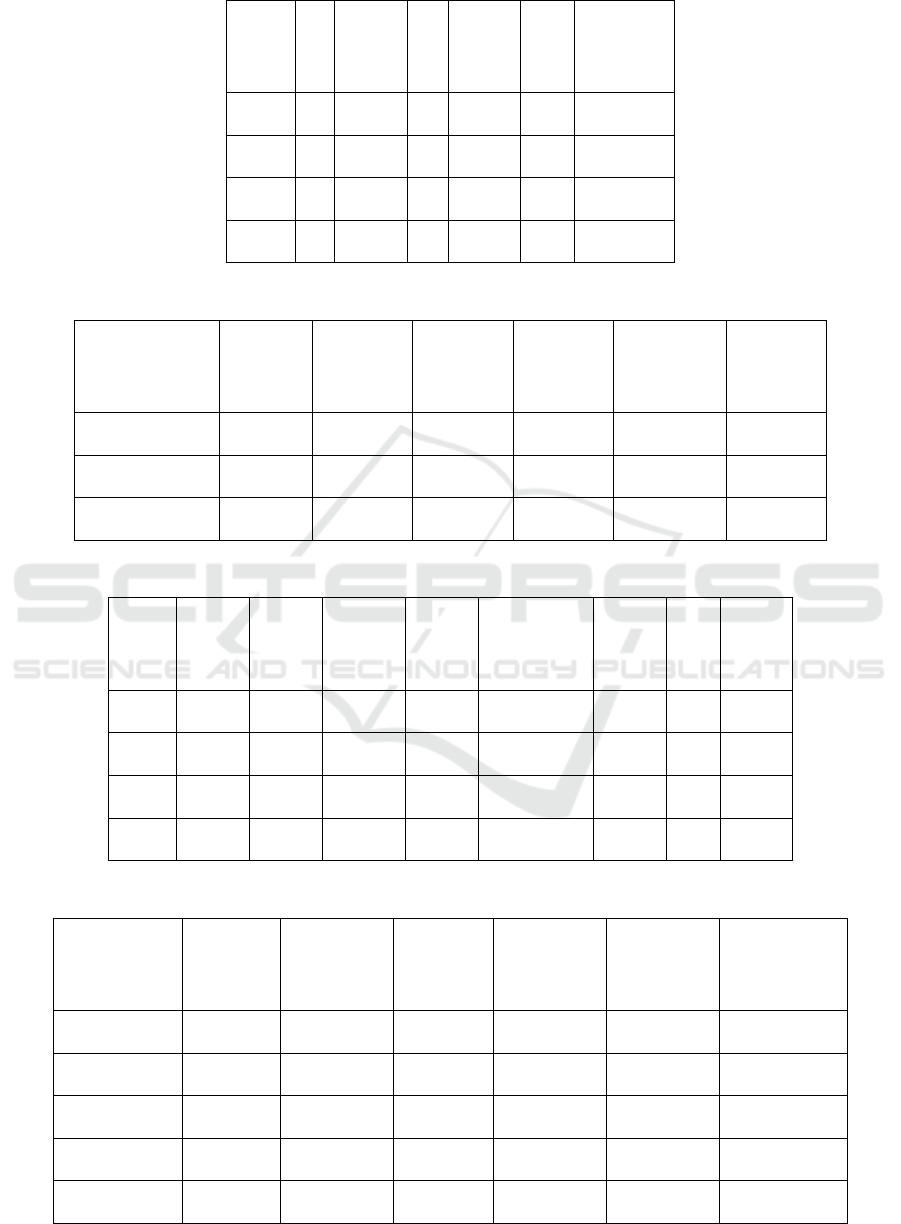
Table 10. Frequency distribution by women parity with IHC results
IHC
results
≤
2
%
sample
>2
%
sample
total
total
precentage
sample
0
18
45 %
18
45 %
36
90%
+1
2
5%
1
2.5%
3
7.5%
+2
0
0%
0
0%
0
0%
+3
0
0%
1
2.5%
1
2.5%
Table 11. Frequency distribution based on women menstrual cycle with Papsmear result
menstrual cycle
frequency
sample
percentage
sample
frequency
abnormal
pap smear
percentage
normal
pap smear
frequency
abnormal
pap smear
percentage
abnormal
pap smear
regularr
25
62.5
13
32.5
12
30
irregular
12
30
5
12.5
7
17.5
not menstruation
3
7.5
2
5
1
2.5
Table 12. Frequency distribution based on women menstrual cycle with IHC results
IHC
results
regular
%
sample
irregular
%
sample
not
menstruation
%
sample
total
total
%
sample
0
24
60 %
9
22.5 %
3
7.5%
36
90%
+1
1
2.5 %
2
5 %
0
0%
3
7.5%
+2
0
0 %
0
0
0
0%
0
0%
+3
0
0 %
1
2.5 %
0
0%
3
7.5%
Table 13. Frequency distribution based on women menstrual cycle with IHC results
FP history
frequency
sample
percentage
sample
frequency
abnormal
pap smear
percentage
normal pap
smear
frequency
abnormal
pap smear
percentage
abnormal pap
smear
hormonal FP
5
12.5
2
5
3
7.5
Simple FP
0
0
0
0
0
0
IUD
3
7.5
2
5
1
2.5
mantap FP
2
5
1
2.5
1
2.5
not using FP
30
75
15
37.5
15
37.5
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
538

Table 14. Frequency distribution based on FP history with IHC results
IHC
results
Hormo
nal FP
%
sample
IUD
%
sample
mantap
FP
%
sample
not using
FP
%
sample
total
% total
sampel
0
4
2
0
30
36
+1
0
0 %
1
2.5%
2
5%
0
3
+2
0
0 %
0
0
0
0
+3
1
2.5%
0
0
0
1
Table 8 shows that most samples (60%) with
status not working with IHC intensity 0 (negative
p53) and 5% with IHC intensity +1 (negative p53) of
5%, and IHC +3 results (positive P53) of 2.5%. Table
9 shows that the history of parity has the same
distribution of ≤ 2 and> 2 with 50% of the sample
with the parity status of women with an abnormal
number of papsmear of 32.5 in the history of parity ≤
2. Table 10 shows that the parity history has the same
distribution of ≤ 2 and >2 with 45% of the sample
with female parity status with IHC intensity 0
(negative p53) and parity ≤ 2 with IHC intensity +1
(negative p53) of 2.5% and IHC result +3 intensity of
2.5%. Table 11 shows that most (62.5%) of samples
with regular women's menstrual cycles with an
abnormal number of pap smear are 30%. Table 12.
demonstrated that most (60%) samples with regular
menstrual cycles with IHC intensity 0 (negative
protein p53), and 2.5% samples with regular
menstrual cycles with IHC +1 (negative p53), and 5%
samples with irregular menstrual cycles with IHC +1
results (negative p53), and 2.5% of samples with
irregular menstrual cycles with IHC +2 results
(negative p53). Table 13 shows that most (75%)
respondents with not FP history with a majority of
paps mear are abnormal on 37.5%. Table 14 shows
that most of the samples are not using FP (30%) with
a result of IHC intensity of 0 (negative p53) and a
sample with the mantap FP of 5% with IHC +1
(negative p53), and a Hormonal FP sample with IHC
+3 result of (2.5%).
4 DISCUSSION
In the results of this study found that the majority of
samples> 35 years. In adult women over 35 years old,
the condition of the reproductive organs begins to
aging, and in theory it is explained that the risk factors
that can increase the incidence of women with
cervical cancer are premenarche and post menopause
(Baradero & Dayrit, 1998). Generally new mucosal cells
mature after women aged 20 years and over. When a
woman has sex at adolescence, It is the most
vulnerable done under the age of 16 years.
This is related to maturation of mucosal cells in
the cervix. At a young age mucosal cells in the cervix
are not yet mature and that means are still susceptible
to stimulation, so they are not ready to receive
stimulation from the outside, including chemical
substances that brought sperm. Because it is still
susceptible, mucosal cells can change the nature of
cancer. But when sex is done after the age of 20 years
in which mucosal cells are no longer too susceptible
to changes. HPV infection is influenced by age factor
and immune condition, both of these factors affect
false positive values. False positive values are
positive HPV DNA testing but after other tests such
as colposcopy, IVA and papsmear, no cervical cancer
is found. women over 30 years of age are more likely
to have an exact or persistent HPV infection (Novel,
Safitri, & Nuswantara, 2009).
The results of this study was the majority of
samples married status. This is in accordance with the
theory that married women increase the risk of
cervical cancer due to sexual behavior. Cervical
cancer can occur because of sexual activity, because
at the time of sexual intercourse the woman can enter
the female reproductive organs that can cause
infections that if not treated immediately can become
cervical cancer after several years later (Lisnawati,
2013).
Women who are sexually active at the age of 20-
35 years and infected by HPV will suffer from
cervical cancer in the 10-20 year period and married
women before the age of 20 years will be at risk of
cervical cancer because at that age the reproductive
organs are not ready to have sexual intercourse at
early age (Smeltzer & Bare 2002), but women who
Biomoleculer Screening on WomenServical Cancers in Medan North Sumatera
539

are slow to marry are also risk factors for cervical
cancer because these women will continue to ovulate
without interruption so that stimulation of the
endometrium occurs continuously so that it can make
endometrial cells change the nature into cancer cells.
The results of this study obtained the majority
with the results of papsmear and abnormal IHC at
most with the level of senior secondary education.
Acceptance of new behavior will be easier if based on
the correct knowledge, awareness and positive
attitude (Notoatmodjo & Soekidjo, 2012). Increased
knowledge will not always cause behavioral changes,
Lack of knowledge that causes poor perineal behavior
of hygiene can have an impact on the increasing
incidence of cervical cancer. Lack of knowledge in
maintaining vaginal hygiene and correct attitude
about maintaining cleanliness and lack of information
leads to a lack of new knowledge gained so that the
behavior of vaginal hygiene becomes dependent on
the environment (Nurhayati & Annisa, 2013).
The results of this study were obtained mostly
with the status of not working.Factory income related
to nutrition and immunity. Low income groups
generally have less quantity and quality of food and
this affects the body immunity. The strong
relationship between the incidence of cervical cancer
with low socioeconomic level. Low-income groups
are usually less accessible with quality health services
including pap smear examination should be done
women aged 35 years and over. Low-income women
usually do not pay attention to nutritional status and
immunity. Income is very influential on the incidence
of cervical cancer. Low income is difficult to
implement individual hygiene, sanitation and
maintenance of health is lacking. According to
Styarini (Setyarini & Tjakraatmadja, 2009), there is a
relationship between cervical cancer with income,
where women with low incomes are 4 times more at
risk than high-income women.
The results of this study found that the history of
parity has the same distribution that is ≤ 2 and> 2.
Based on research results Hidayat, Hasibuan, and
Fitriyati, (2014). that the parity of more than>3 16.03
times the risk of cervical cancer than people who have
the number of parity <3. Women with high parity are
associated with the evolution of cervical columnar
epithelium during pregnancy which causes a new
dynamic of immature metaplastic epithelium that can
increase the risk of cell transformation and trauma to
the cervix, making it easier for HPV infection (Center
for Disease Control and Prevention Human
Papillomavirus-Associated Cancer United State,
2008).
Hormone changes during pregnancy are likely to
make women are more susceptible to HPV infection
or cancerous growth. In this study most experienced
regular menstruation and the majority of abnormal
papsmear as much as 30%. Irregular menstruation can
be caused by hormonal balance disorders.
The results of this study with non-family history
with papsmear and abnormal IHC. Taking more than
5 years of birth control pills containing progesterone
and estrogen has a bad effect on the uterus, which is
an infection of the uterus and allows a woman to have
uterine cancer (Wahyuningsih & Mulyani, 2014).
It can be concluded that the use of contraception
has an effect on cervical cancer. Oral contraceptives
with high estrogen levels cause adhesions of Candida
albicans which are the bacteria that cause flour
albous. Candida albicans can cause adhesions to the
vaginal epithelium and is a medium for fungal
growth. Candida albicans develops well in pH 5-6.5
environments, these changes can be asymptomatic or
cause infection.
Some journals also mentioned that the use of
mouthwashes such as chlorhexidine, benzydamine,
sodium bicarbonate, granulocyte macrophage
colony-stumulating factor (GM-CSF) showed
ineffectiveness in reducing the degree of mucositis.
The use of chlorhexidine for a long time can cause
tooth discoloration and damage to mucous
membranes.
5 CONCLUSION
1) Most percentage (72.5%) of samples were age
group over 35 years and the majority of normal
and abnormal pap smear at age> 35 years was
37.5%.
2) Most percentage (97.5%) of samples with
married status married with majority result of
abnormal pap smear 47.5%.
3) Percentage of the majority (50%) of women with
high school education with the majority of
abnormal papsmear by 25%
4) Most percentage (67.5%) with status not working
with abnormal pap smear results of 35%.
5) The percentage of parity history has the same
distribution that is ≤2 and> 2 with 50% sample
with parity status of women with the majority of
abnormal pap smear of 32.5 in the history of
parity ≤2.
6) Most percentage (62.5%) of samples with regular
women's menstrual cycles with an abnormal pap
smear majority of 30%.
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
540

7) The percentage of most (75%) respondents with
a history of non-FP with a majority of abnormal
pap smear of 37.5%.
8) The percentage of most (70%) samples were age
group over 35 years had IHC intensity 0
(negative p53) and 7.5% intensity +1 (p53
negative) and 2.5% intensity +3 (P53 positive or
protein expression p 53 over expression).
9) The percentage of married marriage status
(87.5%) with majority result of IHC with
intenistas 0 (negative P53) and 7.5% result of
iHC +1 (negative p53) and 2.5% with result of
IHC +3 (P53 positive or protein expression p 53
over expression).
10) The percentage of sample (90%) with IHC
intensity 0 (negative P53) high school (42.5%),
Diploma (15%), Bachelor (32.5%) and IHC
intensity +1 (negative p53) high school (5%),
Diploma (2.5%) and IHC +3 Result (positive p53
/ over p53 expression) of (2.5%).
11) The percentage of sample (60%) with status not
working with resultIHC intenistas 0 (negative
p53), and 5% with result of IHC intensity +1
(negative p53) 5%, and result of IHC +3 (positive
P53) equal to 2.5%.
12) The percentage of samples with parity history
had the same distribution of ≤2 and 22 with 45%
sample with female parity status with IHC
intensity 0 (negative p53) and parity ≤ 2 with
IHC intensity +1 (negative p53) of 2.5% and IHC
intensity +3 result of 2.5%.
13) The percentage of sample (60%) with regular
menstrual cycle with IHC intensity 0 (negative
protein p53), and 2.5% samples with regular
menstrual cycles with IHC +1 (negative p53),
and 5% samples with irregular menstrual cycles
with results IHC +1 (negative p53), and 2.5%
sample with irregular menstrual cycle with IHC
+2 result (negative p53).
14) The percentage of sampel was immune (30%)
with result of IHC intensity 0 (negative p53) and
sample with FP steady at 5% with result of IHC
+1 (negative p53), and Hormonal family
planning sample with IHC +3 result (2.5%).
6 SUGGESTIONS
1) Increasing education activities and health
promotion about cervical cancer prevention by
holding seminar or examination of cervical
cancer detection either Pap smear, IV
examination or IHC examination.
2) For the community to all women play an active
role in the prevention of cervical cancer is to
follow the cervical cancer seminar and early
detection of cervical cancesr examination.
3) For women who have ever done cervical cancer
should re-do periodically at least once a year if
obtained the results are normal and check the
repeat is to do a six-monthly examination.
REFERENCES
Baradero, M., & Dayrit, M. (1998). Seri Asuhan
Keperawatan Pasien Gangguan Sistem Reproduksi &
Seksualitas. Jakarta: EGC, 1998.
Calvagna, M. (2007).Diagnosis of Cervical
Cancer.American Cancer Society. [online]. Available:
http://www.cancer.
Center for Disease Control and Prevention Human
Papillomavirus-Associated Cancer United State.
(2008). MMWR Morb Mortal Wkly Rep 2012 61 (15);
258-261
Hidayat, E., Hasibuan, D., H., S., & Fitriyati, Y. (2014).
Hubungan kejadian kanker serviks dengan jumlah
paritas di RSUD DR. Moewardi, JKKI, Vol. 6, No.3.
Imam, R. (2009). Epidemiologi Kanker Serviks. Indonesian
Journal of Cancer,3.
Kemenkes RI. (2015). Buku Panduan Pelaksanaan IVA-
Sadari. Jakarta: Bakti Husada, 2015.
Lisnawati. (2013). Asuhan Kebidanan terkini Kegawatan
Maternal dan Neonatal. Jakarta: Tran Info Media.
Notoatmodjo and Soekidjo (2012). Ilmu Perilaku
Kesehatan. Jakarta: Rineka Cipta.
Novel, S., S., Safitri, R., & Nuswantara, S. (2009). Aplikasi
Hybride Capture II Sistem dalam Deteksi Dini Kanker
Seerviks. Cermin Dunia Kedokteran, 36, 24-26.
Nurhayati & Annisa (2013). Hubungan Pengetahuan Sikap
dan Perilaku Vaginal Hiegine terhadap Kejadian
Keputihan Patologis pada Remaja Putri Usia 13-17
Tahun di daerah Pondok Cabe Ilir. Karya Tulis Ilmiah
Stata Satu, Universitas Islam Negeri Syarif
Hidayatullah, Jakarta, 2013.
Setyarini, E. & Tjakraatmadja, J. (2009). Factor-faktor yang
berhubungan dengan kejadian kanker leher rahim di
RSUP Dr. Moewali Surakarta, Surakarta, Fakultas Ilmu
Kesehatan Universitas Muhammadiyah Surakarta.
Smeltzer, S. & Bare, B. (2002). Buku Ajar Keperawatan
Medikal Bedah Brunner dan Suddarth, Edisi 8, Vol. 2,
Jakarta : EGC.
Wahyuningsih, T. & Mulyani, E., Y. (2014). Factor Resiko
Terjadinya Lesi Prakanker Serviks Melalui Deteksi
Dini dengan Metode IVA (inspeksi Visual Asam
Asetat). Forum Ilmiah, 11(2), 192-209.
Biomoleculer Screening on WomenServical Cancers in Medan North Sumatera
541
