
Constrictive Pericarditis Due to Pulmonary Tuberculosis
Herwindo Ahmad
1
, Zainal Safri
1
, Refli Hasan
1
, Rahmad Isnanta
1
1
Division of Cardiology, Department of Internal Medicine, Faculty of Medicine,
Universitas Sumatera Utara, Jalan Doktor Mansyur No. 5, Medan, Indonesia
Keywords: Pulmonary Tuberculosis, Constrictive Pericarditis.
Abstract. Background. Pericardium disease can occur due to abnormalities of the pericardium itself or as a result of
systemic disease. One of the diseases that can occur in the pericardium is the constrictive pericarditis
characterized by visceral and parietal pericardium layer attachment. Tuberculosis (TB) is a major cause of
constrictive pericarditis in developing countries. Case report. A 21-year-old complaints were pain like
being stabbed on the left chest, easily tired, swollen legs, cough and weight loss. Chest X-ray examination
were cardiomegaly and infiltrates. Echocardiography examination found pericardium effusion, constrictive
pericarditis with decreased function of cytolic and diastolic left ventricle. Mantoux Text showed positive
results. The treatments were antibiotics, diuretics, antituberculous drugs and steroids. Discussion.
Constrictive pericarditis is a chronic process of pericardium fibrous thickening that inhibits diastolic filling
of the heart, decreases venous return and decreases cardiac output. The diagnosis of constrictive pericarditis
is based on the association between clinical manifestation and from the results of one or more imaging
studies. Medical therapy has a role in the treatment of specific causes, anti-inflammatory, and supportive
effects. Conclusion. We reported a case of constrictive pericarditis due to pulmonary TB.
1 INTRODUCTION
The pericardium has several important functions
such as restricting the stretch or distention of the
cardiac cavity and facilitating the interaction of the
ventricles and the atrium so that changes in pressure
and volume in one part of the heart can affect
pressure and volume in other parts of the heart.
Pericardium also serves as a barrier to the spread of
infection and friction from the tissues surrounding
the heart. Although the pericardium has many
important functions but on the condition that the
pericardium is not found it is reported to have no
significant adverse effects (Francis, 2011).
Pericardium disease can occur due to abnormali-
ties of the pericardium itself or as a result of systemic
disease. Some diseases that can occur in the
pericardium such as pericarditis (acute, subacute,
chronic and recurrent), pericardium effusion, cardiac
tamponade and constrictive pericarditis (Adler, 2015).
Constrictive pericarditis is characterized by
diastolic cardiac filling disorder and increased
ventricular filling pressure due to rigid pericardium
with visceral and parietal pericardial layer
attachment. The symptoms of constrictive
pericarditis are the symptoms of heart failure with
increased jugular venous pressure, shortness of
breath, peripheral oedem, hepatomegaly, and ascites.
Tuberculosis is a major cause of constrictive
pericarditis in developing countries where the
incidence of tuberculosis is still high, but the
incidence in the developed countries is still rare
(Adler, 2015), (Dal-Bianco, 2009), (Lewinter, 2012).
2 CASE REPORT
A 21-year-old man went to the heart center
emergency department on August 2016 with a main
complaint of chest pain. Chest pain was felt by the
patient since 5 days, felt like being stabbed on the
left chest without spreading, nausea, vomiting or
cold sweat. Pain was felt to be more severe if the
patient inhales. Patients also complain of fatigue
easily during the activity within 2 weeks. Swollen
legs were found within 3 days. Cough has been
found since 6 months with white sputum without
blood. Patients admitted weight loss in the last 6
months as much as 10 kg with decreased appetite.
Fever, history of fever, history of shortness of
444
Ahmad, H., Safri, Z., Hasan, R. and Isnanta, R.
Constrictive Pericarditis Due to Pulmonary Tuberculosis.
DOI: 10.5220/0010072504440448
In Proceedings of the International Conference of Science, Technology, Engineering, Environmental and Ramification Researches (ICOSTEERR 2018) - Research in Industry 4.0, pages
444-448
ISBN: 978-989-758-449-7
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
breath, hypertension, diabetes mellitus, smoking,
and drinking alcohol were denied by the patient.
On physical examination, sensorium alert, blood
pressure 100/70 mmHg, pulse 144 times/minute,
regular, pressure and volume enough, respiratory
rate 28 times/minute, body temperature 36.7 ° C.
Pale conjunctiva and icteric sclera was not found.
Increase of jugular vein pressure was found,
kussmaul sign (+). Heart sound S1 and S2 was
normal, murmur (-), gallop sound (-). Lung:
vesicular respiratory sound, rales or wheezing was
not found. Abdomen: soepel. Liver, lien, renal were
not palpable, peristaltic (+) normal. Extrimities:
warm acral, oedem pretibial was found on both legs.
From laboratory test: Hb: 12,4 g%; Ht 39%;
Leucosytes 13.220/mm
3
; PLT 328.000/mm
3
; Ur: 17
mg/dL; Cr 0.59mg/dL; Na 138 mEq/L; K 3.5
mEq/L; Cl 107 mEq/dL; Albumin 2.7 g/dL; Blood
Glucose adr 161 mg/dL, ASTO <200; CRP 0.7
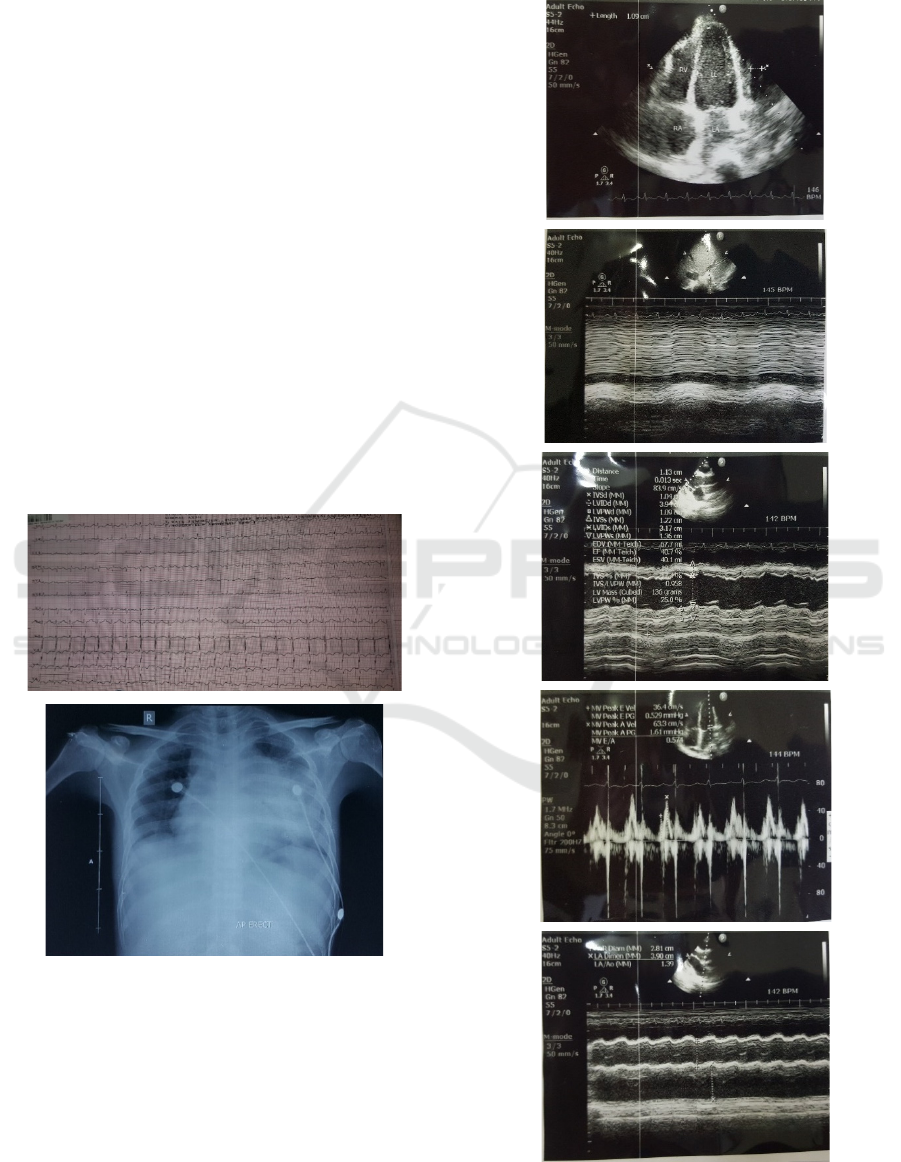
mg/dL. The patient had done electrocardiographic
(ECG) and Chest X-Ray examination (Figure 1), the
conclusions from echocardiography examination and
Doppler Tissue Imaging were pericardiac effusion
and constrictive pericarditis (Figure 2 and Figure 3).
Figure 1: The ECG and Chest X-Ray of the Patient. The
impressions of (ECG) examination were sinus tachycardia
and LVH. Cardiomegaly and infiltrates were found on
Chest X-Ray examination.
The patient was diagnosed with constrictive
pericarditis, mild pericardiac effusion due to suspect
pulmonary tuberculosis and was consulted to the
pulmonologist. Interpretation of mantoux test was
27mm induration, redness (+), itchy (+), conclusion:
a positive result. Sputum culture results: Direct
smear of tuberculosis I and II was negative.
Figure 2: The Echocardiography Results of the Patient.
Constrictive Pericarditis Due to Pulmonary Tuberculosis
445
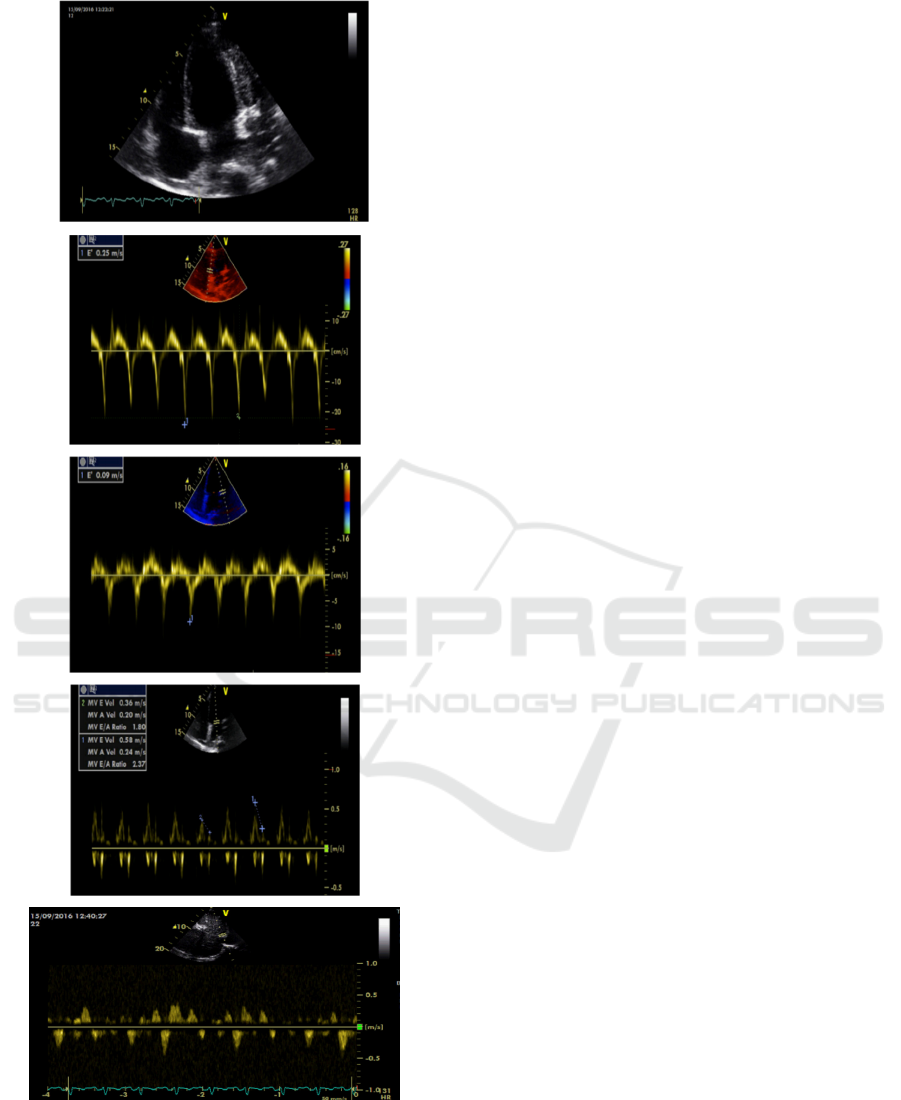
Figure 3: Doppler Tissue Imaging of the Patient. The e'
medial velocity was 25 cm/s and the e’ lateral velocity was
lower (9 cm/s). There was an increase in the difference of
mitral flow rate during inspiration and expiration > 25%.
There was also an increase in backflow of diastolic hapatic
veins at expiration.
Treatments of this patient were bed rest, O2 2-4
L/min with nasal canule, IVFD NaCl 0,9% 10
gtt/min, Cefotaxime 1 gr/8 hours/i.v, Gentamicin
120 mg/12 hours/i.v, anti-tuberculosis first category
drugs (Fixed Dose Combination) 1x3 tab,
prednisone 3x20 mg/oral, furosemide 1x40 mg/oral,
paracetamol 3x500 mg/oral, vitamine B6 1x2 tab.
There was clinical improvement after treatment for
14 days and the patient can get outpatient control.
Heart spaces
and
large blood vessels in the normal
position. Heart valves are good. There is no defect in the
heart chambers. There is a thickening of the pericardium
parietal and visceral with adhesion of the pericardium in
some places. There is a light pericardium effuse. The
systolic and diastolic function of LV decreases.
3 DISCUSSION
Constrictive pericarditis is a chronic process of
pericardium fibrous thickening which is often
followed by calcification and inhibition of diastolic
filling of the heart, decreasing venous return and
decreasing cardiac output. Constrictive pericarditis
is caused by a chronic inflammatory process of the
pericardium that triggers scar formation, fibrosis and
calcification in the pericardium. The incidence rate
of tuberculosis pericarditis is < 4% of pericardium
disease cases in developed countries but far different
when compared with developing countries that is 50-
70% of cases without HIV disease and > 90% in
cases accompanied by HIV disease, especially in
endemic areas for tuberculosis. In developed
countries the most frequent causes are idiopathic,
postoperative, radiation effects. In developing
countries, tuberculosis is the leading cause of
constrictive pericarditis (Adler, 2015; Lewinter,
2012; Little, 2006). In this case, the patient is
diagnosed with pulmonary tuberculosis where
tuberculosis is the most common cause of
constrictive pericarditis in developing countries
including Indonesia.
Constrictive pericarditis is characterized by
diastolic ventricular filling disorder resulting from
pericardium disease. Typical clinical features are
signs and symptoms of right heart failure with good
left and right ventricular function without any
myocardial or other ballast disease. Patients
complaint of fatigue, peripheral edema, shortness of
breath and ascites. Venous congestion, pleural
effusion, hepatomegaly may also occur (Adler,
2015; Mayosi, 2005).
On physical examination we can find an increase
in jugular venous pressure. Kusmmaul sign, ie
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
446

increased venous pressure during inspiration or no
decrease in venous pressure during inpiration, can
also be encountered. Pulsus paradoxus occurs in a
third of cases, especially in pericarditis patients
followed by pericardium effusions. Another typical
sign that can be encountered is the pericardial knock
that arises during the initial diastolic phase due to
the sudden cessation of ventricular filling. On
abdominal examination we can find hepatomegaly
and liver congestion symptoms such as ascites and
jaundice. Oedem in both lower extremities is the
most common in cases of constrictive pericarditis
(Lewinter, 2012), (Talreja, 2008).
In this patient, the main complaints were chest
pain, fatigue, cough, and weight loss weight loss.
The results of physical examination were
tachycardia, increase in jugular venous pressure,
kussmaul sign and pretibial oedem on both legs.
The diagnosis of constrictive pericarditis is based
on the association between signs and symptoms of
right heart failure with diastolic filling disturbance
resulting from constriction in the pericardium from
the results of one or more imaging studies, including
echocardiography, CT, CMR and cardiac
catheterization (Adler, 2015), (Liu, 2009).
Low QRS voltage, nonspecific T-wave changes
and P mitral are common but ECG results are not
specific for the diagnosis of constrictive pericarditis.
On examination of chest X-ray the size of the heart
can be normal or enlarged. Echocardiographic
examination is very important to establish the
diagnosis of constrictive pericarditis (Francis, 2011).
The diagnosis of echocardiography in
constrictive pericarditis is based on findings from
M-mode echocardiography followed by 2D
echocardiography and Doppler hemodynamics in the
respiratory cycle response. In constrictive
pericarditis, the initial mitral inflow diastolic
decreases as inspiration and the isovolumetric
relaxation period elongated. While at expiration, the
mitral inflow returns to normal and the
isovolumetric relaxation retracts. Typical findings of
constrictive pericarditis are an increase in the rate of
mitral inflow in the early diastolic phase by as much
as> 25% during expiration compare with inspiration.
The hepatic venous flow from Pulsed Doppler in
constrictive pericarditis indicates a significant
diastolic flow reversal, which increasing in
expiration over inspiration (Dal-Bianco, 2009)
Doppler Pulsed Tissue examination and color
Doppler Tissue Imaging (DTI) may help to diagnose
constrictive pericarditis. The lateral or septal mitral
anular velocity at baseline > 8 cm/s is said to be the
boundary value for differentiating patients with
constrictive parikarditis and restrictive
cardiomyopathy. This examination is useful when
the initial diastolic mitral flow rate change is not
(Dal-Bianco, 2009), (Vaitkus, 1996).
In this patients the diagnosis of constrictive
pericarditis in addition to anamnesis and physical
examination, also obtained from an ECG
examination that shows sinus tachycardia and LVH.
From the results of chest X-ray obtained
cardiomegaly and found the infiltrate in the left lung
field. On mantoux test examination was found
positive results so that patients are also diagnosed
with pulmonary TB. This patient's
echocardiographic examination was in accordance
with the features of constrictive pericarditis.
Although the main management of constrictive
pericarditis is surgery, medical therapy has a role in
management at least in three conditions. First,
medical therapy for specific causes eg pericarditis
due to tuberculosis. Secondly, medical therapy such
as anti-inflammatory can treat transient constrictive
that occurs in 10-20% of cases within a few months,
generally in temporary phenomenon at the time of
resolution of pericarditis. Third, medical therapy is a
supportive therapy and aims to control congestion
symptoms in which surgery is contraindicated or at
high risk. Anti-tuberculosis drugs can reduce the risk
of 10-80% of occurrence of constrictive pericarditis
due to tuberculosis infection (Adler, 2015; Liu,
2009).
In this patient, the therapy given were antibiotics
(cefotaxime and gentamicin) and steroids namely
prednisone and antituberculosis drug. Patients have
not planned for pericardiotomy surgery.
4 CONCLUSIONS
A 21-year-old male patient with a diagnosis of
constrictive pericarditis due to pulmonary TB has
been reported. The diagnoses were established on
the basis of history, physical examination and
support of ECG, thoracic X-ray, echocardiography
examination, and mantoux test.
Constrictive pericarditis is characterized by
diastolic heart filling disorder and an increase in
ventricular filling pressure due to rigid pericardium
by adhering to the visceral and parietal pericardium.
Tuberculosis is a major cause of constrictive
pericarditis in developing countries where the
incidence of tuberculosis is still high.
Constrictive Pericarditis Due to Pulmonary Tuberculosis
447

REFERENCES
Francis GS, Tang HW and Walsh RA 2011
Pathophysiology of heart failure Hurst’s the Heart vol
13, ed Fuster, Walsh, and Harrington (New York:
McGraw Hill) p 1930-34
Adler Y, Charron P, Imazio M, Badano L, Baron-
Esquivias G, Bogaet J, Brucato A, Gueret P, Klingel K,
Lionis C, Maisch B, Mayosi B, Pavie A, Ristic AD,
Tenas MS, Seferovic P, Swedberg K and Tomkowski
W 2015 Guidelines on the diagnosis and management
of pericardial diseases executive summary: the task
force on the diagnosis and management of pericardial
diseases of the European Society of Cardiology Eur
Heart J 36 p 2921-64
Dal-Bianco JP, Sengupta PP, Mookadam F,
Chandrasekaran K, Tajik J and Khanderia BK, 2009
Role of echocardiography in the diagnosis of
constrictive pericarditis. Journal of the American
Society of Echocardiography 22 25-33
Lewinter MM and Hopkins WE 2012 Pericardial disease
Braunwald’s Heart Disease: Textbook of
Cardiovascular Medicine vol 10, ed Mann DL, Zipes
DP, Libby P, Bonow RO, and Braunwald E
(Philadelphia: Elsevier Saunders) p 1646-52
Little WC and Freeman GL 2006 Pericardial disease
Circulation 113 1622-32
Mayosi BM, Burgess LJ and Doubell AF 2005
Tuberculous pericarditis Circulation 112 3608-16
Talreja DR, Nishimura RA, Oh JK and Holmes DR 2008
Constrictive pericarditis in the modern era: novel
criteria for diagnosis in the cardiac catheterization
laboratory J Am Coll Cardiol 51 315–19
Liu YW, Tsai HR, Li WH, Lin LJ, and Chen JH 2009
Tuberculosis constrictive pericarditis with concurrent
active pulmonary tuberculosis infection: a case report
Cases Journal 2 7010
Vaitkus PT, Cooper KA, Shuman WP and Hardin NJ 1996
Images in cardiovascular medicine: Constrictive
pericarditis. Circulation 93 834
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
448
