
E-Health Implementation in Support of Hospital Service at Indonesia
of Health National Insurance Era
Study on MHR at DMS Surabaya
Titin Wahyuni, Puteri Mahawati Ersalina
STIKes Yayasan RS. Dr. Soetomo
wtitin.2012@gmail.com
Keywords: E-Health, Hospital, Outpatient, Misfile Health Records.
Abstract: E-health is an Outpatient queuing management system at Dr. M. Soewandhie Hospital. This system
provided by Surabaya City Government for supporting the implementation of Health National
Insurance. On the other hand, its success requires support from Dr. M. Soewandhie Hospital in term of
health records availability when service is performed. Based on observations made on 23 to 27 January
2017 found 718 misfile health records with an average of 144 ones per day. This research focuses on
finding cause of misfile health records. We observed 257 ones during June to July, 2017 by purposive
sampling method. The result shows that the most significant cause of misfiling health records based on
observation is the doctors not complete yet health records from inpatient room. Based on the interview
outcome, all of respondents agree at the most significant cause led to misfiling is human error due to
wrong sub shelf and the best effective to avoid the problem by building up electronic health record and
fixing problem at shelving and space. We suggest to design and launch intervention program to
improve readiness providing health record and it suppose to be an effective long term follow up to
assess the sustainability of intervention.
1 INTRODUCTION
Universal health coverage is defined as ensuring
that all people have access to needed promotion,
preventive, curative and rehabilitative health
service, of sufficient quality to be effective, while
also ensuring that people do not suffer financial
hardship when paying to these service. Universal
health coverage has therefore become a major goal
for health reform in many countries, including
Indonesia (WHO, 2017). To Indonesia, it is not just
about to carry out a priority objective of WHO. It
is a part of the implementation of the 1945
constitution as well (Mboi, 2015).
Indonesia launched National Health Insurance
called Jaminan Kesehatan National (JKN) in
January 2014, a way to achieve universal coverage.
It is initially cover around 120M population who
are already engaged in various social health
insurance (SHI) schemes under a fund
management agency called BPJS. In the year 2019,
Indonesia targeted all population is around 250M
people to be coverage. Once when this goal is
achieved, JKN will be the largest program that
coverage the highest population in the world
(WHO Indonesia, 2017).
Thailand became exemplary leader for
achieving universal coverage among South East
Asian Nation. Moreover, Thailand could benefit all
citizens with comprehensive health service. While
Philippines also gave an excellence lesson with its
health service not only portable to utilized inside
the country but it could use outside one as well.
Although it is not a comprehensive one,
Philippines are able to eliminate the threat of
impoverishment due to illness for most of the
population (Thabrany, H., 2015).
Government of Surabaya city has concerned in
developing e-government which one of the
innovation is called as e-health. E-health is an
outpatient of queuing management system. It is an
integrated health system that had been
implementing to 62 Primary Health Services and 2
hospitals owned by government of Surabaya city.
One of them is dr. M. Soewandhie Hospital
(Regulation of Mayor of Surabaya Number 5 Year
2013).
On the other hand, this implementation required
well preparation from hospital particularly in
298
Wahyuni, T. and Ersalina, P.
E-Health Implementation in Support of Hospital Service at Indonesia of Health National Insurance Era - Study on MHR at DMS Surabaya.
In Proceedings of the 4th Annual Meeting of the Indonesian Health Economics Association (INAHEA 2017), pages 298-302
ISBN: 978-989-758-335-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

availability health record of future patient who
would be service at the certain date and time.
When patient who already queuing by e-health
system came at the hospital, filing staff of health
record division is supposed to be prepare patients’
health record at least a night before the actual
admission. In consequence, at the certain day when
they are attending to hospital and health records
are not ready yet due to misfiled, it would make
them cannot receive hospital service at certain time
that had promised as seen as screen on e-health.
Based on our observation on 23 to 27 January
2014 found that a total 718 misfile health records
and 144 ones on the average of ones. Therefore, in
this paper we focused to analyse the causes of
misfile health records of patients who already
registered to queuing system by e-health.
Once a health record is declare as misfiling one,
at the end step of procedure to find out one, if there
is a dead lock, filling staff must provide a new
health record as a solution of misfiling. Therefore,
it able to create duplication of existing health
record. Moreover, it make ones to make the data of
become hard to be synchronous (Karlina et al.,
2016).
2 METHODS
This research focuses on finding cause of misfile
health records. We observed 257 misfile health
records during June to July, 2017 by purposive
sampling method. List of patients who will visit in
the outpatient tomorrow, will be prepared his
medical record by filing officer on D-1. The health
record found will be marked and the undiscovered
will be crossed. We will track on the service day
where it was found and then addressed the cause
and the issues due to in misfiling.
3 RESULT
We conducted interview in order to determine the
cause in a great number misfiling events. Result of
the interview compiled in the Table 1.
Table 1: Interviewed outcome with respondents in term
significant cause of misfile health records events
Respondent
Interview outcome
Filling staff 1
(1
st
respondent)
Health records did not return yet
from inpatient rooms
Health records have moved from
the main of filling shelf
Health records have located at
wrong sub shelf
Health records have been at poly
specialist for surgery preparation
Those health records are owned
by new patients
Filling staff 2
(2
nd
respondent)
Those health records are owned
by new patients
Health records have been at poly
specialist for surgery preparation
Health records did not return yet
from inpatient rooms
Health records have located at
wrong sub shelf
Filling staff 3
(3
rd
respondent)
Health records have located at
wrong sub shelf
Table 1 describe how different considerations
in term significant cause of misfile health records
events among 3 filling staffs. Overall, 2
respondents gave several cause of factors while the
other gave only one cause. Both respondent 1 and
2 are agree to 3 of significant due to ones. They are
health records still at inpatient room, at poly
specialist for surgery preparation, and owned by
new patients. Based on table 1, they contributed at
36%, about 4%, and 5% respectively. Moreover, 3
respondents agree to significant causes of ones are
health records have located at wrong sub shelf.
While it seems only 2% of it significant due to
ones.
In conclude, the most problem based on their
point of view are the most highest significant and
the lowest significant as showed at table 1. In other
words, their answer only significant with
incompleteness health record at inpatient room by
doctors. Comparing their answer within data that
we observed afterward, we also then interviewed
toward the best solution to keep away misfile
health records events. The interview outcome are
presented by table 3. Based on observation in June
to July 2017, we analyse 257 misfile health
records.
E-Health Implementation in Support of Hospital Service at Indonesia of Health National Insurance Era - Study on MHR at DMS Surabaya
299
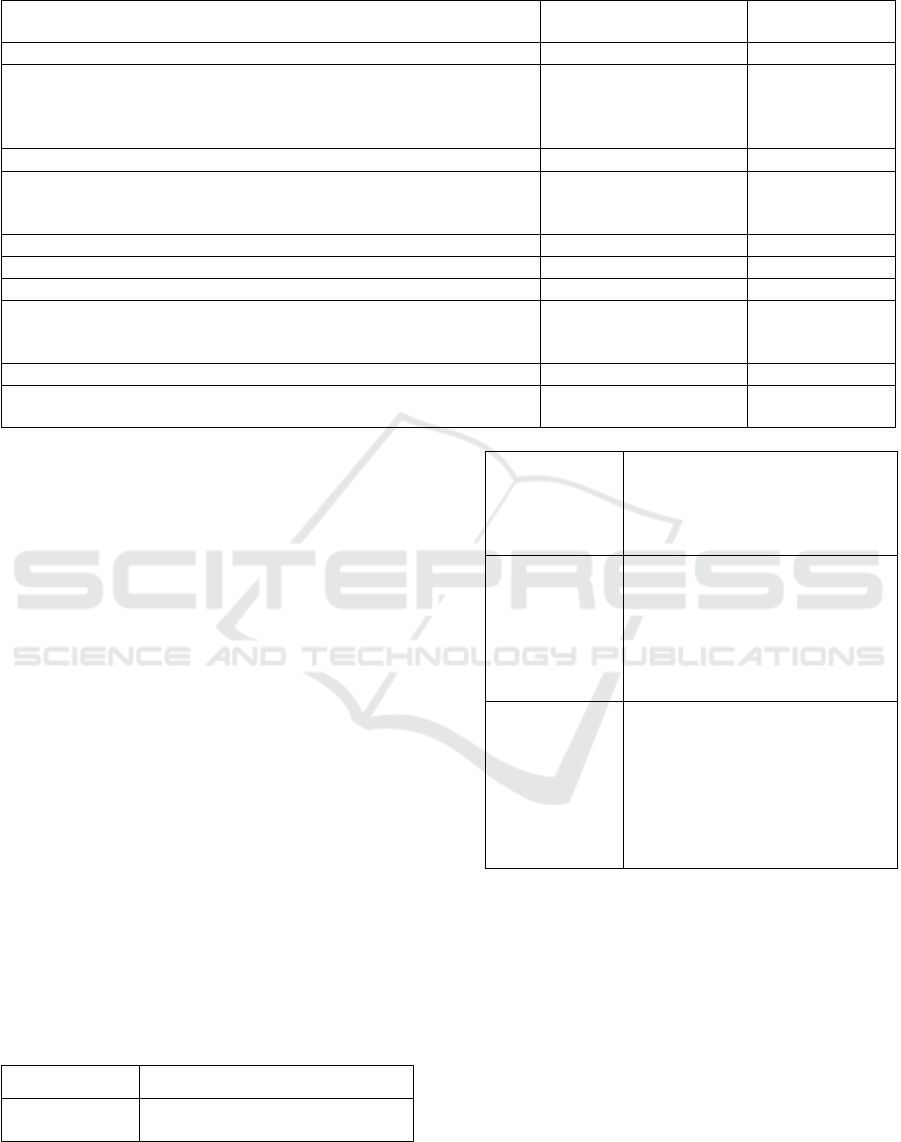
Table 2: Factors and issues contributing in misfiling at outpatient service of DMS Hospital
Factors and issues
Total misfile health
record per day
Percentage (%)
Doctors
a. They do not complete yet health records from inpatient room, so
they do not return yet to filling room. Consist of two issues:
1. Return to health record room by 2x24 hours
2. Return to health record room by more than 2x24 hours
21
71
8
28
b. They do not complete yet health records from emergency room
47
19
Shelving and space
Room is an adequate and resulting overloaded files. Therefore, they
moved from main filling shelve
57
22
Patients
Attending hospital without ID, resulting double numbers
32
12
Filling staffs
a. Wrong sub shelf
b. Declared health record as a misfile when in fact it is due to new
patients category
6
14
2
5
System
Health records at Poly specialist (pro surgery, incompleteness health
record post surgery)
9
4
Table 2 show factors and issues that
considering misfiling health records incidents in
the month June to July 2017 with its percentage.
Overall, doctors contributed to the most significant
factor in misfiling ones incidents while system is
the lowest contribution to them. The most
significant issue are health records not returning
yet from inpatient room to filling room, totally at
36% and most of them as big as 28% is due to
incompleteness of ones for more than 2x24 hours.
Incompleteness ones are also happening both at
emergency room and poly specialist, we can show
from table above it is represented by 19% and
about 4% respectively. Alongside with them, the
second highest frequency is being moved from
main filling self (22%) due to overload of ones. In
this research also found an issue that need to be
concern are double numbers of ones (12%). In
conclude, doctor has a factor and incompleteness
ones is the most significant effect in misfiling ones.
Moreover, We interview 3 respondents
regarding to find significant cause of misfile health
records events according to their opinion.
Table 3: The best effective way to avoid misfile health
records events according to respondents
Respondent
Interview outcome
Filling staff 1
(1
st
respondent)
make the filling room wider or
move into wider room
Filling staff 2
(2
nd
respondent)
Maintain and develop the system
that has been applied, both in the
work and electronic system.
Moreover, it also needs to increase
amount of the shelves
Filling staff 3
(3
rd
respondent)
The electronic health record
should be become hospital's
priority cause of every patients'
history will be recording in it.
Therefore if health records are
declared misfile it can be solve by
looking into it.
Head of health
records division
(4
th
respondent)
It needs to realisation electronic
health record urgently so that if
there are misfile health records
events, service still can be running
without complain due to respond
time of it from patients; doctor
and others persons in charge can
access every data on it
Table 3 describe how different consideration in
term the best effective way to avoid misfile health
records events among 4 respondents. 2 respondents
are agreeing at build up electronic health record
while 2 others have different idea toward the best
solution of it. Electronic health record must be
hospital’s priority regarding respondent 3 and 4
due to several benefit that can be provided by it.
For instance, misfile health record can be tracking
on it; pursuit the respond time of it if there are
misfile health records happening so service still
can be running without complaint from patients.
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
300

While others approve at increase amount of the
shelves (respondent 2) and make the filling room
become wider or move into wider room
(respondent 1). In conclude, we believe that the
best solution based on their idea is making a way
out on problem of the shelving and space by
building up electronic health record and
appropriate filling room.
4 DISCUSSION
Misfiling health records are responsibility filling
staff. Firstly; the result shown that the most
significant cause is doctor factor due to
incompleteness ones. On the other hand, based on
interviewed with the 3 filing staffs, the all agreed
on their owned mistakes due to place at wrong sub
shelf. That is the smallest percentage that shows at
table 2. On the other words, the interview outcome
has different side with observation data that we
take in the month June to July 2017. It also means
that misfiling incidents have never checked or
evaluated before by them therefore they did not
aware about the cause of these evident. Good
medical record keeping is at the forefront of
medical practice. Complete and accurate medical
records will meet all legal, regularly and auditing
requirements (Ebirim NL., Buowari YO., 2013).
Completeness health record is the presence of
all necessary information of patients based on
standard and all entry are dated and signed; it must
be completing by 2x24 hours. Health record
completeness is a key performance indicator that is
associated with delivery of health services in the
hospital. Improving health record completeness
service is an important step towards improving the
quality of hospital. It can also provide valuable
information to help measure progress and
effectiveness (Kasu T, Haftom A, Yemane G, and
Birhanu J, 2017).
Secondly; the highest cause of misfile due to
doctors who have not completed the medical
record more than 24 hours. This cause related to
centralization system in keeping health record
management. This means that each patient has only
one health record, whether they receive outpatient
services or inpatient will be placed in a single file.
So when the patient who has been discharge from
hospital, then make visits for control in outpatient
at the other day and filling staff not found health
record at filling room. It will end up with result in
misfile medical records. This is one of the
shortcomings of the centralized system. The
finding of Kasu T., Haftom A., Yemane G., and
Birhanu J., 2017 projects suggest that a simple of
intervention availing inpatient health record format
and training hospital provider improves the
inpatient health record completeness. Thirdly, the
solution from their point of view is how to build
adequate filing space and change from health
record to electronic health record. However,
shelving and space is the second largest factor that
cause in misfiling health record. Cortes PL, and de
Paula Cortes EG, 2011 the most cases resulted in
multiple patients folder and led to misfiling was
shown to be shelving and space, staff and logistic.
and there was significant reduction in the use of
multiple folder for five months intervention period
by electronic health record implementation.
The electronic health record, with its advance
storage, accessibility and linkage capacities, can be
leveraged to reduce diagnostic errors by providing
quick access to information, the ability to share
assessments in real time between clinicians and
with patients and advanced capabilities to follow
up test result and track medication, whilst also
providing access to electronic sources of
knowledge information at the point of care (schiff
and Bates, 2010).
Hence, electronic health record have potential
to improve patient safety, and the efficiency and
effectiveness of healthcare delivery (Callen J.,
2014). Based on the best way to avoid misfiling,
Teviu EAA et al, 2012 state that proper filing of
patient’s health records ensures easy retrieval and
contributes to decreased patient waiting time at the
hospital and ensures continuity of care. Moreover,
studied show in other developing countries have
observed their record keeping systems to be in
adequate with about half (52,2%) of the records
retrievable within one hour, some records were
poorly designed and there is use of multiple patient
health records by patients (Aziz S and Rao MH,
2002; Kerry TP, 2006 in Teviu EAA et al, 2012).
In the term of satisfaction using electronic
health record, study shown that patients believe
that electronic health record enabled more personal
time with their providers by improving the quality
of visit. Patients could benefit by reducing the
incidence of various provider asking the same
question in previous visit by nurses or physicians
(Rose, Richter, & Kapustin, 2014).
E-Health Implementation in Support of Hospital Service at Indonesia of Health National Insurance Era - Study on MHR at DMS Surabaya
301

5 CONCLUSION
Overall, the most significant cause of misfiling
health records based on observation is the doctor
while the highest issue is the health records have
not returned to filing room for more than 2x24
hours. Based on the interview outcome, all of
respondents agree at the most significant cause led
to misfiling is human error due to wrong sub shelf
and the best effective to avoid the problem by
building up electronic health record and fixing
problem at shelving and space. We recommended
to design and launch intervention program to
improve health record completeness and it
supposed to be an effective long term follow up to
assess the sustainability of intervention.
REFERENCES
Callen J. What is the impact of electronic health records
on the quality of health data?. Health Information
Management Journal. 2014;43(1):42. [cited 2017 28
August]. Available from :
http://himaa2.org.au/HIMJ/sites/default/files/HIMJ%
2043-1%20Callen%20Editorial.pdf
City Government Surabaya. Regulation of Mayor of
Surabaya No.5 Year 2013 of the Technology Use
Guidelines Information and Communication by the
Government Area. 2013. [cited 2017 17 May].
Available from :
https://jdih.surabaya.go.id/pdfdoc/perwali_810.pdf
Pemerintah Kota Daerah Surabaya. Peraturan Walikota
Surabaya No. 5 Tahun 2013 tentang Pedoman
Penggunaan Teknologi Informasi Dan Komunikasi
Oleh Pemerintah Daerah. 2013. [cited 2017 28
August]. Available from :
https://jdih.surabaya.go.id/pdfdoc/perwali_810.pdf
Côrtes PL, Côrtes EG. Hospital information systems: a
study of electronic patient records. JISTEM-Journal
of Information Systems and Technology
Management. 2011;8(1):131-54. [cited 2017 28
August ]. Available from:
http://dx.doi.org/10.1590/S1807-
17752011000100008
Ebirim NL, Buowari YO. Record Keeping by
Anaesthetist in a Developing Country. Afrimedic
Journal. 2013;4(1):29-31. [cited 2017 28 August ].
Available from :
https://www.ajol.info/index.php/afrij/article/downloa
d/94556/83928
Karlina, D., Putri, I. A., Santoso, D. B., Studi, P.,
Rekam, D., Universitas, M., & Mada, G. (2016).
Kejadian Misfile dan Duplikasi Berkas Rekam
Medis Sebagai Pemicu Ketidaksinambungan Data
Rekam Medis. Kesehatan Vokasional, 1(1), 44–52.
Retrieved from
https://jurnal.ugm.ac.id/jkesvo/article/download/274
77/16829
Mboi, N. (2015). Indonesia: On the Way to Universal
Health Care. Health Systems & Reform, 1(2), 91–97.
https://doi.org/10.1080/23288604.2015.1020642
Rose, D., Richter, L. T., & Kapustin, J. (2014). Patient
experiences with electronic medical records: lessons
learned. Journal of the American Association of
Nurse Practitioners, 26(12), 674–80.
https://doi.org/10.1002/2327-6924.12170
Schiff GD, Bates DW. Can electronic clinical
documentation help prevent diagnostic errors?. New
England Journal of Medicine. 2010 Mar
25;362(12):1066-9
Teviu EA, Aikins M, Abdulai TI, Sackey S, Boni P,
Afari E, Wurapa F. Improving medical records filing
in a municipal hospital in Ghana. Ghana medical
journal. 2012 Sep;46(3):136. [cited 2017 28 August
]. Available from :
http://www.nejm.org/doi/full/10.1056/NEJMp09117
34#t=article
Tola K, Abebe H, Gebremariam Y, Jikamo B. Improving
Completeness of Inpatient Medical Records in
Menelik II Referral Hospital, Addis Ababa, Ethiopia.
Advances in Public Health. 2017 Apr 12;2017. [cited
2017 28 August ]. Available from :
https://doi.org/10.1155/2017/8389414
Thabrany, Hasbullah. 2015. Health National Insurance.
2
nd
Ed. Jakarta : Rajawali Press.
Thabrany, Hasbullah. 2015. Jaminan Kesehatan Nasional
Edisi kedua. Jakarta : Rajawali Press.
WHO. (2017a). WHO | What is universal coverage?
WHO. Retrieved from
http://www.who.int/health_financing/universal_cove
rage_definition/en/
WHO, I. (2017b). World Health Organization, Universal
Health Coverage and Health Care Financing
Indonesia. SEARO. Retrieved from
http://www.searo.who.int/indonesia/topics/hs-
uhc/en/
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
302
