
Number and Types of Complication in Type 2 Diabetes Correlated
with Outpatient Treatment Cost Using BPJS Self-Funded Scheme in
Islamic Hospital Jombang
Rofida Lathifah
1,2
*, Abdul Ghofir
2,3
, Djazuly Chalidyanto
1
, Tito Yustiawan
1
1
Faculty of Public Health, Airlangga University, Mulyorejo, Surabaya, Indonesia
2
Islamic Hospital Jombang, Jombang, Indonesia
3
Faculty of Medicine and Health Science, Muhammadiyah University, Yogyakarta, Indonesia
fida619@gmail.com
Keywords: BPJS, Complication, Diabetes, Outpatient, Treatment cost.
Abstract: The treatment cost of type 2 diabetes outpatients with complications is estimated to exceed the cost of
uncomplicated diabetes. However, Ina CBG’s claim was generalised regardless of the diabetes type case
(IDR 155.000/visit). This study aims to determine the correlation between the number and type of
complications in type 2 diabetes patients to treatment cost and their conformity with Ina CBG’s claim. The
research was conducted by way of a cross-sectional study. Secondary data was taken from type 2 diabetes
outpatients using a BPJS self-funded scheme in RSI Jombang from 1
st
January-31
st
December 2014 with
110 samples analysed by Kruskal Wallis, Spearman Rho and Chi Square. There was a positive and
significant correlation between the number and type of complications in type 2 diabetes with the treatment
cost (r=0.414, p=0.001;r=0.430, p=0.001). There was a significant difference (p=0.001) between the average
cost of diabetes without complications (IDR 99.049 ± 9.316) with one complication (IDR 112.722 ± 20.468)
and with two complications or more (IDR 120,711 ± 18,512). It was concluded that there was increase in
the average cost of diabetes outpatients with complications in RSI Jombang but not to the point of
exceeding Ina CBG’s claim.
1 INTRODUCTION
Diabetes mellitus is a metabolic disease
characterised by hyperglycemia resulting from
defects in insulin secretion, insulin action, or both.
The chronic hyperglycemia of diabetes is associated
with the long-term damage, dysfunction, and failure
of various organs, especially the eyes, kidneys,
nerves, heart, and blood vessels (American Diabetes
Association, 2007). Shaw et al., (2010) estimated
that the world prevalence of diabetes among adults
aged 20–79 years was 6.4% (285 million) in 2010,
and will increase to 7.7% (439 million) by 2030. The
prevalence of diabetes mellitus in productive age
urban Indonesians was 4.6% (Mihardja et al., 2014).
The treatment cost of type 2 diabetes is
associated with the progression of the disease and its
complications (Vaivadait & Padaiga, 2014). In the
previous health insurance system, PT. Askes
reported that type 2 diabetes management costs more
than 22.4 million USD in 2010. The patient
management of uncomplicated diabetes requires $40
USD/patient/year and complicated patients require a
higher cost of $800 USD/patient/year (Soewondo,
Ferrario & Tahapary, 2013). However, Ina CBG’s
(Indonesian National Social Health Insurance
reimburse package) claim for type 2 diabetes
outpatients was generalised regardless of the
complication frequency (IDR 155.000/visit).
Healthcare facilities were disallowed to charge fees
to BPJS (Badan Penyelenggara Jaminan Sosial/
Indonesian National Social Health Insurance)
payers. Health care facilities are not allowed to ask
the fee of the patient as long they get the benefit of
health care according to their human rights (Law of
Ministry of Health, 2014). Outpatient treatment
costs for BPJS self-funded payers should not exceed
Ina CBG’s claim. Some hospitals have charged
additional costs to the patient under a consent for
them to gain better treatment. BPJS self-funded
payers who have been diagnosed with type 2
290
Lathifah, R., Ghofir, A., Chalidyanto, D. and Yustiawan, T.
Number and Types of Complication in Type 2 Diabetes Correlated with Outpatient Treatment Cost Using BPJS Self-Funded Scheme in Islamic Hospital Jombang.
In Proceedings of the 4th Annual Meeting of the Indonesian Health Economics Association (INAHEA 2017), pages 290-294
ISBN: 978-989-758-335-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
diabetes are at risk of paying more outside Ina
CBG’s scheme.
In Jombang Islamic Hospital, type 2 diabetes
occupied the top most common diagnosis in the
Outpatient Department and more than 70% patients
were using the BPJS self-funded scheme. Therefore,
this study aims to determine the correlation between
the number and type of complications in type 2
diabetes patients with treatment cost and its
conformity with Ina CBG’s claim in RSI Jombang.
2 METHODS
This research was using retrospective study based on
the data collected from medical records and
treatment bills per visit from type 2 diabetes
outpatients in 2014. Treatment bills included were
internist specialist consultation fees, drug use costs
(for seven days) and ancillary examinations
(laboratory and radiology). The population was the
outpatients in the Internal Medicine Clinic of Islamic
Hospital Jombang using the BPJS self-funded
scheme. The inclusion criteria was that they had
been diagnosed with type 2 diabetes and the
exclusion criteria was uncompleted data or a patient
that had been co-diagnosed with malignancy,
tuberculosis, and HIV. There were 110 samples
taken from the population who met the criteria.
The number of complications was grouped into
three categories; type 2 diabetes without
complications, diabetes with at least one
complication and diabetes with two complications or
more. The types of complications were grouped into
four categories. Type 2 diabetes without
complication, microvascular complications,
macrovascular complications, and both
complications. The treatment cost was classified into
three categories: low (<IDR 100.000), moderate
(IDR100.000-120.000) and high (>IDR 120.000).
Statistical data analysis was performed using
statistic software. Spearman's test was used to
evaluate the correlation between the number of
complications in type 2 diabetes with treatment cost
(p=0.05) while the difference was analysed by
Kruskall Wallis and Mann-Whitney (p=0.05). Chi
Square and Contingency Coefficient was used to
evaluate the correlation between the type of
complications in type 2 diabetes with the treatment
cost.
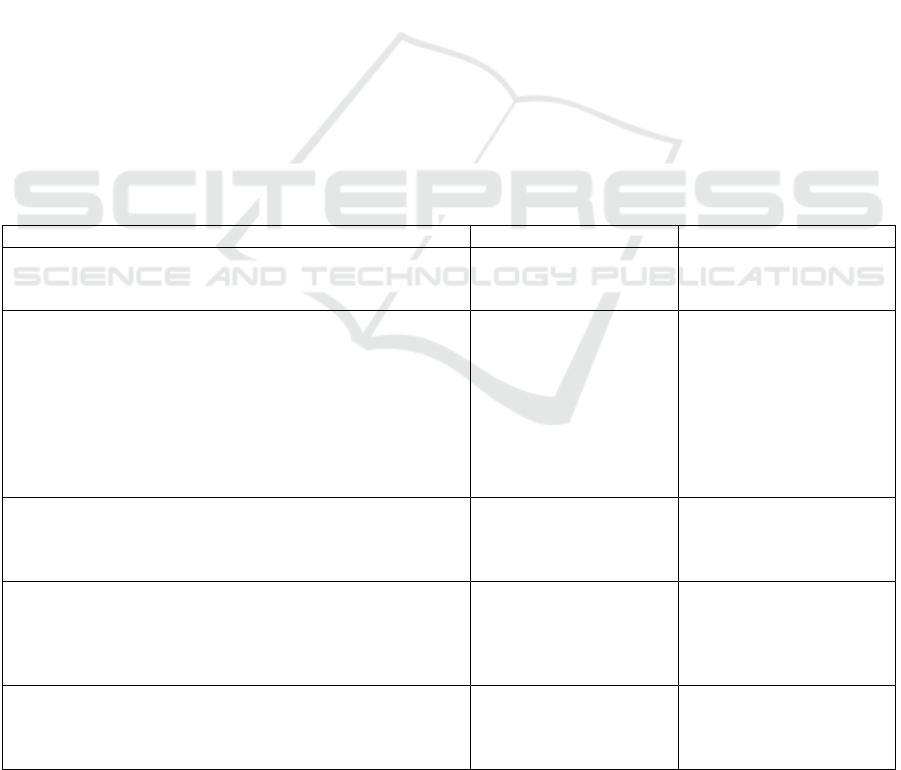
Table 1: Sample characteristic distribution (n=110)
Characteristic
n
%
Gender
Male
Female
42
68
38,2
61,8
Age (years)
<40
41-45
46-50
51-55
56-60
61-65
66-70
>70
4
10
15
21
29
15
11
5
3,64
9,09
13,64
19,09
26,36
13,64
10
4,54
Number of Complication
Without complication
One complication
Two complications or more
17
59
34
15,45
53,65
30,9
Type of Complication
Without complication
Microvascular
Macrovascular
Microvascular & Macrovascular
17
44
28
21
15,45
40
25,45
19,1
Treatment Cost per Visit (IDR)
<100.000
100.000-120.000
>120.000
29
52
29
26,36
47,28
26,36
Number and Types of Complication in Type 2 Diabetes Correlated with Outpatient Treatment Cost Using BPJS Self-Funded Scheme in
Islamic Hospital Jombang
291
3 RESULTS
A total of 110 samples were included in the analysis.
The demographic profile of the patients has been
shown in Table 1. There was a greater proportion of
women diagnosed with type 2 diabetes (61.8%
women vs. 38.2% men). Most of the patients were
56-60 years old (26.36%) and 51-55 years old
(19,09%). In total, 53.65% of patients with type 2
diabetes had at least one complication, with 40%
having microvascular only and 25,45% having
macrovascular only complications. Despite having
the complications, all of the treatment costs did not
exceed Ina CBG’s claim (<IDR 155.000).
3.1 Number of Complications Correlated
with Treatment Cost
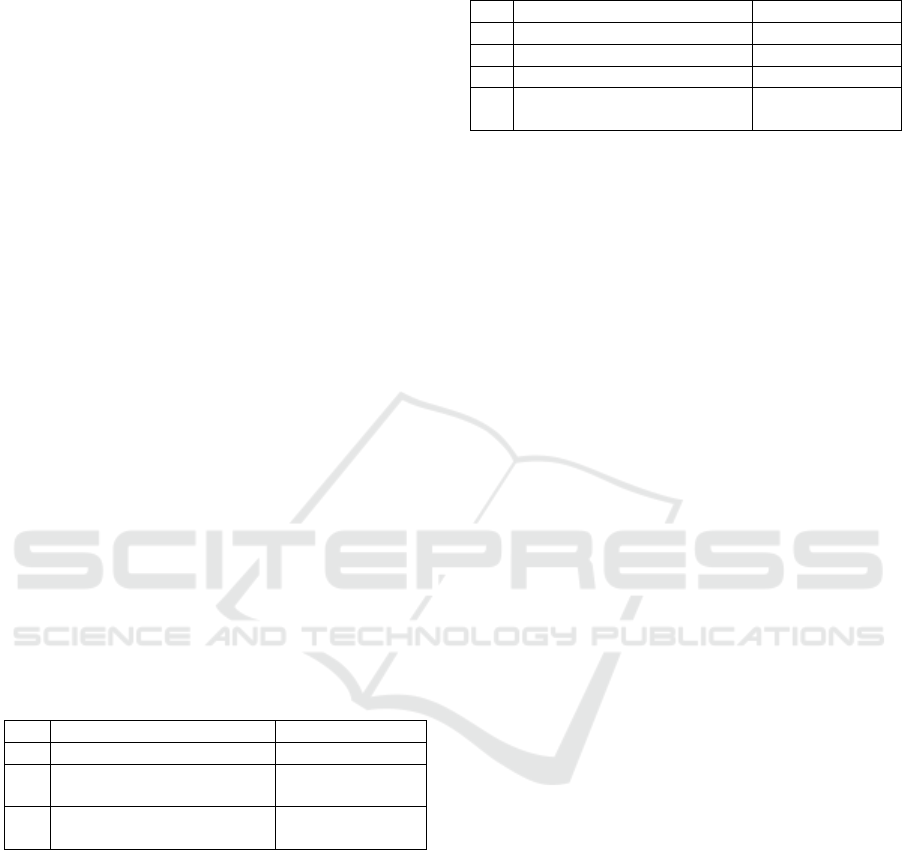
The average treatment cost per patient increased
gradually with the number of complications from
IDR 99.049 ± 9.316 in patients without
complications to IDR 112.722 ± 20.468 in patients
with one complication and IDR 120.711 ± 18.512 in
patients with more than one complication. There was
a positive and significant correlation between the
number of complications in type 2 diabetes with the
treatment cost (r=0.414, p=0.001) and there was also
a significant difference between the average cost of
diabetes without complications, with one
complication and with two complications or more
(p=0.001).
Table 2: Average treatment cost per patient per visit with
number of complications
No
Number of Complication
Mean
1
Without Complication
99.049 ± 9.316
a
2
One Complication
112.722 ±
20.468
b
3
Two Complications or
more
120.711 ±
18.512
c
Different notation shows signifficance difference*p<0.05
3.2 Type of Complication Correlated with
Treatment Cost
There was a positive and significant correlation
between the type of complications in type 2 diabetes
with treatment cost (r=0.430, p=0.001). Patients with
both microvascular and macrovascular
complications had higher costs (IDR 124.449 ±
21.133) compared to those with either microvascular
(IDR 115.828 ± 22.057) or macrovascular (IDR
108.747 ± 12.430) complications, and also within
type 2 diabetes without complications (IDR 99.049
± 9.316).
Table 3: Average treatment cost per patient per visit with
the type of complication
No
Type of Complication
Mean
1
Without Complication
99.049 ± 9.316
2
Microvascular Complications
115.828 ± 22.057
3
Macrovascular Complications
108.747 ± 12.430
4
Microvascular and
Macrovascular Complications
124.449 ± 21.133
*p<0.05
4 DISCUSSION
This was the first study conducted in RSI Jombang
that analysed type 2 diabetes complications and its
correlation with treatment cost. Most of the patients
in RSI Jombang were BPJS payers and the payment
scheme for BPJS reimbursement package used in Ina
CBG’s claim. Ina CBG’s claim for type 2 diabetes
outpatient was generalised regardless of the
complications (IDR 155.000/visit). Thus, it is
important to know the correlation between the
number and type of complication in type 2 diabetes
with treatment cost so that it can be managed
efficiently.
The treatment cost of type 2 diabetes is
associated with the progression of the disease and its
complications (Vaivadait & Padaiga, 2014). This
study found that there was a positive and moderate
correlation between the number of type 2 diabetes
complications and the average cost per visit
(r=0.414, p=0.001). Therefore, it can be concluded
that increase number of complications related with
higher average cost per visit. A study in India also
found that the total costs for patients without
complications reached INR 4.493 (USD 92.15)
compared to INR 14.691.75 (USD 301.32) for
patients with complications (Yesudian, et al., 2014).
Therefore, it is important for patients and hospitals
to maintain blood sugar levels in type 2 diabetes
patients to reduce the risk of them developing
complications so then the treatment cost can be
lowered.
A previous study in Singapore proved that
microvascular and macrovascular complications
tend to increase the cost of care (Shuyu, et al.,
2015). Another study by Dimitrova et al., (2015)
showed increase of diabetes management cost for
microvascular complication by 23% and
macrovascular complication by 31%. Similar result
was found in this study. It was confirmed that there
was a positive and moderate correlation between the
type of complications in type 2 diabetes with the
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
292

average cost per visit (r=0.430, p=0.001). There
were significant cost increases in relation to both
microvascular (IDR 115.828 ± 22.057) and
macrovascular complications (IDR 108.747 ±
12.430) compared with no complications (IDR
99.049 ± 9.316). Highest cost was found in type 2
diabetes with both microvascular and macrovascular
complications (IDR 124.449 ± 21.133). Result of
this study confirmed the previous study results that
patients with both microvascular and macrovascular
complications had a higher cost than patients
without both complications (Henrikson, et al., 2000).
Previous study in Indonesia also showed that
microvascular and/or macrovascular complication
increased the treatment cost up to 130% compared
with non-complicated diabetes (Andayani et al.,
2010).
On average, annually treatment cost for diabetic
patient with microvascular complication cost $1900
more than non-complicated diabetes while
macrovascular cost $3900 more (Nichols et al.,
2008). Thus, type 2 diabetes complications impact
on treatment cost should be considered by hospitals
to provide appropriate treatment and prevention for
both microvascular and macrovascular
complications. Prevention and early treatment can
save the diabetes treatment cost up to $6836
annually (Palmer et al., 2004).
In addition, there was a significant difference
between the average treatment cost of type 2
diabetes with microvascular and macrovascular
complications. The average treatment cost was
higher in type 2 diabetes with microvascular
complications. Contrary to the study in the US
whereas macrovascular complications were the
major component of type 2 diabetes costs compared
to microvascular complications (Caro, Ward &
O’Brien., 2002). This may be due to the
hospitalisation costs were included in the previous
study because macrovascular disease-related
hospitalisations were more common in patients with
type 2 diabetes related to unregulated diabetes
(Dimitrova, et al., 2015). Moreover, the direct cost
for hospitalisation purposes (inpatient care) for type
2 diabetes was the largest expenditure (Vaivadait &
Padaiga, 2014). Whereas in this research, no
hospitalisation cost was included.
BPJS self-funded payers have the possibility of
ilegally charged with additional fees outside the Ina
CBG package ranged from IDR 4.000-2.000.000
(Gultom, 2015). In this study, the highest average
cost per visit was found in type 2 diabetes patients
with two or more complications (IDR 120.711 ±
18.512), and also in relation to both microvascular
and macrovascular complications (IDR 124.449 ±
21.133). Neither exceeded the outpatient reimburse
package from Ina CBG’s claim (IDR 155.000). This
suggests that despite the increase in the average cost
per visit for type 2 diabetes outpatients with
complications, Ina CBG’s package can still be
adequate in RSI Jombang. This study confirmed that
the BPJS outpatient reimburse package for type 2
diabetes with complications has covered the total
costs spent by RSI Jombang. Therefore, additional
fees are unnecessary (not needed) for now. This
because the hospital already has good policies and
efficient procedures (medical examination and drug
selection) to give appropriate treatment. Therefore,
as long as the hospital can practice these good
management process, no additional fees should be
needed. This achievement is important since in
2019, all hospital in Indonesia should participate in
BPJS scheme (Mboi, 2015). In return, this will
improve hospital efficiency for BPJS treatments.
5 CONCLUSIONS
This study concluded that there was a positive and
signifficant correlation between the number of
complications in type 2 diabetes with the average
treatment cost of the patients (BPJS self-funded
payers) in the Internal Medicine Clinic of RSI
Jombang. The hospital must strive to improve
treatment efficiency in order to control treatment
costs. This study also found that the BPJS outpatient
reimburse package was sufficient enough to cover
type 2 diabetes and its complications treatment in
RSI Jombang, regardless that the average cost was
increased.
REFERENCES
American Diabetes Association. Diagnosis and
Classification of Diabetes Mellitus. 2004. Diabetes
Care [Internet]. 2004;27(Supplement 1):S5–10.
Available from:
http://care.diabetesjournals.org/cgi/doi/10.2337/diacar
e.27.2007.S5
Andayani T, Ibrahim M, Asdie A. Assessing the impact of
complications on the direct medical costs of type 2
diabetes mellitus outpatients. Int J Cur Phar Res.
2010;9(2):32–35.
Caro JJ, Ward AJ, O’Brien JA. 2002. Lifetime Costs of
Complications Resulting from Type 2 Diabetes in the
U.S. Diabetes Care [Internet]. 2002 Mar 1;25(3):476
LP-481. Available from:
Number and Types of Complication in Type 2 Diabetes Correlated with Outpatient Treatment Cost Using BPJS Self-Funded Scheme in
Islamic Hospital Jombang
293

http://care.diabetesjournals.org/content/25/3/476.abstr
act
Dimitrova M, Doneva M, Valov V, Yordanova S, Manova
M, Savova A, et al. 2015. Cost of hospitalizations due
to microvascular and macrovascular complications in
type 1 and type 2 diabetic patients in Bulgaria.
Biotechnol Biotechnol Equip [Internet].
2015;29(4):805–13. Available from:
http://dx.doi.org/10.1080/13102818.2015.1042912
Gultom, Novianti. 2015., Illegal Cost Sharing for Hospital
Care: Survey from Indonesian National Health
Security Member [Internet].
http://inahea.org/files/hari1/4.%20Novianti%20Br%20
Gultom.pdf. Accessed at 25 December 2017
Henriksson F, Agardh CD, Berne C, Bolinder J, Lönnqvist
F, Stenström P, et al. 2000., Direct medical costs for
patients with type 2 diabetes in Sweden. J Intern Med.
2000;248(5):387–96.
Law of Ministry of Health Number 28 Year 2014 About
National Health Insurance Program Implementation
Guide
Mboi Nafsiah. 2015., Indonesia: On the Way to Universal
Health Care, Health Systems & Reform, 1:2, 91-97
Mihardja, L., Soetrisno, U., & Soegondo, S. 2014.,
Prevalence and clinical profile of diabetes mellitus in
productive aged urban Indonesians. Journal of
Diabetes Investigation, 5(5), 507–512.
http://doi.org/10.1111/jdi.12177
Palmer AJ, Roze S, Valentine WJ, Spinas GA, Shaw JE,
Zimmet PZ. 2004., Intensive lifestyle changes or
metformin in patients with impaired glucose tolerance:
modeling the long-term health economic implications
of the diabetes prevention program in Australia,
France, Germany, Switzerland, and the United
Kingdom. Clin Ther.26:304–321.
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the
prevalence of diabetes for 2010 and 2030. Diabetes
Res Clin Pract 2010; 87: 4–14
Shuyu Ng C, Toh M, Ko Y, Lee J. 2015., Direct medical
cost of type 2 diabetes in Singapore. PLoS One.
10(3):1–11.
Soewondo P, Ferrario A, Tahapary DL. 2013., Challenges
in diabetes management in Indonesia: a literature
review. Global Health [Internet]. 9:63–80. Available
from:
http://search.proquest.com.virtual.anu.edu.au/docview/
1491517774/fulltextPDF/E53ABED4535C4A40PQ/1
37?accountid=8330
Vaivadait J, Padaiga Ž. 2014., Direct cost of patients with
type 2 diabetes mellitus healthcare and its
complications in Lithuania. Science Direct., 0:0–6.
Yesudian CAK, Grepstad M, Visintin E, Ferrario A.
2014., The economic burden of diabetes in India: a
review of the literature. Global Health [Internet].
2014;10:80. Available from:
http://www.ncbi.nlm.nih.gov/pubmed/25443136%5Cn
http://www.pubmedcentral.nih.gov/articlerender.fcgi?
artid=PMC4279984
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
294
