
The Changing Nature of Campus Health Insurance: Testing
Portability Issues of National Health Insurance
Nuzulul Kusuma Putri and Ernawaty Ernawaty
Faculty of Public Health Universitas Airlangga, Mulyorejo, Surabaya, Indonesia
nuzululkusuma@fkm.unair.ac.id
Keywords: Migrant students, Campus, Health insurance, National health insurance.
Abstract: Before National Health Insurance was implemented, the majority of leading universities in Indonesia
already covered their students with a health insurance scheme. They managed their own campus health
insurance independently. Both National Health Insurance in 2014 and single tuition policy in 2015 brought
huge change to campus health insurance. This study aims to analyse students' needs in health insurance after
implementation of these policies. This is an exploratory study with cross-sectional design. The sample was
taken by voluntary sample through online questionnaire. There were 83 students across different academic
degree participated in this study. Most of the students (65.1%) came from various districts outside the
campus district and chose to reside in boarder houses around the campus. There were only 52.9% of the
students already listed as National Health Insurance participants. Out-of-pocket risk belongs to 35.5%
students who were not covered by health insurance at all. Almost all of the students who already
participated in National Health Insurance (93.3%) were registered in the primary healthcare in their
hometown. The students are already paying for single tuition which does not accommodate health
insurance. A real changing need of migrant students for health insurance coverage exists in the National
Health Insurance era.
1 INTRODUCTION
Universal Health Coverage swept many countries
in the last decade, including Indonesia. Even though
Indonesia is the biggest archipelago country with a
widely dispersed territory, National Health
Insurance is chosen as the health insurance
mechanism rather than region-based insurance. This
decision has consequences in the portability
challenges of the preferred health insurance scheme.
Previous region-based health insurance mechanisms
already implemented by local government should be
merged into a national scheme. It should enable not
only raising the pooling level in local government,
but also maintaining the cross-regional participation
transfer (Pan et al., 2016).
Previously, the majority of universities in
Indonesia had institutionally managed health
services for their students before the enactment of
the National Health Insurance. The provision of this
health service is funded through a student health
insurance scheme that is managed independently by
the university and which is limited only for students
in the university. Student health insurance is
regulated through the policy of each rector.
Generally, this fund pooling is collected through a
semi-annual contribution in addition to the tuition
fee. These funds are managed to finance the health
of students during their education. However, in
accordance with the mandate of the Ministry of
Education, universities are not permitted to collect
additional fees outside the national rate. However,
the calculation of this national rate does not
accommodate student healthcare insurance. The
National Health Insurance that was launched one
year previously also makes this situation more
complicated. The availability of parental health
insurance can have significant effects on the
probability that a young individual enrols as a full-
time student in university (Jung et al., 2013).
Unfortunately, there is no individual student
membership in National Health Insurance. To be
able to be covered by National Health Insurance,
students should be registered with all of their family
members.
The huge variations of health insurance
mechanisms bring many obstacles to the citizens
who wish to temporarily move to another region for
some years. In Indonesia, young adults from rural
regions who have just graduated from senior high
14
Putri, N. and Ernawaty, .
The Changing Nature of Campus Health Insurance: Testing Portability Issues of National Health Insurance.
In Proceedings of the 4th Annual Meeting of the Indonesian Health Economics Association (INAHEA 2017), pages 14-19
ISBN: 978-989-758-335-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
school compete to be able to enrol in the best
universities, which are mostly located in urban
regions. According to Callahan (2007), young adults
are twice as likely to be uninsured as children or
older adults. This specific group is a form of a
mobile population with a disproportionate number of
unemployed or irregularly employed members who
must weigh the financial and time costs of their
study and living costs.
Moreover, Pan et al. (2016) explained that a
migrant population which is already covered by
health insurance is commonly restricted from
claiming benefits in the destination region. On the
other hand, these migrants consistently underuse
services in both their communities of origin and
their destination cities. The probability for students
to voluntary register into health insurance is also
possibly small. Undergraduate students appear to
have formed perceptions on health insurance which
is similar to adult including their family (Price PhD,
MPH et al. 2010). The unclear identity of
civilization is worsen their willingness to participate
in a national health insurance program. Study by
Ybarra et al. (2017) addressed a gap in the literature
on access and use of health insurance and routine
medical and dental care among children by including
the legal statuses of both parents and children, there
are limitations.
Based on those background, this study examines
how the portability issue of National Health
Insurance in Indonesia has impacted the students’
need of health insurance after implementation of the
policies.
2 METHOD
This is an exploratory study analysing the
implications of National Health Insurance policies
affecting a university providing a healthcare service
for its students during college. The data were
collected by cross-sectional survey in the second
year of implementation of National Health
Insurance. The sample was taken by voluntary
sample through online questionnaire. The
questionnaires were broadcast to various student
groups on the official social media of the university.
At the end of a week of data collection period, there
were 83 students across different academic degrees
and universities who participated in this study.
The survey captures the student characteristics
related to National Health Insurance membership
requirement and student utilisation of healthcare
service during college. The need of college students
for health insurance after implementation of
National Health Insurance was analysed by
comparing the gap between both sections.
3 RESULT & DISCUSSION
The majority of respondents (65.1%) are migrant
students whose home is not in the same city as the
campus location. Most of the students choose to live
near the campus by moving to the city in which
campus is located. Many of the students who
participated in this study are of undergraduate level.
This means that most of the students are of young
adult age. This age group is dominantly dependent
on their parents for all their living costs. Based on
the membership conditions in the National Health
Insurance policy, this age group is still able to be
covered by parental health insurance by showing
that they are still not financially independent. The
possibility of parental health insurance is high due to
fact that more than half of the parent population are
wage earners. The National Health Insurance policy
officially regulates that the wage earners must be
registered by their employers in National Health
Insurance. The majority of migrant students
(52.9%), who are basically at some distance from
their parents’ authorisation during college, are
already protected through the National Health
Insurance mechanism. Unfortunately, the rest of the
migrant students are barely covered by any health
insurance during college. Moreover, there are still
30.1% of students who are not covered by health
insurance at all.
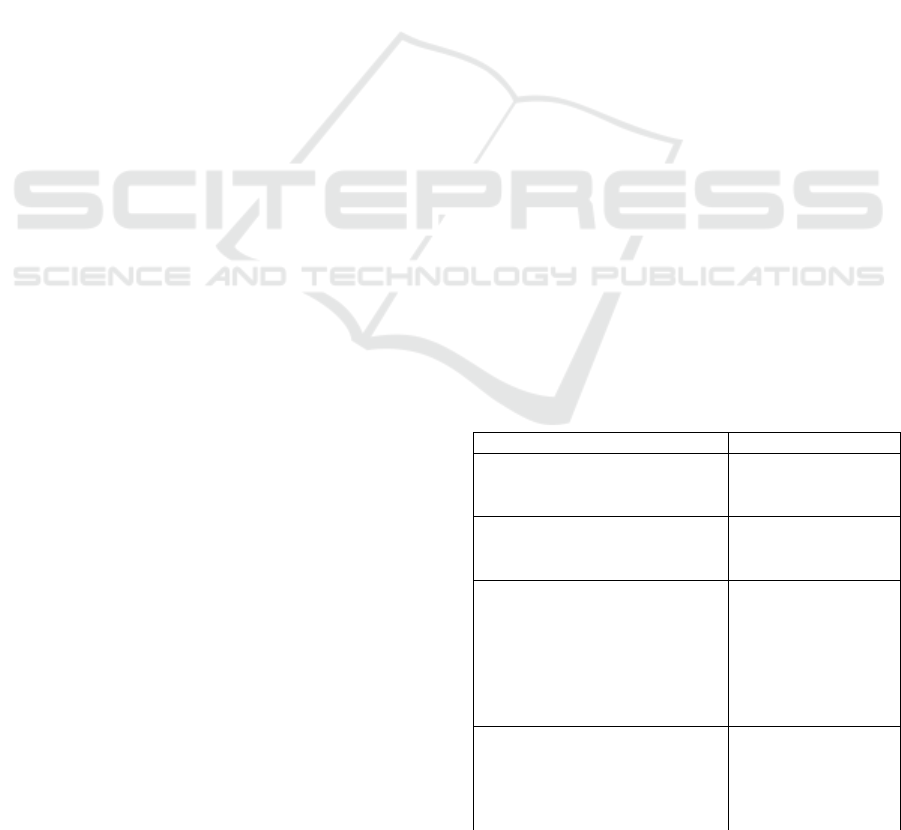
Table 1: Student characteristics
n
%
Student origin
Not migrant student
29
34.9
Migrant student
54
65.1
Home base while study
Move to campus location
73
88.0
Stay in hometown
10
12.0
Education level
Diploma
1
1.2
Undergraduate student
(extension)
11
13.3
Undergraduate student
(regular)
57
68.7
Post Graduate
14
16.9
Parents’ job
Civil servants
25
30.1
Unemployment
20
24.1
Informal workers
15
18.1
Private company employee
14
16.9
The Changing Nature of Campus Health Insurance: Testing Portability Issues of National Health Insurance
15
n
%
Pensioner
9
10.8
Health Insurance
National Health Insurance
44
53.0
Commercial Health
Insurance
10
12.0
Both
4
4.8
None
25
30.1
Those characteristics impact the health insurance
utilisation. Migrant students who are not covered by
health insurance should be able to set aside their
living cost for healthcare purposes when sick. In this
case, a university health insurance scheme is very
much needed to ensure accessible healthcare service
during college. In 2019, when the National Health
Insurance is targeted to reach universal health
coverage, the university health insurance scheme
should be considered as another option to crawling
the niche market of students that are left behind by
the implementation of National Health Insurance.
A second alignment that should also be
considered is the existence of students who are
already registered as National Health Insurance
participants, but still choose primary healthcare in
their hometown. Based on the National Health
Insurance regulations, participants should choose
one primary healthcare to be the patient’s first
contact in using the healthcare facilities. By
choosing the primary healthcare facility, participants
can only be treated by that chosen primary
healthcare. Participants are not be allowed to access
other primary healthcare, except for the emergency
room. The portability issue has become the main
problem in this case.
3.1 The Chosen Primary Healthcare: A
Matter of Portability Issues
In the term of National Health Insurance
implementation, participants cannot directly utilise
the referral hospital without appropriate medical
indications. There is a strict referral mechanism
which has been created to ensure that there will be
no unnecessary treatment which potentially
disembogues high treatment cost.
National Health Insurance participants should
choose only one primary healthcare facility. This
primary healthcare facility is responsible for treating
the registered participants. This will be paid for by a
capitation mechanism based on the number of
National Health Insurance participants registered in
the primary healthcare facility. Participants do not
need to pay anything to the primary healthcare
facility when accessing the services. Vice versa, the
primary healthcare facility is prohibited to take a fee
for its service to the participants. Unfortunately,
participants cannot access the other primary
healthcare facilities freely. If participants want to
access a different one, they must change their
primary healthcare facility. Table 2 shows that most
of the students who already registered as National
Health Insurance participants are varied according to
the primary healthcare facility type chosen.
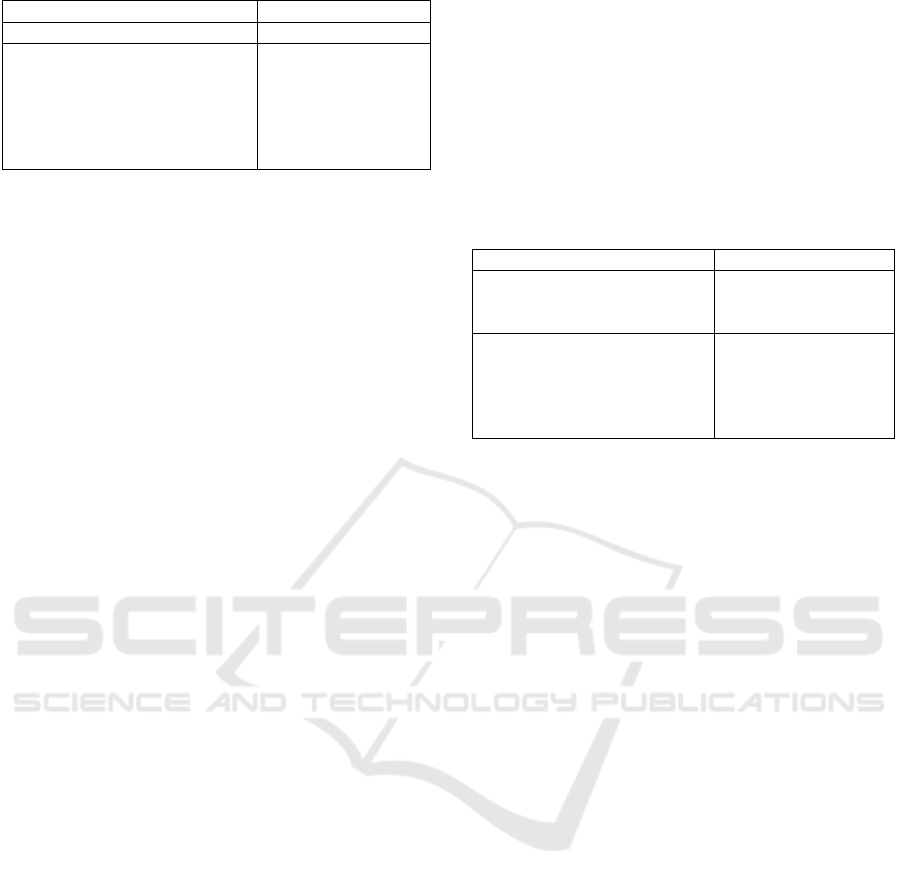
Table 2 The chosen primary healthcare facility by students
n
%
Location
Hometown
40
90.9
City of present campus
4
9.1
Type
General practitioner
13
29.5
24-hour clinic
4
9.1
Company-affiliated clinic
2
4.5
Public health centre
25
56.8
Most of the primary healthcare facilities chosen
by students are located in the student’s hometown.
Even though these students realise the long period of
study in college, they have decided to not change
their primary healthcare facility to a primary
healthcare facility located near their present college.
This means that this group of students will be face
difficulties when assessing a primary healthcare
facility using the National Health Insurance.
Students either need to return to their hometown to
access primary healthcare without charge or pay to
get treatment in their current city.
What if there is an emergency situation? National
Health Insurance accommodates emergency
situations, but with specific medical indications for
each disease or accident. Students with National
Health Insurance can use emergency treatment only
in the emergency room of a hospital without
consideration of where their primary healthcare
facility is situated. Even though students can access
it without any fee, incidence of emergency situations
is commonly rare. Most of the illnesses among
students are not considered as emergency cases. As
such, primary healthcare still becomes the first need
of students.
In spite of decentralization which promises to
bring health equity among citizens, the implications
of decentralised governance of health systems on
health- related equity are varied and depend on pre-
existing socio-economic and organisational context
(Costa-Font & Moscone 2008). It also argued that
decentralization results in ambiguous consequences
on efficiency; equity consequences are controversial
and address the relevance of redistribution
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
16
mechanisms (Alves et al. 2013). Whereas
decentralization is pointed to responsible financing
the mobile citizens across the district area.
3.2 Students’ Need of Healthcare during
College
Normally, undergraduate students spend 3-4
years of their life struggling to graduate from
college. During this period, there are many
possibilities of students getting sick or having
accidents. Table 3 shows how students deal with
these conditions during college.
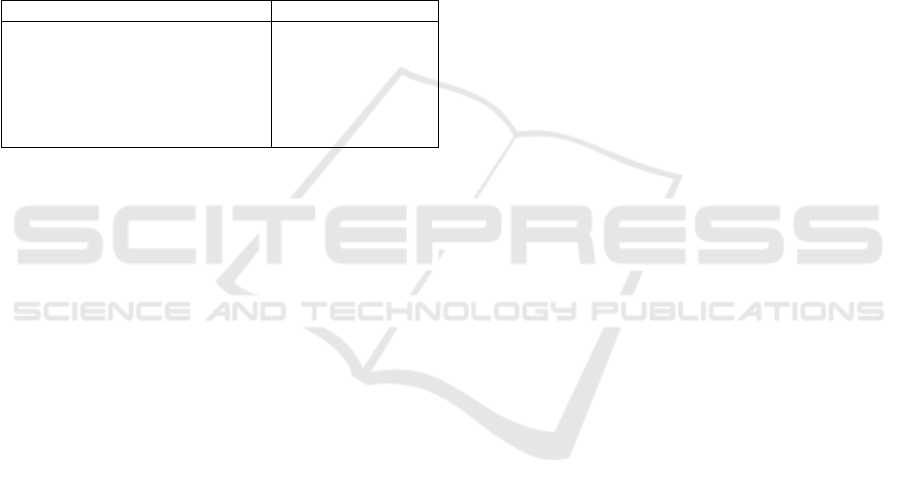
Table 3: Health-seeking behaviour of students during
college
Health-seeking behaviour
n
%
Self-treatment
24
28.9
Utilise private healthcare (OOP)
18
21.7
Utilise health facility with
commercial insurance
2
2.4
Utilise campus clinic
32
38.6
Return to hometown
7
8.4
Most of the students choose to utilise the
healthcare facility that is provided by their
university. This shows that the most accessible
healthcare treatment for students during college is
the campus clinic. Students also tend to cure their
sickness by self-treatment. Self-treatment is
commonly found in Indonesia due to the ease of
obtaining over-the-counter (OTC) medicine. As
educated people, students are confident in guessing
what their illness is and what kind of medicine they
should buy.
Surprisingly, none of students who participated
in this study utilised a healthcare facility using the
National Health Insurance scheme in the college
location. Students who were registered as National
Health Insurance participants chose to return to their
hometown to get treatment. This indicates that
portability issues still exist in the implementation of
National Health Insurance among migrant members.
Private health providers, including private healthcare
facilities and commercial health insurance providers,
could take advantage through this situation. There
are 21.7% of students who prefer to utilise the
private healthcare facility. Most of the students spent
Rp150,000 ($11) each time in utilising this private
healthcare. They pay this through an out-of-pocket
(OOP) mechanism.
Experience of how China finances its health
insurance system shows that the behaviour
management and purchasing mechanisms of
National Health Insurance perform poorly (Liu et al.,
2014). National Health Insurance participation has a
weak negative or even no significant association
with the OOP of hospitalised patients. National
Health Insurance seems to fail to reduce people’s
OOP. This also happens in our study. The trend of
students using OOP is high even though National
Health Insurance is already implemented.
There are emerging healthcare needs of migrant
students considering the location of the primary
healthcare facility they choose. The majority of
migrant students (93.3%) registered as National
Health Insurance participants still belong to the
primary healthcare facility in their hometown.
Vietnam’s experience clearly suggests that health
insurance strongly increases the access and reduces
the financial burden in healthcare utilisation
(Sepehri et al., 2009). In the case of migrant students
in Indonesia, rural-to-urban migrants should be
given increased portability. Pan et al. (2016) suggest
that the government should think about raising the
level of pooling or develop specific policies on
cross-regional transfer of entitlements. Our findings
show that National Health Insurance simply cannot
promote the students’ ability to access healthcare in
the campus location if the portability issue still
exists.
3.3 Inefficiency of Healthcare Service among
Students
This study provides evidence that portability is
something that should be rethought in providing
insurance for college students. Different from other
levels of education, students in college are
commonly separated from their parents during study.
They must take care of their health by themselves.
Rising et al. (2007) explained that even though
health insurance facilitates access to care, enrolment
alone is not enough to ensure the receipt of
preventive health care. Study by Jung et al. (2013)
revealed that the availability of parental health
insurance can have significant effects on the
probability that a young individual enrols as a full-
time student. College enrolment policy is the first
screening effort to capture the ability of each student
in protecting their life during college. A study about
the health need of college students also shows that
they learn to manage their own health, gain their
health knowledge and begin to start health habits
during study period (Nguyen et al. 2016). These
findings imply that campus student health centres
should be better evaluate and facilitate health
education.
The Changing Nature of Campus Health Insurance: Testing Portability Issues of National Health Insurance
17

Before National Health Insurance
implementation, the college enrolment system in
Indonesia never prescribed that such students should
be covered by health insurance. By 2019, Indonesia
is targeted to achieve Universal Health Coverage.
Considering this roadmap, since 2017, the National
Health Insurance provider has cooperated with
universities to ensure that all new students are
already registered. Unfortunately, a university
cannot push their students to change their primary
healthcare facility to the campus clinic. This
potentially causes inefficiency in campus clinic
management. Universities should finance their
clinics in providing healthcare service for students.
On the other hand, students still have to pay the
National Health Insurance dues.
Moreover, most students in university in
Indonesia are regular undergraduate students who
have used the single tuition system for college
payment. In the single tuition system, the university
only permitted to collect funds from students once in
one education year. The amount of this fund is
determined by the Ministry of High Education. A
university should be able to manage this fund for all
education processes. Unfortunately, in the single
tuition fee policy, the amount of funds for students’
healthcare during college is unclear. University
clinics have difficulty in managing the health portion
that is embedded in the single tuition fee. The
benefit package received by students at the
university clinic is highly dependent on the
university’s ability in financing the campus clinic.
4 CONCLUSION
Indonesia faces big challenges regarding its
portability issues. The wide area of Indonesia brings
consequences in the application of National Health
Insurance across different primary healthcare
facilities across the country. Migrant college
students are one of the vulnerable groups of
population that have high risk in this case. The
portability issue regarding health insurance for
college students not only disadvantage them, but
also induces inefficiency in the campus clinic
management. The campus enrolment system should
be designed to accommodate this portability issue in
order to guarantee that all students will be able to
access a qualified healthcare service during study.
ACKNOWLEDGEMENTS
We would like to send our appreciation to the
management of Airlangga University Healthcare
Centre (AHCC) for intensive discussion about
campus clinic management in the National Health
Insurance scheme.
REFERENCES
Alves, J., Peralta, S. & Perelman, J., 2013. Efficiency and
equity consequences of decentralization in health: An
economic perspective. Revista Portuguesa de Saude
Publica, 31(1), pp.74–83. Available at:
http://dx.doi.org/10.1016/j.rpsp.2013.01.002.
Callahan, S.T., 2007. Bridging the gaps in health
insurance coverage for young adults. The Journal of
adolescent health : official publication of the Society
for Adolescent Medicine, 41(4), pp.321–2. Available
at: http://www.ncbi.nlm.nih.gov/pubmed/17875456.
Costa-Font, J. & Moscone, F., 2008. The impact of
decentralization and inter-territorial interactions on
Spanish health expenditure. Empirical Economics,
34(1), pp.167–184.
Jung, J., Hall, D.M.H. & Rhoads, T., 2013. Does the
availability of parental health insurance affect the
college enrollment decision of young Americans?
Economics of Education Review, 32(1), pp.49–65.
Available at:
http://dx.doi.org/10.1016/j.econedurev.2012.09.010.
Liu, K., Wu, Q. & Liu, J., 2014. Examining the
association between social health insurance
participation and patients’ out-of-pocket payments in
China: The role of institutional arrangement. Social
Science and Medicine, 113(2014), pp.95–103.
Available at:
http://dx.doi.org/10.1016/j.socscimed.2014.05.011.
Nguyen, J. et al., 2016. Use and interest in complementary
and alternative medicine among college students
seeking healthcare at a university campus student
health center. Complementary Therapies in Clinical
Practice, 24(2016), pp.103–108. Available at:
http://dx.doi.org/10.1016/j.ctcp.2016.06.001.
Pan, X.-F., Xu, J. & Meng, Q., 2016. Integrating social
health insurance systems in China. The Lancet,
387(10025), pp.1274–1275. Available at:
http://www.thelancet.com/article/S0140673616300216
/fulltext.
Price PhD, MPH, J.H. et al., 2010. College Students’
Perceptions and Experiences With Health Insurance.
Journal of the National Medical Association, 102(12),
pp.1222–1230. Available at:
http://proxygw.wrlc.org/login?url=http://search.proque
st.com/docview/822764203?accountid=11243%5Cnhtt
p://findit.library.gwu.edu/go?ctx_ver=Z39.88-
2004&ctx_enc=info:ofi/enc:UTF-
8&rfr_id=info:sid/ProQ:sciencejournals&rft_val_fmt=
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
18

info:ofi/fmt:kev:mtx:journal.
Rising, J.P. et al., 2007. Healthy Young Adults:
Description and Use of an Innovative Health Insurance
Program. Journal of Adolescent Health, 41(4),
pp.350–356.
Sepehri, A., Sarma, S. & Serieux, J., 2009. Who is giving
up the free lunch? The insured patients’ decision to
access health insurance benefits and its determinants:
Evidence from a low-income country. Health Policy,
92(2–3), pp.250–258.
Ybarra, M., Ha, Y. & Chang, J., 2017. Health insurance
coverage and routine health care use among children
by family immigration status. Children and Youth
Services Review, 79(2016), pp.97–106. Available at:
http://dx.doi.org/10.1016/j.childyouth.2017.05.027.
The Changing Nature of Campus Health Insurance: Testing Portability Issues of National Health Insurance
19
