
Wireless Sensor Network based System for the Prevention of Hospital
Acquired Infections
Iuliana Bocicor
1
, Maria Dasc
˘
alu
4
, Agnieszka Gaczowska
2
, Sorin Hostiuc
3
, Alin Moldoveanu
4
,
Antonio Molina
5
, Arthur-Jozsef Molnar
1
, Ionut
,
Negoi
3
and Vlad Racovit
,
˘
a
1
1
SC Info World SRL, Bucharest, Romania
2
NZOZ Eskulap, Skierniewice, Poland
3
Carol Davila University of Medicine and Pharmacy, Bucharest
4
Polytechnic University of Bucharest, Romania
5
Innovatec Sensing&Communication, Alcoi, Spain
Keywords:
Hospital Acquired Infection, Nosocomial Infection, Clinical Workflow Monitoring, Cyber-physical System,
Wireless Sensor Network.
Abstract:
Hospital acquired infections are a serious threat to the health and well-being of patients and medical staff
within clinical units. Many of these infections arise as a consequence of medical personnel that come into
contact with contaminated persons, surfaces or equipment and then with patients, without following proper
hygiene procedures. In this paper we present our ongoing efforts in the development of a wireless sensor
network based cyber-physical system which aims to prevent hospital infections by increasing compliance to
established hygiene guidelines. The solution, currently developed under European Union funding integrates a
network of sensors for monitoring clinical workflows and ambient conditions, a workflow engine that executes
encoded workflow instances and monitoring software that provides real-time information in case of infection
risk detection. As a motivating example, we employ the workflow in the general practitioner’s office in or-
der to comprehensively present types of sensors and their positioning in the monitored location. Using the
information collected by deployed sensors, the system is capable of immediately detecting infection risks and
taking action to prevent the spread of infections.
1 INTRODUCTION
Hospital acquired infections (HAI) are a serious threat
to the health and well-being of both patients and
medical staff within clinical units. Various micro-
organisms, especially multi drug resistant bacteria
may lead to significant hospital related morbidity and
mortality. These infections have high related costs
and represent a direct occupational hazard for clini-
cal personnel. Hospital infections are a worldwide
problem, regardless of geographical, political, so-
cial or economic factors (World Health Organization,
2002), (World Health Organization, 2010). Further-
more, technological development and sophistication
of medical care does not automatically result in lowe-
red infection rates (Tikhomirov, 1987), (Coello et al.,
1993), (World Health Organization, 2010), (European
Centre for Disease Prevention and Control, 2015).
According to the findings of the World Health Orga-
nization, average HAI prevalence in Europe is 7.1%,
in the United States it is 4.5%. In low- and middle-
income countries infection rates vary between 5.7%
and 19.1% (World Health Organization, 2011). In
intensive care units located in high-income countries
the proportion of infected patients can be as high as
51%, while in low- and middle-income countries it
can reach 88.9% (World Health Organization, 2011).
Unfortunately, many of these infections lead to pa-
tient deaths. Annually, infections are accountable for
37 000 deaths in Europe and 99 000 deaths in the USA
(World Health Organization, 2011). While measures
and precautions are being taken to successfully reduce
these rates (Centers for Disease Control and Preven-
tion, 2016), there is still much room for improvement.
Many hospital infections arise as a consequence
of medical personnel that come into contact with con-
taminated surfaces or equipment, relatives coming
in contact with patients or as auto infections, which
158
Bocicor, I., Dasc
ˇ
alu, M., Gaczowska, A., Hostiuc, S., Moldoveanu, A., Molina, A., Molnar, A-J., Negoi, I. and Racovi¸t
ˇ
a, V.
Wireless Sensor Network based System for the Prevention of Hospital Acquired Infections.
DOI: 10.5220/0006357801580167
In Proceedings of the 12th International Conference on Evaluation of Novel Approaches to Software Engineering (ENASE 2017), pages 158-167
ISBN: 978-989-758-250-9
Copyright © 2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

occur by touching sensitive body parts, such as the
face, with the hands. The most common target sites
for hospital infection are the urinary and respiratory
tracts, which are often involved in minimally-invasive
procedures such as catheter-related procedures.
While the methodology for prevention exists, it
is often ignored due to lack of time, unavailability
of appropriate equipment or because of inadequate
staff training. Research shows that the most impor-
tant transmission route are staff members who come
into contact with patients or contaminated equipment
without following proper hygiene procedures (Ham-
mer, 2013). More particularly, most often transmis-
sion is made by touching a patient or contaminated
equipment and then touching another patient without
proper hand hygiene (Pittet, 2001). Recent guideli-
nes, such as ”Five moments for hand-hygiene” (World
Health Organization, 2015) provide concise and well-
structured information on efficient disinfection means
to significantly reduce the risk of infection.
In this paper we present our progress in the de-
velopment of a cyber-physical system based on a wi-
reless sensor network (WSN) that is targeted towards
HAI prevention. Our solution employs a sensor net-
work that will monitor clinical workflows and am-
bient conditions, integrated with configurable soft-
ware to detect deviation from established hygiene
practices. The sensor network collects information
in real-time about substance and material presence.
Availability of antimicrobial agents and sterile glo-
ves, as well as environmental conditions that affect
pathogen spread, such as oxygen level, airflow, and
temperature will be monitored. To complete the pic-
ture, the system will facilitate monitoring of complex
processes such as management of indwelling urinary
catheters, postoperative care, intubation and mecha-
nical ventilation. Given the complexity of these pro-
cesses, as well as the diversity of hospital regulati-
ons, these processes will be described using software
workflows. Each clinical process will be modelled
using one workflow instance executed by a software
workflow engine. When the sequence of transitions
inferred by the system from sensor data presents de-
viations from the expected flow, the system will alert
responsible personnel.
The current stage of development represents a
system proof of concept, including multifunctional
smart sensors for monitoring the use of soap, antimi-
crobial gel and water sink together with a first clini-
cal workflow that describes the required hygiene pro-
cedures in the general practitioner’s office. This pa-
per details the smart devices employed, the hardware-
software integration as well as the software compo-
nents that ensure the cyber-physical system achieves
its objective of lowering the number and severity of
hospital infections.
The present paper is structured as follows. The
following section presents some of the last decade’s
advancements, from an Information and Communica-
tion Technologies (ICT) perspective. This includes
several software-based or cyber-physical systems de-
veloped to increase compliance to guidelines and de-
crease infection rates. Section 2 offers a detailed des-
cription of the workflow in the general practitioner’s
office, as well as the main challenges faced when en-
coding this process using a software-based workflow
model. The wireless sensor network custom designed
for the system is depicted in Section 3, where all as-
pects related to its hardware and software components
are covered. Section 4 focuses on presenting the soft-
ware workflow engine that interprets events and mo-
nitors execution of configured workflows. Moreover,
the means by which the hardware part of the system is
integrated with the software workflow engine, as well
as the communication infrastructure employed are il-
lustrated in this section. Finally, we outline our con-
clusions and further work in the last section.
1.1 Existing Solutions
Because HAI have significant detrimental effects, in
recent decades health care facilities have started to
implement prevention programmes for patients and
medical staff. There are even practical guides devi-
sed by specialised agencies (World Health Organi-
zation, 2012), which can be used as starting points
for the development of good practice plans concer-
ning workplace and patient safety. Following the cur-
rent technological developments in all medical areas,
technology is also present for monitoring and preven-
tion of HAI. This is illustrated by the development
of various software-based or cyber-physical solutions
that monitor and ensure compliance. In this section,
we present some of the most popular such systems.
1.1.1 Monitoring Hand Hygiene
Inadequate hand hygiene is responsible for a large
proportion of infections (Pittet, 2001). There are se-
veral automated solutions to reduce infections cau-
sed by improper hand hygiene, most of which use
continuous surveillance and immediate notification
in case non-compliance is detected (Shhedi et al.,
2015). IntelligentM (Ryan, 2013) and Hyginex (Hy-
ginex, 2015) are two solutions that monitor employ-
ees using bracelet-like devices equipped with Radio
Frequency Identification (RFID) technology and mo-
tion sensors. Whenever a hygiene event has been
omitted, the device alerts them either using vibration
Wireless Sensor Network based System for the Prevention of Hospital Acquired Infections
159

(IntelligentM) or coloured lights (Hyginex). Biovi-
gil technology (BIOVIGIL Healthcare Systems, Inc.,
2015) and MedSense (General Sensing, 2014) are de-
signed having the same purpose, only in these cases
bracelets are replaced with badges worn by healthcare
workers. The Biovigil device uses chemical sensors
to detect whether hand hygiene is observed according
to established standards. The system can be configu-
red to remind clinicians to disinfect their hands be-
fore entering patient wards, or before administering
procedures such as intravenous drips or catheter in-
sertion. Furthermore, these systems record hygiene
events, centralise them and enable analysis, visua-
lisation and report generation. SwipeSense (Swipe
Sense, 2015) employs small, alcohol-based devices
and wearable gel dispensers. This allows medical per-
sonnel to perform hand hygiene without interrupting
their activities to go to a sink or disinfectant dispen-
ser (Simonette, 2013). In opposition to the systems
mentioned so far, which use sensors placed at patient
ward entrances, UltraClenz’s Patient Safeguard Sy-
stem (UltraClenz, 2016) is ”bed-centric” and prompts
workers to sanitize before and after every patient con-
tact. The DebMed system (DebMed - The Hand Hy-
giene Compliance and Skin Care Experts, 2016) does
not use RFID technology, nor any devices for the me-
dical personnel, but instead estimates the number of
hand hygiene opportunities per patient-day and com-
pares this number with the actual hand hygiene events
that were performed, which are determined using a
network of wireless-enabled dispensers.
1.1.2 Disinfection Robots
Dangerous pathogens can remain in the air or on dif-
ferent types of surfaces in a hospital room for long
periods after the infection source was removed. To
tackle this issue, which cannot always be resolved
using traditional cleaning and disinfection procedu-
res, several types of disinfection robots have been de-
veloped. Generally, they are able to perform thorough
disinfection using ultraviolet (UV) light or chemi-
cal substances. The Xenex ”Germ-Zapping Robot”
(Xenex, 2015) can disinfect a room using pulses of
high-intensity, high-energy ultraviolet light. The ro-
bot must be taken inside the room to be disinfected
and in most cases, the deactivation of pathogens ta-
kes place in five minutes. Tru-D Smart UVC (Tru-D
Smart UVC, 2016) scans the room to be disinfected
using eight sensors and computes the optimal short
wavelength ultraviolet light dose required for disin-
fection according to the size, geometry, surface re-
flectivity as well as the amount and location of equip-
ment found in the room. The robot performs disin-
fection of the entire room, from top to bottom in one
cycle and from one location, ensuring that the ultravi-
olet light reaches even shadowed areas. The Bioquell
Q-10 robots (Bioquell, 2016) emit a powerful anti-
bacterial bleaching agent, called hydrogen peroxide
to kill multi-drug resistant organisms. As hydrogen
peroxide is toxic to humans, after disinfection the Q-
10 uses another solution to ensure that it is safe for
humans to enter the room.
1.1.3 Managing Infection and Outbreaks
A different procedure in the fight against infection
is implemented by the Protocol Watch decision sup-
port system for prevention and management of sepsis
(Philips, 2015). Protocol Watch regularly checks cer-
tain medical parameters of patients, to reduce the time
elapsed between the moment sepsis is first detected
and beginning of treatment. If the system detects that
certain conditions indicative of sepsis are met, it alerts
medical staff and indicates which tests, observations
and interventions must be performed, according to es-
tablished prevention and treatment protocols.
Another goal pursued by clinicians when dealing
with hospital infection is the identification of control
policies and optimal treatment in infection outbreaks.
A comprehensive approach that uses electronic health
records to build healthcare worker contact networks is
described in (Curtis et al., 2013). Its main goal con-
cerns putting efficient vaccination policies into place
in case of infection outbreaks.
Among other relevant software systems developed
to enhance treatment policy in case of infection outb-
reak or epidemics are RL6:Infection (RL Solutions,
2015) and Accreditrack (Excelion Technology Inc.,
2013). RL6:Infection is a software solution developed
to assist hospitals in the processes of controlling and
monitoring infections and outbreaks, while Accre-
ditrack is designed to ensure compliance with hand
hygiene guidelines, verify infection management pro-
cesses as well as to provide procedural visibility and
transparency.
1.2 The HAI-OPS Platform
The proposed platform is developed within the Hos-
pital Acquired Infection and Outbreak Prevention Sy-
stem (HAI-OPS) research project (HAI-OPS, 2017).
Its main objective is to decrease overall mortality and
morbidity associated with hospital infection. It is
designed to handle both singular infection cases as
well as outbreaks, by targeting most common sour-
ces and transmission pathways. Operationally, the
platform will leverage advances in computing po-
wer and availability of custom-developed, afforda-
ble hardware that will be combined with a configura-
ENASE 2017 - 12th International Conference on Evaluation of Novel Approaches to Software Engineering
160

ble, workflow-based software system (Bocicor et al.,
2016).
Existing solutions, such as those detailed in the
section above (Ryan, 2013; Hyginex, 2015; BIOVI-
GIL Healthcare Systems, Inc., 2015; General Sen-
sing, 2014) can be successfully employed to monitor
a single process, such as hand hygiene, or equipment
and room disinfection (Xenex, 2015; Tru-D Smart
UVC, 2016; Bioquell, 2016). While these processes
are important for keeping patients and staff safe from
infection, there are many other processes that can lead
to hospital infection. Among the most prevalent, we
mention catheter management, mechanical ventila-
tion, invasive procedures and surgical site care (World
Health Organization, 2002; Coello et al., 1993). One
solution for monitoring multiple processes would be
to deploy several such systems in parallel. Howe-
ver, given that eHealth interoperability is currently
an open issue, this is not only cost-ineffective, but
technologically infeasible. We believe that monito-
ring several clinical and maintenance workflows can
be successfully addressed using a single system. Such
a system must be configurable so that it covers diffe-
rences between clinical unit location and layout, dif-
ferences in types and specifics of undertaken proce-
dures, as well as variation between hygiene guideli-
nes that must be observed by staff. The HAI-OPS
platform is designed to address these issues in both
hardware as well as software. First of all, using cu-
stomized, but affordable hardware allows sensors to
be deployed in key locations in cost effective manner.
Workflow engines allow researchers to create custom
BPMN-encoded (Object Management Group, 2015)
workflows that encode key events in monitored pro-
cesses. Furthermore, implementation of a user inter-
face for workflow management will allow epidemio-
logists to further customize the monitored workflows.
To the best of our knowledge, our proposed system is
the first of its kind to combine a sensor network and
software in a cyber-physical system of the proposed
versatility.
2 GENERAL PRACTITIONER’S
OFFICE WORKFLOW
The cyber-physical system depicted in this paper em-
ploys pre-defined workflows that describe the proces-
ses that the system will monitor. They allow the sy-
stem to take real-time action in case an infection risk
is detected. Our development approach is bottom-up,
and starts with modelling some of the less complex
workflows, which involve only medical staff and pa-
tients. The more complex workflows, that also in-
volve equipment, such as endoscopic or surgical pro-
cedures will be addressed at a later time. Thus, the
first workflow we approach for the system prototype,
which is also the subject of the present paper’s moti-
vating example, is the workflow of the general practi-
tioner’s office.
2.1 Process Description
The general practitioner (GP) is a medical doctor
whose practice is not limited to a certain speciality
and who provides treatment and preventive care to pa-
tients. As opposed to physicians working with inpa-
tients admitted to hospital for certain procedures, the
general practitioner works with outpatients, who re-
quire consultation or treatments which do not necessi-
tate hospital admission. All information regarding the
GP office, as well as the consultation workflow des-
cribed were supplied by NZOZ ESKULAP (NZOZ
Eskulap, 2016), an outpatient clinic from Poland that
is targeted for the first pilot deployment of our system.
Figure 3 illustrates the general practitioner’s office la-
yout from the Polish clinic. The office contains a desk
for the physician, a consultation bed and, most impor-
tantly for our use case, an area with several elements
for ensuring hygienic conditions: a sink, a waste bin
and an area dedicated to disinfectants and disinfectant
dispensers. The same figure also depicts the planned
layout of the wireless sensor network used for mo-
nitoring the workflow. These are described in more
detail in Section 3.
In order to ensure compliance with the infection-
prevention guidelines in the Polish clinic, the first step
was identifying the hygiene practices to which the ge-
neral practitioner must adhere to before, during and
after patient consultation. The conventional workflow
for an outpatient consultation, including all required
actions for ensuring conformity with hygiene stan-
dards are depicted within the following sequence of
steps:
1. Patient enters the office.
2. The GP starts a conversation with the patient, in
order to learn about their medical history, current
treatment and reason for the visit. Generally, the
physician uses pen and paper or a hospital infor-
mation system to record information to the patient
file.
3. The GP prepares to examine the patient. The
preparation process is crucial with regards to in-
fection prevention. According to current regulati-
ons within the target clinic, the doctor must sani-
tize their hands according to 10 steps for effective
hygiene. These are:
Wireless Sensor Network based System for the Prevention of Hospital Acquired Infections
161

(a) Wet hands thoroughly.
(b) Soap up, using the liquid soap dispenser. The
used tap must be elbow or wrist operated. The
physician must rub palms.
(c) Rub palms with finger interlaced.
(d) Massage between fingers, right palm over the
left hand and then vice-versa.
(e) Scrub with fingers locked, including fingertips.
(f) Rub rotationally, with thumbs locked.
(g) Rinse thoroughly.
(h) Dry hands using a paper towel that must be pla-
ced in proximity to the hand washing facility.
(i) Work towel between fingers.
(j) Dry around and under the nails.
4. The GP throws the wet towel to a special waste
bin.
5. The GP starts patient examination.
6. After the examination, the GP uses an alcohol-
based sanitizer for hand disinfection.
7. The GP goes back to the desk and records exami-
nation results using pen and paper or the hospital
information system.
8. Patient leaves the office.
The procedure described above concerns a regular
examination. However, for special cases such as ex-
aminations involving the head, eyes, ears, nose and
throat (HEENT), or when the patient presents with
skin infection, the doctor must also employ nitrile or
latex disposable gloves. Gloves should also be worn
whenever there might be contact with blood, body
fluids, mucous membranes or non-intact skin. Glo-
ves must be put on immediately before the task to be
performed, and removed and discarded as soon as the
procedure is completed.
The BPMN workflow for the consultation process
is illustrated in Figure 1. Sections 3 and 4 describe
how the wireless sensor network is used for monito-
ring and how the workflow engine monitors the exe-
cution of hygiene-relevant events. In the case a devi-
ation from the expected steps of the workflow is de-
tected, a real-time alert is generated and sent to the
GP using a mobile device in their possession.
2.2 Workflow Description
The general practitioner workflow is shown using
BPMN specification in Figure 1. For the description
of the workflow we use both Figures 1 and 3, as the
events specified in the workflow are detected by har-
dware devices placed in different locations in the of-
fice. As soon as the patient enters the office, this is
detected by the infrared array sensor element placed
near the entrance (Goga et al., 2016). The system re-
cords and interprets the received data and a workflow
instance is started. As illustrated in Figure 1, the first
steps required from the GP is to start the water sink,
use the soap dispenser and then stop the sink. The sy-
stem interprets this as hand hygiene being performed.
These events are detected by the sensor elements in
the sink and those in the disinfectant dispenser area,
which are all connected to smart nodes placed near the
physician’s desk. This enables transmitting the data to
the software server via wireless network. While cur-
rent regulations described in the previous section re-
quire a specific sequence of actions to be undertaken
for hand hygiene to be considered effective, our sy-
stem only checks that the sink and disinfectants were
operated. The main reason for this is that the system
is envisaged as an additional aid for medical person-
nel that ensures their safety from possible infection.
The system is designed on the principle that medical
personnel are responsible and aware of the detailed
actions they must undertake to ensure their own, as
well as their patients’ safety.
The intermediate step of the workflow concerning
patient examination starts when the system has de-
tected that hand hygiene compliance is achieved. Ot-
herwise, the system generates and stores a hygiene
alert, which is immediately sent to the general practi-
tioner. The two activities are exclusive: if an alert is
generated, the workflow instance is stopped and the
recorded hygiene breach is recorded. In case of an
alert, the GP must perform hand hygiene, after which
the system initiates a new workflow instance. In case
initial hand hygiene and patient consultation are car-
ried out according to the workflow, the GP must dis-
infect their hands using antimicrobial gel after the last
contact with the patient. This event is again recorded
by the system using the same sensors situated in the
disinfectant dispenser area and the smart nodes near
the physician’s desk. The workflow is thus comple-
ted. All the information related to patient entry/exit,
hygiene compliance and alerts is saved to persistent
storage for further reuse, including statistics and ad-
vanced analyses for finding the source or propagation
of an outbreak.
2.3 Current Challenges
Although seemingly straightforward, the process des-
cribed above can become quite complicated, mainly
due to various types of constraints and interferences
that may occur. Below we present the main challenges
to the system, with regard to the GP office workflow
and the methods we use to approach and overcome
ENASE 2017 - 12th International Conference on Evaluation of Novel Approaches to Software Engineering
162
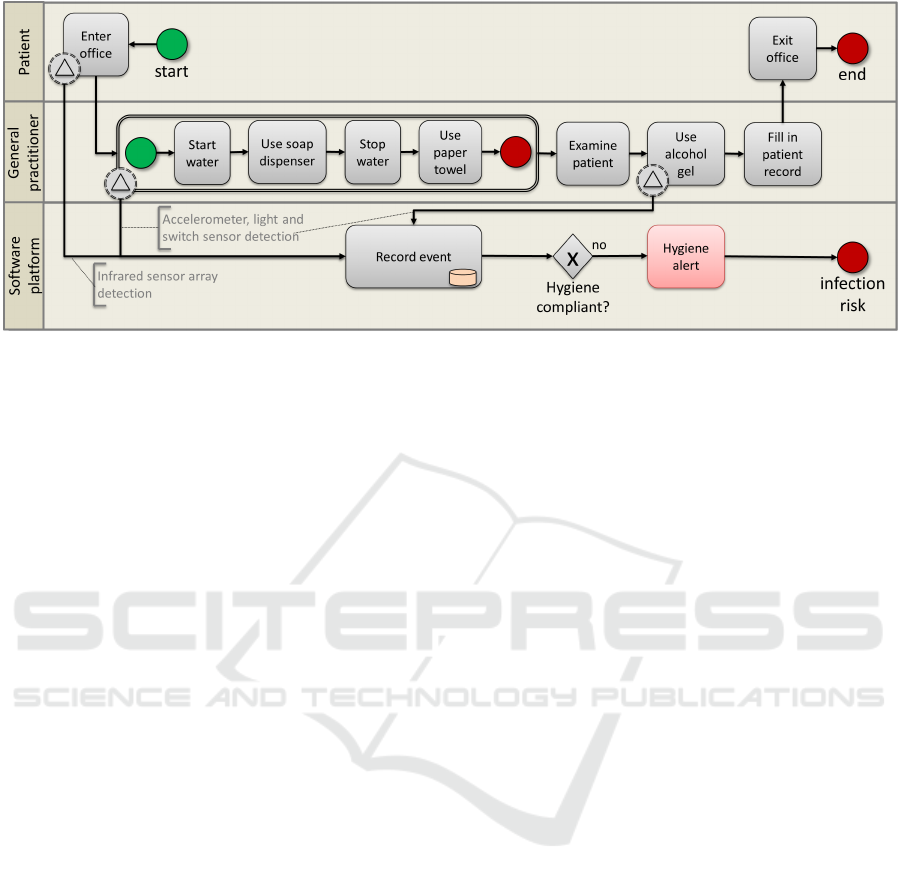
Figure 1: General Practitioner Workflow.
some of them. Others are still open to discussion and
solutions are currently being investigated.
First and foremost, one key aspect to consider is
achieving minimal overhead on the clinical process
and minimal intrusive interaction, from the user ex-
perience point of view. It is important that the system
does not impose any constraints and does not restrict
the doctor’s movements. In many clinical units, in-
cluding the one targeted for pilot deployment, hospi-
tal regulations specify that personnel are not allowed
to wear jewellery, watches or bracelets, as these can
hamper their freedom of movement and spread bacte-
ria, especially if these wearables are difficult to dis-
infect. To tackle this, the proposed system does not
require the use of additional wearables. Monitoring is
done using the deployed wireless sensor network no-
des, which are placed in key locations within the GP
office, as described in Section 3. In addition, medi-
cal personnel already employ chest-mounted badges
to which radio-frequency tags can be easily added.
The placement of the wireless sensors is an essen-
tial challenge in itself, as locations must be chosen in
a manner that allows a complete and preferably op-
timal surveillance of monitored workflows. The ar-
rangement of sensors in the office must be adjusted
to the process, but should also be sufficiently gene-
ral in order to allow monitoring several workflows: in
this case, both the regular consultation workflow as
well as HEENT examinations. Thus, in addition to
placing wireless sensors at the office entrance, sink,
soap or disinfectant dispenser, in order to ensure com-
plete process monitoring, a device is also placed on
the waste bin, to detect when gloves are thrown away.
Device positioning in the GP office is discussed in
more detail within Section 3.
One of the remaining challenges for cyber-
physical systems such as the proposed one concerns
short-term human interactions that are difficult to de-
tect. In the case of the GP workflow, how should the
system detect and react to a person entering the GP of-
fice during an examination? In this case, the hygiene
event performed by the GP before patient examination
is considered cancelled, as the third person can conta-
minate the physician or patient with micro-organisms.
Medical staff wear badges that can be used to identify
them using the sensors deployed near the entrance;
however, if the person is not part of the medical staff,
they cannot be identified. A potential solution is that
once the system detects someone entering the office,
regardless of whether the person is medical staff or
not, the system triggers the execution of a new work-
flow, including the necessary hygiene events. In case
this is not performed, the GP is alerted to take imme-
diate corrective action.
3 THE SENSOR NETWORK
A wireless sensor network consists of a group of elec-
tronic devices in which every node controls one or
more sensors that measure physical phenomena such
as light, heat or proper acceleration. All collected me-
asurements are sent using a wireless network protocol
to another device featuring more powerful processing
capabilities. Depending on their functionality, nodes
are classified into dummy and smart nodes. As the
name suggests, dummy nodes consist of small devi-
ces that have to effectuate just one simple task: de-
tect a generated event and pass the information to a
smart node. A dummy node is particularly charac-
terized by its small size (35x35mm) and low power
consumption. Some sensors, like RFID readers, do
not generate events by themselves and require a pre-
processing stage, which can be exclusively carried out
by a powered device. Smart nodes must be able to
Wireless Sensor Network based System for the Prevention of Hospital Acquired Infections
163
collect key actions detected from dummy nodes and
generate more complex events comprising informa-
tion regarding four relative clauses: who is the person
involved, what was the action generated, when it hap-
pened and where it happened.
3.1 Sensor Types
Required sensors were selected to enable monitoring
the clinical workflow detailed in Section 2. From the
mentioned steps, sensors in dummy nodes should be
applied mainly to detect key actions, such as the uti-
lization of hygienic elements that can be found in the
GPs office: water sink, soap dispenser, waste bin, al-
cohol sanitizer and glove dispenser. The main sensor
types required to ensure effective monitoring of the
general practitioner office workflow are as follows:
1. Accelerometer. These sensors measure changes
in gravitational acceleration on two or three axes,
allowing to detect changes in motion and orien-
tation. Accelerometers may be attached to water
taps, which regulate water flow on the vertical axis
and temperature on the horizontal. They may also
be applied to sanitizer or glove dispensers, where
detected motion implies that they have been used
by a practitioner or checked by cleaning staff.
2. Proximity and Light Sensor. Proximity sensors
emit infrared radiation and look for changes in the
return signal. This type of sensors are already ap-
plied in some water sinks and soap containers, but
to the best of our knowledge none of them have
communication capabilities to report actions.
3. Switch Detection. A switch is just an electronic
component that interrupts the flow of electric cur-
rent from one conductor to another. It may be
operated by a moving object, which makes it a
great choice for applications such as detecting the
use of waste bins or opening of a door. This is
the least energy consuming element from the list,
because it does not have to expend energy doing
continuous measurement.
Dummy nodes generate action events indicating,
for instance, that someone used the soap dispenser or
the waste bin, but it is the smart node who has to fill
in information and identify who generated the action.
To achieve that goal, it is necessary to process and
combine the output from the following two sensors:
1. Infrared Array Sensor. It is a thermopyle type
infrared sensor which detects the amount of infra-
red rays. It has a built-in lens with a 60 degree
viewing angle. The sensor offers output for ther-
mal presence, direction and temperature values.
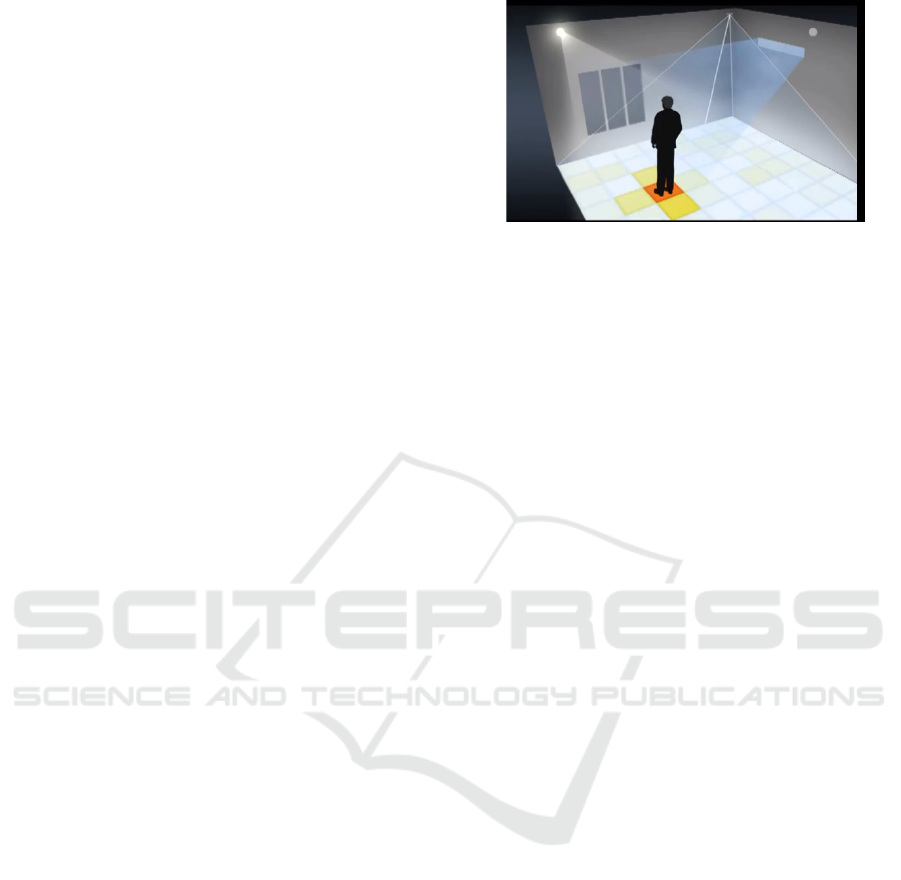
Figure 2: Infrared array sensor detecting people inside the
GP office.
2. RFID Reader. Radio-frequency identification
works using tag-based identification. Tags are
small devices similar to stickers that may be car-
ried by people, animals or objects. They can also
be easily attached to wearables such as badges or
mobile equipment. The frequency range and ap-
plied antenna depend on the application and indi-
rectly on the distance between readers and tags. In
some clinics, medical and cleaning staff are used
to carry a badge with an identification card based
on this principle.
3.2 Device Positioning
Device positioning and calibration are crucial for the
proper functioning of the system. In the case of
dummy sensors, the proximity sensor may detect false
positives if the distance range is not correctly adjusted
or if the sensor is incorrectly placed. When applied
to water sinks or gel dispensers, the proximity sensor
must be tied to the tap pointing downwards. The sy-
stem registers when someone places their hand under
the tap and when they stop using it. Figure 3 illustra-
tes the positioning of both smart and dummy nodes
within the general practitioner’s office.
In addition to the proximity sensor, the RFID an-
tenna and passive infrared array sensor must also
be placed according to their detection range. RFID
readers provide received signal strength indication
(RSSI) levels for detected tags, a measure which is
proportional to the distance between them. Patch an-
tennas consist of a planar dielectric substrate material
with a radiating patch on one side and a ground plane
on the other. The radiating side must point to the GP’s
office where elements to be identified are located and
the ground plane must point to the corridor, ceiling or
to an adjacent room. Radio frequency power output
must be configured to meet European Union regulati-
ons and to avoid false positive detections as much as
possible.
Passive infrared array sensors complement the
ENASE 2017 - 12th International Conference on Evaluation of Novel Approaches to Software Engineering
164
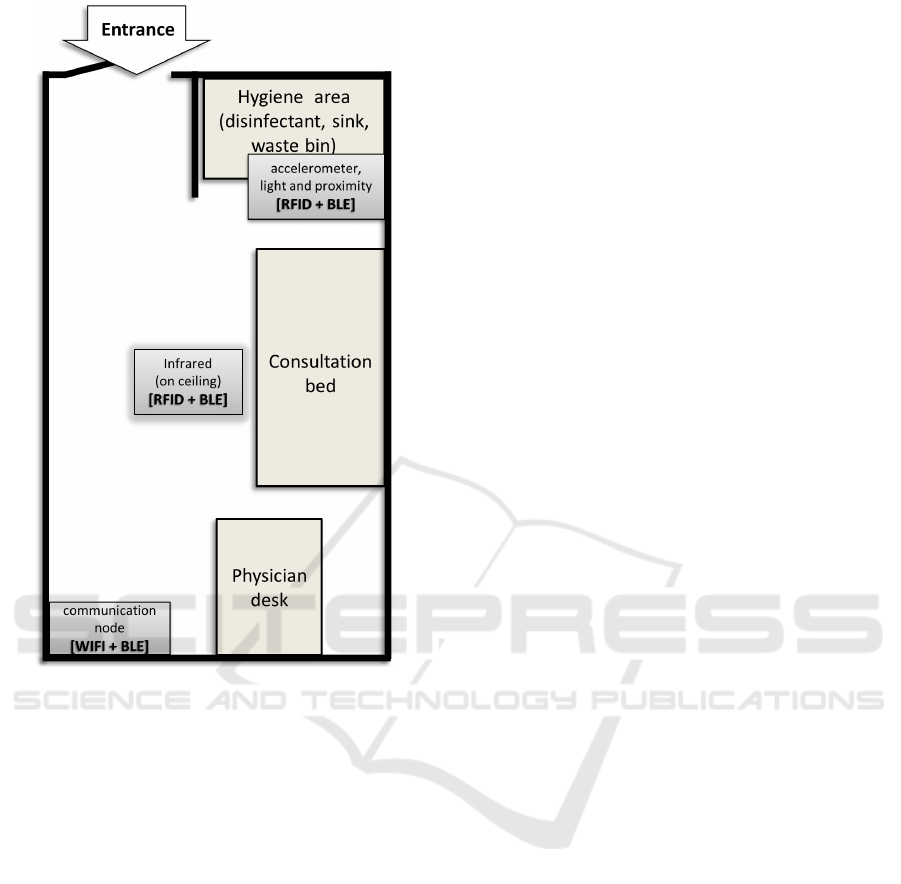
Figure 3: Layout of the general practitioner office augmen-
ted with wireless sensor network.
information from RFID readers. If this information is
combined properly, the dummy node is able to locate
people inside the room, identify people wearing an
RFID card (typically clinical staff) and detect people
who are not wearing tags (typically patients). The
passive infrared sensor must be placed on the ceiling,
pointing downwards and centred in the room, as seen
in Figure 2. If the sensor’s angle of view is not enough
and doesn’t fit the whole room, scalability is achieved
using several sensors.
3.3 Communication Protocols
As already stated, the main features of dummy no-
des are their small size and low power consumption.
Both features are very closely correlated, because in
most cases product size is determined by the battery.
In this case, the power consumption in dummy no-
des is so low, that they can be powered using coin
batteries. The reduced power consumption is due to
the integration of a Bluetooth Low Energy (BLE) mo-
dule (Bluetooth SIG, Inc., 2017). Compared to previ-
ous Bluetooth standards, BLE is intended to provide
considerably reduced power consumption and lower
cost, while maintaining a communication range of up
to 150 meters with connected devices.
Smart nodes have more complex processing, com-
munication and thus, higher power requirements than
dummy nodes. They are continuously listening for
input BLE connections and when data is received, the
result is forwarded to a database server for persistent
storage and subsequent analyses. Connection with
this server is carried out using existent network infra-
structure, regardless of whether it is wired or wireless.
Every smart device is identified within the network
using a unique IP address and has a fixed location in-
side the building.
4 HARDWARE-SOFTWARE
INTEGRATION
The software side of the system implements the
client-server paradigm and employs a software ser-
ver to which an arbitrary number of heterogeneous
clients can have simultaneous connection. The ser-
ver contains components that receive sensor data from
the network, a persistence layer that manages sen-
sor readings as well as a workflow engine that execu-
tes workflow instances in real-time, generating alerts
when sensor readings indicate deviations from ex-
pected workflow transitions. The main software com-
ponents of the system are as follows:
1. Connected Device Controller. The connected
devices, or smart nodes, constitute the principal
hardware component of the platform. They are re-
sponsible for monitoring the clinical environment
using sensors and sending sensor readings to the
software server. By themselves, they cannot de-
cide whether an infection risk is present. Each
connected device includes a software controller,
a generic software component that runs indepen-
dently of the software server. Its objectives are to
ensure the correct functioning of smart nodes and
to send sensor readings to the software server.
2. Data Acquisition. This is the software compo-
nent that will be responsible with receiving sensor
readings. Received data is stored within the per-
sistence layer, from which it is read and used by
other components. This includes advanced ana-
lyses components yet to be developed which do
not make the object of the present paper. The ser-
ver adopts a REST architecture (Fielding, 2000)
to receive sensor data acquired as presented in
Section 3. The data interchange format employed
Wireless Sensor Network based System for the Prevention of Hospital Acquired Infections
165

is JavaScript Object Notation. Information con-
tained in files received from sensors includes the
event’s timestamp, a Uniform Resource Locator
that identifies which node generated the infor-
mation as well as sensor reading values. For
instance, a sensor monitoring temperature will
transmit a temperature value in degrees Celsius.
A sensor monitoring the presence of an individual
will transmit a boolean value, according to whet-
her presence was detected. An RFID reader will
transmit the RFID tag identifier and the received
signal strength indicator value.
3. Workflow Engine Adapter. This software com-
ponent is a fac¸ade to the workflow engine imple-
mentation used by the system. Its main purpose
is to abstract the particularities of the workflow
engine. This allows the system to operate with
any major off the shelf workflow engine imple-
mentation. This component provides the required
features that allow for the creation, update and de-
letion of clinical workflows monitored by the sy-
stem. The workflow engine interprets events, such
as inputs from deployed sensors (e.g. hand wa-
shing detected), and acts upon them according to
a predefined process. The actions are configurable
and can vary from saving a new entry into a data-
base, sending an e-mail or emitting a real-time no-
tification via an external application or short mes-
sage service. Its input is represented by process
descriptions. Processes are composed of activi-
ties connected with transitions. Processes repre-
sent an execution flow. Each execution of a pro-
cess definition is called a process instance. As an
example, hand disinfection in the general practiti-
oner’s office can be represented as a process. Each
time a patient enters the office a new process in-
stance is started, managed by the business process
management system. Some activities, such as re-
cording an event, or sending an alert are automa-
tic. Others involve waiting for an external event
to occur, such as a sensing device reporting the
physician has disinfected hands. The workflow
engine keeps track of the state of process executi-
ons and manages creation and progress of process
executions.
4. Data Store. This component of the software ser-
ver acts as the system’s persistence layer for all
system data. In addition to user, alert, connected
devices and workflow data, it includes a com-
plete record of data received from connected sen-
sors. This is required in order to facilitate advan-
ced analyses for outbreak prevention, identifica-
tion and monitoring. The data store will be imple-
mented using an SQL database.
5 CONCLUSIONS
This paper details the ongoing effort in the develop-
ment of a cyber-physical system intended for preven-
ting hospital infections. The HAI-OPS platform will
integrate a wireless sensor network and a software
server that uses a workflow execution engine to mo-
nitor key steps within various clinical processes that
were identified as responsible for a large proportion
of hospital infection. When key steps to ensure pro-
cess hygiene are not taken, the system will generate
real-time alerts. The present paper focuses on descri-
bing and modelling an initial clinical process used as
motivating example: outpatient consultations within
the general practitioner’s office. This process is the
one selected for implementation during the system’s
first pilot deployment within a Polish outpatient clinic
(NZOZ Eskulap, 2016). Although we directed our at-
tention specifically towards the motivating workflow,
the system is designed to allow for deployment of di-
verse sensor network configurations, as well as facili-
tate creation and execution of many different clinical
workflows.
Upcoming system development will build on exis-
ting achievements. First of all, the system will be used
to model more complex clinical workflows, including
endoscopic and minor surgery procedures, which will
be implemented in the pilot site location. Second
of all, as part of the project a graphical component
will be developed to allow management of monitored
workflows. In addition, we aim to leverage availa-
ble sensor readings by implementing advanced repor-
ting and evaluation capabilities. These are expected to
help clinical epidemiologists in pinpointing infection
and outbreak sources using visualizations such as risk
maps and healthcare worker contact networks (Hla-
dish et al., 2012).
ACKNOWLEDGEMENT
This work was undertaken as part of the HAI-OPS
project funded by the European Union, under the Eu-
rostars programme
1
.
REFERENCES
Bioquell (2016). Bioquell q-10.
http://www.bioquell.com/en-uk/products/life-science-
products/archive-hc-products/bioquell-q10/.
BIOVIGIL Healthcare Systems, Inc. (2015). Biovigil and
our team. http://www.biovigilsystems.com/about/.
1
https://www.eurostars-eureka.eu/project/id/9831
ENASE 2017 - 12th International Conference on Evaluation of Novel Approaches to Software Engineering
166

Bluetooth SIG, Inc. (2017). Bluetooth low energy.
https://www.bluetooth.com/what-is-bluetooth-
technology/how-it-works/low-energy.
Bocicor, M. I., Molnar, A.-J., and Taslitchi, C. (2016).
Preventing hospital acquired infections through a
workflow-based cyber-physical system. In Procee-
dings of the 11th International Conference on Evalu-
ation of Novel Software Approaches to Software Engi-
neering, pages 63–68.
Centers for Disease Control and Preven-
tion (2016). HAI data and statistics.
https://www.cdc.gov/hai/surveillance/.
Coello, R., Glenister, H., Fereres, J., Bartlett, C., Leigh, D.,
Sedgwick, J., and Cooke, E. (1993). The cost of in-
fection in surgical patients: a case-control study. Jour-
nal of Hospital Infections, 25:239–250.
Curtis, D., Hlady, C., Kanade, G., Pemmaraju, S., Pol-
green, P., and Segre, A. (2013). Healthcare wor-
ker contact networks and the prevention of hospital-
acquired infections. Plos One. DOI: 10.1371/jour-
nal.pone.0079906.
DebMed - The Hand Hygiene Compliance and Skin Care
Experts (2016). A different approach to hand hygiene
compliance. http://debmed.com/products/electronic-
hand-hygiene-compliance-monitoring/a-different-
approach/.
European Centre for Disease Prevention and Control
(2015). Annual epidemiological report. antimicrobial
resistance and healthcare-associated infections. 2014.
http://ecdc.europa.eu/en/publications/Publications/
antimicrobial-resistance-annual-epidemiological-
report.pdf.
Excelion Technology Inc. (2013). Accreditrack.
http://www.exceliontech.com/accreditrack.html.
Fielding, R. T. (2000). Architectural styles and the design of
network-based software architectures. Doctoral dis-
sertation, University of California.
General Sensing (2014). Medsense clear.
hand hygiene compliance monitoring.
http://www.generalsensing.com/medsenseclear/.
Goga, N., Vasilateanu, A., Mihailescu, M. N., Guta, L.,
Molnar, A.-J., Bocicor, I., Bolea, L., and Stoica, D.
(2016). Evaluating indoor localization using wifi for
patient tracking. In International Symposium on Fun-
damentals of Electrical Engineering (ISFEE).
HAI-OPS (2017). home page. http://haiops.eu.
Hammer, S. (2013). Hand washing:
Reducing nosocomial infections.
http://iwsp.human.cornell.edu/files/2013/09/Hand-
Washing-Reducing-Nosocomial-Infections-
2j1mlfb.pdf.
Hladish, T., Melamud, E., Barrera, L. A., Galvani, A., and
Meyers, L. A. (2012). Epifire: An open source c++
library and application for contact network epidemio-
logy. BMC Bioinformatics, 13(1):76.
Hyginex (2015). Introducing hyginex generation 3.
http://www.hyginex.com/.
NZOZ Eskulap (2016). NZOZ eskulap.
www.eskulapskierniewice.pl/.
Object Management Group (2015). Business process model
and notation. http://www.bpmn.org/.
Philips (2015). Protocolwatch - SSC Sepsis.
http://www.healthcare.philips.com/main/products/
patient monitoring/products/protocol watch/.
Pittet, D. (2001). Improving adherence to hand hygiene
practice: a multidisciplinary approach. Emerging In-
fectious Diseases, 7:234–240.
RL Solutions (2015). The rl6 suite / infection surveillance.
http://www.rlsolutions.com/rl-products/infection-
surveillance.
Ryan, J. (2013). Medtech profiles: Intelligentm
- a simple yet powerful app to dramati-
cally reduce hospital-acquired infections.
https://medtechboston.medstro.com/profiles-
intelligentm/.
Shhedi, Z. A., Moldoveanu, A., Moldoveanu, F., and Tas-
litchi, C. (2015). Real-time hand hygiene monitoring
system for hai prevention. In The 5th IEEE Interna-
tional Conference on E-Health and Bioengineering -
EHB 2015.
Simonette, M. (2013). Tech soluti-
ons to hospital acquired infections.
http://www.healthbizdecoded.com/2013/06/tech-
solutions-to-hospital-acquired-infections/.
Swipe Sense (2015). Hand hygiene. redefined.
https://www.swipesense.com/.
Tikhomirov, E. (1987). Who programme for the control of
hospital infections. Chemioterapia, 6:148–151.
Tru-D Smart UVC (2016). About tru-d. http://tru-
d.com/why-uvc-disinfection/.
UltraClenz (2016). Patient safeguard system.
http://www.ultraclenz.com/patient-safeguard-
system/.
World Health Organization (2002). Prevention of
hospital-acquired infections - a practical guide.
http://www.who.int/csr/resources/publications/
whocdscsreph200212.pdf.
World Health Organization (2010). The burden
of health care-associated infection worldwide.
http://www.who.int/gpsc/country
work/
summary 20100430 en.pdf.
World Health Organization (2011). Health
care-associated infections - fact sheet.
http://www.who.int/gpsc/country work/
gpsc ccisc fact sheet en.pdf.
World Health Organization (2012). Prevention of
hospital-acquired infections - a practical guide.
http://apps.who.int/medicinedocs/documents/
s16355e/s16355e.pdf.
World Health Organization (2015). Clean care is
safer care - five moments for hand hygiene.
http://www.who.int/gpsc/tools/Five moments/en/.
Xenex (2015). Xenex germ-zapping robots.
http://www.xenex.com/.
Wireless Sensor Network based System for the Prevention of Hospital Acquired Infections
167
