
Business Models & Business Cases for Point-Of-Care Testing
A. J. Staring, L. O. Meertens and N. Sikkel
University of Twente, PO Box 217, Enschede, The Netherlands
a.j.satring@alumnus.utwente.nl, {l.o.meertens, k.sikkel}@utwente.nl
Keywords: Business Modelling, Modelling Method, Business Model, Business Case, Healthcare.
Abstract: Point-Of-Care Testing (POCT) enables clinical tests at or near the patient, with test results that are available
instantly or in a very short time frame, to assist caregivers with immediate diagnosis and/or clinical
intervention. The goal of POCT is to provide accurate, reliable, fast, and cost-effective information about
patient condition. POCT can be part of the solution to the rising healthcare and welfare costs without any loss
of healthcare quality. In this research, business models are used to create business cases in order to assess the
viability of POCT. Two methods to create business models were designed by tailoring and extending them
from an existing method. It was found that the method used has impact on the resulting business case. POCT
was assessed to be viable in all business cases created for the specific case study used.
1 INTRODUCTION:
POINT-OF-CARE-TESTING
Healthcare and welfare costs are rising, in the
Netherlands, as well as other developed countries.
Solutions need to be found to keep these costs within
reasonable limits (Busse, 2001; Hagist and Kotlikoff,
2006), without loss of healthcare quality (Davis and
Erixon, 2008). Point-Of-Care Testing (POCT) can be
part of the solution. The goal of POCT is to provide
accurate, reliable, fast, and cost-effective information
about patient condition (St-Louis, 2000). Ehrmeyer
and Laessig (2007) define POCT as “patient
specimens assayed at or near the patient with the
assumption that test results will be available instantly
or in a very short time frame to assist caregivers with
immediate diagnosis and/or clinical intervention”.
Already several forms of POCT exist, such as
glucose testing and urine dipsticks (Altieri and
Camarca, 2001). These used to be laboratory tests
exclusively, but have evolved to focus solely on
measuring the most critical parameters of the
designed test. By focusing on only a few parameters,
the test becomes more specific, faster, and the devices
smaller (Dondelinger, 2009).
Although many advantages of POCT have been
proven, such as fast diagnosis (Middendorf, 2010),
error reduction (Drenck, 2001), and reducing the time
patients stay in hospitals (Kiwa Carity, 2014), it has
been pointed out that POCT may not be a cost-
beneficial development always (Lehmann, 2001).
2 RESEARCH GOAL AND
METHODOLOGY
This research aims to provide insight in the viability
of POCT as part of the solution to the rising
healthcare and welfare costs. We focus on a single
case study in Dutch health care. For this case study,
we create and evaluate several business cases.
Business cases are a generally accepted way of
assessing costs and benefits, as they provide “a
justification for a proposed project or undertaking on
the basis of its expected commercial benefit” (Oxford
University Press, n.d.). To avoid creating arbitrary
business cases from scratch, we apply the Business
Modelling Method (BMM) (Meertens et al., 2012)
and subsequently the Business Model to Business
Case method (BM2BC) (Meertens et al., 2013).
In the process, we aim to validate the BMM’s use
to create business models in a structured and
repeatable way. In addition, extension of the BMM
towards business cases may improve its value and
applicability.
The process is as follows. First, we develop
several derivatives of the BMM, so that we have
methods to create business models that are tailored
for healthcare and POCT specifically (section 3).
Then, we apply these methods to create business
models for our case study (section 4). Finally, we
create business cases based on the business models
and analyse them to assess their viability (section 5).
54
Staring A., Meertens L. and Sikkel N.
Business Models Business Cases for Point-Of-Care Testing.
DOI: 10.5220/0006222200540063
In Proceedings of the Sixth International Symposium on Business Modeling and Software Design (BMSD 2016), pages 54-63
ISBN: 978-989-758-190-8
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

3 TAILORING THE BUSINESS
MODELLING METHOD
The basic BMM consists of four steps to create a
single business model in a structured and repeatable
way (Meertens et al., 2012). As such, it aims to fill
the research gap “Design tools” as defined by Pateli
and Giaglis (2004) and Vermolen (2010).
The four basic steps are: 1. Identify roles,
2. Recognize relations, 3. Specify activities, and
4. Quantify model. The result of each step serves as
input for the next step. The resulting business model
is suitable for analysis of the current situation. It can
also form the basis for further predictions, such as
business cases, scenarios, and alternative innovations.
When using business modelling to evaluate new
or alternate business ideas, two additional steps
should be followed: 5. Design alternatives, and
6. Analyse alternatives. These steps are not strictly
part of the method to create business models. The first
four steps can even be reused when designing the
alternatives. In addition, several other steps could
follow, such as implementing the chosen business
model alternative. Section 3.2 provides details of each
step.
While for each of the steps example methods are
given, none of these is enforced. This allows tailoring
the BMM to the demands of the specific situation.
3.1 Extending the BMM
One extension step for the BMM is considered in this
research. It splits step 4 (quantify model) of the basic
BMM into two separate parts for costs and benefits.
This makes it more suitable for business case
analysis.
While step 4 of BMM aims to quantify the model,
previous work only focusses on the costs of the model
(Meertens et al., 2012). As a business that only spends
money will not last long, revenue needs to be
generated. Quantifying using only cost accounting
methods is not sufficient.
Pricing methods can be used if to model “To be”-
business models. To model the “As is”-business
model, numbers from accounting systems and
(annual) reports can be taken. To model the “To be”-
business model pricing methods need to be used to
determine the price.
Three approaches can be taken to set a price: cost-
based, competition-based, and customer-based (Peter
et al., 1991). Each of these approaches has its own
advantages and disadvantages, as well as
specializations.
3.2 Tailoring: Two Derivations of the
BMM
While the previous sections outline the global process
of the BMM, in this section we will provide two
derivatives of it. These derivatives, BMMa and
BMMb, are tailored by choosing appropriate methods
for each of the steps. As Van Dijk (2015) identified
roles and recognized relations for the same case
study, steps 1 and 2 follow the methods he used. Only
from step 3 onwards do the two derivatives differ
from each other.
3.2.1 Step 1: Identify Roles
The first step focusses on identifying the relevant
parties (i.e. roles) involved in a business model.
Originally, the BMM suggests stakeholder analysis
for this step.
In the preliminary research, Van Dijk (2015)
chose to use the three-stage stakeholder analysis
method presented by Pouloudi (1998). This method
was designed for healthcare settings, such as our case
study. For these reasons, we include this method in
step 1 for both derivatives.
3.2.2 Step 2: Recognise Relations
The second step aims to recognise and characterise
the relationships among the roles identified in the first
step. Step 2 prepares for step 3, and follows naturally
from the first step. The result can be as simple as a
role-relationship matrix (Meertens et al., 2012).
While a stakeholder analysis often follows a hub-and-
spoke pattern, the second step of the BMM forces to
specify and rethink all possible relations between the
roles. The relations consist of interaction between two
roles, with some form of value exchange. This is in
line with Gordijn and Akkermans (2001) who state
that all roles in a business model can capture value
from the business model.
From this perspective, the proposed technique for
this step, e3-value modelling, is a valid one. The e3-
value model models the economic-value exchanges
between actors (Andersson et al., 2009; Kartseva et
al., 2006). This economic-value exchange can be
tangible as well as intangible (Allee, 2008; Andersson
et al., 2009). Van Dijk (2015) used e3value to
visualise value exchanges with and without
MobiHealth for the case study of this research. For
these reasons, we include e3value in step 2 for both
derivatives.
Business Models & Business Cases for Point-Of-Care Testing
55

3.2.3 Step 3: Specify Activities
The third step specifies the activities needed for the
roles to maintain their relationships and value
exchanges. Every role-relationship, as recognized in
the previous step, consists of at least one interaction
between two roles, requiring activities by both roles.
The activities reveal what should happen for the
business to function properly.
Originally, the BMM proposes techniques from
business process management to create the intended
output. For tailoring, we follow this guideline and
limit the difference between BMMa and BMMb to
the choice of Business Process Modelling Language
(BPML).
For BMMa, we choose Business Process
Modelling and Notation (BPMN) (OMG, 2006).
BPMN models consist of diagrams for both business
users and developers. BPMN aims to simplify the
understanding of business activity flows and
processes. BPMN is chosen as it is the de facto
standard for business process modelling.
For BMMb, we choose Event-Driven Process
Chain (EPC) (Scheer and Schneider, 1992). EPC was
developed for modelling business processes with the
goal to be easily understood and used by business
people. EPC is chosen, as it is aims to be understood
by business people, similar to the business models
and cases for this case.
3.2.4 Step 4: Quantify Model
The fourth step turns the qualitative model into a
quantitative model by obtaining numbers on cost and
volume of the activities, which the previous step
specified. This step helps to see what is happening in
more detail, and allows for objective comparison
between business models (Meertens et al., 2012).
Numbers on cost and volume of activities are needed
to completely overview the costs captured by the
business model.
The origin of numbers depends on whether the
“As is”-business model or “future”-business model is
being modelled. To model the “As is”-business
model, numbers from accounting systems and
(annual) reports can be taken. To model the “To be”-
business model, cost accounting methods need to be
used to estimate the costs.
For an organisation to assign costs, several
systems are available, both traditional systems and
more refined systems, such as Activity-Based
Costing (ABC) (Drury, 2008). Two main types of
cost accounting methods exist: absorption costing,
and variable costing. Their calculations differ mainly
on the way they allocate overhead. Therefore, their
results mainly differ when sales and production do
not match (e.g. seasonal sales with production in the
rest of the year).
ABC in general is a type of absorption costing, but
is argued to have its flaws (Anderson and Kaplan,
2003). Time-driven Activity-Based Costing (TD-
ABC) is an improvement of basic ABC by requiring
estimates of only two parameters: unit cost of
supplying capacity, and time required to perform a
transaction or an activity.
For BMMa, we choose the modern TD-ABC
method, as its parameters best match the available
input for the case study.
For BMMb, we choose variable costing as
described by Drury (2008). Variable costing is
considered less complex, and therefore better matches
the choice for understandability by business people.
As healthcare in general has service-based
organizations, sales and production occur at the same
moment, and therefore, the results should be the same
as for absorption costing.
3.2.5 Extension Step: Pricing Method
This extension adds to the previous step by focusing
on quantifying the revenues instead of the costs. As
we want to design not only “As is” models, but also
“To be” models, a pricing method is needed to
determine the future revenue.
The most common used pricing method is the
cost-based pricing method called cost-plus pricing
(Drury, 2008; Gregson, 2012), also known as mark-
up pricing. A limitation of cost-plus pricing is that
demand is ignored. The price is set by adding a mark-
up to the cost, and this may bear no relationship to the
price-demand relationship. It assumes that prices
should depend solely on costs (Drury, 2008). An
other frequently used pricing method is value-based
pricing (Gregson, 2012). The difference between
value-based pricing and cost-plus pricing is “pricing
down from value versus pricing up from cost”. Value-
based pricing is a customer-based pricing method as
the added value for the customer is translated into a
price. Value-based pricing is setting a price that
accurately reflects customers’ perception of value and
proposes a process to do so (Bernstein and Macias,
2002).
For BMMa, we choose cost-plus pricing, as it is
most commonly used method.
For BMMb, we choose value-based pricing, as
this allows to confidently set the right price, as well
as making a realistic prediction of revenue and
profitability, which are two objectives of the process.
Sixth International Symposium on Business Modeling and Software Design
56

4 CASE STUDY: BUSINESS
MODELS FOR POCT BY
MOBIHEALTH
The eHealth technology provider MobiHealth is the
main actor for the case study of this research.
MobiHealth is a Dutch company that was founded in
2007. The company’s roots lie in the European
projects MobiHealth and HealthService24. In these
projects, a prototype for mobile telemonitoring was
designed, tested, and clinically validated in several
European countries.
As this case study focusses on POCT, we will first
describe the setting in which this takes place.
However, the main part of this section applies the
derivatives of the BMM to the case. The “As is”-
business models reflect the situation without
automated processing of POCT by MobiHealth. In
the “To be”-business models MobiHealth takes part
and performs offers different services. The “As is”
and “To be”-business models reflect the same
situations using two methods, BMMa and BMMb.
4.1 Case Study Setting: POCT at a
General Practitioner in the
Netherlands
When a sample needs to be taken for a test, this can
either be done at the general practice (by the assistant
or the general practitioner) or at the laboratory.
Whether or not the sample is taken at the laboratory
or at the general practice, it needs to be processed by
the laboratory. If the sample is taken at the general
practice, the sample needs to be transported by
courier to the laboratory. Depending on the location
of the general practice and the production volume (i.e.
number of samples taken), the courier will visit the
general practice at least once a day. When the sample
is transported to the laboratory, the laboratory
performs the necessary test(s) on it using specialised
equipment. The test results are printed; a so-called
printout. The printouts are entered by hand into the
laboratory information system (LIS) and double-
checked by a second pair of eyes. A third party
transports the test results entered into the LIS to the
system of the general practitioner (HIS; Huisarts
informatie systeem). When the test results are entered
into the HIS, the general practitioner is able to check
the test results of their patients.
Some general practitioners, not all, have POCT
equipment in their practice. This allows them to not
only take test samples, but also test it using the POCT
device. The result is shown on the display of the
device and allows the general practitioner to act upon
the result immediately. The test results displayed on
the POCT device need to be transcribed on a form or
can be printed from the device directly. These forms
and printouts are transported by the courier to the
laboratory to be entered into the LIS. Sometimes, the
data is send by email to the laboratory either by
scanning it in or the assistant typing the email. The
processing of test results can take up to a couple of
days. Performing tests on test samples can, depending
on the capacity of the equipment and volume, also
take a couple of days. Although the general
practitioner has the test results immediate available
using the POCT device, still the processing takes a
couple of days.
MobiHealth has developed a service to process
the test results of the POCT device automatically.
They do this by adding hardware to the POCT device
to read the test results and send it to the computer of
the general practitioner. The results are then send
directly into the LIS. Using the existing integration
between the LIS and HIS, the test results are entered
into the HIS. This eliminates the time needed for the
courier to take the results to the laboratory and the
time it takes to enter the data into the LIS.
The laboratory supplies reagents to the general
practitioner. These reagents can be used in the POCT
device, but also to take samples or perform other
medical operations. Only when a general practitioner
submits a test sample or printout (by either courier,
email, or using the service of MobiHealth) the
laboratory is able to claim a reimbursement at the
health insurer. The reimbursement is a fixed
negotiated amount per test (amount depends on the
type of test). Because of this, it is very important for
the laboratory that performed tests are submitted by
the general practitioner.
4.2 Business Model Foundation:
Identified Roles and Relations
Van Dijk (2015) did the first two steps of the BMM
for this case in previous work. Therefore, his work is
a solid foundation to build upon in the following
sections.
The first step of BMM, identifies roles taking part
in the business model. The roles identified by Van
Dijk (2015) is an extensive list. Not all roles can be
found in the e3value model, as several are grouped.
Groups of roles show a relationship more clearly than
the individual roles themselves. Also it simplifies the
situation and increase transparency and
understanding. The listed roles match the roles in the
extended e3value model (Staring, 2015). The roles
can be found in Table 1.
Business Models & Business Cases for Point-Of-Care Testing
57
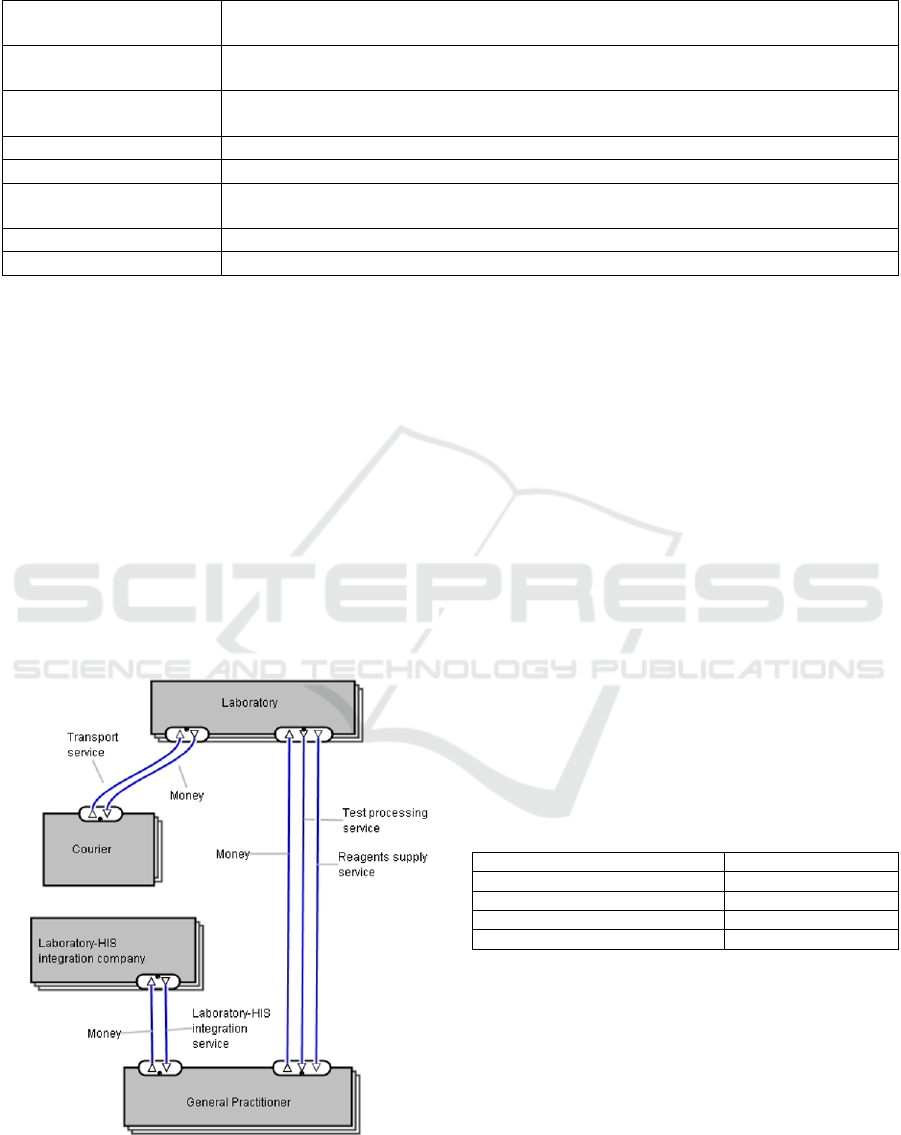
Table 1: Identified roles, including descriptions.
Courier
transports reagents from the laboratory to the general practice and test samples and print outs from the
general practice to the laboratory.
General practitioner works in a general practice; multiple general practitioners can work at a single general practice.
Health insurance company reimburse general practitioners and laboratories; issue health insurance policies to (potential) patients.
Patient person in need of medical attention..
MobiHealth provides integration service between POCT device and laboratory.
Laboratory-HIS integration
company
provides one-way integration service between laboratory information system (LIS) and the
information system of the general practitioner (HIS).
Laboratory responsible for performing tests on test samples.
POCT device supplier manufacturer/seller of POCT devices
The second step of BMM requires determining the
relationships among the roles. Figure 1 shows the
relationships in a simplified e3value model for a
situation with courier, “As is”-model. Several of the
roles and relationships that were in the extended
model have been left out, as they are not influenced
by the “To be”-business models.
4.3 As Is Models
4.3.1 Specify Activities
Four processes are identified from Figure 1. These are
the activities for the business model, as shown in
Table 2. For each of the process, business process
diagrams have been elaborated by Staring (2015).
Figure 1: Simplified "As Is" e3value model.
The reagents supply process relates the reagents
supply service and the test processing process. Both
services are provided by the laboratory and are used
by the general practitioner. The test processing
process uses two other processes: the transport
process (related to the transport service provided by
the courier) and the laboratory-HIS integration
process (related to the laboratory-HIS integration
service provided by the laboratory-HIS integration
company). The transport process is used by the
laboratory to pick up the test samples from the general
practitioner. The laboratory initializes the laboratory-
HIS integration process, but it is of value to the
general practitioner as this enables test results to flow
back into their systems (HIS).
4.3.2 Quantify Model
The specified activities in the previous step are
quantified to determine the costs. Table 2 shows the
results from this quantification step. As no overhead
costs are occurred within the identified activities, the
costs are the same for both methods.
Table 2: Costs for "As is"-business models.
Activity Costs in euros
Reagent supply 0 (reimbursed)
Test processing 2 / test
Transport N/A
Laboratory-HIS integration 15/month/practice
As described in the case study, the laboratory
sends the reagents to the GP for free. The laboratory
does make costs for the reagents, but these are
covered by the health insurer and fall outside the
scope of the business models. Similarly, a third party
handles the laboratory-HIS integration process. The
costs for this are the same for both the “As is” and
“To be” model. For these reasons, these two
processes are not handled anymore hereafter.
Sixth International Symposium on Business Modeling and Software Design
58
4.3.3 Pricing Method
As we are examining the As is-model, the different
pricing methods are not applicable. The actual set
prices can be used for the current situation. These are
directly the costs for the GP, as shown in Table 2.
4.4 To Be Models
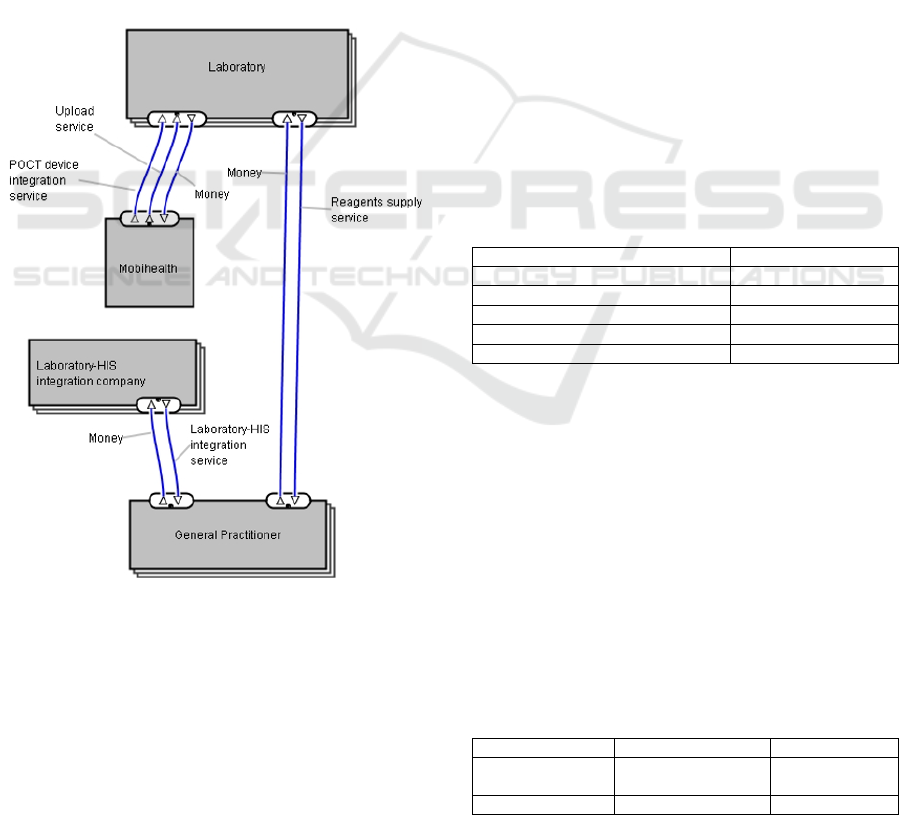
The “To be” scenario is an outcome of “step 5: Design
alternatives”. The alternative that we examine in this
case, introduces MobiHealth’s automated processing
of POCT test results, as a replacement of the courier
service. In the research for this paper, other more
radical alternatives were designed as well (Staring,
2015).
Figure 2 shows the relationships in a simplified
e3value model for a situation without courier, but
with MobiHealth, “To be.”
Figure 2: Simplified "To Be" e3value model.
4.4.1 Specify Activities
Similar to the “As is”-situation, four processes are
identified for the “To be”-models. The reagents
supply process still is the same, yet the other
processes differ. The POCT device integration
process is initialised by the general practitioner and
replaces the test processing service of the laboratory
as the POCT device takes care of testing. The POCT
device integration process relates to the POCT device
integration service in the e3value model. Tests
performed with the POCT devices are uploaded to the
laboratory by the test upload service of MobiHealth.
Using the existing laboratory-HIS integration, the
results are pulled from the LIS to the HIS by the
laboratory-HIS integration process.
While different BPMLs were used to model the
processes for BMMa (BPMN) and BMMb (EPC), the
resulting set of specified activities remain the same
(Staring, 2015). Therefore, these models are not
included in this paper.
4.4.2 Quantify Model
The costs for the activities specified in the previous
step are determined using the methods defined in
BMMa and BMMb. Table 3 shows the costs per
activity. The costs for the administration of the POCT
device integration is for the laboratory, while
integration and hardware are costs for MobiHealth.
While different cost accounting methods were
used to determine the costs for BMMa (TD-ABC) and
BMMb (variable costing), the results were the same.
This is logical, since no overhead is visible in the
process, and that is where the methods differ.
Table 3: Costs for "To be"-business models.
Activity Costs in euros
POCT device integration
Administration 6.25 / device
Integration 50 / device
Hardware 100 / device
Test upload process N/A
4.4.3 Pricing Method
Both the specified activities and the costs, determined
in the previous sections, are used to set the prices
using the methods defined in BMMa and BMMb.
Table shows the results of this second quantification
step.
For the POCT device integration activities,
MobiHealth sends the laboratory an invoice for the
integration of POCT devices with their systems, the
costs for the integration includes time and hardware.
From the costs in the previous step, this is estimated
to be 150 euros per POCT device.
Table 4: Pricing for "To be"-business models.
BMMa BMMb
POCT device
integration
100 euros profit
margin
0 euros (free)
Test upload process 0.30 euro per upload 1 euro per upload
Business Models & Business Cases for Point-Of-Care Testing
59
For BMMa, using the Cost-plus pricing method,
interviews revealed a 100 euros profit margin.
For BMMb, using the Value-based pricing
method, device integration allows MobiHealth to
ensure future revenue by hooking the GPs up to their
systems. Therefore, this process is mainly of value to
MobiHealth itself and they should not charge for this.
In the test upload process, MobiHealth sends the
laboratory an invoice per upload for their services.
While the costs for this service are difficult to
estimate or allocate, prices may still be set.
For BMMa, using the Cost-plus pricing method,
interviews revealed a fixed profit margin. A profit
margin of 30 eurocents is used per upload, as costs
are estimated to be close to zero.
For BMMb, using the Value-based pricing
method, test upload is a high value service for
MobiHealth and for the laboratory as this enables the
POCT test results to flow to the laboratory.
MobiHealth can therefore ask 1 euro per upload.
5 BUSINESS CASE
DEVELOPMENT AND
ANALYSIS
This section attempts to complete “step 6: Analyse
alternatives” of the BMM. We create business cases
based on the business models developed in the
previous section. To create the business cases, we use
the Business Model to Business Case method
(BM2BC). It is not an extension of BMM, but rather
a method that comes after BMM to further quantify
and compare business models (Meertens et al., 2013).
It is based on the work of Ward et al., (2008), but is
tailored to the development of business cases based
on business models. Similar to their work, it has eight
components that the business case needs to address.
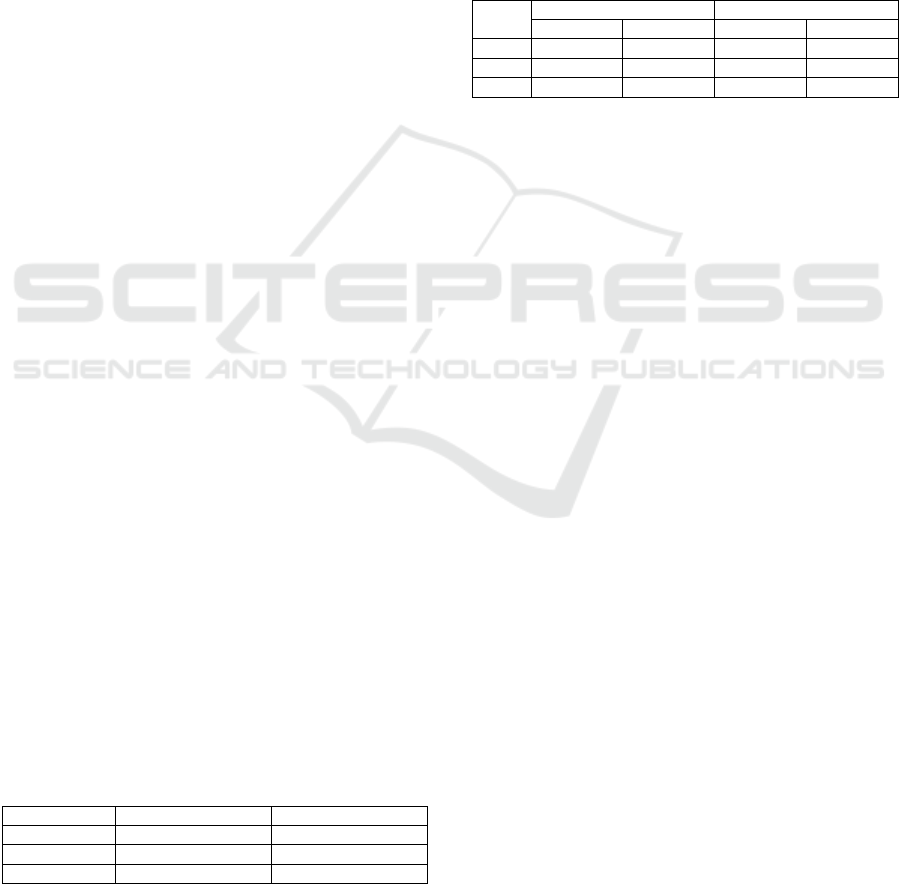
The created business cases are also the subject of
a sensitivity analyses. Since the number or POCT
tests performed and the number of POCT devices per
general practice (multiple general practitioners can
work in the same practice) determine the outcome of
the bottom line, different scenarios have been
constructed, as Table 5 shows. The scenarios are
based on the case study and interviews.
Table 5: Scenarios for sensitivity analysis.
POCT tests per year Devices per practice
Scenario 1
720 2
Scenario 2
960 3
Scenario 3
1200 3
Instead of only looking at the bottom line (shown
in Table 6), we used tools for three elements of the
business case: effects, risks, and costs. An effects
radar shows how the positive and negative effects are
distributed among the different business models
(Davis and Erixon, 2008). Risks per business model
are mapped on a matrix. This clearly shows how risk
is shaped overall, and which alternative involves most
risk (Bentley, 2010). A costs & benefits radar shows
the financial dynamics of each business model. All
these tools visually provide more insight in the
business cases and the differences per business
model.
Table 6: Cashflow per GP over a 5 year period (in euros).
BMMa BMMb
Lab MH Lab MH
1
5,707.50 1,180.00 3,587.00 3,300.00
2
7,591.25 1,540.00 4,781.25 4,350.00
3
9,479.00 1,900.00 5,975.00 5,300.00
As this paper focuses on the viability of POCT,
and the differences between two derivatives of the
BMM, only the details applicable for this are handled
here. The full details of the research are available in
other work (i.e. Staring, 2015).
The viability of POCT in the case study is good.
As Table 6 shows, both the laboratory (Lab), and
MobiHealth (MH) profit from the introduction of
POCT and MobiHealth’s automated processing
solution. In the business cases, the difference in
pricing method between BMMa and BMMb is
translated to the distribution of the benefits for the
laboratory and MobiHealth.
6 METHOD EVALUATION AND
LIMITATIONS
A pitfall in BMM is that the extensiveness of the first
two steps have a large impact on the result. When
roles or relationships are missed, this will result in not
specifying their activities and they will not be
quantified. In some cases, this has to do with the
scope at which BMM is applied. In other cases roles
and relationships are easily overlooked.
The third step in BMM proved to be very
important as it allowed to quantify the business model
by showing costs objects and points where revenue
was made. The difference between the used methods
was not significant in terms of results. Both methods
suit their purpose in specifying the activities needed
to maintain value exchanges between the roles in the
e3value model. However, there is a difference in
terms of accessibility of the method. BPMN was more
Sixth International Symposium on Business Modeling and Software Design
60

complete than EPC as the language was richer in
elements. EPC on the other hand was easier to
understand by non-technical people.
The difference in cost determination in the usage
of time-driven ABC and variable costing proved to be
non-existent. This is because the specified activities
showed no overhead. Overhead is treated differently
in the different methods. When the processes are
specified in more detail overhead could become
visible and the used methods would show a
difference. The level of detail at which the processes
are modelled might be too high to reveal any
overhead in the process. Although any level is better
than none and the current models do provide enough
insight to perform calculations upon. Still some
calculations were unable to be performed as this
would require specifics on an individual basis. The
calculations for the transport process were neglected
as it was highly depended on the distance between the
laboratory and general practice as well as the route
taken by the courier.
Time-driven ABC proved to be an effective
method to calculate the costs, as it was easy to obtain
the time it took to complete an activity (simple time
measurements). Quantifying the processes specified
in the previous step follows a natural path, but is also
limits the quantification of the business model. For
example, costs on infrastructure, human capital, or
other fixed costs may not be covered when following
BMM.
The extension with of a pricing method proved to
be useful, especially in the development of business
cases. The cost-plus pricing method was easy to
implement and ensured that costs were covered. The
value-based pricing method allowed for a new
perspective and focussed on environmental and
strategic factors to incorporate into the price. It is
important to note that the costs for one role can be the
price for another role. However, most costs need to be
converted using a pricing method, or are internal
costs.
After the business models were developed, the
Business Case method for Business Models
(BM2BC) was used to create business cases. BM2BC
listed the components required to build a business
case. However, no relationship or method existed to
derive effects and risks from the business models.
Therefore, we are unable to verify the completeness
of those components. For example, it is unknown
whether all effects and risks are covered in the
business cases. The most obvious ones have been
covered, but the identification of effects and risks is
subject to the cognitive capabilities of the researchers.
The researcher could (unconsciously) have decided a
certain effect or risk is outside the scope the business
model and business case. The cost/benefits
component was trivial given the two quantitative
steps in BMM. This again proved the value of the
added pricing method to BMM. Resource restrictions
are not considered a real problem in BM2BC, which
is a potential pitfall, as human capital or liquidity
requirements are not taken into account. They might
come up in the implementation planning stage of the
business case, but is should be under consideration
during the decision-making in the alternative
selection stage.
An assumption that was made, which clearly
shows the difference between theory and practice, is
that business models and business cases assume only
a single business model can be in existence at a time.
The “To be”-business models remove the need for a
courier, while in practice the courier still plays part in
transporting reagents. Not all test can be performed
by POCT devices either, requiring the patient to go
the laboratory or a courier to transport a test sample
(as per the “As is”-business models). In essence, there
will always be a combination of “As is” and “To be”-
business models.
Concluding, BMM and ultimately the derivatives
proved to be a useful method to build business
models. It provided a natural logical structured
method covering all components of a business model.
BM2BC was used to create the business cases
because of its focus on business models and provided,
similar to any other business case method, a list of
components which should be included in a business
case. The e3value model proved to be useful. It
extended the role-relationship matrix by showing the
value exchanges for each relationship. To maintain
the relationships, the activities were modelled. In
terms of communication to non-technical people EPC
was the best choice, but if the goal is to later develop
a business support tool BPMN should be used. As the
activities showed no overhead, the methods used to
calculate the costs showed no differences. In addition,
the cost determination is likely to be incomplete as
BMM only quantifies the specified activities. The
added pricing method made it possible to calculate
the benefits in the business case and was therefore
essential to be included in the business model. The
meta-business model visually summarised the
business model making it ideal to communicate to
others.
7 SUMMARY
In summary, the findings in this paper are threefold.
Firstly, in the case study, all of the business cases for
Business Models & Business Cases for Point-Of-Care Testing
61

POCT were assessed to be viable.
Secondly, the basis of the BMM allows for
reproducible creation of business models, as two
different derivatives came up with the same results,
although their calculation and representation is
different.
Thirdly, extending the BMM with an extra step,
namely selecting a pricing method, showed to be
useful for creating business cases.
ACKNOWLEDGEMENTS
The original research for this paper was part of the
IntoPOCT project sponsored by ZonMW (The
Netherlands Organization for Health Research and
Development), as part of the programme “Actieplan
eHealth”. Involved partners were MobiHealth
(eHealth provider), Reinier MDC (laboratory), and
University of Twente. At the time of writing, the
POCT service of the case study is provided by
Mobipoct B.V.
REFERENCES
Allee, V. (2008). Value network analysis and value
conversion of tangible and intangible assets. Journal of
Intellectual Capital, 9(1), 5–24.
Altieri, M. F., & Camarca, M. (2001). Point of care testing.
Clinical Pediatric Emergency Medicine, 2(4), 275–279.
Anderson, S. R., & Kaplan, R. S. (2003). Time-driven
activity-based costing. Harvard Business Review,
82(11).
Andersson, B., Johannesson, P., & Bergholtz, M. (2009).
Purpose driven value model design. In Proc. CAiSE
workshop BUSITAL (Vol. 9). Citeseer.
Bentley, C. (2010). Prince2: a practical handbook.
Routledge.
Bernstein, J., & Macias, D. (2002). Engineering new-
product success: The new-product pricing process at
Emerson. Industrial Marketing Management, 31(1),
51–64.
Busse, R. (2001). Expenditure on health care in the EU:
making projections for the future based on the past. The
European Journal of Health Economics (HEPAC),
2(4), 158–161.
Davis, L., & Erixon, F. (2008). The health of nations:
Conceptualizing approaches to trade in health Care.
ECIPE Policy Briefs, 4, 1–12.
Dondelinger, R. M. (2009). Point-of-Care Testing.
Biomedical Instrumentation & Technology, 43(3), 214–
218.
Drenck, N.-E. (2001). Point of care testing in Critical Care
Medicine: the clinician’s view. Clinica Chimica Acta,
307(1–2), 3–7.
Drury, C. (2008). Management and cost accounting. Cen-
gage Learning.
Ehrmeyer, S. S., & Laessig, R. H. (2007). Point-of-care
testing, medical error, and patient safety: a 2007
assessment. Clinical Chemical Laboratory Medicine,
45(6), 766–773.
Gordijn, J., & Akkermans, H. (2001). Designing and
evaluating e-business models. IEEE Intelligent
Systems, 16(4), 11–17.
Gregson, A. (2012). Pricing strategies for small business.
Self-Counsel Press.
Hagist, C., & Kotlikoff, L. J. (2006). Health care spending:
What the future will look like.
Kartseva, V., Gordijn, J., & Tan, Y.-H. (2006). Toward a
modeling tool for designing control mechanisms for
network organizations. International Journal of
Electronic Commerce, 10(2), 58–84.
Kiwa Carity. (2014). Het pad naar duurzame
hartfalenzorg: Een praktijkonderzoek naar
optimalisatie van het zorgpad chronisch hartfalen met
de inzet van telemonitoring (p. 54). Kiwa Carity.
Lehmann, C. (2001). Management of point-of-care testing
in home health care. Clinical Leadership &
Management Review : the Journal of CLMA, 16(1), 27–
31.
Meertens, L. O., Iacob, M.-E., & Nieuwenhuis, L. (Bart) J.
M. (2012). A Method for Business Model
Development. In B. Shishkov (Ed.), Business Modeling
and Software Design (pp. 113–129). Springer Berlin
Heidelberg.
Meertens, L. O., Starreveld, E., Iacob, M.-E., &
Nieuwenhuis, B. (2013). Creating a Business Case from
a Business Model. In B. Shishkov (Ed.), Business
Modeling and Software Design (pp. 46–63). Springer
International Publishing.
Middendorf, I. (2010). Point-of-care testing impacts
outcomes.
OMG. (2006). BPMN 1.0: OMG Final Adopted
Specification (standard No. dtc/06-02-01). Object
Management Group.
Oxford University Press. (n.d.). “business case”. In Oxford
Dictionaries.
Pateli, A. G., & Giaglis, G. M. (2004). A research
framework for analysing eBusiness models. European
Journal of Information Systems, 13(4), 302–314.
Peter, J. P., Donnelly, J. H., & Tarpey, L. X. (1991). A
preface to marketing management. Irwin Homewood,
IL.
Pouloudi, A. (1998). Stakeholder analysis for
interorganisational information systems in healthcare.
London School of Economics and Political Science,
London.
Scheer, A. W., & Schneider, K. (1992). ARIS (Architecture
of integrated Information Systems). Springer.
Staring, A. J. (2015). Business models & business cases for
point-of-care testing. MSc. Thesis, University of
Twente.
St-Louis, P. (2000). Status of point-of-care testing:
promise, realities, and possibilities. Clinical
Biochemistry, 33(6), 427–440.
Van Dijk, F. (2015). Barriers of Market Entry with POCT:
Sixth International Symposium on Business Modeling and Software Design
62

A Case Study. In Proceedings of the TSConIT,
University of Twente, Enschede, Netherlands.
Vermolen, R. (2010). Reflecting on IS Business Model
Research: Current Gaps and Future Directions. In
Proceedings of the 13th Twente Student Conference on
IT, University of Twente, Enschede, Netherlands.
Ward, J., Daniel, E. & Peppard, J., (2008). Building better
business cases for IT investments. MIS quarterly
executive, 7(1), pp.1–15.
Business Models & Business Cases for Point-Of-Care Testing
63
