
Characterisation of Clinical Practice Guideline Changes
Yamiko Joseph Msosa, C. Maria Keet and Melissa Densmore
Department of Computer Science, The University of Cape Town, Cape Town, South Africa
Keywords:
Clinical Practice Guidelines, Computer-Interpretable Guidelines, Clinical Decision Support, Low Resource.
Abstract:
Sub-Saharan Africa is facing a double crisis of high disease burden and shortage of healthcare resources.
To cope with this challenge, many countries have adopted the practice of task-shifting with clinical practice
guidelines (CPGs) as a key component. It is not unusual for CPGs to be revised or proved wrong, spurring
frequent updates of state-mandated CPGs. This negatively affects maintainability of healthcare applications
using those CPGs. Therefore, it is essential that the types of CPG changes are understood in order to develop
clinical decision support systems that are maintainable through adequate support for CPGs. We take a bottom-
up approach to analyse successive sets of CPGs so as to elucidate and characterise types of CPG changes over
time. The identified 10 type of changes in decisions, actions, and recommendations are exhaustive and affect
fine-grained structural components of a CPG. We also determined their occurrences using Malawi’s HIV CPGs
of 2008, 2011, and 2014 as case study. The results showed that the number of changes, as well as the type of
changes that occur in successive versions, varies widely.
1 INTRODUCTION
Low and middle income countries in regions such as
the sub-Saharan Africa are facing severe disease bur-
dens (Hotez and Kamath, 2009). Due to HIV/AIDS,
out-migration, and inadequate investment, low and
middle income countries are also facing a crisis in
human health resources (Chen et al., 2004), which is
crippling already fragile health systems in these re-
gions (Willis-Shattuck et al., 2008).
To nevertheless increase the efficiency of the de-
livery of healthcare services, the practice of task-
shifting has been adopted as a policy in low and mid-
dle income countries (Fulton et al., 2011). Clinical
practice guidelines (CPGs) allow task-shifted health
workers to effectively manage the most prevalent
manifestations of disease and are thus essential for na-
tional treatment programs in low and middle income
countries (Lewis et al., 2011).
CPGs are constantly changing due to the fact that
the science and technology behind clinical practice
is improving. These evolving scientific and clini-
cal practice insights in conjunction with properties
of information systems require advanced features in
computer-interpretable guidelines (CIGs) to be sup-
ported (Zamborlini et al., 2014). Yet, also main-
taining healthcare information systems require re-
sources, and frequent changing CPGs even more, as
came afore as problematic in a contextual inquiry with
stakeholders (Msosa et al., 2015).
In order to realise practical maintenance of com-
puterised CPGs especially to assist task-shifters, it is
necessary to know what changes when a CPG is up-
dated and how often, so that an easily maintainable
system can be developed. This study sets out to gain
insight into the types of CPG changes that, in turn,
can inform supporting changes in CIGs. We used a
bottom-up approach to elucidate the types of changes
using three successive CPG documents from Malawi.
This resulted in a specification of 10 types of changes,
which are exhaustive, and we obtained additional data
on their incidence in the CPG documents examined.
The rest of the paper starts by providing back-
ground and further contextual information (Sec-
tion 2). This is followed by the materials and meth-
ods of the investigation in Section 3. Section 4 is the
main part of the paper, containing the characterisation
of the types of CPG changes and their incidence. The
paper then discusses the findings (Section 5) and con-
cludes in Section 6.
2 BACKGROUND
This section describes some preliminaries on CPGs,
their computerisation and the health system context
248
Msosa, Y., Keet, C. and Densmore, M.
Characterisation of Clinical Practice Guideline Changes.
DOI: 10.5220/0005664302480255
In Proceedings of the 9th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2016) - Volume 5: HEALTHINF, pages 248-255
ISBN: 978-989-758-170-0
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

in Malawi, of which some of the problems are known
(e.g., (Msosa et al., 2015)).
2.1 Task-shifting and EHRs in Malawi
With a very low doctor to patient ratio, Malawi has
adopted task shifting to cope with the human resource
and disease burden crises (Zachariah et al., 2009).
Task-shifting refers to a process of delegation of tasks
to existing or new cadres of health workers with lower
qualifications or less training (Fulton et al., 2011).
The task-shifting process requires the development of
standardised protocols, including simplified clinical
practice guidelines (CPGs), simplified recording and
reporting systems and simplified monitoring and eval-
uation (Zachariah et al., 2009).
Several studies have reported the use of EHR sys-
tems to support health services in developing coun-
tries (Fraser et al., 2005). A number of services such
as antiretoviral therapy and diabetes are increasingly
being supported by EHR systems in Malawi (Douglas
et al., 2011). These systems have enabled automation
of some clinical functions that result in increased ef-
ficiency (Chawani, 2014).
2.2 Clinical Practice Guidelines
CPGs are “systematically developed statements to as-
sist practitioner and patient decisions about appro-
priate healthcare for specific clinical circumstances”
(Field et al., 1992). CPGs serve as reminders in situa-
tions where it is likely that a health worker can forget
steps, can find it difficult to follow steps or where er-
rors can be expensive (Coiera, 2003). A key element
in practising evidence-based medicine is considering
CPGs when they do exist at the point of healthcare
delivery (Bates et al., 2003).
2.3 Computer-interpretable Guidelines
CPG formalisation as CIGs in active computer-based
CDSSs has the potential to improve adherence to
CPGs. The CIG-based CDSSs are able to monitor
the actions and observations of care providers and
to recommend relevant guideline-based care-provider
actions at the point of care (de Clercq et al., 2008).
These CIG-based CDSSs are more likely to influence
clinician behaviour than narrative guidelines making
them essential for medical decision making (Peleg,
2013).
The key knowledge in a CPG is a set of one or
more guideline recommendations that can be broken
down into a series of situation-action statements, such
that, if the antecedent circumstances exist, then a set
of actions should be performed (Shiffman, 1997). All
guideline representation ontologies have a set of med-
ical decisions(conditions) and relevant recommended
actions, and a set of temporal rules that relate decision
evaluation results to associated actions (Zheng et al.,
2009).
2.4 Versioning of CIGs
Mechanisms of version management, in clinical
knowledge management, are required so that reason-
ing within CDSSs is related to correct guideline rec-
ommendations in different versions of a CPG, which
may be used by different people at a single point
in time (Peleg and Tu, 2006). CPG versioning has
not been adequately addressed in existing CIG for-
malisms (Kaiser and Miksch, 2009) despite version
management being mainly researched in the domain
of ontology evolution, vocabulary versioning and ver-
sioning of CIGs (Peleg and Tu, 2006). There are two
approaches to CIG versioning. The first, is the model-
centric approach, where a versioning tool is used to
support the creation of new or the modification of ex-
isting CPGs by tracking change operations of basic
structural components of a CIG model (Peleg and Tu,
2006). The second, is the document-centric approach,
where CPG changes are tracked in the original guide-
line document and systematically applied to its corre-
sponding formal or semi-formal CIG model (Kaiser
and Miksch, 2009).
3 MATERIALS AND METHODS
Copies of guideline documents were requested and
obtained from the Central Monitoring and Evaluation
Division (CMED) of the Malawi Ministry of Health.
The only guideline documents that were requested
were the ones that had been used in the past or were
still in use by healthcare workers in public health fa-
cilities.
After obtaining the guideline documents, a set of
guideline documents spanning at least three succes-
sive versions of CPGs was selected. Each guide-
line document, within the set, was examined to iden-
tify and extract candidate guideline recommenda-
tions. Thereafter, the extracted candidate guideline
recommendations were encoded into Guideline Ele-
ments Model (GEM) using GEM Cutter version 3.0.
GEM Cutter was selected because it has a structure
that is close to the structure of published CPG text
from guideline documents and uses a documentary
approach to CPG modelling (Douali et al., 2014).
Candidate guideline recommendations whose condi-
Characterisation of Clinical Practice Guideline Changes
249

tions and actions were clearly specified in the origi-
nating guideline document were encoded. Other clin-
ical facts and supporting information for CPGs were
not encoded.
After extracting and encoding the candidate
guideline recommendations, the first and the second
version of CPGs from the selected set were com-
pared. Thereafter, the comparison was repeated for
the second and third versions of the CPGs. For each
comparison cycle, an inductive learning approach was
used to extract and document guideline changes. In-
ductive learning allows people to discover patterns
in a seemingly chaotic collections of observations
(Michalski, 1983) making it a powerful strategy for
helping people deepen their understanding of content
(Silver et al., 2012). To begin with, a candidate guide-
line recommendation from the GEM encoded sample
was selected. Thereafter, the candidate recommenda-
tion was analysed to identify an equivalent guideline
recommendation in a successive version of the CPG.
In those instances where an equivalent guideline rec-
ommendation was found, the two versions of the can-
didate guideline recommendation were compared to
record the change and either specify a change or re-
fine an existing specification of a change. This pro-
cess was repeated until all candidate guideline recom-
mendations were analysed in each comparison cycle.
Finally, the recorded incidents of the changes be-
tween the first and the second version of the CPGs
were analysed. This analysis was repeated for the sec-
ond and the third version of the CPGs.
4 TYPES OF CHANGES AND
THEIR INCIDENCE
We first describe some basic results on encoding the
guidelines, and proceed to the main section on types
of CPG changes. The last subsection contains results
on the CPGs of Malawi.
4.1 Encoding Clinical Practice
Guideline Recommendations
Three successive versions of CPGs for the provision
of HIV services in Malawi were identified. The three
versions of the CPGs were published by the Malawi
Ministry of Health in 2008, 2011 and 2014.
All 114 pages of the 2008 version of the CPG text
for providing HIV services were examined for the
presence of candidate guideline recommendations.
Having examined the guideline text, 13 CPGs were
identified from which 105 candidate guideline recom-
mendations were extracted and encoded into GEM.
The 79 pages of the 2011 version of the CPG text
for providing HIV services were examined for the
presence of candidate guideline recommendations.
After examining the guideline text, 21 CPGs were
identified from which 85 candidate guideline recom-
mendations were extracted and encoded into GEM.
Finally, all the 95 pages of the 2014 version of the
CPG text for providing HIV services were examined
for the presence of candidate guideline recommenda-
tions. After examining the guideline text, 19 CPGs
were identified from which 98 candidate guideline
recommendations were extracted and encoded into
GEM.
4.2 Comparing CPG Versions
The 2008 version were compared with the 2011 ver-
sion of the GEM encoded CPGs to identify and spec-
ify the changes between the two. Thereafter, the pro-
cess was repeated with the 2011 and the 2014 version
of the GEM encoded CPGs. Ten different types of
CPG changes across three categories were identified.
The next section describes each type of change in
detail, using both an example of the actual changes—
indicated in bold in the examples—and a generalised
specification of the change. For this generalised spec-
ification, we use the following notation. Let the fol-
lowing denotations hold for CPG structural elements:
clinical practice guideline be CPG, guideline recom-
mendation be GR, condition be C, decision variable
be DV, value for a decision variable be DVV, recom-
mended action be RA, action verb be AV, and a verb
complement for an action verb be AVC. Then the state
before the change is indicated with a subscript time
“
t
” and the changed CPG one chronon later, “
t+1
”
(which for the examined CPGs is 3 years). Anything
unchanged is omitted from the notation to avoid clut-
ter.
4.3 CPG Change Categories
There are 10 change categories in total.
4.3.1 Addition of a Decision Variable to a
Guideline Condition
A decision variable can be added to the condition for
CPG execution if and only if the condition for the
guideline recommendation already has at least one de-
cision variable.
CPG
t
= {DV
1
, ..., DV
n
; ...}
CPG
t+1
= {DV
1
, ..., DV
n+1
; ...}
HEALTHINF 2016 - 9th International Conference on Health Informatics
250

For example, the guideline recommendation for pro-
viding ART in special situations for older children
from age three years and older that have active TB,
had an additional decision variable ‘weight’ intro-
duced in the 2014 version of the CPG as shown be-
low:
2011 version
IF Active TB = [present] AND
On ART = [No] AND
Age >= [3 years & < 15 years] AND
HIV test result = [Positive]
THEN
Prescribe AZT/3TC + EFV AND
Initiate ART within 14 days
2014 version
IF Active TB = [present] AND
On ART = [No] AND
HIV test result = [positive] AND
Age >= [3 years] AND
Weight < [35 kg]
THEN
Prescribe regimen 4P/4A AND
Initiate ART within 14 days
4.3.2 Change of a Decision Variable Value
A value of a decision variable can be changed in a
condition for CPG execution when a guideline recom-
mendation has a set of decision variables for a condi-
tion under which the guideline is to execute when the
condition is true.
CPG
t
= {C
1
{DV
1
,DVV
1
=a}, ..., C
n
{DV
n
,DVV
n
}; ...}
CPG
t+1
= C
1
{{DV
1
,DVV
1
=b}, ..., C
n
{DV
n
,DVV
n
}; ...}
where a 6= b
Equally, the guideline recommendation for determin-
ing ART eligibility in children aged 12 months and
above, had the value of the decision variable Age
changed as follows:
2011 version
IF Age = [12 to 24 months] AND
HIV test result = [positive]
THEN
Patient is eligible for ART
2014 version
IF Age = [12 to 60 months] AND
HIV test result = [positive]
THEN
Patient is eligible for ART
4.3.3 Removal of a Decision Variable from a
Guideline Condition
A decision variable can be removed from the condi-
tion for CPG execution if and only if the set of deci-
sion variables under which the guideline is to execute
when the condition is true, has at least two variables.
CPG
t
= {DV
1
...DV
n
; ...}
CPG
t+1
= {DV
1
...DV
n−1
; ...}
For instance, the guideline recommendation for sus-
pecting ART failure due to a new WHO clinical stage
condition, had the CD4 count decision variable re-
moved from the 2011 version of the CPG as follows:
2008 version
IF On ART = [Yes] AND
Duration of ART = [12 months or more] AND
Adhering to therapy = [Yes] AND
New WHO stage 4 = [Present] AND
CD4 count = [< 200 cells/mm
3
]
THEN
Patient has suspected ART drug failure
2011 version
IF On ART = [Yes] AND
Duration of ART = [12 months or more] AND
New WHO stage 3 or 4 = [Present] AND
THEN
Patient has suspected ART drug failure
4.3.4 Change of a Decision Variable
A decision variable can be replaced with another de-
cision variable within a condition for CPG execution
if and only if the condition under which the guideline
is to execute exists.
CPG
t
= {{DV
1
=a} ...DV
n
; ...}
CPG
t+1
= {{DV
1
=b} ...DV
n
; ...}
where a 6= b
For example, the guideline recommendation for de-
termining dosage of CPT in infants aged five months
or younger, had the Age decision variable changed to
weight in the inclusion criteria of the guideline rec-
ommendation for the 2011 version of the CPG as fol-
lows:
2008 version
IF Age = [6 weeks to 5 months] AND
Eligible for CPT = [Yes]
THEN
CPT dosage is 120mg once a day
2011 version
IF Weight = [< 6kg] AND
Eligible for CPT = [Yes]
THEN
CPT dosage is 120mg once a day
4.3.5 Addition of a Recommended Action
A recommended action can be added to a set of rec-
ommended actions within a guideline recommenda-
tion for CPG execution if and only if a guideline rec-
ommendation has got at least one recommended ac-
tion.
CPG
t
= {RA
1
...RA
n
; ...}
CPG
t+1
= {RA
1
...RA
n+1
; ...}
Characterisation of Clinical Practice Guideline Changes
251

Equally, the guideline recommendation for managing
a patient presenting with renal failure, had an addi-
tional recommended action added to the 2011 version
as follows:
2008 version
IF On ART = [No] AND
Renal failure = [Present] AND
HIV test result = [Positive]
THEN
Refer to district or central hospital AND
Do not exclude from treatment
2011 version
IF On ART = [No] AND
Renal failure = [Present] AND
Age category = [Adult] AND
HIV test result = [Positive]
THEN
Refer to district or central hospital AND
Prescribe Regimen 4 AND
Start ART within 7 days of diagnosis
4.3.6 Removal of a Recommended Action
A recommended action can be removed from an ac-
tion set for CPG execution if and only if the guideline
recommendation under which the CPG is to execute
has more than one recommended action.
CPG
t
= {RA
1
...RA
n
; ...}
CPG
t+1
= {RA
1
...RA
n−1
; ...}
For example, the guideline recommendation for man-
aging a patient presenting with renal failure, had the
recommended action for “automatically excluding pa-
tients from treatment” removed from the 2011 version
of the CPG as follows:
2008 version
IF On ART = [No] AND
Renal failure = [Present] AND
HIV test result = [Positive]
THEN
Refer to district or central hospital AND
Do not exclude from treatment
2011 version
IF On ART = [No] AND
Renal failure = [Present] AND
Age category = [Adult] AND
HIV test result = [Positive]
THEN
Refer to district or central hospital AND
Prescribe Regimen 4 to patient AND
Start ART within 7 days of diagnosis
4.3.7 Change of an Action Verb Complement
A verb complement of an action verb within a recom-
mended action for CPG execution, can be replaced
with another verb complement, if and only if at least
one recommended action in the guideline recommen-
dation under which the CPG is to execute exists.
CPG
t
= {RA
1
{AV
1
,AVC
1
=a}, ..., RA
n
{AV
n
,AVC
n
}; ...}
CPG
t+1
= {RA
1
{AV
1
,AVC
1
=b}, ..., RA
n
{AV
n
,AVC
n
}; ...}
where a 6= b
For instance, the guideline recommendation for man-
aging a patient presenting with renal failure in adults,
had the action verb complement for the ‘medication
prescription’ action changed in the 2014 version of
the CPG as follows:
2011 version
IF On ART = [No] AND
Renal failure = [Present] AND
HIV test result = [Positive] AND
Age = [>= 15 years]
THEN
Refer to district or central hospital AND
Prescribe Regimen 4 AND
Start ART within 7 days of diagnosis
2014 version
IF On ART = [No] AND
Renal failure = [Present] AND
HIV test result = [Positive]
THEN
Refer to district or central hospital AND
Prescribe Regimen 0 AND
Start ART within 7 days of diagnosis
4.3.8 Change of a Recommended Action
A recommended action for CPG execution can be
replaced with another recommended action if and
only if the guideline recommendation under which the
CPG is to execute has at least one recommended ac-
tion.
CPG
t
= {{RA
1
=a} ...RA
n
; ...}
CPG
t+1
= {{RA
1
=b} ...RA
n
; ...}
where a 6= b
For example, the guideline recommendation for man-
aging a patient presenting with acute hepatitis, had the
recommended action changed in the 2011 version of
the CPG as follows:
2008 version
IF On ART = [No] AND
Jaundice = [Present] AND
HIV test result = [Positive]
THEN
Do not prescribe Regimen 1
2011 version
IF On ART = [No] AND
Jaundice = [Present] AND
HIV test result = [Positive]
THEN
Refer to district/central hospital
HEALTHINF 2016 - 9th International Conference on Health Informatics
252

4.3.9 Addition of a Guideline Recommendation
A candidate guideline recommendation can be added
to a CPG if and only if the CPG has at least one exist-
ing candidate guideline recommendation.
CPG
t
= {GR
1
...GR
n
; ...}
CPG
t+1
= {GR
1
...GR
n+1
; ...}
For example, the candidate guideline recommenda-
tion for determining ART eligibility in infants pre-
senting with Cryptococcal meningitis was added to
the 2011 version of the CPG for determining ART el-
igibility.
4.3.10 Removal of a Guideline Recommendation
A candidate guideline recommendation can be re-
moved from a CPG if and only if the CPG has two
or more candidate guideline recommendations.
CPG
t
= {GR
1
...GR
n
; ...}
CPG
t+1
= {GR
1
...GR
n−1
; ...}
For instance, the candidate guideline recommenda-
tion for determining ART eligibility in infants asso-
ciated with recent HIV related maternal death was re-
moved from the 2011 version of the CPG for deter-
mining ART eligibility.
4.4 CPG Change Occurrences
Given the aforementioned type of changes, we anal-
ysed their incidence for the HIV CPGs of Malawi. A
summary of the frequencies of CPG changes is pre-
sented in Table 1.
Of the 30 candidate guideline recommendations
that were carried over from the 2008 to the 2011 ver-
sion of the CPGs, 27 were modified with 41 inci-
dents of guideline recommendation changes. Simi-
larly, 12 candidate guideline recommendations were
modified with 17 incidents of guideline recommenda-
tion changes from the 82 candidate guideline recom-
mendations that were carried over from the 2011 to
the 2014 version of the CPGs.
The frequencies of the changes that were identi-
fied between 2008 and 2011 version of the CPGs were
higher than those frequencies identified between the
2011 and the 2014 version of the CPGs. Three types
of changes, addition of a a recommended action, re-
moval of a recommended action and change of recom-
mended action, that occurred between the 2008 and
2011 version of the CPGs were not identified in the
changes that occurred between the 2011 and the 2014
version of the CPGs.
4.5 Analysis of Existing CIG Models
Having identified the characteristics of CPG changes,
we further analysed existing CIG models with respect
to the changes. CIG models were identified from ex-
isting literature accessible through Google Scholar,
PubMed and Open Clinical portal. GLIF, Arden
Syntax, SAGE, EON, PROforma and Asbru (Peleg,
2013) were analysed with regards to CPG changes.
Project websites, where accessible, were accessed to
analyse any tutorials and demonstrations that were
found. Any knowledge modelling tools that were
freely available were also downloaded and analysed.
We analysed Arden Syntax Checker for Windows,
AsbruView, Tallis, SAGE workbench and GLIF On-
tology in Prot
´
eg
´
e.
The results of the analysis are now presented. Ta-
ble 2 summarises CPG structural components that
are explicitly defined in existing CIG models and are
directly accessible within existing knowledge mod-
elling tools. An alignment of our terms and repre-
sentation primitives from the existing CIG models are
presented in table 3. From these results, we can see
that fine-grained CPG structural components that are
affected by the changes characterised in the previous
section, are not explicitly defined as modelling ele-
ments in existing CIG models. The fine-grained com-
ponents in existing CIG models are implicitly defined
as part of other structural components, specified ei-
ther as free text or using a formal expression language
such as GELLO (Sordo et al., 2003). As a result, all
the changes that were presented in the previous sec-
tion and affect fine-grained CPG structural compo-
nents cannot be represented using existing CIG mod-
els.
5 DISCUSSION
Evidence-based CPGs, available to task-shifted health
workers at the point-of-care through CDSSs, are a
necessity towards improving the delivery of care.
Due to the evolving nature of clinical practice, CIGs
in CDSSs need to be updated on a continuous ba-
sis to provide recommendations based on up-to-
date evidence-based CPGs. Characteristics of CPG
changes need to be specified precisely if CPG change
operations are to be modelled accurately to ensure ad-
equate clinical knowledge evolution support in CIGs.
The complexity of CIG models, a demanding and
time-consuming formalisation process, demands au-
tomating parts of the modelling process and mod-
elling adaptations to decrease the required implemen-
tation effort for CIGs (Kaiser and Miksch, 2009).
Fundamental change operations of a CIG are de-
fined from the addition, removing and changing of
basic structural components of a CPG. The 10 types
Characterisation of Clinical Practice Guideline Changes
253
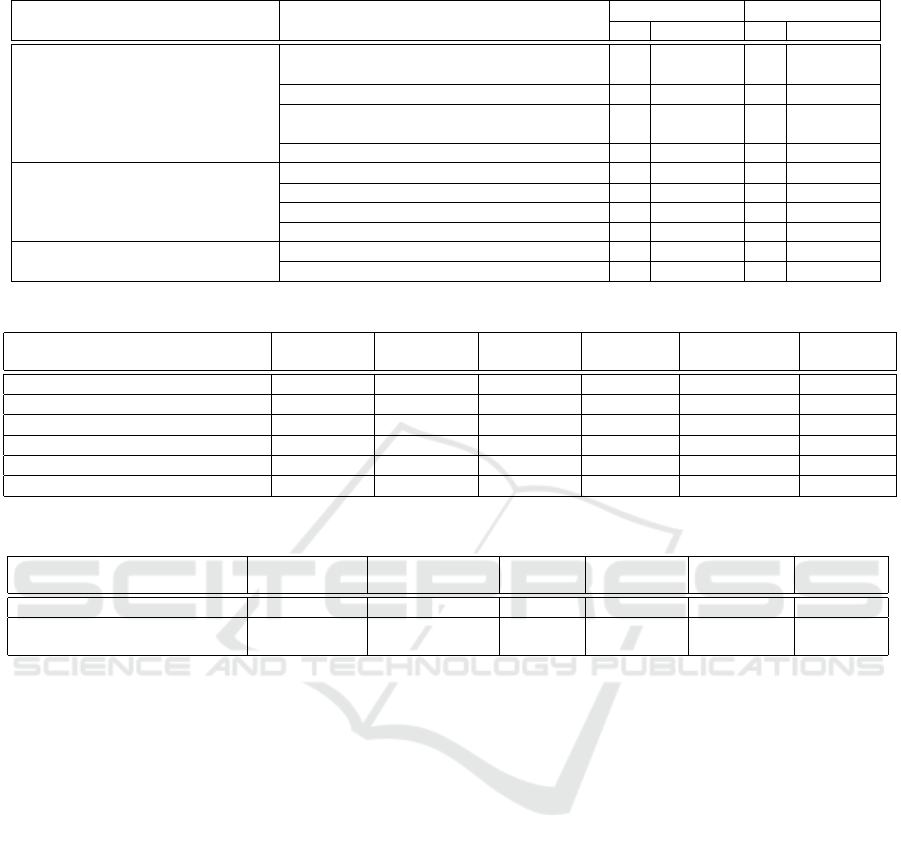
Table 1: Frequency of changes in the Malawi clinical management of HIV CPGs.
Category Type of change
2008/2011 2011/2014
# % of total # % of total
Decision modification
Addition of a decision variable to a guide-
line condition
3 1.8 2 5.6
Change of a decision variable value 13 7.6 4 11.1
Removal of a decision variable from a
guideline condition
2 3.8 2 1.2
Change of a decision variable 12 7.0 5 13.9
Action modification
Addition of a recommended action 2 1.2 0 0.0
Removal of a recommended action 2 1.2 0 0.0
Change of an action verb complement 5 2.9 4 11.1
Change of a recommended action 2 1.2 0 0.0
Recommendation modification
Addition of a recommendation 55 32.2 16 44.4
Removal of a recommendation 75 43.9 3 8.3
Table 2: CPG structural components explicitly defined in CIG models.
Structural Component Arden
Syntax
GLIF SAGE EON PROforma Asbru
Condition (C) Yes Yes Yes Yes Yes Yes
Decision variable (DV) No No No No No No
Decision variable value (DVV) No No No No No No
Recommended action (RA) Yes Yes Yes Yes Yes Yes
Action verb (AV) No No No No No No
Action verb complement (AVC) No No No No No No
Table 3: Representation primitives in existing CIG models.
Structural Component Arden
Syntax
GLIF SAGE EON PROforma Asbru
Condition (C) Logic slot Decision step Decision Decision Decision Plan
Recommended action (RA) Action slot Action spec Action Action/
Activity
Action/
Inquiry
Condition
of CPG changes identified within three categories
cover changes that affect both coarse-grained and
fine-grained structural components of a CPG. The
coarseness of the basic structural components in ex-
isting CIG models can not sufficiently allow for spec-
ification of precise semantics for CPG change opera-
tions. This limits the ability to explore the properties
and limitations of existing CIG models with respect
to handling the 10 types of CPG changes. Extensions
to include the fine-grained structural components in a
CIG would provide a sufficient foundation for mod-
elling change operations that can be used to provide
adequate knowledge evolution support in an imple-
mentation.
The categorisation of changes can also apply to
other developing countries with similar characteris-
tics, such as those in the sub-Saharan Africa. In ad-
dition, the categorisation of changes can also apply
to other clinical domains that deploy or task-shifted
health workers such as clinical management of dia-
betes.
There was a significant difference between the up-
dates introduced in the 2011 and the 2014 version of
the CPGs with regards to the number of new guide-
line recommendations that were introduced in each
update. This might have been due to the fact that
Malawi introduced new recommendations into the
2011 Malawi CPGs for providing HIV services based
on the 2010 World Health Organisation (WHO) rec-
ommendations for managing HIV-positive pregnant
and breastfeeding women (WHO Regional Office for
Africa, 2014).
Having identified the characteristics of types of
CPG changes and their incidences, precise semantics
for modelling and handling CPG changes can be for-
mally specified. The CPG changes and their related
semantics would give one a basis for modifying and
extending existing CIG models and related modelling
platforms with capabilities for handling CPG updates.
6 CONCLUSION
An evidence-based characterisation of the types of
CPG changes and their incidences has been described.
For each type of change, each structural component
that exhibits a change and a description of how that
HEALTHINF 2016 - 9th International Conference on Health Informatics
254

particular change occurs has been specified precisely
to facilitate its implementation. The characterisa-
tion of the types of changes serve as a foundation
for devising formal semantics for handling CPG up-
dates in a CIG model suitable for regions that have
adopted task-shifting. The CIG model would later
serve as a template for CIG implementation with ad-
equate knowledge evolution support within an overall
CDSS architecture. Future work would include de-
termining an appropriate criteria for establishing the
level of severity associated with each type of change
so as to assist in prioritising the types of changes that
can be supported during tool implementation.
We have commenced with the design of enhanced
CIG-based CDSSs that are based on a CIG model that
explicitly defines fine-grained structural components
and precise change operations of a CPG. This model
allows us to develop CIG maintenance tools that can
handle the various types of CPG changes to ensure
maintainability and potential for longevity of the re-
sulting e-health solutions.
ACKNOWLEDGEMENTS
This work is supported by the HPI Research School in
Service Oriented Computing and the Research Centre
in ICT4D at the University of Cape Town.
REFERENCES
Bates, D. W., Kuperman, G. J., et al. (2003). Ten command-
ments for effective clinical decision support: Mak-
ing the practice of evidence-based medicine a reality.
JAMIA, 10(6):523–530.
Chawani, M. S. (2014). A Cross-case Analysis of the Ef-
fects of EMR Deployment on Antenatal Care Services
in Rural Health Centres in Malawi. Journal of Health
Informatics in Africa, 2(1).
Chen, L., Evans, T., et al. (2004). Human resources
for health: overcoming the crisis. The Lancet,
364(9449):1984–1990.
Coiera, E. (2003). Guide to Health Informatics. Oxford
University Press Inc.
de Clercq, P., Kaiser, K., and Hasman, A. (2008).
Computer-interpretable guideline formalisms. Studies
in Health Technology and Informatics, 139:22–43.
Douali, N., Csaba, H., et al. (2014). Diagnosis Sup-
port System based on clinical guidelines: compari-
son between Case-Based Fuzzy Cognitive Maps and
Bayesian Networks. Computer Methods and Pro-
grams in Biomedicine, 113(1):133–143.
Douglas, G. P. et al. (2011). Simplicity and usability:
Lessons from a touchscreen electronic medical record
system in Malawi. Interactions, 18(6):50–53.
Field, M. J. et al. (1992). Guidelines for Clinical Practice::
From Development to Use. National Academies Press.
Fraser, H. S. F., Biondich, P., et al. (2005). Implementing
electronic medical record systems in developing coun-
tries. Informatics in Primary Care, 13.
Fulton, B. D. et al. (2011). Health workforce skill mix and
task shifting in low income countries: a review of re-
cent evidence. Hum Resour Health, 9(1):1.
Hotez, P. J. and Kamath, A. (2009). Neglected tropical dis-
eases in sub-saharan africa: Review of their preva-
lence, distribution, and disease burden. PLoS Negl
Trop Dis, 3(8):e412.
Kaiser, K. and Miksch, S. (2009). Versioning computer-
interpretable guidelines: Semi-automatic modeling
of living guidelines using an information extraction
method. AIM, 46(1):55–66.
Lewis, Z. L., Mello-Thoms, C., et al. (2011). The feasibility
of automating audit and feedback for ART guideline
adherence in Malawi. JAMIA, 18(6):868–874.
Michalski, R. S. (1983). A theory and methodology of in-
ductive learning. In Michalski, R. S. et al., editors,
Machine Learning, Symbolic Computation, pages 83–
134. Springer Berlin Heidelberg.
Msosa, Y. J., Densmore, M., and Keet, C. M. (2015). To-
wards an architectural design of a guideline-driven
EMR system: A contextual inquiry of malawi. In Pro-
ceedings of ICTD, ICTD ’15, pages 49:1–49:4. ACM.
Peleg, M. (2013). Computer-interpretable clinical guide-
lines: A methodological review. Journal of Biomedi-
cal Informatics, 46(4):744–763.
Peleg, M. and Tu, S. (2006). Decision support, knowledge
representation and management in medicine. Yearb
Med Inform, 45:72–80.
Shiffman, R. N. (1997). Representation of clinical practice
guidelines in conventional and augmented decision ta-
bles. JAMIA, 4(5):382–393.
Silver, H. F., Dewing, R. T., and Perini, M. J. (2012). The
Core Six: Essential Strategies for Achieving Excel-
lence with the Common Core. ASCD.
Sordo, M. et al. (2003). GELLO: An Object-Oriented
Query and Expression Language for Clinical Deci-
sion Support. AMIA Annual Symposium Proceedings,
2003:1012.
WHO Regional Office for Africa (2014). Implementation of
Option B+ for prevention of mother-to-child transmis-
sion of HIV: the Malawi experience. Technical report,
The World Health Organisation.
Willis-Shattuck, M. et al. (2008). Motivation and retention
of health workers in developing countries: a system-
atic review. BMC Health Services Research, 8(1):247.
Zachariah, R., Ford, N., et al. (2009). Task shifting in
HIV/AIDS: opportunities, challenges and proposed
actions for sub-Saharan Africa. Transactions of the
Royal Society of Tropical Medicine and Hygiene,
103(6):549–558.
Zamborlini et al. (2014). Towards a conceptual model
for enhancing reasoning about clinical guidelines. In
Miksch, S. et al., editors, Knowledge Representation
for Health Care, number 8903 in LNCS, pages 29–
44. Springer.
Zheng et al. (2009). Guideline representation ontologies for
evidence-based medicine practice. Handbook of Re-
search on Advances in Health Informatics and Elec-
tronic Healthcare Applications: Global Adoption and
Impact of Information Communication Technologies,
page 234.
Characterisation of Clinical Practice Guideline Changes
255
