
Mapping of Terminology Standards
A Way for Interoperability
Sven Van Laere, Frank Verbeke, Frederik Questier, Ronald Buyl and Marc Nyssen
Department of Biostatistics and Medical Informatics – Public Health,
Vrije Universiteit Brussel, Laarbeeklaan 103, 1090 Jette, Belgium
{svvlaere, fverbeke, fquestie, rbuyl, mnyssen}@vub.ac.be
Keywords: Terminology standard, interoperability, eHealth
Abstract: Standards in medicine are essential to enable communication between healthcare providers. These standards
can be used either for exchanging information, or for coding and documenting the health status of a patient.
In this position paper we focus on the latter, namely terminology standards. However, the multidisciplinary
field of medicine makes use of many different standards. We propose to invest in an interoperable electronic
health record (EHR) that can be understood by all different levels of health care providers independent of the
kind of terminology standard they use. To make this record interoperable, we suggest mapping standards in
order to make uniform communication possible. We suggest using mappings between a reference
terminology (RT) and other terminology standards. By using this approach we limit the number of mappings
that have to be provided. The Systematized Nomenclature of Medicine, Clinical Terms (SNOMED CT) can
be used as a RT, because of its extensive character and the preserved semantics towards other terminology
standards. Moreover, a lot of mappings from SNOMED CT to other standards are already defined previously.
1 INTRODUCTION
In medical practice a lot of standards are
used (Gaynor, Myung, Gupta, Rawn, & Moulton,
2008), not only for exchanging information between
medical instances, i.e. communication standards, but
also for documenting and coding of medical data, i.e.
terminology standards. In this paper we will focus on
terminology standards and their variety. Different
terminology standards are used, even for referring to
an identical concept: GP’s use the International
Classification of Primary Care, 2nd edition (ICPC-2),
physicians in hospitals use the Systematized
Nomenclature of Medicine, Clinical Terms
(SNOMED CT), coding teams in hospitals use the
International Classification of Diseases and Related
Health Problems, version 10 (ICD-10) for
reimbursement claims, and so on.
Next to the multidisciplinary use of standards by
the various health care providers, we also need to deal
with differing structures in these standards. In this
article we accept the definition of de Lusignan (2005)
who makes a distinction between codes,
classifications, terminologies and nomenclatures.
De Lusignan defined them as follows:
Codes assign a label to a certain concept.
A classification groups concepts together,
defined by a common characteristic.
Terminologies assign labels to a certain
domain.
Nomenclatures assign codes to concepts that
can even be combined to constitute new
complex concepts.
If we look back in history, medical records were
represented only using free text for a long time. The
reason codes became important was since text-based
retrieval is hard. Not much later, the idea of linking
similar clinical ideas together resulted in
classifications. Nowadays terminology standards use
codes that uniquely represent concepts, e.g. code A00
represents the cholera disorder using ICD-10
encoding. Moreover this terminology makes use of
groupings, e.g. the block of codes represented by code
A00 up to A09, represents Intestinal infectious
diseases, the cholera disorder is thus an intestinal
infectious disease.
76
Van Laere S., Verbeke F., Questier F., Buyl R. and Nyssen M.
Mapping of Terminology Standards - A Way for Interoperability.
DOI: 10.5220/0005889700760080
In Proceedings of the Fourth International Conference on Telecommunications and Remote Sensing (ICTRS 2015), pages 76-80
ISBN: 978-989-758-152-6
Copyright
c
2015 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
Classification concepts have a single relationship
with their direct predecessor; this can be either an is
a relationship or a grouping relationship that is more
generic. For example, the ICD-10 concept J20 with
description “Acute bronchitis” is the parent of the
concept with code J20.0 with description “Acute
bronchitis due to Mycoplasma pneumonia”. In
ICD-10, the textual representation of the codes
expresses the relationship with their parent. Next to
classifications, we have nomenclatures, e.g.
SNOMED CT, that also include more specialized
relationships to express associations such as
laterality, finding site, severity, … Moreover, in
SNOMED CT, if there is a concept that is not yet
included in the standard, one can also rely on its post-
coordinated representation by combining
SNOMED CT concepts (Cornet, Nyström, &
Karlsson, 2013).
Documentation and coding of problems,
diagnoses and treatments is getting more valuable to
work towards an electronic health record
(EHR) (Dickerson & Sensmeier, 2010). The data of
this record should not only be used in a uniform way,
it should also be possible to interpret the EHR in the
same way, from a GP in his medical practice to a
physician in the hospital. In healthcare all providers
work together in order to deliver the best care to the
patient. However, since in the different levels of
healthcare, different terminology standards are being
used with different underlying structures, we should
address the topic on how to align these standards to
make them interoperable.
Often a combination of free text and coded text is
used in patient record documents. Working towards
optimal use of coding inside the health record will
lead to better documentation of the patient’s health
status and eventually more appropriate treatment will
lead to improvement of a patient's health.
This paper proposes to introduce a bridge between
different terminology standards using a reference
terminology (RT). This RT must fulfill the
requirement of being semantic interoperable with
other terminology standards. We will further discuss
how we can work towards this interoperability in
Section 2. We will provide a discussion in Section 3
and give a conclusion in Section 4.
2 MAPPING STANDARDS
Currently, many care providers have to reenter the
same data over and over again. When a patient
contacts a GP for a problem and needs to be referred
to the hospital, the GP’s data is copied by reentering
the data in its appropriate form by the physician in a
hospital. Instead of entering data over and over again,
we propose to introduce a mapping between different
terminology standards.
2.1 Mapping
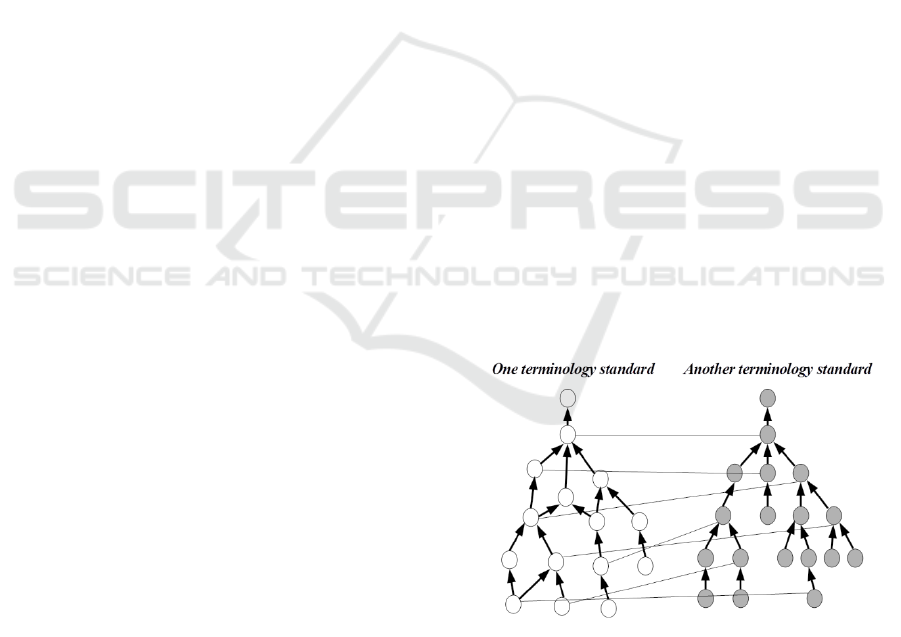
A mapping is a linkage between a concept from one
standard to another standard (see Figure 1) based on
the equivalence between the two concepts. This is not
only done by comparing the syntactical
representation of a concept, i.e. the description of a
concept. We propose to make mappings between
standards, using the following guidelines:
Consider the place in the hierarchy of a
terminology standard;
Consider the semantics of a concept;
Consider the relationship with other
concepts around a concept (if appropriate).
When we apply the process of mapping concepts
of different terminology standards, we do have two
approaches: manual mapping or semi-automatic
mapping. In the manual approach we rely on human
knowledge of medical experts, linguists, terminology
experts… Or we can use a computer algorithm that
queries for candidate mappings based on the lexical
representation of a concept, i.e. the description. After
the candidate mappings are identified, human review
of the automatic mapping is still required to evaluate
the found mappings according to the abovementioned
guidelines. This approach is thus less time consuming
w.r.t. the manual mapping approach where experts
manually identify and validate the mappings.
Figure 1: Mapping from one standard to another.
2.2 Semantic interoperability
In healthcare, interoperability is defined as the state
which exists between two application entities, when
one application entity can accept and understand data
Mapping of Terminology Standard
A Way for Interoperability
77

from the other and perform that task without the need
for extra operator intervention. (Aguilar, 2005)
Interoperability can be established at the level of
semantics, i.e. semantic interoperability. This means
that the information should be understood at the level
of domain concepts.
When links between terminology standards are
established, we ensure translation of one standard to
another is computer processable without losing the
aspect of semantics is possible. The degree of
semantic interoperability then depends on the level of
agreement regarding the terminologies and the
conceptual representation behind it.
In the process of communication between a GP
and a physician, they both are allowed to use their
own proper language (i.e. codes of a terminology
standard). By using mappings we can find the
equivalent concept in the other terminology standard
if a mapping is provided.
2.3 Wide variety of standards
Since a wide variety of medical standards exists and
insufficient effort is invested in e-health standard’s
interoperability, we assume it is worth-while to invest
in providing mappings between different standards.
We propose to do this in a step by step approach as
proposed by the International Health Terminology
Standards Development Organisation (IHTSDO,
2014), since this mapping process will be a time-
consuming effort. Since clinical terminologies
typically consist of several thousands of concept
codes per terminology, we propose to provide
mappings per medical domain, such as cardiology,
nursing, and others instead of mapping the whole
terminology at once. We can then evaluate the
process of mapping one domain and – if successful –
apply it to another domain.
Even if we know the principles for mapping, the
problem of the wide variety of medical vocabularies
still remains:
ICPC-2 classifies patient data and clinical
activities in the domain of general/family
practice and primary care (Verbeke, Schrans,
Deroose, & De Maeseneer, 2006);
ICD-10 is a classification used to monitor the
incidence and the prevalence of diseases and
other health problems (WHO, 2015);
Logical Observation Identifier Names and
Codes (LOINC) is the universal standard for
identifying medical laboratory observations
(McDonald et al., 2003);
NANDA is an international classification used
in the nursing domain (Müller-Staub, Lavin,
Needham, & van Achterberg, 2007);
SNOMED CT is a nomenclature used for
exchanging healthcare information between
physicians and other healthcare providers
(Donnelly, 2006);
…
2.4 Reference terminology
If we apply a mapping from each terminology
standard to another (see Figure 2a), we end up with
𝑁∙(𝑁−1)
2
mappings that are necessary, where N is the
number of standards. We propose the use of a
common reference terminology (RT) from which we
map to each medical standard (see Figure 2b). The
number of mappings needed is then equal to N.
For this reference terminology, it is key to find the
terminology that is the most comprehensive in the
medical domain, containing also concepts from
various domains. SNOMED CT covers more than
310,000 concepts and is likely to be the most
appropriate to use as RT. Moreover, SNOMED CT is
the only standard providing both pre-coordinated and
post-coordinated expressions (Benson, 2010).
Pre-coordination is used when a clinical idea is
represented by a single concept id, e.g. fracture of
tibia is represented by concept id 31978002.
Post-coordinated expressions on the other hand use a
combination of concept ids to represent a concept,
e.g. fracture of the left tibia can be represented as
31978002 : 272741003 = 7771000, that represents
fracture of tibia : laterality = left.
Figure 2a: Mapping each standard to every other standard.
2b: Mapping using a reference terminology (RT)
3 DISCUSSION
In this paper we propose an approach for a more
interoperable health record of the patient. We have to
explore the possibilities of mappings fully in a certain
Fourth International Conference on Telecommunications and Remote Sensing
78

healthcare domain and evaluate the benefits of it. We
propose to use SNOMED CT as a reference
terminology (RT).
At the time of writing an EU project, named
ASSESS CT - Assessing SNOMED CT for Large Scale
eHealth Deployments in the EU (ASSESS-CT, 2015),
is attempting to evaluate the fitness of the
international clinical terminology SNOMED CT as a
potential standard for EU-wide e-health deployments.
Based on the ASSESS-CT project, an evaluation must
be made of the advantages and disadvantages of using
SNOMED CT as potential RT standard for the EU. If
this fitness evaluation turns out negative, we may
need to investigate the possibility of using
another RT.
An argument in favor of using SNOMED CT as a
RT is that there already exists a lot of mappings from
SNOMED CT to other terminology standards:
ICD-10
ICD-10-CM (CM indicates a clinical
modification of the ICD standard)
ICD-9-CM
ICD-O3 (ICD for the oncology domain)
ICPC-2
LOINC
Nursing classifications, such as NANDA, NIC,
ICNP, …
Pharmaceutical classifications such as WHO’s
ATC and the US National Library of
Medicine’s RxNorm
CPT (medical procedure codes)
Another candidate RT is the Unified Medical
Language Systems (UMLS) that was designed and is
maintained by the National Library of Medicine
(NLM) (Humphreys, Lindberg, Schoolman, &
Barnett, 1998). UMLS is a collection of vocabularies
biomedical health sciences already providing the
linkage between them. This system exists of three
knowledge sources: the Metathesaurus, the Semantic
Network, and the SPECIALIST Lexicon and Lexical
Tools. UMLS clusters terms of terminology standards
that are equal in one UMLS concept and assigns them
a unique id. SNOMED CT is also integrated in this
Metathesaurus. Though UMLS does not follow the
semantics of SNOMED CT completely (NLM, 2007).
As stated by Garla and Brandt (2012) the tool support
for using UMLS with respect to SNOMED CT is
more robust, whereas semantic differences within
UMLS may affect the accuracy of similarity
measures. Since the semantics are of utmost
importance, we opt to use SNOMED CT instead.
If we use mappings between terminology
standards, these mappings are not always
bidirectional in use: if a mapping between two
concepts of two terminology standards does exist, this
is not necessarily the case in reverse. For example the
map from SNOMED CT to ICD-10, cannot be
reversed since it is common for many details, and
different SNOMED CT concepts map to a single
ICD-10 code. Reversing the map is not possible since
one ICD-10 code would refer to many different
SNOMED CT concepts.
We believe working together towards a more
integrated EHR, based on a RT, will benefit to the
care of patient. The inter-terminology mapping
should preferably be an automated background
process that is transparent to the health care provider
or EHR user and should not interfere with the routine
clinical documentation practice.
Since the RT will be used in the shared EHR, the
semantics will be implied by the RT. Moreover, by
making use of the mappings, care providers will
always be able to view the content using the
terminology standard that was originally used.
Eventually, more extensive use of a RT will also
create new clinical decision support opportunities
leading to better patient care.
4 CONCLUSIONS
For recording of information in health care, a
combination of free text and coded text is often used.
In order to improve information sharing for the
purpose of patient care or for the management of the
hospital, we should invest in mechanisms enabling
full and transparent use of coded information in the
health record. Most service providers already use one
or more terminology standards. However, across
different service providers different standards are
used. Therefore, sharing information and knowledge
about the patient often does not happen in an
interoperable way.
This paper proposes a reference terminology
based mapping approach in order to meet this
requirement. A reference terminology (RT) has the
advantage of limiting the number of mappings that
must be made. The proposed RT is SNOMED CT,
because it is the most extensive medical terminology
in use, it supports both pre- and post-coordination and
the semantics are preserved with respect to other
terminology standards. Another reason for choosing
SNOMED CT is the amount of resources that are
available. There already do exist a lot of mappings
from SNOMED CT to other terminology standards,
respecting the accuracy of similarity metrics between
different terminology standards.
Mapping of Terminology Standard
A Way for Interoperability
79

Sufficient effort should be invested in making the
mappings database more complete. This is a time
consuming process and therefore a step by step
approach is suggested. Start by testing the idea in one
domain and then apply it in another one. Eventually
this will lead to a shared EHR ensuring
interoperability between care providers. Large
collections of structured data related to patient health
status and health care provider activity can ultimately
contribute to EHR systems capable of providing
clinical decision support.
REFERENCES
Aguilar, A. 2005. Semantic Interoperability in the Context
of e-Health. In CDH Seminar ’05, Galway, Ireland.
ASSESS-CT. 2015. ASSESS CT - Assessing SNOMED CT
for Large Scale eHealth Deployments in the EU.
Available from: http://www.assess-ct.eu
Benson, T. 2010. SNOMED CT. In Benson, T. (ed.),
Principles of Health Interoperability HL7 and
SNOMED (pp. 189–215). doi:10.1007/978-1-84882-
803-2
Cornet, R., Nyström, M., & Karlsson, D. 2013. User-
directed coordination in SNOMED CT. In C. U.
Lehmann, E. Ammenwerth, & C. Nøhr (Eds.), Studies
in Health Technology and Informatics (Vol. 192, pp.
72–76). doi:10.3233/978-1-61499-289-9-72
De Lusignan, S. 2005. Codes, classifications, terminologies
and nomenclatures: definition, development and
application in practice. Informatics in Primary Care,
13(1), 65-70. Retrieved from:
http://www.ingentaconnect.com/ content/bcs/ipc
Donnely, K. 2006. SNOMED-CT: The advanced
terminology and coding system for eHealth. Studies in
Health Technology and Informatics, 121, 279-290.
Dickerson, A.E. & Sensmeier, J. 2010. Sharing data to
ensure continuity of care. Nursing Management, 41(7),
19-22. doi:10.1097/01.NUMA.0000384142.04693.58
Garla, V.N. & Brandt, C. 2012. Semantic similarity in the
biomedical domain: an evaluation across knowledge
sources. BMC Bioinformatics, 13, 261-273.
doi:10.1186/1471-2105-13-261
Gaynor, M., Myung, D., Gupta, A., Rawn, J., & Moulton,
S. 2008. Interoperability of medical applications and
devices. In R. H. Sprague Jr. (Ed.), Proceedings of the
41st Hawaii International Conference on Systems
Science, 7-10 January 2008, Waikoloa, Big Island, HI,
USA. doi:10.1109/HICSS.2008.217
Humphreys, B. L., Lindberg, D. A. B., Schoolman, H. M.,
& Barnett, G. O. 1998. The Unified Medical Language
System: An Informatics Research Collaboration.
Journal of the American Medical Informatics
Association, 5(1), 1-11.
doi:10.1136/jamia.1998.0050001
IHTSDO. 2014. Mapping to SNOMED CT. Discussion and
Guidance on Mapping Based Solutions Design for
Migration or Transformation. Available from
https://csfe.aceworkspace.net/sf/go/doc10065
McDonald, C.J. et al. 2003. LOINC, a Universal Standard
for Identifying Laboratory Observations: A 5-Year
Update. Clinical Chemistry, 49(4), 624-633.
doi:10.1373/49.4.624
Müller-Staub, M., Lavin, M. A., Needham, I., & van
Achterberg, T. 2007. Meeting the criteria of a nursing
diagnosis classification: Evaluation of ICNP®, ICF,
NANDA and ZEFP. International Journal of Nursing
Studies, 44(5), 702-713.
doi:10.1016/j.ijnurstu.2006.02.001
NLM. 2007. Insertion of SNOMED CT® into the UMLS®
Metathesaurus®: Explanatory Notes. Available from
https://www.nlm.nih.gov/research/
umls/Snomed/snomed_represented.html
WHO. 2015. International Classification of
Diseases (ICD). Available from http://www.who.int/
classifications/icd/en/.
Verbeke, M., Schrans, D., Deroose, S., & De Maeseneer, J.
2006. The International Classification of Primary Care
(ICPC-2): an essential tool in the EPR of the GP.
Studies in Health Technology and Informatics, 124,
809–814. doi: 10.3233/978-1-58603-647-8-809
Fourth International Conference on Telecommunications and Remote Sensing
80
