
A Proposal to Incorporate Digital Auscultation and Its Processing into an
Existing Electronic Health Record
P. Gomes
1
, S. Frade
2,4
A. Castro
3
, R. Cruz-Correia
2,4
and M. Coimbra
1
1
Instituto de Telecomunicac¸
˜
oes, Faculdade de Ci
ˆ
encias, Universidade do Porto, Porto, Portugal
2
Faculdade de Medicina, Universidade do Porto, Porto, Portugal
3
Faculdade de Engenharia, Universidade do Porto, Porto, Portugal
4
CINTESIS - Center for Research in Health Technologies and Information Systems, Porto, Portugal
Keywords:
Auscultation, Digital Stethoscope, HL7, OpenEHR, e-Health.
Abstract:
This paper aims to describe and discuss a proposal to incorporate digital auscultation and its processing into
an existing EHR. The architecture was planned to be used in both primary and hospital care, and includes a
digital stethoscope; an exam collection module; an integration module; an EHR web service; and an EHR.
Special attention was given to standardize communications using HL7 and openEHR. The proposed imple-
mentation uses a commercial stethoscope, an android app to collect the data, a mirth integration engine that
communicates using HL7 or openEHR through REST or SOAP calls. The signal processing of the sounds
is also included. The auscultation sound files are made available to the EHR users. This solution will open
the possibility to have richer patient records than can be very important for patient care, research and medical
teaching. It also raises issues regarding ethical and legal concerns that must be considered in future research.
1 INTRODUCTION
The ageing population has increased steadily over the
past few years. According to the World Health Or-
ganization, in almost all countries, the proportion of
people aged over 60 years, is growing rapidly as a re-
sult of increased life expectancy and reduced fertility
rates (WHO, 2014; WHO, 2011). This raises the con-
cern to focused not only on the treatment of disease
and monitoring, but also in its prevention and active
ageing (Rechel et al., 2013; SCPSDC, 2013).
Health problems in the elderly are usually linked
to accidents, development of non-communicable dis-
eases, poverty, social isolation and exclusion, abuse,
and mental health disorders. It is also recognized that
the limitations characteristic of this population, may
often prevent their access to health care, which makes
it imperative to identify these patients for closer mon-
itoring. Remote monitoring of this population earns
great interest not only in preventing the disease, but
also in promoting an active lifestyle, and the detec-
tion of possible complications (WHO, 2012; Euro-
peanCommission, 2013). An integrated health sys-
tem brings many benefits from the point of view of
patients and health professionals. From the side of
the patient, these systems allow a myriad of oppor-
tunities, from monitoring of chronically ill patients,
health promotion and self-care, improving their over-
all condition. From the perspective of health profes-
sionals, this new paradigm allows a direct costs de-
crease by reducing the number of hospitalizations, the
risks associated with nosocomial infections, and over-
crowding. These technologies allow the extension of
health care to patients away from urban centers, en-
suring greater equity in health care, and providing fur-
ther support to the health professional through med-
ical decision support systems and alarms (Ferreira
et al., 2013; Pereira et al., 2013).
The ICT for Future Health project, led by the
University of Porto, aims to address this emerging
reality by incorporating three health data gathering
modalities into a unified Electronic Health Record
(EHR), deployed in the zone of influence of a pri-
mary care center in the northern region of Portugal
(USF Nova Via) that covers a population of around
7000 isolated elderly inhabitants. These three modal-
ities are: continuous self assessment of patients using
wearable sensing, self assessment of patients within a
health kiosk environment, and assessment of patients
by clinicians either at home or in a primary care envi-
ronment. In this paper we will address the integration
of the later into the unified EHR of the ICT for Future
143
Gomes P., Frade S., Castro A., Cruz-Correia R. and Coimbra M..
A Proposal to Incorporate Digital Auscultation and Its Processing into an Existing Electronic Health Record.
DOI: 10.5220/0005222901430150
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2015), pages 143-150
ISBN: 978-989-758-068-0
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

Health project.
1.1 Heart Auscultation
Auscultation is a standard medical exam for heart
pathology screening, and although it is the gold stan-
dard for heart condition monitoring, it is a difficult
skill to master (Carapetis et al., 2008). Besides, there
is not still a way of storing this important data for
patient follow-up; the current practice does not take
this into consideration, losing important information
in case of disease detection/evolution. There is not
yet a standard for heart sound collection and trans-
mission that may allow different professionals to eval-
uate the same signal (general practitioner and cardi-
ologist e.g.). The DigiScope data collection system
presented in Figure 1 was designed to fill this gap,
collecting an auscultation using an electronic stetho-
scope, along with patient clinical data and annotations
(Pereira et al., 2013).
Figure 1: DigiScope collector (DSCollector), used for elec-
tronic auscultation, with an electronic stethoscope and a
tablet.
1.2 Electronic Health Records & HL7
OpenEHR (openEHR, 2013) is a non-proprietary
standard architecture for electronic health records.
OpenEHR lets you capture and store clinical knowl-
edge in a structured manner, independent of software,
providing interoperability of health information sys-
tems, avoiding trapping data in proprietary systems
and increasing support for distributed clinical work
flows. OpenEHR allows the standardization of the
Electronic Health Record (EHR) architecture follow-
ing a multi-level modelling approach, which sepa-
rates information from knowledge (Beale and Heard,
2008). The first level (the reference model - RM)
specifies a generic model according to which data will
be stored and communicated. The second level (the
archetype model) defines constraints in the reference
model that represent concepts in a specific domain.
Trough the use of archetypes (structured concepts of
clinical knowledge) and templates (combination of
archetypes related to a particular clinical task), the
semantic meaning and functionality is kept indepen-
dent of the systems collecting or holding the data (e.g.
clinical records, mobile systems). The archetypes
can be developed in any language and later be trans-
lated to other languages (e.g., Portuguese, English,
Chinese, Swedish) keeping their original meaning.
In addition, terminologies can be associated within
archetypes elements supporting their definition.
Health Level 7 (HL7) is a well established
message-based standard developed by the American
National Standards Institute (ANSI) accredited stan-
dards developing organization Health Level 7 Inc. It
aims to develop coherent and extensible standards for
the exchange, management and integration of elec-
tronic information in the clinical and administrative
domain (Health Level Seven International, 2007).
HL7 refers to the Application Level of the OSI seven
layers model. This level describes how data are ex-
changed and the timing of the interchange as well
as the handling of communication errors. According
to Health Level Seven, HL7 version 2.5 is the most
widely implemented standard for health care informa-
tion worldwide.
HL7 contains many optional data segments which
makes it very flexible but at the same time impossible
to guarantee standard conformance of any vendors’
implementation. This has the regrettable consequence
that vendors might need more time to analyse and
plan their interface to assure that the same optional
features are used by both parties (Health Level Seven
International, 2007). The vagueness in the standard,
the lack of a consistent application data model, a for-
mal methodology to model data artefacts and the lack
of well defined application user roles were issues ad-
dressed in HL7 version 3.0. It uses an object-oriented
development methodology based on a data model, the
Reference Information Model (RIM), to create mes-
sages. RIM provides an explicit representation of
semantic and lexical connection that exists between
the information transferred in HL7 version 3.0 mes-
sages (Health Level Seven International, 2007).
1.3 Aim
Since auscultation is the first line of screening of car-
diovascular pathologies, but it is still not part of the
electronic health record, this paper aims to describe
and discuss a proposal to incorporate digital auscul-
tation and its processing into an existing electronic
health record.
HEALTHINF2015-InternationalConferenceonHealthInformatics
144

2 STORYBOARD
The new paradigms of societal change imposed to
healthcare have taken monitoring and data storage to a
new level of systems interoperability. To better illus-
trate this new scenario, we will describe a storyboard
to facilitate understanding of our service application.
2.1 At Primary Care Unit
Mrs. Amelia is a 72 years old woman, living alone in
a rural house far from the city centre. Mrs. Amelia
is autonomous, although she presents a few chronic
health conditions: type II diabetes, hypertension and
dyslipidemia. Mrs. Amelia has regular appointments
with her general practitioner (GP) in her primary care
unit, to analyze and manage her health condition, and
when necessary, adjust the medication. Her consul-
tation includes several physical observations, as stan-
dard clinical practice routine, including a heart aus-
cultation. Her GP auscultates her with an electronic
stethoscope, connected to a tablet (DSCollector), that
links this information to her electronic health record
(EHR), storing each auscultation as an observation of
the consultation, identified with her national health
identification number.
The heart sound, or phonocardiogram (PCG)
record, is stored with her clinical data and with the de-
scription of the findings of the auscultation redeemed
by the GP. When the collected PCG is sent to the EHR
in the server, it passes through a signal processing unit
that automatically extracts several features from the
auscultation useful for clinical evaluation (heart rate,
S12 and S21 time intervals, presence of murmurs and
its shape and intensity, extra heart sounds, or hyper-
phonesis e.g.). This information is then fed to a ma-
chine learning algorithm that incorporates PCG fea-
tures with the patient clinical data, providing an ad-
visory system for the GP in case of warning signs,
that may lead to further evaluation from a Cardiology
specialist. This way, there is a register of the evolu-
tion of the heart sound and a possible alarm in case of
missed events by the GP. In her last appointment Mrs.
Amelia condition was stable, and she returned to her
home until the next appointment.
2.2 At Home to a Central Hospital
Last week, Mrs. Amelia had a small accident and
fractured her left foot, leaving her with limited mo-
bility. Since Mrs. Amelia lives in a small village, far
from the city centre, she was unable to continue her
regular appointments, and the health care was deliv-
ered to her directly at home by a nurse. Every time
the nurse leaves the primary care unit, the tablet con-
nects to the central server, and receives the data from
the scheduled patients for home visit that day. Ev-
ery patient scheduled for visit has his/her information
on the tablet, and after observation, the collected data
will be synchronized with the server to update in case
of change, and save the auscultation as an observa-
tion on the EHR. If for some reason, the health care
professional needs to visit a patient that is not consid-
ered in the schedule of that day, he/she may add a new
patient, using the national health identification num-
ber; after collection, and when synchronizing with the
central server, this may be introduced as a new pa-
tient, with the correspondent exam, or as an observa-
tion for an existing patient in the database, identified
through the national health identification number.
Since Mrs. Amelia has a combination of chronic
conditions, on each visit the health professional col-
lects several physiological variables in a tablet, in-
cluding her auscultation according to the clinical stan-
dards. The visiting nurse was trained to perform an
auscultation, directly sent to Mrs. Amelias EHR at the
central server, and later analyzed by her GP. The PCG
collected during the last visit was processed at the
server, detecting a systolic murmur in her PCG. This
event generated an alarm to her GP, that listened to
her auscultation, confirming the clinical finding. Mrs.
Amelia GP shared the auscultation with the Cardiolo-
gist from the regional hospital, for a second opinion,
who considered that Mrs. Amelia was indicated for
further evaluation. Mrs. Amelia was immediately re-
ferred to a Cardiology consultation, where she contin-
ued to be accompanied.
Data collected in both scenarios includes the per-
sonal information (age, weight, height and gender),
clinical data resulting from the examination (systolic
and diastolic blood pressure, oximetry, and a text field
for comments), and the auscultation file (audio files,
one for each auscultation spot).
3 ARCHITECTURE
The proposed architecture (figure 2) is composed by 5
modules that are independent of each other. We have
the digital stethoscope; the collection module; the in-
tegration module; the EHR web service; and finally
the EHR.
In the digital stethoscope we use is the Littmann
3200 stethoscope without any modification, this
choice was made taking in consideration the accep-
tance from the medical staff and usability purposes.
The collection module is assured with the DSCol-
lector application. An android application that will
AProposaltoIncorporateDigitalAuscultationandItsProcessingintoanExistingElectronicHealthRecord
145
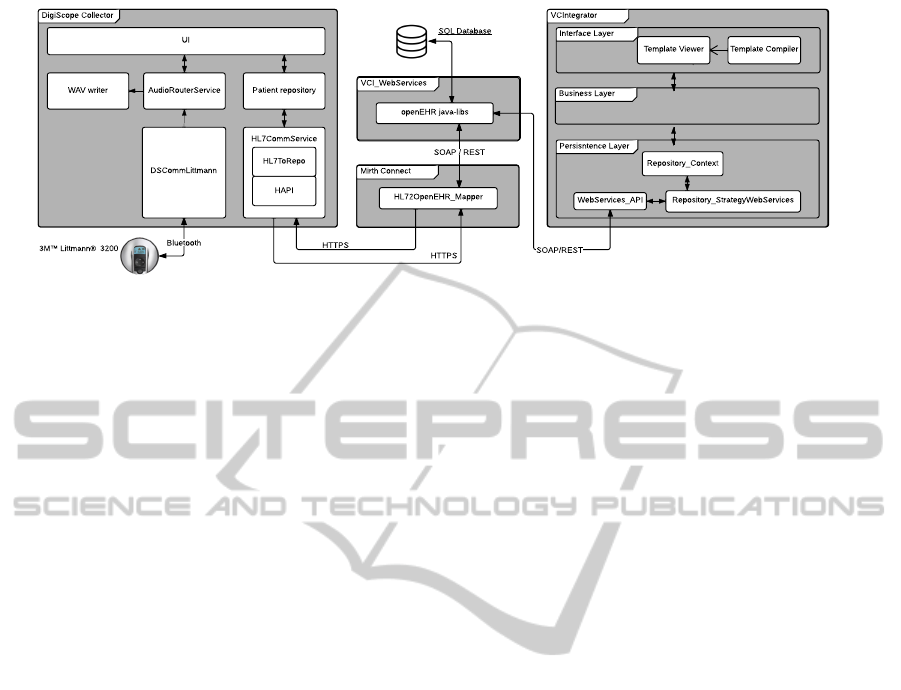
Figure 2: Architecture proposed with all the modules and information flows. The Littmann stethoscope sends the auscultation
to the Digiscope Collector (collection module) via bluetooth. Then, this module communicates using HL7 messages with the
Mirth Connect (integration module). Which in turn parses the messages, transforming them in the structure expected by the
EHR web service. This flow allows that a patient record can be sent from the mobile application to the EHR repository.
assure the communication with the stethoscope (via
bluetooth) and the storage of all the data collected
during the appointment between the healthcare pro-
fessional and the patient. This data is then compiled
in standard HL7 messages that can be sent to the EHR
modules (via HTTPS).
The integration module is our Mirth Connect that
can receive any standard HL7 message, process it and
translate it to the structure known by the EHR web
service module. This module is also capable of do-
ing the reverse communication flow, in our scenario
the collection module can also request information
about patients which requires being capable to receive
HL7 queries and sent responses in accordance with
the standard. The EHR web service module allows
an external application or service to send EHR with
a structure known to the EHR. This module can be
seen as the door to the VCIntegrator module and that
is why we need the integration module to transform
the HL7 structure to this one operated in the VCIn-
tegrator, this communication can be done with SOAP
or REST.
Finally we have the EHR itself, which has its own
structure based in OpenEHR and all the functional-
ities that are required in a systems like this. In this
architecture, our EHR is handled by the VCIntegra-
tor that is feed with patient records by our EHR web
service, this communication can be done by SOAP or
REST as well.
An important aspect to understand in the architec-
ture is the main information flows between the mod-
ules. We have two information flows that we need to
address: the retrieve of the patient list that the health-
care professional needs to visit; and the upload of the
patients records to the EHR repository. As seen in the
figure 2, the request of a patient list is made by an
HL7 request from the DSCollector to the Mirth Con-
nect, this one will parse the message and will do the
same request to the EHR web service, that will re-
trieve the list from the VCIntegrator and send it back
using the same route.
The other information flow is simpler, because
there is no need to answer. The DSCollector will up-
load the patients records to the Mirth Connect, using
HL7 messages, and this module will parse them and
send them to the EHR web service in the expected
structure.
4 IMPLEMENTATION
In this section we will address the HL7 messages that
are required to communicate between the collection
and integration modules and we will also explain how
each module was implemented.
4.1 HL7 Communication Between
Modules
The communication between the DSCollector and the
VCIntegrator will be made by HL7 standard mes-
sages, and using the already approved IHE models.
The IHE has already defined and validated two frame-
works from where we can adapt. The Patient De-
mographics Query (PDQ) and the Patient Identifier
Cross-Referencing (PIX), are two frameworks that
handle patients list exchange between any systems
(IHE, 2013). In figure 3) it is possible to see all the
message handling between the collection and the in-
tegration modules.
Each interaction between the two modules re-
quires an authentication of the user, and all the mes-
sages are exchanged under the security of this authen-
tication. The first step of the protocol is to send a
HEALTHINF2015-InternationalConferenceonHealthInformatics
146
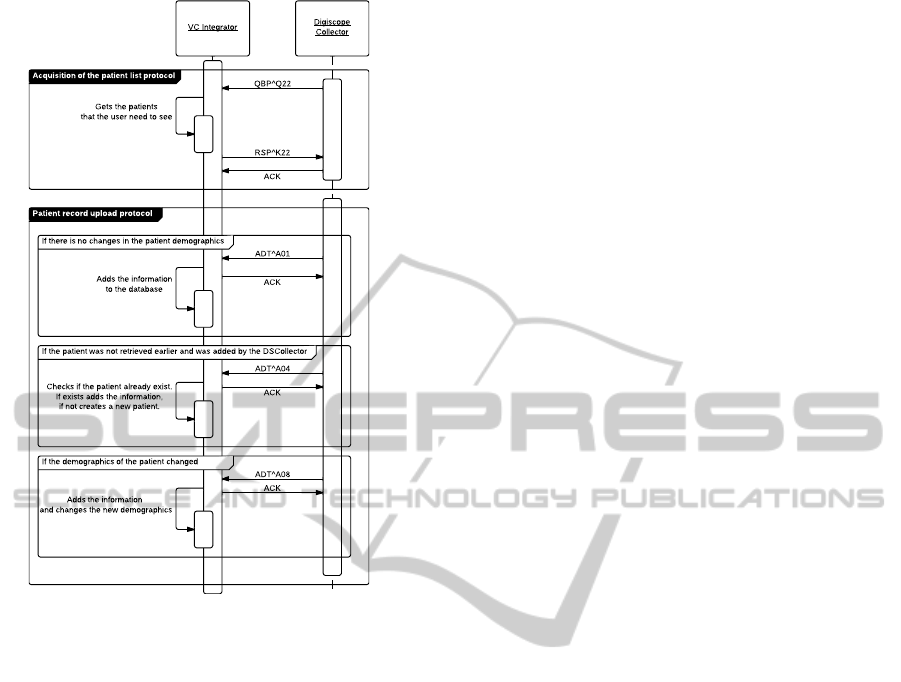
Figure 3: Communication protocol to exchange HL7 mes-
sages between the DSCollector and the VCIntegrator.
QBPˆQ22 to request all the demographics of the pa-
tients that the physician needs to see that day. In that
message it is important to notice the specific method
to request this list. Usually this message is used
to request a list of patients based on a demographic
field, but in this case, we send the identification of the
physician that is requesting his schedule. This way
we respect the standard, and the receiving application
knows what to do (see field QPD.3.1 in the Message
1) and which physician list should he send (identifi-
cation on the field QPD.3.2 in the Message 1).
Message 1: An example of a QBPˆQ22 message. This
message is requesting the list of patients that the physician,
identified in the filed QPD.3.2, needs to see during is work
day.
MSH|ˆ˜\&|DSCOLLECTOR|DSCOLLECTOR|VCINTEGRATOR|VCINTEGRATOR
|201408310830||QBPˆQ22|201408310830_5498465678|P|2.5
QPD|Q22ˆGetScheduleˆHL7|201408310830_7489764|@PV1
.7.1ˆ516886416
RCP|I|10ˆRD
With this message the VC Integrator should return
a RSPˆK22, which is the standard response to the pre-
vious message. This message is fully compliant with
the standard and should only return the demographics
of the patients to visit in that day by the requesting
physician (see Message 2). After this procedure the
physician has all the information needed to go to the
patients houses and proceed with the appointments.
Message 2: An example of a RSPˆK22 message with the
demographics of the patients.
MSH|ˆ˜\&|VCINTEGRATOR|VCINTEGRATOR|DSCOLLECTOR|DSCOLLECTOR
|201408310832||RSPˆK22|201408310832_6546871463|P|2.5
MSA|AA|201408310830_5498465678
QAK|201408310830_7489764|OK||2|2|0
QPD|Q22ˆGetScheduleˆHL7|201408310830_7489764|@PV1
.7.1ˆ516886416
PID|1||16546846||GomesˆPedro||19900101|M|||Rua do Campo
Alegreˆ1021/1055ˆPortoˆPortoˆ4169-007ˆPortugal
||+351123456789
PID|3||55587236||FradeˆSamuel||19900101|M|||Rua Dr. Plcido
da Costaˆs/nˆPortoˆPortoˆ4200-450ˆPortugal||+351123456789
In the end of the day, he needs to upload all the
data collected from the appointments to the VC In-
tegrator. In this procedure, the physician needs to
authenticate himself in the VC Integrator and send
all the patients observed as new admissions. If the
patient demographics were retrieved earlier and no
changes were made in the demographics, the DSCol-
lector needs to send a simple admission (ADTˆA01
message in Message 3) with the clinical data gath-
ered during the appointment. However, if any of the
demographics has changed, the admission should im-
ply that a change has been made (ADTˆA08 message,
similar to Message 3). And the last scenario hap-
pens when, for any reason, the physician has an ap-
pointment with an unscheduled patient that was not
retrieved earlier. In this case, we need to inform the
receiving application that the patient that we are send-
ing, does not have an identification known in the re-
ceiving database (ADTˆA04 message, similar to Mes-
sage 3) and should be added as a new patient if not
founded, or added as a normal admission if founded.
Message 3: An example of an ADTˆA01 message. This
message is used to inform of an admission. The messages
ADTˆA04 and ADTˆA08, also used in our protocol, are
very similar to this one, they use the same tags and fields
and only in the MSH header is possible to understand which
kind of message is being sent.
MSH|ˆ˜\&|DSCOLLECTOR|DSCOLLECTOR|VCINTEGRATOR|VCINTEGRATOR
|201408311800||ADTˆA01|201408311800_515674657|P|2.5
EVN|A01|201408311048
PID|16546846||16546846||GomesˆPedro||19900101|M|||Rua do
Campo Alegreˆ1021/1055ˆPortoˆPortoˆ4169-007ˆPortugal
||+351123456789
PV1||I|||||ID
ˆ516886416|||||||||||||||||||||||||||||||||||||201408311048
OBX|1|ST|8302-2ˆBody heightˆLN||180|CM
OBX|2|ST|29463-7ˆBody weightˆLN||80|KG
OBX|3|ST|8480-6ˆSystolic blood pressureˆLN||120|MMHG
OBX|4|ST|8462-4ˆDiastolic blood pressureˆLN||80|MMHG
OBX|5|ST|20564-1ˆOxygen saturationˆLN||98|%
AProposaltoIncorporateDigitalAuscultationandItsProcessingintoanExistingElectronicHealthRecord
147

OBX|6|ST|DS-OPENFIELDˆOBSˆDS||medicalObservation|txt
OBX|7|ST|DS-PCGAVˆPCG_AORTICˆDS||file encoded in Base64|wav
OBX|8|ST|DS-PCGPVˆPCG_PULMONARYˆDS||file encoded in Base64|
wav
OBX|9|ST|DS-PCGTVˆPCG_TRICUSPIDˆDS||file encoded in Base64|
wav
OBX|10|ST|DS-PCGMVˆPCG_MITRALˆDS||file encoded in Base64|
wav
In this messages, the most important segment for
our proposal is the OBX segment, because this is the
segment that carries the clinical information collected
during the appointment. In the Message 3, as exam-
ple, we can see that the DSCollector sends ten obser-
vations collected during the appointment. Some of
the fields are already common in this kind of proce-
dure, such as height, weight or oxygen saturation and
are sent using the LOINC coding system. We also
have an open field where the physician can add infor-
mation not accounted for, but the most relevant fields
are the last four. In this OBX segments we are send-
ing the phonocardiogram of the patient divided in the
four major focal points, the aortic, pulmonary, tricus-
pid and mitral valve. This sounds are collected using
the DSCollector (see section 4.3) and then encoded in
Base64 to be sent inside this message, as commonly
used in the email attachments.
4.2 Mirth/VCIntegrator
VCIntegrator (VirtualCare, 2014) is an online elec-
tronic health record which implemented the openEHR
standard, on which the health record forms are auto-
matically generated based on openEHR templates and
the data saved, following the openEHR specification.
As long as the data is stored in this specified format
it can be loaded into the associated form. The HL7
messages are received by a Mirth Connect citemirth
server interface which has three channels configured:
one channel to receive the collected raw data, another
channel for signal processing and a channel intended
for internal use that sends the data to VCIntegrator
java backend webservices for storage. This way the
channels can be easily arranged to several possible
scenarios: either to ignore the signal processing and
just store raw data, store both incoming data in paral-
lel, or just forward the raw data to signal processing
servers. The data sent via webservices can be visu-
alized in VCIntegrator user inteface in the respective
form and visual components. The extraction of the
data from the HL7 messages into openEHR specifi-
cation is done, at the moment, by mapping each of
the HL7 data fields with the corresponding openEHR
archetype data elements, each with a unique identi-
fiable openEHR path. This is currently being done
inside Mirth Connect using java, but further work
should be put into a more automated solution. The
webservice layer provides a solution for both SOAP
and REST specifications. In order to be able to store
the data, in either specifications, using the accord-
ing client implementation, the client must first iden-
tify itself, then proceed with the patient EHR identi-
fication and set it as the current working EHR, iden-
tify the working openEHR Template and set the data
to record (create Composition) and finally submit the
Composition to the EHR. During these procedures the
audit details are being generated and then saved to-
gether with the data. Creating the openEHR template
for this work consisted in (1) identifying the clinical
statements recorded by the DSCollector, (2) develop
a structured representation of these statements, (3)
search for existing archetypes in the openEHR Clini-
cal Knowledge Manager (CKM) (openEHR commu-
nity, ) to represent the clinical statements, (4) create
the template. Since the structured representation of
the clinical statements and the archetypes were avail-
able, it was possible to create the template. The struc-
tured representation helped to create the framework
of the template, where the archetypes were arranged.
The development of the template was made on the
Ocean Template Designer software that allows com-
posing a set of archetypes into a template which is
also available for free download on the Ocean Infor-
matics website. The following openEHR arquetypes
were obtained from the openEHR Clinical Knowl-
edge Manager (CKM) and are used to represent the
clinical data, as a template, collected by the DSCol-
lector:
• openEHR-EHR-COMPOSITION.encounter.v1
• openEHR-EHR-CLUSTER.individual personal.v1
• openEHR-EHR-CLUSTER.person name.v1
• openEHR-EHR-OBSERVATION.blood pressure.v1
• openEHR-EHR-OBSERVATION.body weight.v1
• openEHR-EHR-OBSERVATION.height.v1
• openEHR-EHR-OBSERVATION.indirect oximetry.v1
• openEHR-EHR-EVALUATION.clinical synopsis.v1
4.3 DSCollector
The DSColector is an Android based application
that allows healthcare professionals to collect clinical
data, such as weight, height, blood pressure, etc; and
the phonocardiogram from any patient anywhere. The
most relevant feature of this application is the acquisi-
tion of the phonocardiogram in order to store it in the
electronic health record of the patient. In order to do
that, the DSCollector handles a bluetooth communi-
cation with an electronic stethoscope (in our case, the
Littmann 3200), and using a simple protocol, stores
HEALTHINF2015-InternationalConferenceonHealthInformatics
148
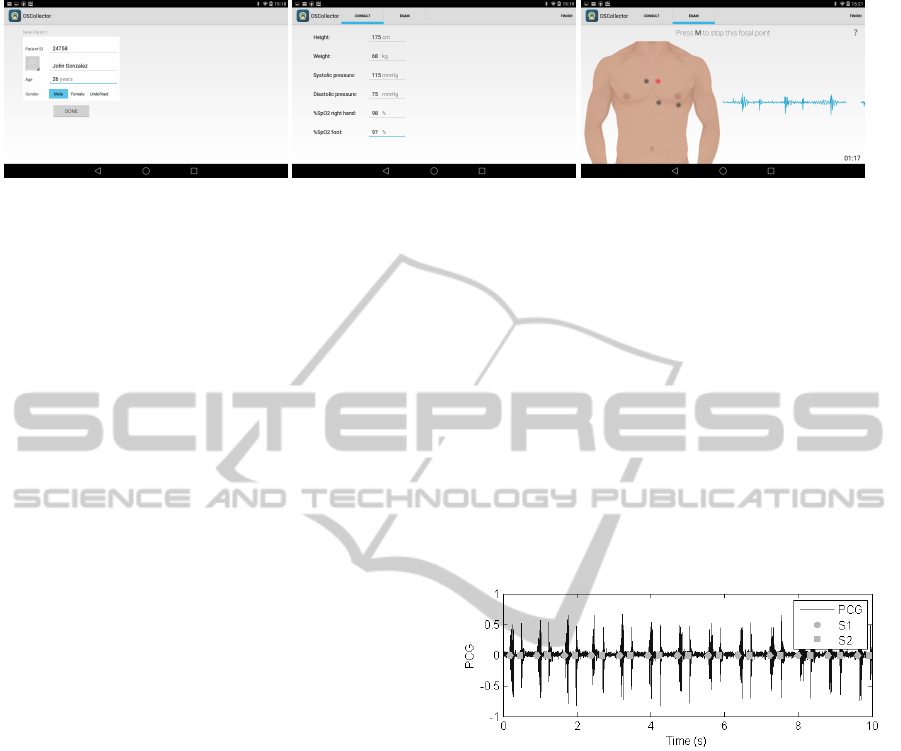
(a) (b) (c)
Figure 4: DSCollector screenshots of some of the acquisition stages during an appointment. 4(a) Patient creation layout. 4(b)
Clinical information gathered from the patient. 4(c) Acquisition of the pulmonary valve sound.
4 different sounds from the patient, being them the
4 most common heart focal points (pulmonary valve,
aortic valve, mitral valve and tricuspid valve).
As seen in figure 4 we can see the usual workflow
of this application. The healthcare professional needs
to first chose one electronic stethoscope to connect to,
and he can then proceed with the appointment, this
step is only required to do in the beginning of the ap-
plication and not for every patient. After that he can
chose to add a new patient or to create a new one, if
he chose to create one, he is requested to enter the pa-
tient identification number (that should be unique un-
der the national or private healthcare information sys-
tem), name, age and gender. After the patient creation
or after choosing an existence patient, the healthcare
professional is requested to enter all the clinical data
as he would retrieve in a standard appointment plus
the auscultation.
In the figure 4(c) it possible to see how this proce-
dure is done, the healthcare professional is requested
to collect 4 individual sounds from the patient, being
allowed to record more if required, from the same fo-
cal point.
All this data is then stored in the device and it will
be ready to be sent to any system that can receive HL7
messages (see section 4.1). From all the data gathered
with this device, only the sound files are not common
data to be sent in an electronic health record, but as
you can see in message 3 in the section 4.1, what we
do is to encode the sound to Base64, as it is done with
email messages, and send them inside the HL7 mes-
sage. All the HL7 handling is made with the help of
the HAPI parser an library for Java.
5 HEART SOUND SIGNAL
PROCESSING
As described earlier, after data collection, clinical
data are sent to the server for storage, and in parallel,
several signal processing tasks will be performed over
the collected PCG. The objective is to automatically
extract relevant signal features, as soon as the PCG
reaches the server, and produce a report with this in-
formation. This report will be later attached to the ob-
servation; if any alarming feature is detected, a warn-
ing may be sent to the clinician for earlier further eval-
uation of the patient. Several algorithms are already
implemented for PCG analysis, and features extrac-
tion (Ferreira et al., 2013; Castro et al., 2013; Pedrosa
et al., 2014; Oliveira et al., 2014; Castro et al., 2014):
auscultation spot segmentation; heart sound envelope;
heart cycle segmentation; signal quality; heart sounds
amplitude and duration; murmur detection; S2 com-
ponents’ analysis.
Figure 5: Example of a phonocardiogram collected in a real
clinical environment with heart sounds detection and classi-
fication (heart rate, S12 and S21 time intervals estimation).
Figure 5 presents an example of an auscultation
collected in a clinical scenario, with heart sounds de-
tection, and features extraction.
Figure 6 shows a proposal for data presentation to
the healthcare professional, with the results of the sig-
nal processing integrated in the EHR. A report with
these features may be generated, as well as a graph-
ical representation of the PCG, which may be very
helpful for clinical assessment and is not available for
standard acoustic auscultation.
6 DISCUSSION
In this paper we have proposed a framework for in-
tegrating the health data gathered by a clinician dur-
ing a patient evaluation either at home or in a primary
AProposaltoIncorporateDigitalAuscultationandItsProcessingintoanExistingElectronicHealthRecord
149
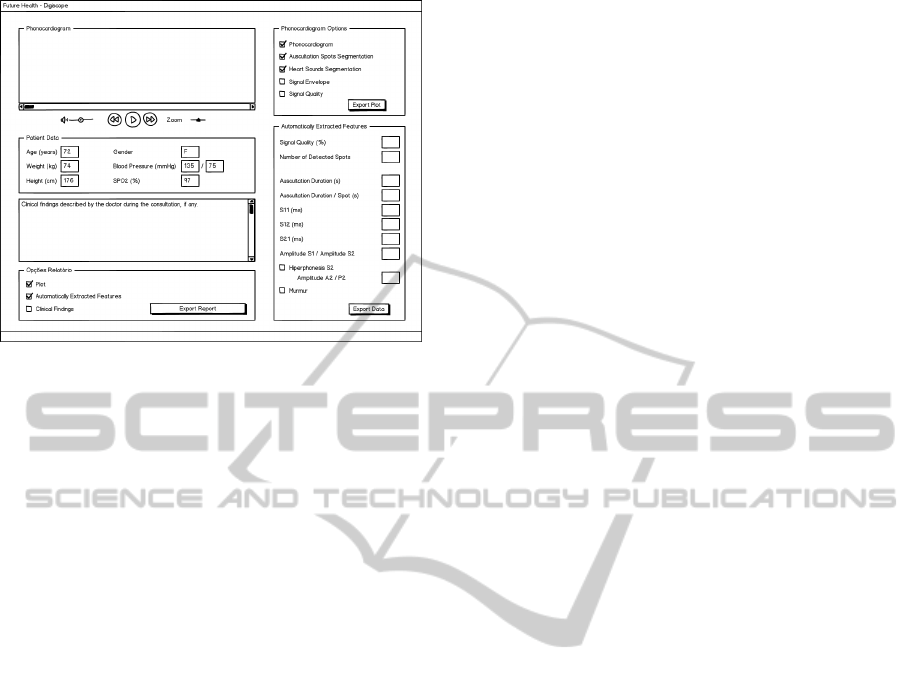
Figure 6: Proposal of data presentation to the healthcare
professional including the signal processing results.
care environment. We have focused on the ausculta-
tion signal since it is by far the less explored in both
literature and similar projects, given its challenging
hardware and gathering protocol requirements.
A full solution is proposed that includes not only
communication and storage protocols but also pro-
vides the framework with fundamental signal process-
ing and data visualization capabilities.
As part of the workplan of the ICT for Future
Health project, this framework will be implemented,
deployed and evaluated at the USF Nova Via primary
care center in Vila Nova de Gaia, Portugal, in early
2015.
ACKNOWLEDGEMENTS
This work was partially funded by the Fundac¸
˜
ao
para a Ci
ˆ
encia e Tecnologia (FCT, Portuguese Foun-
dation for Science and Technology) under the ref-
erence Heart Safe PTDC/EEI-PRO/2857/2012; and
Project I-CITY - ICT for Future Health/Faculdade de
Engenharia da Universidade do Porto, NORTE-07-
0124-FEDER-000068, funded by the Fundo Europeu
de Desenvolvimento Regional (FEDER) through the
Programa Operacional do Norte (ON2) and by na-
tional funds through FCT/MEC (PIDDAC).
REFERENCES
(2013). IHE - IT Infrastructure Tecnhical Framework. IHE,
volume 2a edition.
Beale, T. and Heard, S. (2008). OpenEHR architecture
overview.
Carapetis, J. R. et al. (2008). Evaluation of a screening pro-
tocol using auscultation and portable echocardiogra-
phy to detect asymptomatic rheumatic heart disease in
Tongan schoolchildren. Nature Clinical Practice Car-
diovascular Medicine, 5(7):411–417.
Castro, A., Mattos, S. S., and Coimbra, M. T. (2014). Non-
invasive blood pressure and the second heart sound
analysis. In Engineering in Medicine and Biology So-
ciety (EMBC).
Castro, A., Vinhoza, T., Mattos, S., and Coimbra, M.
(2013). Heart sound segmentation of pediatric aus-
cultations using wavelet analysis. In Engineering in
Medicine and Biology Society (EMBC).
EuropeanCommission (2013). Active and healthy ageing
for you & with you.
Ferreira, P., Vinhoza, T., Castro, A., Mourato, F., Tavares,
T., Mattos, S., Dutra, I., and Coimbra, M. (2013).
Knowledge on heart condition of children based
on demographic and physiological features. In
Computer-Based Medical Systems (CBMS), pages
314–319.
Health Level Seven International (2007). What is HL7?
Oliveira, J., Castro, A., and Coimbra, M. T. (2014). Ex-
ploring embedding matrices and the entropy gradient
for the segmentation of heart sounds in real noisy en-
vironments. In Engineering in Medicine and Biology
Society (EMBC).
openEHR (2013). What is openEHR.
openEHR community. Clinical knowledge manager.
Pedrosa, J., Castro, A., and Vinhoza, T. (2014). Auto-
matic heart sound segmentation and murmur detec-
tion inpediatric phonocardiograms. In Engineering in
Medicine and Biology Society (EMBC).
Pereira, D., Gomes, P., Mota, l., Costa, E., Cruz-Correia,
R., and Coimbra, M. (2013). Combining a tablet and
an electronic stethoscope to create a new interaction
paradigm for teaching cardiac auscultation. In HCI In-
ternational 2013, volume 374 of Communications in
Computer and Information Science, pages 206–209.
Rechel, B., Grundy, E., Robine, J.-M., Cylus, J., Macken-
bach, J. P., Knai, C., and McKee, M. (2013). Ageing
in the european union. The Lancet, 381(9874):1312–
1322.
SCPSDC (2013). Ready for ageing? (Report of Ses-
sion 201213 Select Committee on Public Service and
Demographic Change, e Authority of the House of
Lords).
VirtualCare (2014). Vcintegrator.
WHO (2011). Global health and aging.
WHO (2012). Good health adds life to years.
WHO (2014). Health topics, ageing.
HEALTHINF2015-InternationalConferenceonHealthInformatics
150
