
Towards Distributed Sociotechnical System for Reporting Critical
Laboratory Results
Msury Mahunnah
1
, Annike Koorts
2
and Kuldar Taveter
1
1
Department of Informatics, Tallinn University of Technology, Ehitajate tee 5, Tallinn, Estonia
2
Clinical Chemistry and Hematology Laboratory, North Estonia Medical Center, J. Sütiste tee 19, Tallinn, Estonia
Keywords: Critical Laboratory Results, Agent Oriented Modelling, Sociotechnical System.
Abstract: In healthcare domain, reporting of laboratory results by biomedical scientists to caregivers is a common
practice. Many healthcare centres follow different kind of guidelines for reporting laboratory results for the
purpose of improving the process. In this paper, we first analyze current procedure for reporting Critical
Laboratory Results (CLRs) followed by North Estonia Medical Centre (NEMC) located in Estonia. We then
identify weaknesses and argue that reporting of CLRs requires advanced mechanisms because a patient with
CLRs is always in need of a prompt treatment or decisions on medication from the appropriate caregiver.
We then critically analyze a problem of reporting CLRs to caregivers with the aim to support this process by
appropriate sociotechnical system. We do this by using the approach of agent-oriented modelling. The
analysis is followed by models for designing a distributed sociotechnical system for managing CLRs.
1 INTRODUCTION
In today’s world, we interact with an ever-increasing
array of mobile devices such as smart phones and
personal digital assistants. Such devices are
changing the way people in today’s society behave
and communicate (Hellström and Tröften, 2010).
The abundance of mobile technologies has enabled a
promising direction in today’s healthcare. In the
healthcare domain, monitoring and reporting of
laboratory test results to an appropriate caregiver
(physician, nurse, midwife, etc.) is a common
practice. The laboratory test results have two main
categories – Normal Laboratory Results (NRLs) and
Critical Laboratory Results (CLRs) (Kuperman et al.
1998). NRLs represent the medical condition of a
patient that does not require a prompt response from
a caregiver while CLRs are any values or their
interpretations for which delays in reporting can
result in serious adverse outcomes for patients. Thus,
patients with CLRs need prompt treatment or
decisions on medication by the appropriate caregiver
(Tate et al., 1995); (Kuperman et al., 1996); (Hanna
et al. 2005).
The advancement of mobile technologies
provides opportunities for designing intelligent
distributed systems that support reporting of CLRs
to appropriate caregivers. Because of the distributed
nature of the healthcare domain, we are interested in
designing intelligent systems that support each
healthcare professional according to the role played
by her/him at a given time in a given location. Such
systems can be termed as distributed sociotechnical
systems. Sterling and Taveter (2009) have suggested
an approach called Agent Oriented Modelling
(AOM) for designing distributed sociotechnical
systems made up of humans and their intelligent
digital assistants, which are respectively termed as
human agents and man-made agents. These agents
should be able to sense the environment via, for
example, medical sensors, reason, act and socialize
with one another when achieving objectives of the
sociotechnical system.
The contribution of this paper is twofold: from
the medical perspective, we have critically analyzed
different mechanisms for reporting CLRs from
existing literatures together with the actual practice
carried out at the North Estonia Medical Centre
(NEMC). Then, we recommended a combined usage
of specialty, medical knowledge, and availability
information of the caregiver, which, to the best of
our knowledge, is a new approach for choosing an
appropriate caregiver for receiving CLRs. From the
technological perspective, we presented the analysis
and design models of the intelligent distributed
sociotechnical system consisting of human agents
269
Mahunnah M., Koorts A. and Taveter K..
Towards Distributed Sociotechnical System for Reporting Critical Laboratory Results.
DOI: 10.5220/0004329102690276
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2013), pages 269-276
ISBN: 978-989-8565-37-2
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)

and man-made agents by using the previous-
mentioned AOM approach for designing
sociotechnical systems (Sterling and Taveter, 2009).
The rest of this article is organized as follows.
Section 2 presents the problem of efficiently
handling of CLRs experienced by NEMC. The
models for the analysis of the problem domain are
then discussed in Section 3 with the help of AOM.
Likewise by means of AOM, Section 4 describes the
design of a sociotechnical system for reporting
CLRs to appropriate caregivers. Section 5 discusses
related work and Section 6 draws the conclusions
and presents the future work.
2 PROBLEM DOMAIN
Among the objectives of any healthcare centre is to
provide patients with a better quality care. In
achieving its objectives, the exchange of medical
information between caregivers, who are naturally
distributed and have different responsibilities,
should be handled efficiently. In this paper we focus
on the actual procedure followed by North Estonian
Medical Centre (NEMC) laboratory during the
process of reporting CLRs to an appropriate
caregiver. NEMC is the foremost Estonian hospital
with main buildings situated in different locations of
Tallinn and Kose counties. The hospital has 3626
employees, including 590 doctors, 1352 of nursing
staff, and 862 other caregivers. At any given time,
there are over 100 resident physicians in the
hospital.
The NEMC laboratory has written guidelines for
reporting laboratory results. These guidelines
describe procedures for verification of results and
reporting them to appropriate caregivers. The
Laboratory Information System (LIS) uses Process
Systems Manager (PSM) middleware software for
receiving orders from the Hospital Information
System (HIS) and sending them to the medical
equipments in a laboratory for the purpose of
conducting laboratory tests. When the tests are
complete, the PSM receives results from the medical
laboratory, auto-verifies the results, and sends them
to the HIS, where they are stored in the appropriate
patient record. Auto-verification means that the PSM
system checks the results against various pre-
specified criteria and proactively decides how to
proceed with the results. The results that comply to
the pre-specified criteria are automatically released
and stored in the patient record in the HIS, while
other results are blocked to be reviewed by a
biomedical scientist.
In the PSM critical values are described for
several laboratory tests, such as S-P, fS-Gluc, fS-K,
fS-Ca, fS-Mg, fS-Na, B-Hct, B-Hgb, B-WBC, B-
RBC, and P-INR. When CLRs are detected, the
system blocks them and marks by red background. A
biomedical scientist then reviews all blocked results.
For each of the identified CLRs, the corresponding
laboratory tests will be repeated by using a different
medical equipment to check for analytical errors. If
the outcomes of the repeated laboratory tests are
detected as CLRs for the second time, a biomedical
scientist will call to inform the physician who
ordered the tests. The NEMC laboratory guidelines
require the laboratory staff to report the detected
CLRs within 30 minutes to the physician who
ordered the tests. If the physician who ordered the
tests is unavailable, the laboratory staff is supposed
to report to the departmental nurse. The laboratory
staff will try three times and if upon all three times
neither physician nor departmental nurse is
available, the laboratory staff will stop trying to
contact them and the CLRs will be transmitted
electronically as NRLs to the HIS. In case of either
successful or unsuccessful attempt to reach the
physician or the departmental nurse by phone, the
guidelines require the laboratory staff to record the
reported CLRs on the paper-based registration form.
We have identified several weaknesses in the
current procedure of reporting CLRs at the NEMC
laboratory. Firstly, the procedure of reporting CLRs
involves many people. This leads into two major
problems: (1) high risk of human errors (2) delay in
reporting CLRs. For instance, due to a human error,
in some cases the order form for laboratory results
does not contain the phone number of the
corresponding physician, which causes a delay in
reporting CLRs detected. By automating the
reporting process by means of a new information
system, data integrity will be ensured while the
integration of the new information system with the
existing laboratory systems will reduce human errors
as well as the time required to report CLRs.
Secondly, when the physician who ordered the
laboratory tests is unreachable, the laboratory
guidelines suggest the laboratory staff to make a
phone call to the departmental nurse who will then
try to find another appropriate physician. If the
departmental nurse is also unreachable, the CLRs
will be sent to HIS as NLRs. We highly recommend
improving this procedure for reporting CLRs
because the current practice allows significant risks
for human lives, which can be avoided. We suggest
to improve the current system by introducing a new
information system that takes advantage of the
HEALTHINF2013-InternationalConferenceonHealthInformatics
270

advancement in mobile technologies, such as the use
of location sensors that can accurately identifythe
appropriate physicians. We propose to design a new
information system as a sociotechnical system – a
software intensive system that has defined
operational processes followed by human operators
and which operates within an organization (Sterling
and Taveter, 2009). In a sociotechnical system
envisioned by us, humans acting in specific roles in
healthcare organizations, such as laboratory
technicians, biomedical scientists, and physicians,
are supported by software agents. The most essential
feature of the proposed sociotechnical system lies in
the software agents’ behaviors to be described in
Section IV. The behaviours of agents are designed
and implemented by applying Artificial Intelligence
(AI) reasoning techniques such as abduction and
deduction, which enables a software agent to act
proactively when choosing an appropriate physician
for receiving CLRs. As a result, if the physician to
receive a report on CLRs is not available, the agents
in the system will proactively identify and suggest
other most appropriate physicians according to their
availability, location, medical knowledge, and
specialty. The last observed weakness is the use of
paper-based forms for the registration of CLRs.
Paper-based forms should be replaced by
automatically generated log files that include
information about: (1) reported CLRs (2) CLRs
received by caregivers (3) delivery time (4)
acknowledgment time. This will also provide an
efficient method for quality control.
3 DOMAIN ANALYSIS
As was already mentioned at the end of Section II,
the envisioned system is a sociotechnical system
where humans playing certain roles are supported by
appropriate intelligent digital assistants, which may
also be termed as agents. Analysis of such systems
should follow an appropriate methodology due to its
complexity. There are various Agent Oriented
Software Engineering (AOSE) methodologies
available, such as Tropos (Bresciani et al., 2004),
MaSE (Wood and DeLoach, 2001), and Prometheus
(Padgham and Winikoff, 2003). However, they all
put the emphasis on designing systems consisting of
software agents rather than sociotechnical systems,
where software agents support humans. Sterling and
Taveter (2009) proposed a suitable approach that
includes features similar to AOSE methodologies
but is geared towards designing socio-technical
systems consisting of humans and software agents,
which are respectively termed as human agents and
man-made agents (Sterling and Taveter, 2009). A
sociotechnical system proposed in this paper
consists of healthcare professionals and intelligent
software agents that assist them with the aim of
improving the reporting of CLRs. We next give a
brief overview of agent-oriented modelling. This is
followed by the description of how agent-oriented
modelling has been applied to designing the socio-
technical system for reporting CLRs.
In the centre of AOM lies the viewpoint
framework represented as Table 1. The viewpoint
framework is the conceptual framework that consists
of a matrix with three rows representing different
abstraction layers – analysis of the problem domain,
design, and implementation – and three columns
representing the viewpoint aspects of interaction,
information, and behaviour (Sterling and Taveter,
2009). Each cell in this matrix represents a specific
viewpoint by mapping one or more model type(s) of
AOM. This paper presents the analysis and design of
sociotechnical system by using two analysis models
and three design models.
Table 1: The model types of Agent-Oriented Modelling.
Viewpoint aspect
Abstraction
layer
Interaction Information Behaviour
Analysis
Role models
and
organisation
model
Domain
model
Goal models
and
motivational
scenarios
Design
Agent
models,
acquaintance
models, and
interaction
models
Knowledge
models
Scenarios
and
behaviour
models
Platform-
specific
design
Platform-specific design models
We start by overviewing goal models. Generally,
goal model serves as a container for three main
components: functional goals commonly referred as
goals, quality goals, and roles. Similarly to other
kinds of systems, a socio-technical system is
described by functional requirements as well as non-
functional requirements, which are captured in a
goal model by goals and quality goals, respectively.
Goals and quality goals can be further decomposed
into sub-goals and sub-quality goals, where each
sub-goal represents some aspect of achieving its
parent goal. Goal models serve as communication
mediums between technical and non-technical
stakeholders and provide both with a better
understanding of the problem domain.
TowardsDistributedSociotechnicalSystemforReportingCriticalLaboratoryResults
271
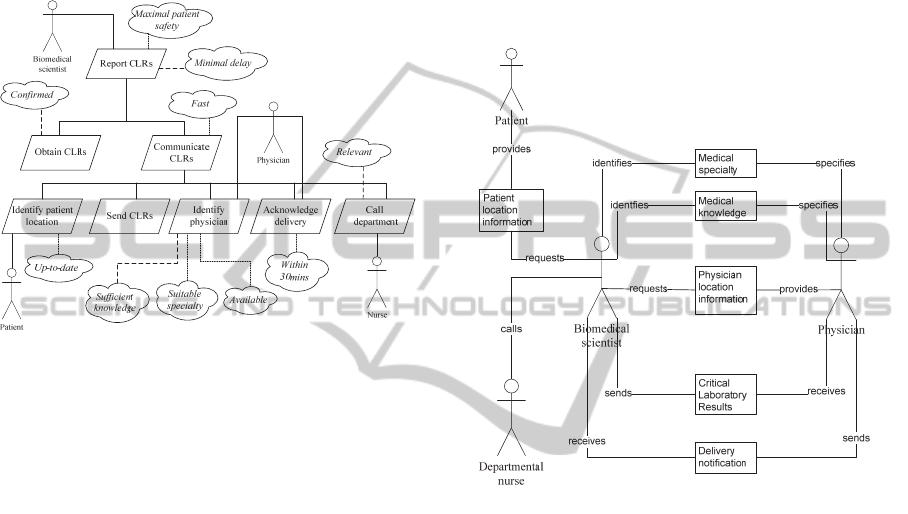
Figure 1 describes the goal model for managing
CLRs. The top level goal represents the purpose of
the sociotechnical system to be designed, which is to
report CLRs. This goal is characterized by the
quality goals of maximal patient safety and minimal
delay. The latter means the process of reporting
CLRs should take very little time, while the former
targets at improving patient safety.
Figure 1: Goal model for the problem analysis.
As seen in Figure 1, the highest-level goal has been
decomposed into two sub-goals – obtain CLRs and
communicate CLRs. The latter has the quality goal
“Fast” to make note of the non-functional
requirement that the whole process of
communicating CLRs should take as little time as
possible. How to ensure the speed is a design issue,
which is not considered during the analysis phase.
The “Communicate CLRs” goal is then further
decomposed into five sub-goals: identify patient
location, send CLRs, identify physician,
acknowledge delivery, and call department. The
remaining quality goals are attached to the lowest
level sub-goals as represented in Figure 1. The
figure also includes the roles – Biomedical scientist,
Patient, Physician, and Nurse – that are required for
achieving the functional goals to which they are
attached and their subgoals.
During the process of analyzing a problem
domain, the knowledge to be handled by the system
is captured by domain model. Domain model
represents the environment(s) in which the system is
to be situated, the types of resources produced and
stored by them, as well as the existing relationship
between the roles, environment(s), and resources.
Figure 2 presents a domain model that contains six
information resources, which are produced and used
in the healthcare environment to facilitate
interactions between agents performing the roles of
Biomedical scientist, Physician, Nurse, and Patient,
in order to achieve the goals of the sociotechnical
system. For example, in Figure 2 the information
resource “Physician location information” is
produced by the role Physician and is directly
utilized by the role Biomedical scientist for the
purpose of achieving the overall goal of the
sociotechnical system to report CLRs with maximal
patient safety and minimal delay.
Figure 2: Domain model for analysing knowledge handled
by the sociotechnical system.
4 DESIGN MODELS FOR THE
SOCIOTECHNICAL SYSTEM
In this section, we present design models of a
distributed sociotechnical system for the problem
domain that was analyzed in Section 3. The design
of a sociotechnical system is guided by AOM model
types under the three viewpoint aspects of platform-
independent design – interaction, information and
behaviour – described in Table 1. As introduced in
Section 2, the sociotechnical system to be designed
consists of both man-made and human agents. The
latter are people such as physician, biomedical
scientist, and nurse found in any healthcare
institution, while man-made agents are intelligent
digital assistants implemented in software that can
run on hand-held devices for the purpose of
executing some or all of the responsibilities of the
roles of the sociotechnical system. An intelligent
HEALTHINF2013-InternationalConferenceonHealthInformatics
272
digital assistant normally interacts with the
corresponding human agent. For example, the
intelligent digital assistant of a physician interacts
with the physician when performing the Physician
role in the sociotechnical system. The decision on
mapping system roles to human agents or/and man-
made agents is documented by agent models, while
the design of interaction pathways between agents of
the decided types is captured by the agent
acquaintance model.
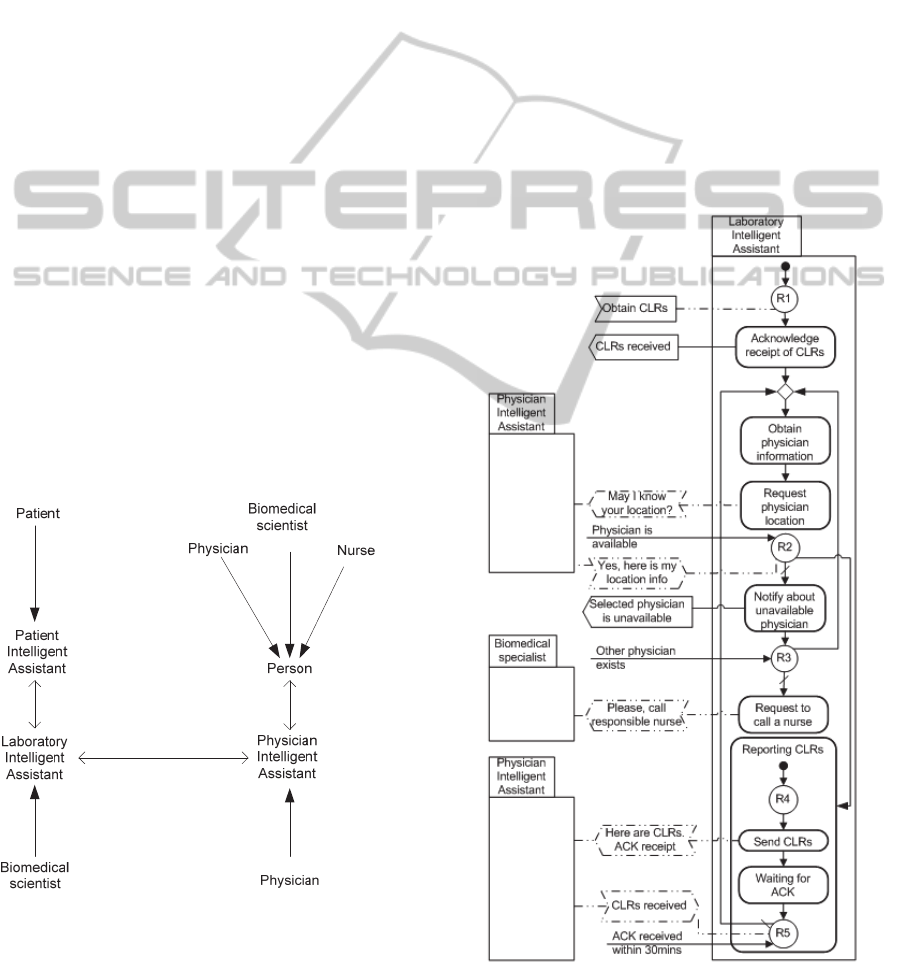
Figure 3 represents a merged agent model and
the agent acquaintance model. According to the
model depicted in Figure 3, some responsibilities of
the roles Biomedical scientist and Physician of the
sociotechnical system are carried out by man-made
agents of the type Laboratory Intelligent Assistant
and Physician Intelligent Assistant, respectively,
while the responsibilities of the patient role are
executed by man-made agent of the type Patient
Intelligent Assistant. The responsibilities of the role
Patient that the patient intelligent assistant has to
fulfil include identifying the patient location and
communicating the location information to the
laboratory intelligent assistant. The remaining
responsibilities of the system roles are then carried
out by human agents playing the roles of Physician,
Biomedical scientist, and Nurse. With the
combination of agent models and agent acquaintance
model, we have decided the backbone of the socio-
technical system. Figure 3 also represents interaction
pathways between decided agent types.
Figure 3: A merged agent and acquaintance model.
In order for an agent to autonomously and
intelligently respond to events originating in its
environment or in other agents, a set of rules is
normally created, presenting the agent’s behaviours.
Together with the information about specialty,
medical knowledge and location of physicians and
other healthcare professionals, which is stored in the
sociotechnical system, behaviour model for each of
involved man-made agents needs to be designed.
The behaviour model of agents of the type
Laboratory Intelligent Assistant contains rules that
provide agents with capabilities to proactively
suggest appropriate choice of an alternative
physician. For instance, in cases when the
responsible physician leaves the healthcare premises
or the responsible physician is located at a
significant distance from the patient of interest, this
information is instantly updated in the system. After
completion of the updating process, the AI reasoning
techniques of abduction (Kakas et al., 1992) and
and/or deduction may be used to proactively assign
Figure 4: Agent behaviour model of a laboratory
intelligent assistant.
TowardsDistributedSociotechnicalSystemforReportingCriticalLaboratoryResults
273

the responsibilities of the responsible physician to
another physician who is most appropriate at the
given time without any intervention by humans. In
some rare cases when the laboratory intelligent
assistant is not able to suggest an appropriate
physician, it proactively alerts a biomedical scientist
to call a departmental nurse, following the current
procedure of reporting CLRs.
Behaviour models enable both proactive and
reactive behaviours of agents in the sociotechnical
system to be captured. Figure 4 represents the
behaviour model of an agent of the type Laboratory
Intelligent Assistant. Figure 4 models a proactive
behaviour of a laboratory intelligent assistant, where
a message of the type “May I know your location?”
is sent to the appropriate physician intelligent
assistant. Checking the availability of another
appropriate physician is modelled with the help of
rule R3. This rule R3 is triggered by the
unavailability of the responsible physician, which is
computed from the values of knowledge items
embedded in the database of the sociotechnical
system. As an example of reactive behaviour, an
activity of type “Acknowledge receipt of CLRs” in
figure 4 is triggered by rule R1 after obtaining
detected and confirmed CLRs from PSM. The
corresponding event “Obtain CLRs” is modelled as a
non-action event originating in the environment.
5 RELATED WORK
Over many years different kinds of studies and
researches across the world have been conducted in
the area of managing CLRs (Shabot et al., 1990);
(Tate et al., 1995); (Kuperman et al., 1996);
(Iordache et al., 2001); (Poon et al., 2002); (Park et
al., 2008); (Guidi et al., 2009); (Bromuri et al.,
2011). Among the objectives of this paper is
analyzing the procedures suggested by different
studies for reporting CLRs to caregivers. In the
study conducted at Taipei Veterans’ General
Hospital (Chen et al., 2002), physicians received
CLRs, while the study at the LDH hospital (Tate et
al., 1995) suggested and used nurses as appropriate
caregivers to receive CLRs. At Brigham and
Women's Hospital (Kuperman et al., 1996), the list
of appropriate staff to receive CLRs included
telephone operators who have little medical
knowledge but who are always available. When
CLRs were received by telephone operators, they
manually identified appropriate caregiver according
to their knowledge and thereafter made telephone
calls to inform about the CLRs. When comparing
these three studies (Tate et al., 1995); (Kuperman et
al., 1996); (Chen et al., 2002) and considering
advanced mobile technologies that facilitate location
identification, real-time interactions, and advanced
ways of knowledge management, we recommend
physicians as appropriate choice of caregivers for
receiving CLRs due to the need of prompt treatment
or decision on medication.
Although we recommended physicians as
appropriate choice of caregivers for receiving CLRs,
the major challenge here is working out selection
mechanisms for identifying the physician. We have
suggested three main factors that are expected to
lead to a better choice of a physician to receive
CLRs. Firstly a physician should have sufficient
medical knowledge. This is due to noticeable
knowledge variations between different levels of a
physician, from interns to experts. The second
feature is medical specialty. There are many
specialties in a healthcare domain, such as
haematology, gynaecology, and paediatrics. This
suggests that CLRs detected from pregnant woman
are more meaningful and can be efficiently utilized
when reported to gynaecologists rather than other
types of specialized physicians. The third feature is
the availability of a physician. The availability
feature was also discussed in the study conducted by
Dighe et al. (2006). In that study, the response time
of a physician concerning Intensive Care Unit (ICU)
patients with CLRs was much lower than that for
non-ICU patients. This was because the availability
of a physician is guaranteed for ICU patients, while
the case is different for non-ICU patients. Following
this observation, Dighe et al. (2006) recommended
more research work on the ways for reducing
response time to CLRs for non-ICU patients.
6 CONCLUSIONS AND FUTURE
WORK
We have addressed the ways of improving the
mechanisms for reporting CLRs to appropriate
caregivers after being detected in the medical
laboratory. The distributed nature of the problem
domain together with the need of designing software
systems that would be intertwined with social
processes motivated the choice of AOM (Sterling
and Taveter, 2009) as a suitable approach for the
analysis of the problem domain and design of an
appropriate sociotechnical system. We also
recommended physicians as the best choice among
caregivers for receiving CLRs because of the need
HEALTHINF2013-InternationalConferenceonHealthInformatics
274

for prompt treatment or decision on medication. In
this article, three main features for choosing
appropriate physicians were suggested, discussed,
and presented as quality goals in the goal model –
specialty, medical knowledge, and availability. The
problem domain was further analysed by means of
the domain model of AOM. The domain model was
used to capture the knowledge handled by the
sociotechnical system.
In Section 3, we conducted the analysis of the
problem domain by means of AOM analysis models.
In Section 4, the design of the sociotechnical system
was presented and related to the outcomes of the
domain analysis discussed in Section 3. In particular,
an agent and acquaintance model was used for
mapping the domain roles to human agents as well
as to the types of man-made agents and for
identifying interaction pathways between the agents.
This was followed by discussing the modelling of
proactive and reactive behaviours of agents, which
we illustrated by an agent behaviour model of the
laboratory intelligent assistant.
With the ultimate goal of introducing a
distributed sociotechnical system for reporting
CLRs, we have categorized the future work into
three main phases. Firstly, we will improve the
behaviour model presented in Section 4 by applying
abduction (Kakas et al., 1992) and/or deduction AI
reasoning techniques that optimize information
about specialty, medical knowledge, and availability
for choosing an appropriate physician. Secondly, the
prototype of a sociotechnical system consisting of
intelligent digital assistants suggested in this paper
will be developed. Finally, the issues related to the
interoperability of healthcare systems will be
considered due to the need of integrating the
proposed sociotechnical system with the existing
healthcare systems.
ACKNOWLEDGEMENTS
This research was supported by the Estonian IT
Academy program.
REFERENCES
Bresciani, P., Perini, A., Giorgini, P., Giunchiglia, F. and
Mylopoulos, J., 2004. Tropos: An agent-oriented
software development methodology. Autonomous
Agents and Multi-Agent Systems, 8(3), pp.203–236.
Bromuri, S., Schumacher, M. I., Stathis, K. and Ruiz, J.,
2011. Monitoring gestational diabetes mellitus with
cognitive agents and agent environments. In
Proceedings of the 2011 IEEE/WIC/ACM
International Conferences on Web Intelligence and
Intelligent Agent Technology-Volume 02. pp. 409–
414.
Chen, H. T., Ma, W. C. & others, 2002. Design and
implementation of a real-time clinical alerting system
for intensive care unit. In Proceedings of the AMIA
Symposium. p. 131.
Dighe, A. S., Rao, A., Coakley, A. B., Lewandrowski, K.
B., 2006. Analysis of laboratory critical value
reporting at a large academic medical center.
American journal of clinical pathology, 125(5),
pp.758–764.
Guidi, G. C., Poli, G., Bassi, A., Giobelli, L., Benetollo, P.
P. and Lippi, G., 2009. Development and
implementation of an automatic system for
verification, validation and delivery of laboratory test
results. Clinical Chemistry and Laboratory Medicine,
47(11), pp.1355–1360.
Hanna, D., Griswold, P., Leape, L. L., Bates, D. W., 2005.
Communicating critical test results: safe practice
recommendations. Joint Commission Journal on
Quality and Patient Safety, 31(2), pp.68–80.
Hellström, J. & Tröften, P. E., 2010. The innovative use of
mobile applications in East Africa, Swedish
international development cooperation agency (Sida).
Iordache, S. D., Orso, D. and Zelingher, J., 2001. A
comprehensive computerized critical laboratory results
alerting system for ambulatory and hospitalized
patients. Studies in health technology and informatics,
(1), pp.469–473
Kakas, A. C., Kowalski, R. A. and Toni, F., 1992.
“Abductive logic programming,” J. Log. Comput., vol.
2, no. 6, pp. 719–770,1992.
Kuperman, G. J., Teich, J.M., Bates, D. W., Hiltz, F.L.,
Hurley, J. M., Lee, R. Y., Paterno, M. D., 1996.
Detecting alerts, notifying the physician, and offering
action items: a comprehensive alerting system. In
Proceedings of the AMIA Annual Fall Symposium. p.
704.
Kuperman, G. J., Boyle, D., Jha, A., Rittenberg, E.,
Ma'Luf, N., Tanasijevic, M. J., Teich, J. M.,
Winkelman, J., Bates, D.W., 1998. How promptly are
inpatients treated for critical laboratory results?, Am
Med Inform Assoc.
North Estonia Medical Centre, Information. Available at:
http://www.regionaalhaigla.ee/?op=body&id=180
[Accessed October 23, 2012].
Padgham, L. & Winikoff, M., 2003. Prometheus: a
methodology for developing intelligent agents. Agent-
oriented software engineering III, pp.174–185.
Park, H. I., Min, W. K., Lee, W., Park, H., Park, C. J., Chi,
H. S. and Chun. S., 2008. Evaluating the short
message service alerting system for critical value
notification via PDA telephones. Annals of Clinical &
TowardsDistributedSociotechnicalSystemforReportingCriticalLaboratoryResults
275

Laboratory Science, 38(2), pp.149–156.
Poon, E. G., Kuperman, G. J., Fiskio, J., Bates, D. W.,
2002. Real-time notification of laboratory data
requested by users through alphanumeric pagers, Am
Med Inform Assoc.
Shabot, M. M., LoBue, M., Leyerle, B. J., Dubin, S. B.,
1990. Decision support alerts for clinical laboratory
and blood gas data. Journal of Clinical Monitoring and
Computing, 7(1), 27–31.
Sterling, L. & Taveter, K., 2009. The art of agent-oriented
modeling, Mit Pr.
Tate, K. E., Gardner, R. M. & Scherting, K., 1995. Nurses,
pagers, and patient-specific criteria: three keys to
improved critical value reporting. In Proceedings of
the Annual Symposium on Computer Application in
Medical Care. p. 164.
Wood, M. & DeLoach, S., 2001. An overview of the
multiagent systems engineering methodology. In
Agent-Oriented Software Engineering. pp. 1–53.
HEALTHINF2013-InternationalConferenceonHealthInformatics
276
