
Study and Evaluation of Palmar Blood Volume Pulse for
Heart Rate Monitoring in a Multimodal Framework
Hugo Silva
1,2
, Joana Sousa
1,2
and Hugo Gamboa
1,3
1
PLUX - Wireless Biosignals, S.A., Av. 5 de Outubro, n. 70 - 6, 1050-059 Lisbon, Portugal
2
IT - Instituto Superior T
´
ecnico, Av. Rovisco Pais, n. 1, 1049-001 Lisboa, Portugal
3
CEFITEC - Faculdade de Ci
ˆ
encias e Tecnologia, Universidade Nova de Lisboa,
2829-516 Caparica, Portugal
Abstract. Within the field of biosignal acquisition and processing, there is a
growing need for combining multiple modalities. Clinical psychology is an area
where this is often the case, and one example are the studies where heart rate
and electrodermal activity need to be acquired simultaneously. Both of these pa-
rameters are typically measured in distinct anatomical regions (the former at the
chest, and the later at the hand level), which raises wearability issues as in some
cases two independent devices are used; finger clip sensors already enable heart
rate measurement at the hand level, however they can be limiting for free living
and quality of life activities. In this paper we perform a study and evaluation of
an experimental blood volume pulse sensor, to assess the feasibility of measuring
the heart rate at the hand palms, and thus enabling the design of more convenient
systems for multimodal data acquisition.
1 Introduction
Blood Volume Pulse (BVP) sensors are a commonly used method for assessing the
cardiovascular activity at the arterial level [1]. Their operating principle is based on
photoplethysmography, that is, by externally applying a light source in the visible or
invisible wavelengths to the tissues, and measuring the amount of light that reaches
a photodetector [2]. The detector can be positioned to measure either by reflection or
transmission; as the heart pumps blood through the arteries, and subsequently through
the peripheral vessels, the translucency of the vessels changes due to the increased
blood volume, modifying the way that the emitted light is reflected or transmitted to the
photodetector [3]. The typical output of the sensor is then a signal where each cardiac
cycle is expressed as a pulse wave (Figure 1(a)).
In this paper we present a study and evaluation of a palmar BVP sensor for heart rate
measurement, designed to be integrated in multimodal systems for biosignal acquisition
at the hand level. The studied arrangement further expands the current state-of-the-
art in the field by improving wearability aspects. Unlike existing systems, taking into
account that the sensor is placed at the hand palm, no additional volume is moved
on to the fingers, enabling the wearer to make normal use of the hand. Experimental
results have shown a good correlation between the measurements taken at the hand
palm and at the fingertip, validating the palmar placement as an adequate alternative to
Silva H., Sousa J. and Gamboa H..
Study and Evaluation of Palmar Blood Volume Pulse for Heart Rate Monitoring in a Multimodal Framework.
DOI: 10.5220/0003884900350040
In Proceedings of the 2nd International Workshop on Computing Paradigms for Mental Health (MindCare-2012), pages 35-40
ISBN: 978-989-8425-92-8
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)
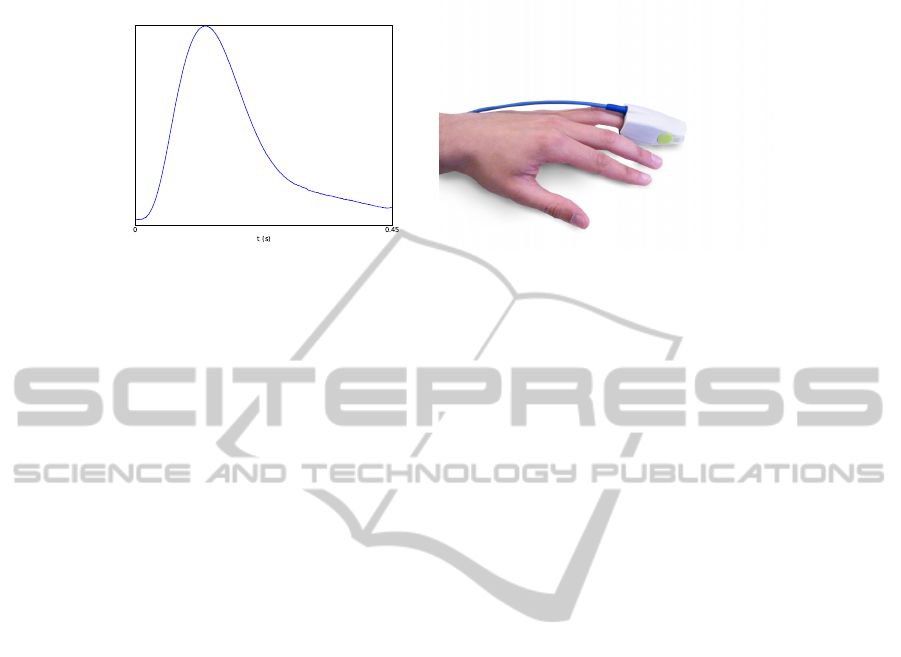
(a) Pulse wave signal (b) Common sensor placement
Fig. 1. Example of a Blood Volume Pulse (BVP) signal and typical fingertip sensor.
standard approaches. The remainder of the paper describes the motivation for our work
in Section 2, presents the materials and methods in Section 3, and highlights the results
and conclusions in Sections 4 and 5 respectively.
2 Motivation
The heart rate has became a widespread biosignal measurement for self-management
and assessment, with extensive application in a variety of contexts such as clinical diag-
nosis, sports activities, and affective computing, among others [4–6]. Chest straps have
risen as a standard for unobtrusive data acquisition, and although these form factors are
concealed by the clothing and thus, discrete for regular use, a growing number of ap-
plications require the measurement of multiple parameters simultaneously. This is the
case of clinical psychology [7, 8], where besides the heart rate and derived information,
electrodermal activity is also used as a psychological or physiological arousal indica-
tor. As electrodermal activity is more noticeable at the hand palms and fingers, several
usability difficulties arise when both parameters need to be measured simultaneously,
since two independent devices are generally required.
Due to the close relation between BVP signals and the cardiac activity, the heart rate
is one of the parameters generally extracted from the collected data. Furthermore, BVP
sensors can be applied to any place in the body irrigated by blood vessels, particularly in
peripheral areas, making it an appealing alternative to the more intrusive cheat mounted
apparatuses. The most common placement is at the fingertip [9] (Figure 1(b)); however,
for long term or continuous use, this anatomic placement limits the regular activities
of it’s wearer as the fingers play a fundamental role in most daily tasks. Furthermore,
for patients with schizophrenia, psychosis, autism, among other, to place biomedical
sensors at the finger is hard to the medical staff, because these patients have high move-
ments and tendency to remove the finger clip. Thus, a BVP glove can overcome some
of these issues, since the patient wears a glove, which is hard to remove and it as not
being subject to the fingers movements.
From BVP signal, Heart Rate (HR) and RR intervals can be extracted, allowing the
Heart Rate Variability (HRV) analysis in terms of time and frequency domains. HRV is
36

widely related to the mental diseases, since it can provide information about the emo-
tional state of the patient, by its correlation with the automatic heart modulation being
a powerful tool for clinical use. For example, the HRV spectral analysis reveals that
the vagal activity is the major contribution to the high frequencies component. Fur-
thermore, it is also argued that the low frequency (LF) and high frequency (HF) ratio
reflects the sympathovagal balance or the sympathetic modulation. These parameters
are very important since some authors defend that there is a significant increase of LF
band and significant increment of the HR for panic disorders patients and significant
lower values of R-R intervals and HF peak of spectral analysis in depressive patients
than in the health people.
In addition to the HR and HRV analysis, the BVP sensor can be updated with other
emitter, becomes in an oximetry sensor, which allows to measure both HR and oximetry
parameters. BVP sensor can also be combined with an ECG sensor and through the
Pulse Transient Time (PPT) technique allowing to measure the blood pressure.
Thus, sensors designed for other areas such as the earlobe can also be found, nonethe-
less, the placement at the hand level is particularly advantageous for the design of mul-
timodal measurement units, as it enables the combination of BVP signals with other
parameters (e.g. electrodermal activity).
3 Methodology
Our work targeted the comparison of heart rate measurements taken at the hand palm
and at the fingertip, aiming at the feasibility evaluation of palmar sensors for that pur-
pose. We used a set of two BVP sensors, a standard transmissive sensor placed at the tip
of the ring finger, and an experimental reflective sensor in a side-by-side, dual-emitter,
single detector configuration (Figure 2(a)), placed at the base of the hypothenar emi-
nence, near the point where it meets the wrist (Figure 2(b)). This palmar location was
identified as the least affected area within hand whenever finger movements occur. The
palm sensor was compared with a finger tip since this last one is considered the gold
standard to measure heart rate based on PPG technique for clinical practice. Further-
more, the finger tip used as standard it was also validated by [10], which compared
the HR and HRV extracted from the finger tip sensor and ECG sensor. The authors
have shown a strong positive association between all the parameters calculated using
the finger BVP and ECG signals.
A bioPLUX research wireless biosignal acquisition unit was used for data acquisi-
tion, enabling synchronous sampling and real-time transmission of the collected data
to a base station. For the measurements at the fingertip, a bvpPLUX sensor was used;
for the experimental palmar sensor, the base circuitry of a bvpPLUX was used but the
emitter/detector arrangement was adapted according to what previously described. Raw
sensor data was acquired with 1000Hz sampling rate and 12-bit resolution; through of-
fline signal processing, we computed the heart rate information and performed statisti-
cal analysis of the results. Figure 3 depicts an example of the raw signals obtained with
each of the sensors.
37
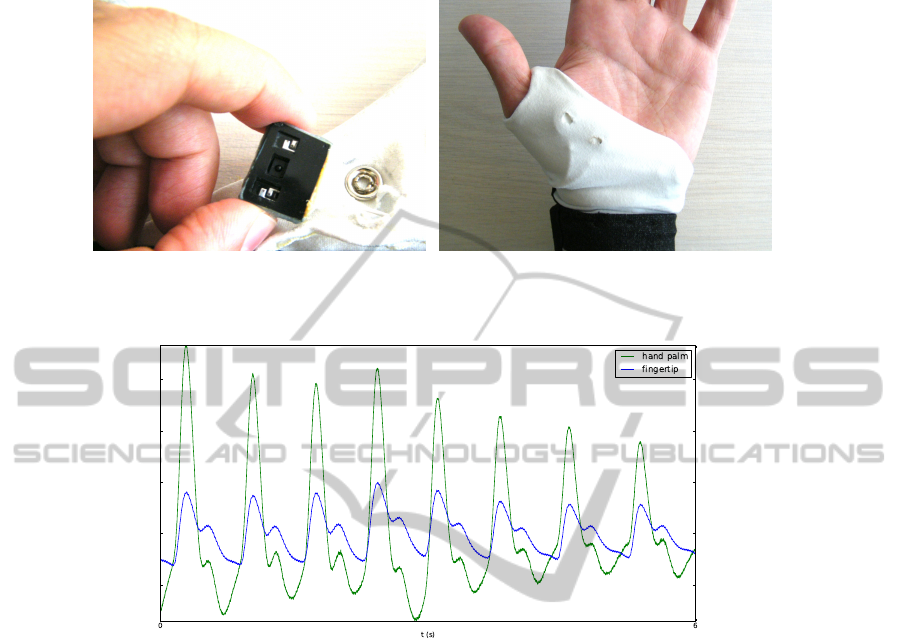
(a) Palmar sensor (b) Hand placement
Fig. 2. Blood Volume Pulse (BVP) sensor and placement at the hand palm.
Fig. 3. Palmar and fingerprint BVP signal.
4 Results
Experimental evaluation was performed on a group of 10 healthy subjects, composed
by 5 males and 5 females, with an average age of 26±3 years, and quietly sat in order to
avoid movement artifacts. We intend to validate the palm position with the finger and so
no movement artifact must be in the signal. These artifacts mask the BVP signals, not
allowing to visualize the raw BVP signal and extract the cardiac and signal parameters.
Data was acquired at rest for a period of 5 minutes, and analysed with respect to the
accuracy of heart rate calculation (HR), signal-to-noise ratio (SNR), and root mean
square (RMS). Table 1 outlines the main results; which revealed a very strong positive
association between the measurements obtained by both sensors.
The heart rate exhibits a coefficient of determination R
2
> 98%, and a p− value >
0.05, showing that the outcomes are not statistically different. The measurement di-
vergence between both sensors is 1bpm at most, as shown by the average heart rate
difference of 0.25bpm ± 0.45. Another interesting finding is a pulse latency between
38

Table 1. Fingertip and hand palm BVP sensors comparison.
Fingertip Hand Palm
M ± SD M ± SD
HR (bpm) 70.13 ± 10.51 70.38 ± 10.07
SNR (dB) 132.70 ± 61.43 173.30 ± 60.21
RMS (V) 0.22 ± 0.12 0.07 ± 0.05
the hand palm and the fingertip; from the collected data, an average 0.14 ± 0.38s lag
was found, with the maximum being 0.73± 0.08s for one of the tested subjects, and the
minimum being 0s for two others. At the palmar level, the experimental BVP sensor
used in the tests also presented a higher SNR, and a lower RMS.
5 Conclusions
The heart rate is one of the most widely adopted biomedical indicators in use to date,
and state-of-the-art research has focused on finding wearable and easy to use acquisi-
tion methods applicable in free living and quality of life activities. While chest straps
currently provide a convenient acquisition possibilities, with a very high level of dis-
cretion, a problem arises in applications that require the combination of heart rate with
other indicators that need to be measured in body areas other than the chest.
Clinical psychology is one such area, where measurements as the electrodermal
activity (typically measured at the hand palms or fingers), also provide important psy-
chophysiological information. Blood Volume Pulse (BVP) sensors, stand as alternative
method for heart rate assessment at the hand level, however current measurement ap-
proaches greatly limit the subjects normal activities, as they require the sensor to be
clipped to a finger. In our work, we further extend the stat-of-the-art in the field, by
evaluating the feasibility of using the BVP for heart rate assessment at the palmar level,
thus enabling the design of more integrated and practical multimodal measurement sys-
tems.
Results obtained from real-world data have revealed a high correlation between
measurements taken at the hand palm and at the standard finger tip location (R
2
>
98%), as shown also by the average divergence of 0.25bpm. Another interesting find-
ing was a latency between the palmar and finger BVP pulses; this, together with further
validation on a larger set of test subjects will be the focus of future work within our
group and in daily-use condition. This will allow to lead filter studies in order to under-
stand how to remove the movement artifacts into the BVP signal and, consequently, to
improve the feasibility of the measures. Furthermore, usability and hygiene conditions
will be also evaluated, which will enable to make adjustment in the glove and become
it more comfortable and usable for clinical practice.
Acknowledgements
This work was partially funded by the Seventh Framework Programme (FP7) under the
39

”ICT4Depression” project (ref. 248778), and by the Fundac¸
˜
ao para a Ci
ˆ
encia e Tecnolo-
gia (FCT) under the grant SFRH/BD/65248/2009, whose support the authors gratefully
acknowledge.
References
1. Duun, S., Haahr, R., Birkelund, K., Thomsen, E.: A ring-shaped photodiode designed for use
in a reflectance pulse oximetry sensor in wireless health monitoring applications. Sensors
Journal, IEEE 10 (2010) 261–268
2. Webster, J.: Design of Pulse Oximeters. Taylor & Francis (1997)
3. Reisner, A., Shaltis, P., McCombie, D., Asada, H.: Utility of the photoplethysmogram in
circulatory monitoring. Anesthesiology 108 (2008) 950
4. Picard, R. W.: Affective Computing. 1st edn. The MIT Press (2000)
5. Chung, E. K.: Pocketguide to ECG Diagnosis. Blackwell Publishing Professional (2000)
6. Haahr, R., Duun, S., Thomsen, E., Hoppe, K., Branebjerg, J.: A wearable electronic patch
for wireless continuous monitoring of chronically diseased patients. In: Medical Devices and
Biosensors, 2008. ISSS-MDBS 2008. 5th International Summer School and Symposium on,
IEEE (2008) 66–70
7. Boucsein, W.: Electrodermal Activity. 1st edn. Springer (1992)
8. Trull, T. J.: Clinical Psychology (with InfoTrac). 7 edn. Wadsworth Publishing (2004)
9. Nonin: Nonin - nonin medical inc. [online] avalilable at: http://www.nonin.com/ [accessed
5 september 2011] (2011)
10. Medeiros, J., Martins, R., Palma, S., Gamboa, H., Reis, M.: Development of a blood volume
pulse sensor to measure heart rate variability. In: Proceedings of the IBEROSENSOR 2010.
(2010)
40
