
E-HEALTH DRIVERS AND BARRIERS FOR CLOUD
COMPUTING ADOPTION
Marco Nalin, Ilaria Baroni and Alberto Sanna
Fondazione Centro San Raffaele del Monte Tabor, via Olgettina 60, Milan, Italy
Keywords: TClouds, Cloud computing, Electronic health record, EHR, eHealth, Privacy, Security.
Abstract: Cloud Computing is rapidly changing, or at least reorganizing, the IT domain. Several sectors are already
benefitting from this change, others are slower in the adoption. Healthcare sector, and eHealth in particular,
could take important advantage from Cloud Computing, but there are limitations that still need to be
overcome for a proper adoption. This paper explores the main drivers that could lead eHealth toward Clouds
and the main risks and recommendations that should be taken into account.
1 INTRODUCTION
There is a lot of discussion around Cloud Computing
and whether it is just a marketing buzz, a new word
for describing already existing technologies or
something really innovative that will change the IT
service models. The definition of Cloud Computing
itself is already quite controversial, not only are
there hundreds (or even thousands) of versions
around the Net, but there are also several articles and
websites trying to summarize a unique definition.
Being free to choose any of them, we opt for the
generic definition provided by IBM (Amrhein and
Quint, 2009): “cloud computing is an all-inclusive
solution in which all computing resources
(hardware, software, networking, storage, and so
on) are provided rapidly to users as demand
dictates”.
As expressed in Berkeley view on Cloud
Computing (Armbrust, 2009), there are some
common characteristics in the definitions: 1) the
infinite availability of resources, accessible on
demand at least in the users’ perception, 2) the
elimination of big initial investments from the users,
and 3) the pay-per-use business model.
Also the term “eHealth” is very generic and it
encompasses a set of different application domains.
The macro areas that are nowadays referred to as
“eHealth” regards technologies that makes the a)
patient’s life, b) the doctor’s life and c) the medical
information exchange and processing easier. These
areas are:
Grid Services for Clinical Research: in clinical
practice, medical research and personalized
healthcare, there’s a growing demand for the
integration and exploitation of heterogeneous
biomedical information. Grid technologies are
taking place to federate different data sources,
providing access and query functionalities to
distributed information in a unified and integrated
way. Moreover, they are able to offer ? without
interruption computing resources.
Virtual Healthcare Professionals Network:
many times, healthcare professionals need to
cooperate or exchange information about patients
and clinical practice. These networks allow
professional teams to collaborate and share data or
opinions, about patients or other specific arguments,
through digital facilities.
Consumer Health Informatics (e.g., PHR): this
domain includes more or less all the electronic
resources that can be used not only by patients but
also by healthy individuals, for topics on medicine
or healthcare.
A clear example is the PHR (Personal Health
Record), defined by Markle Foundation definition as
“an Internet-based set of tools that allows people to
access and coordinate their lifelong health
information and make appropriate parts of it
available to those who need it” (Markle Foundation,
2003, p. 14). Two examples of PHR are Google
Health and Microsoft HealthVault.
Electronic Health Record: the EHR is the
personal record created by hospitals, clinics or other
385
Nalin M., Baroni I. and Sanna A..
E-HEALTH DRIVERS AND BARRIERS FOR CLOUD COMPUTING ADOPTION.
DOI: 10.5220/0003379703850390
In Proceedings of the 1st International Conference on Cloud Computing and Services Science (CLOSER-2011), pages 385-390
ISBN: 978-989-8425-52-2
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)
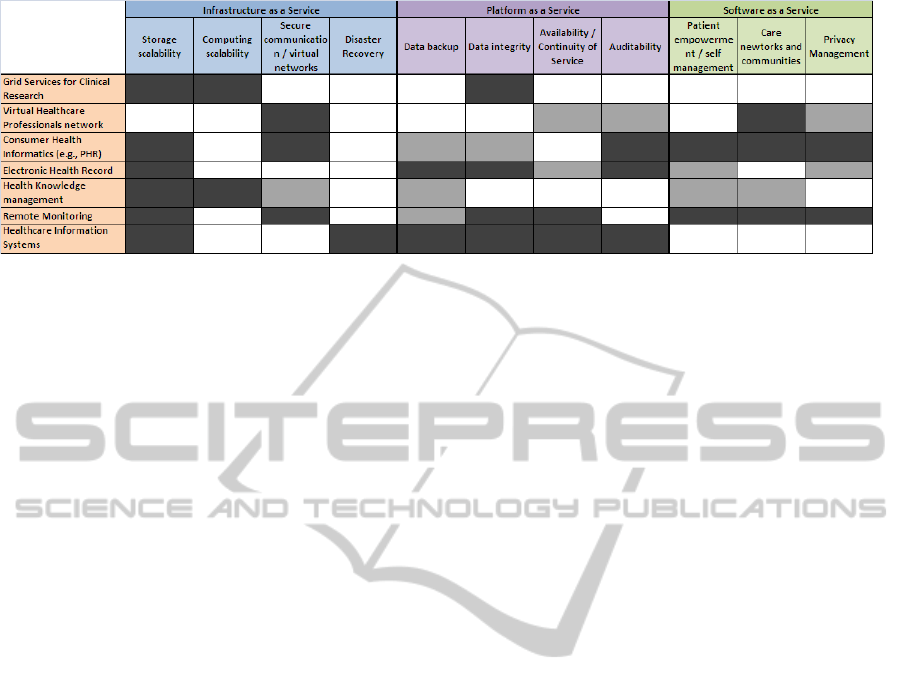
Figure 1: eHealth domains and Cloud services matrix.
healthcare providers that can be exported for use in
other institutions. There are some standards that can
be used for this purpose: HL7, ANSI X12, CEN,
DICOM, etc. The EHR is important to ensure a good
interoperability in the communication between
medical structures thus resulting in the improvement
in cost and time effectiveness within the healthcare
system.
According to a report from marketing research firm
Kalorama Information, the market for EHR systems
will grow by 14.1% annually through 2012.
Health Knowledge Management: is the
implementation of an IT system that can support the
creation, capture, retrieve, share and effective
application of knowledge for the improvement in
health. In 2005, WHO began a global initiative for
the diffusion of the Knowledge Management
Strategy aimed to implement programs capable of
bridging the gap between knowledge and practice,
the "know-do gap". ICT solutions could help in
providing and retrieving always updated medical
knowledge through the use of semantic technologies
and ontologies.
Remote Monitoring: (e.g., telemedicine, m-
Health, Ambient Assisted Living, home healthcare,
etc.): it includes all kind of remote communication
of data among patient and healthcare professional,
done through electronic resources. Some example
of remote monitoring are telemedicine that allows
treatment and care services given directly at the
patient’s home (sometimes called in a more generic
term as “home healthcare”); m-Health, that includes
the collection of data from devices; Ambient
Assisted Living that provides all methods, concepts
and electronic systems useful to support an assisted
person.
Healthcare Information Systems: it can be
described as the core of the Hospital/Medical IT
structure system. It’s usually composed by the
clinical data repository, clinical decision support
system, checked medical vocabulary, computerized
provider order entry, pharmacy management system,
and the electronic medication administration record
(like solutions for appointments and work schedule
management).
This paper will explore the potentialities and
limitations that the use of cloud infrastructures and
platforms for the eHealth sectors. In particular,
section 2 will describe the main drivers and
opportunities that could lead to adoption of Cloud
infrastructure from Health Organizations, while
section 3 will underline some important aspects to
take into account before opting for such choice.
2 BENEFITS OF EHEALTH
FROM CLOUD SOLUTIONS
As many other domains, eHealth could benefit a lot
from the three main innovative infrastructural
aspects (Armbrust et al, 2009) of cloud computing:
the illusion of infinite computing resources available
on demand, the elimination of an up-front
commitment by Cloud and the ability to pay for use
of computing resources. However there can be more
specific advantages in the use of Cloud Computing
solutions for the different sub-domains of eHealth
mentioned above, as shown in Figure 1, that can be
proposed at Infrastructure as a Service (IaaS),
Platform as a Service (PaaS), or Software as a
Service (SaaS) levels. In particular, some of these
domains’ requirements are:
a) IaaS - Storage Scalability: Research from a
global survey (BridgeHead 2010) from hospitals and
healthcare organizations worldwide revealed that
medical images, scanned documents, email and
advances towards the EHR are going to be the cause
for a meaningful increase in healthcare data that is
already challenging hospitals. Most of the
participants in this survey (41%) claimed that they
CLOSER 2011 - International Conference on Cloud Computing and Services Science
386

are expecting an increase in the data volume up to
25%, while approximately one fifth of them (18%) is
expecting a growth from 25% to 50%. Besides
traditional Healthcare Information Systems, there
are other emerging fields of eHealth that could lead
to exponential growth in the database size. For
example remote monitoring, especially if the
patient’s monitoring is continuous (regardless of the
activity to be monitored, e.g., ECG, physical
activity, etc.), and with a lot of patients, we can
expect rapid expansion of the data volume. Cloud
Computing allows to easily scale storage capacity
when needed.
b) IaaS - Computing Scalability: Cloud
Computing offers also computing power scalability
which may be particularly important for some
eHealth domains. One example is the Grid Services
for Clinical Research. Health institutions which
perform also clinical/medical research can have the
need to perform analysis on large volumes of data,
requiring also large computational power. However
these studies are not continuous, which makes Cloud
Computing particularly suitable for these
applications, with its pay-per-use model. Another
example may be the information search on large
database of trusted medical knowledge. In this case,
a lot of computing power may be needed if several
users perform searches on journals, articles, etc. at
the same time, but this is hard to predict in advance.
c) IaaS - Virtual Networks: An interesting IaaS
feature that the Cloud could offer is the creation of
virtual networks to connect healthcare institutions
(like in the case of Virtual Healthcare Professionals
networks), or to connect patients and healthcare
institutions (like in the case of remote monitoring,
e.g., telemedicine, AAL, etc.).
d) IaaS - Disaster Recovery: The results from
BridgeHead survey reported what are the top
priorities in the next investments for IT budget in
healthcare organizations. Disaster recovery, together
with Data Backup and Business Continuity, was a
priority for 44.3% of the respondents. Cloud
Computing could offer backups and redundancy at
lower costs with respect to legacy systems.
e) PaaS - Data Backup: In line with the previous
point, Data Backup is a top priority for many
organizations. It was separated because Data Backup
deals more with databases and data structure (PaaS
level), while Disaster Recovery deals more with
storages and virtualization (IaaS level).
f) PaaS - Data Integrity: Medical data integrity
should be guaranteed to assure the correctness of the
care process. This should be guaranteed both in
Healthcare Information Systems and in possible
EHR applications running on the Cloud.
g) PaaS - Availability/Continuity of Service:
Business continuity and availability are very
important in most of the medical applications,
especially those dealing with possible emergency
situations detection (e.g., remote patients’
monitoring) and management (e.g., availability of
the EHR in a dangerous situation). The main
objection to the adoption of Cloud Computing (65%)
in the BridgeHead survey was the hospitals’
concerns about the security and availability of
healthcare data given the great number of threats,
including privacy breaches and identity theft. Other
objections include cost (26.1%) and a lack of
confidence that Cloud offers greater benefits with
respect to local storage media (26.1%). In theory,
Cloud solutions will assure better continuity than
legacy systems, but on this Cloud Providers still
need to convince their possible customers, as shown
from the results of the BridgeHead survey.
h) PaaS - Auditability: The possibility to ensure
that the IT system is compliant with existing
regulations is very important for eHealth
applications, in particular for what concerns the
management of patients’ data in accordance with
privacy protection directives. PaaS type of services
should ensure the auditability to attract Health
Organization in investing in this kind of solutions.
This is particularly critical for example in managing
EHR or PHR applications, but also in case the Cloud
will host and run Hospital Information Systems.
i)
SaaS - Patient Empowerment in Self-
management: One of the main driver for the
adoption of Cloud Computing in eHealth can be the
trend that sees the patients becoming more and more
protagonist of their health management process
(Mandl and Kohane, 2008). Thanks to the
information and communication technologies,
patient-doctor relationship is evolving and may be
potentially resulting in more shared decision making
process. A study conducted over 6369 persons
claimed that almost two thirds (63.7%) of adults
searched online for some type of health or medical
information either for themselves or for someone
else through the Internet. In general, evidence shows
that, even if health professionals remain the most
trusted source of Health information, electronic
media are becoming more and more important too,
and in some cases, patients are looking for
information online before talking with their
physicians (Hesse et al, 2005). In the new scenario
just depicted, it clearly shows the limitations of the
vision of EHR stored locally on an internal
E-HEALTH DRIVERS AND BARRIERS FOR CLOUD COMPUTING ADOPTION
387

Healthcare Organization database. Cloud Computing
platforms at different levels of abstractions, could
support this new paradigm of eHealth. The proposals
of Google (with GoogleHealth) and Microsoft (with
their Health Vault) of Health related SaaS platforms
is a demonstration of the business opportunities and
benefits of Cloud Computing applications in this
domain.
j) SaaS - Care networks and Communities: SaaS
solutions could also facilitate the shift from
traditional EHR to Patient-Controlled Health
Records (PCHR), as well as the creation of patients
support networks and online medical communities,
which are more and more a reality thanks to Web 2.0
technologies (Lo and Parham, 2010).
k) SaaS - Privacy Management: The possibility to
manage privacy settings of personal data must be
ensured for the success of SaaS solutions for
eHealth. In particular this problem will be described
in the next section. The access control to patients’
data is not only role-based but also context-bases.
For example, patient’s relatives may have access to
the patient’s record in cases of emergency (in cases
where data is required while the patient is
unconscious and cannot provide his/her consent), but
not in normal conditions. In the development of
platforms that will make the exchange of medical
data seamless and easy, patient must be sure that
his/her data are treated not only according to
national/international regulations, but also to their
personal preferences.
Figure 1 shows a table with the eHealth domains and
the requirements listed above. The cells have been
coloured in dark gray to identify areas in which the
adoption of Cloud Computing solutions can have a
meaningful impact, while in light gray we indicated
areas in which Cloud Computing is not critical to
satisfy that requirement but can contribute to achieve
it.
3 ANALYSIS AND LIMITATIONS
OF THE EXISTING CLOUDS
Cloud Computing offers a lot of potential
advantages to Health and eHealth applications as
described in the previous section, however there are
still several obstacles related to the adoption, the
growth and the policy management of the Cloud. In
particular the main problems are 1) availability of
service, 2) data lock-in (and interoperability), the 3)
data confidentiality and auditability, 4) data
protection regulations compliance, and 5) security:
1) Availability: availability is a crucial issue for
any company whose business continuity is critical,
and Healthcare Organizations are a perfect example
for this. Cloud providers should be able to
demonstrate that they can guarantee the continuity of
service in order to convince healthcare providers to
move their systems to cloud. For example,
unavailability of data is intolerable for Healthcare
Organizations in case of the need to access patients’
health records in critical situations or during an audit
for certifications, etc. These questions are to be
addressed by a recent FP7 project TClouds
(TClouds, 2011) funded by the European
Commission. The TClouds project proposes a
solution that involves the creation of a federation of
Clouds Providers to ensure availability and avoid
single point of failure, in case one cloud provider in
the federation has problems.
2) Data Lock-in: APIs for Cloud Computing itself
are still essentially proprietary, or at least have not
been the subject of active standardization (Armburst
et al, 2009). The fact that healthcare organization
cannot easily migrate their data and software from
one Cloud Provider to another is a major implicit
risk in the adoption of a cloud infrastructure. For
example, Hospitals are required by law to keep
medical records for a long period of time, and the
“survival” of the Cloud Provider is not guaranteed
(as in any new IT market, competitive pressure,
inadequate business strategy, lack of financial
support, etc, could lead some providers to go out of
business or at least to force them to restructure their
service portfolio offering).
3) Data Confidentiality and Auditability: As far
as data confidentiality is concerned, it is more a
psychological problem of not having the data under
direct control but there is no reason to think that
Cloud Infrastructure can’t have the same security
level of in-house applications. Many of the obstacles
can be overcome immediately with technologies
such as encrypted storage, VLAN etc. Encrypting
data approach was successfully used by TC3, a
healthcare company with access to sensitive patient
records, when moving their HIPAA-compliant
application to Amazon Web Services (Amazon,
2010). Besides standard security policies, Cloud
Computing should consider additional risks like in
the case of multiple tenancies and the reuse of
hardware resources, where there is also a high risk
due to insecure or incomplete data deletion (an
important issue in medical cases). It’s also critical to
define system administrators and how to manage
security by service providers, to avoid damage
CLOSER 2011 - International Conference on Cloud Computing and Services Science
388

caused by malicious insider: the risk is often greater
than expected.
Furthermore, it is reasonable to expect even not
malicious violation of data confidentiality, for
example in case Cloud Providers observe data traffic
in the Cloud for legitimate security protocols and
procedures.
4) Regulation Compliance: it may be difficult for
the health organization (in its role as data controller)
to effectively check the data handling practices of
the Cloud Provider and thus to be sure that the data
is handled in a lawful way. As an example of
privacy policies compliance, Google Health and
Microsoft HealthVault both declared that their
services aren’t covered by the Health Insurance
Portability and Accountability Act (HIPAA), whose
privacy rules protect the privacy of individually
identifiable health information, they don't store data
on behalf of health care providers and their primary
relationship is with the users (Microsoft, 2009;
Google, 2010).
To support the growth of the use of these
technologies ensuring protection of patient’s
privacy, the Health Information Technology for
Economic and Clinical Health (HITECH) Act
recently extended the requirements provided by
HIPAA, also to the PHRs vendors. HITECH Act
compliance is at the moment untested and
presumably, the Google and Microsoft repositories
are not aligned with it yet (U.S. Department of
Health & Human Services, 2010; Gordon M., 2010).
The TClouds project will identify legal constraints
and privacy risks associated with cross-border cloud
deployments. This analysis will drive the
implementation of a federation of Clouds platform.
5) Security: The European Network and
Information Security Agency (ENISA) provides
some recommendations to prevent issues and risks
related with Cloud Computing (Perilli A. et al,
2010). First of all Cloud customers need assurance
that providers are implementing appropriate security
strategies to mitigate security risks (they need this in
order to make sound business decisions and to
maintain or obtain security certifications). The
parties of a contract should pay particular attention
to their rights and obligations related to notifications
of breaches in security, data transfers, creation of
derivative works, change of control, and access to
data by law enforcement entities. Moreover, they
should carefully consider whether standard
limitations on liability adequately represent
allocations of responsibility given the parties’ use of
the cloud, or responsibilities for infrastructure.
These issues are especially delicate if we consider
that the medical data are sensitive data. How to build
trust in the Cloud, data protection in large scale
cross-organizational systems, and large scale
computer system engineering (resource isolation
mechanisms, interoperability, resilience, …), are
priority areas of research in order to foster the
adoption of Cloud Computing infrastructure both
from traditional Healthcare providers and eHealth
providers.
4 CONCLUSIONS
Healthcare infrastructures relies more and more on
ICT infrastructures, thanks to continuous
computerization of healthcare processes and
digitalization of clinical documents. Furthermore,
new trends in eHealth see more and more the patient
as a proactive actor (and not anymore an object) of
these processes. Cloud Computing seems to be a
perfect solution supporting these trends, and
providing cost-efficient and scalable solutions,
however Cloud Providers should guarantee as
commodity, important features of their platform like
resiliency, auditability, privacy protection,
compliance with regulations, etc.
As described in this paper, there are several
“definitions” of eHealth and many of them can
benefit from Cloud solutions at different levels.
However this implies that very different actors
should be convinced to invest in this kind of
technologies, both as cloud providers and users,
ranging from hospitals, care networks,
National/Regional healthcare systems, big IT
enterprises (e.g., Google, Microsoft), small/medium
enterprises (e.g., telemedicine companies), etc. For
this reason, it is hard to predict how the Cloud
market will move in the next years and who will be
the first adopters, even if some first solutions are
already appearing and demonstrating sound business
opportunities (e.g., Microsoft HealthVault).
As far as the European scenario is concerned, for
the moment the emerging cloud computing market is
already led by US players, which could lead to
difficulty in compliance with European and national
specific regulations. US centricity and lack of
verifiable resilience and privacy are reasons why
today’s cloud infrastructures can only be used for
applications that are neither business critical nor
privacy sensitive. For this reason, many European
eHealth businesses cannot benefit yet from the
advantages offered by cloud solutions. While private
clouds could be an answer in this sense, they will
E-HEALTH DRIVERS AND BARRIERS FOR CLOUD COMPUTING ADOPTION
389

never reach economies of scale and scope that are
needed to provide cost effective solutions.
In this sense, besides designing a platform to
improve privacy and resiliency of existing Clouds,
the TClouds project will also identify business and
legal challenges, in order to build a regulatory
framework for enabling privacy-enhanced cross-
border infrastructure Clouds.
ACKNOWLEDGEMENTS
This research has been partially supported by the
TClouds project http://www.tclouds-project.eu
funded by the EU 7
th
Framework Programme
([FP7/2007-2013]), grant number ICT-257243.
REFERENCES
Amazon Web Service Case Study: TC3 Health. 2010.
Retrived November 15, 2010, form http://aws.
amazon.com/solutions/case-studies/tc3-health/
Amrhein, D., Quint, S. 2009. Cloud computing for the
enterprise: Part 1: Capturing the cloud. Retrieved
November 2, 2010, from http://www.ibm.com/
developerworks/websphere/techjournal/0904_amrhein/
0904_amrhein.html
Armbrust, M., Fox, A., Griffith, R., Joseph, A. D., Katz,
R. H., Konwinski, A., Lee, G., Patterson, D. A.,
Rabkin, A., Stoica, I., and Zaharia, M. 2009. Above the
Clouds: A Berkeley View of Cloud Computing.
Retrieved November 2, 2010, from http://www.eecs.
berkeley.edu/Pubs/TechRpts/2009/EECS-2009-28.pdf
BridgeHead. 2010. Report: The BridgeHead Software
International 2010 Data Management Healthcheck
Survey Retrieved November 2, 2010, from
http://www.bridgeheadsoftware.com/pdfs/BH_Rpt_Da
ta-management-survey-results_A4.pdf
Google. 2010. Google Health and HIPAA. Retrieved
November 15, 2010, from http://www.google.com/
intl/en-US/health/hipaa.html
Gordon M. 2010. HITECH Extends Privacy Obligations to
EHRs and PHR Vendors. Retrieved November 15,
2010, from http://www.itbusinessedge.com/cm/
community/features/guestopinions/blog/hitech-extend
s-privacy-obligations-to-ehrs-and-phr-vendors/?cs=38
631
Hesse, B. W., Nelson, D. E., Kreps, G. L., Croyle, R. T.,
Arora, N. K., Rimer, B. K., and Viswanath, K. 2005.
Trust and Sources of Health Information. Arch Intern
Med. 2005;165:2618-2624
Lo, B., and Parham., L. 2010. The Impact of Web 2.0 on
the Doctor-Patient Relationship. The Journal of Law,
Medicine & Ethics, vol. 38, Issue 1, (Spring 2010)
pp.17–26
Mandl, K. D., and Kohane, I. S. 2008. Tectonic shifts in
the health information economy. N Engl J Med 2008
Apr 17;358(16):1732-1737.
Markle Foundation. 2003. The Personal Health Working
Group Final Report. Retrieved March 2, 2010, from
http://www.connectingforhealth.org/resources/final_ph
wg_report1.pdf
Microsoft. 2009. Microsoft HealthVault and HIPAA.
Retrieved November 15, 2010, from
http://msdn.microsoft.com/en-us/healthvault/cc50732
0.aspx
Perilli, A., Manieri, A., Algom, A., Balding, C., Bunker,
G., Rhoton, J., Broda, M., Rohr, M., Brian, O.,
Lindstorm, P., Dickman, P., Massonet, P., Samani, R.,
Pascoe, S., Nair, S., Balboni, S. 2009. Benefits, risks
and recommendations for information security.
Retrieved November 15, 2010, from http://www.
enisa.europa.eu/
Tang, T. C., and Lee, T. H. 2009. Your Doctor’s Office or
the Internet? Two Paths to Personal Health Records,
New England Journal of Medicine 360 (2009): 1276-
1278.
TClouds. 2011. “Trustworthy Clouds”. Retrieved February
25, 2011, from: http://www.tclouds-project.eu/
U.S. Department of Health & Human Services. 2010.
HITECH Act Rulemaking and Implementation Update,
Retrieved November 15, 2010, from http://www.hhs.
gov/ocr/privacy/hipaa/understanding/coveredentities/h
itechblurb.html
World Health Organization. n.d.
Department of
Knowledge Management and Sharing (KMS).
Retrieved March 2, 2010, from http://www.who.int/
kms/en/
CLOSER 2011 - International Conference on Cloud Computing and Services Science
390
