
THINKING SPATIALLY, ACTING COLLABORATIVELY
A GIS-based Health Decision Support System for Improving
the Collaborative Health-planning Practice
Ori Gudes
1, 2
, Virendra Pathak
1
, Elizabeth Kendall
2
and Tan Yigitcanlar
1
1
School of Urban Development, Queensland University of Technology, 2 George Street, Brisbane, Australia
2
Griffith Health Institute, Griffith University, University Drive, Meadowbrook, Australia
Keywords: Spatial health decision support systems, Collaborative health planning, DSS, e-Health.
Abstract: The field of collaborative health planning faces significant challenges due to the lack of effective
information, systems and the absence of a framework to make informed decisions. These challenges have
been magnified by the rise of the healthy cities movement, consequently, there have been more frequent
calls for localised, collaborative and evidence-driven decision-making. Some studies in the past have
reported that the use of decision support systems (DSS) for planning healthy cities may lead to: increase
collaboration between stakeholders and the general public, improve the accuracy and quality of the
decision-making processes and improve the availability of data and information for health decision-makers.
These links have not yet been fully tested and only a handful of studies have evaluated the impact of DSS
on stakeholders, policy-makers and health planners. This study suggests a framework for developing healthy
cities and introduces an online Geographic Information Systems (GIS)-based DSS for improving the
collaborative health planning. It also presents preliminary findings of an ongoing case study conducted in
the Logan-Beaudesert region of Queensland, Australia. These findings highlight the perceptions of decision-
making prior to the implementation of the DSS intervention. Further, the findings help us to understand the
potential role of the DSS to improve collaborative health planning practice
.
1 INTRODUCTION
In recent years, a model of planning known as the
‘Collaborative health planning’ has evolved to
become one of the key foundations of contemporary
health planning. This model is grounded in both
‘communicative planning theory’ and ‘population
health theory’ (Gudes et al. 2010). Growing
evidence from the literature shows that large health
systems seeking to create collaborative health
planning projects face many planning challenges,
including engaging multiple stakeholder groups;
making consensus-based decisions; bringing
evidence into the decision-making processes;
planning in a participatory manner; and exploring
the full spectrum of health determinants based on
diverse sources of information.
For this reason, Northridge et al. (2003) argued
that stronger collaborations were needed between
urban planners, health policy-makers, and
community members to ensure effective planning in
the light of ‘Healthy Cities (WHO, 1999)’ initiative.
It is recognised that evidence-based decision making
is critical to the collaborative planning process and
the evidence-based approach is based on an effective
access to data. It was noted that the smart use of data
and publicly available information on health is
essential to generate informed decision-making
(NHHRC, 2009). Literature has suggested that
increasing and improving access to relevant data
may lead to an improved decision-making processes.
Thus, there is a need to develop a framework for
stakeholders to support them to access relevant data.
Some studies have justified the use of decision
support systems (DSS) in planning for healthy cities
as these systems have been found to improve the
planning process (Cromley & McLafferty 2003).
These systems have been gaining prominence in
recent years and have been described by several
researchers over the last few decades as an efficient
support tool for health planning (Reinke 1972;
Reeves & Coile 1989; Higgs & Gould 2001).
148
Gudes O., Pathak V., Kendall E. and Yigitcanlar T..
THINKING SPATIALLY, ACTING COLLABORATIVELY - A GIS-based Health Decision Support System for Improving the Collaborative Health-planning
Practice .
DOI: 10.5220/0003131101480155
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 148-155
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

However, knowledge about the impact of DSS on
health planners is relatively limited. This study
provides a framework for organising and delivering
information to planners to use in developing healthy
cities. It also introduces an online Geographic
Information Systems (GIS)-based DSS, developed
for improving the collaborative health planning. To
ascertain whether the DSS has a valuable impact on
health planners, a study is currently being conducted
in the Logan-Beaudesert Health Coalition (LBHC).
This paper provides an overview of the healthy cities
movement and collaborative health planning,
introduces ICT and E-Health approaches and the
DSS. It then discusses a proposed framework for
organising information that can contribute to
collaborative health planning. Preliminary results are
presented to demonstrate the perceptions of
decision-making within the LBHC and the potential
role of the DSS.
2 THE HEALTHY CITIES
& COLLABORATIVE HEALTH
PLANNING
The ‘Healthy Cities’ initiative was officially
introduced in 1986 by Ilona Kickbusch at a
conference of the World Health Organisation
(WHO) in Copenhagen, Denmark. To date, “about
90 cities are members of the WHO European
Healthy Cities Network, and 30 national Healthy
Cities networks across the WHO European Region
have more than 1400 cities and towns as
members”(WHO, 2010). Also, according to Health
Cities Illawarra
(2010), “since 1985 over 3000
healthy cities, towns, villages and islands have been
established throughout the world”. In order to plan
effectively for healthy cities, the historic
collaboration between urban planning and public
health professionals must be revived, and this
collaboration must be based on informed evidence-
based decision-making (Northridge et al., 2003).
However, evidence-based decision-making has been
hindered by the fact that there are no models to
define the type of information that must be
considered by health planners and there is no
method for sharing this information in a meaningful
form. As Flynn (1996) concluded, every community
is unique, with different physical, social, political
and cultural contexts that must be understood in the
planning process. Therefore, it is necessary for
planners to develop a thorough understanding of
each individual community health profile and its
features that influence health. Schulz and Northridge
(2004) developed a public health framework for
health impact assessments. This framework
summarises the different levels of factors that impact
upon health and, therefore, should be considered in
health planning. According to Northridge et al.
(2003), factors that contribute to health can be
divided into four levels, namely: Macro, Meso,
Micro and Individual. According to the model, these
factors interact to contribute to health in the
community, so must all be considered when
undertaking health planning.
Some evidence in the literature supports the
application of collaborative health planning within
the healthy cities approach. First, and broadly,
collaborative planning promotes democratic
decision-making that facilitates shared ownership
and engagement in solutions (Murray 2006). Murray
has also suggested a model to evaluate the level of
collaboration in planning. The model identifies
different levels of collaboration (i.e. Networking,
Cooperation, Coordination, Coalition and
Collaboration) that might be applied. Additionally,
he highlighted the following domains of decision-
making that define collaborative health planning:
Evidence-based decision-making; Perceived
consensus; Participation in decision-making; and
Perceived satisfaction of decision-making. Second, it
encourages planners to communicate, interact and
negotiate with other sectors in order to resolve
disputes between groups that may have some
investment in the planning process (Campbell &
Fainstein 1996). Third, it facilitates a more
collaborative form of governance which in turn
implies a more collaborative and efficient delivery
of services to the community(Bishop & Davis 2001).
Therefore, collaborative health planning has the
potential to become a fundamental approach to
planning.
3 ICT AND E-HEALTH
APPROACHES
The World Health Organisation (WHO) defines E-
health as ‘the cost-effective and secure use of
information and communications technologies in
support of health-related fields, including health-
care services, health surveillance, health literature,
and health education, knowledge and research’. The
literature has highlighted the benefits of using E-
health and ICT tools to obtain better understanding
of health planning for policy-makers. Amongst these
THINKING SPATIALLY, ACTING COLLABORATIVELY - A GIS-based Health Decision Support System for
Improving the Collaborative Health-planning Practice
149

some prospective benefits are: increased access to
healthcare services and health-related information,
improved ability to diagnose and track diseases,
more actionable public health information and
expanded access to ongoing medical education and
training for health practitioners (Wave, 2009).
The
National Electronic Decision Support Taskforce (2008)
has also emphasised that EDSS (Electronic DSS) are
essential components of designing a national e-
health strategy.
Conversely, only little research has been focused
on the potential of E-health environments and ICT
tools to alleviate the negative health consequences of
social determinants of health (Han et al., 2010). As
the awareness to the importance of broad
understanding of social determinants of health
grows, it would be crucial to evaluate the impact of
ICT tools and E-health initiatives leveraging health
planners and decision-makers knowledge. Thus, ICT
tools and E-health initiatives should be focused on
finding innovative ways to enhance the day-to-day
work efficiency of health planners.
One of the innovative ways to present, store,
analyse and manipulate information is by adding its
spatial aspect. Particularly, given that social
determinants of health are spatially oriented. In this
regard, E-health initiatives may provide new
standards of accessibility to spatial health data. For
instance, health information could be geocoded and
displayed spatially, so end-users can create maps by
using different layers of spatial information overlaid
each other. Further, spatial analysis can be applied
by mapping layers of socio-economics,
demographics, and projected regional growth
forecasts, thus providing a new way of looking at
health concerns. Thus, application of spatial
technologies is an important step towards a better
understanding of public health issues and their
inherent complexities and for gaining insight into the
spatial distribution of health determinants (Higgs &
Gould, 2001). However, it is essential to expand the
use of this tool through online ICT platforms or as
part of broader E-health initiatives, to support health
decision-making processes.
4 A FRAMEWORK
FOR COLLABORATIVE
HEALTH-PLANNING
The overall aim of decision support systems (DSS),
without substituting decision-makers, is to improve
the efficiency of the decisions made by stakeholders,
optimising their overall performance and minimising
judgemental biases (Turban 1993). A framework has
been proposed for collaborative health planning that
illustrates the overall place of DSS within a healthy
cities’ planning initiative (See Appendix). However,
it is imperative that the DSS be based on a broad
information framework. Specifically, it is suggested
that the Information Management Framework based
on Schulz and Northridge (2004) should guide the
development of a community health profile, with
information being derived from multiple sources.
The ability to present this information in
meaningful, accessible and usable ways is a critical
challenge for establishing healthy cities. In this
regard, Duhl and Sanchez (1999) defined a list of six
fundamental characteristics (Health public policy,
Innovation, Community participation, Intersectoral
action, Policy decision making and Commitment to
health) that would be needed to create a healthy city.
If these characteristics are adopted, it is likely that a
healthy city will emerge. Thus, this framework
suggests that by utilising a DSS as part of a broader
healthy cities planning process, it is more likely that
healthy community will be established.
One of the innovative ways to present, store,
analyse and manipulate information for local
decision-making is by adding a spatial aspect,
particularly given that social determinants of health
are spatially oriented (i.e., grounded in place). In this
regard, health information could be geo-coded (into
Geographical Information Systems [GIS] software)
and displayed spatially, so end-users can create
maps by using different layers of spatial information
overlaid on each other. This method provides a new
way of looking at health concerns and may lead to
new decision-making. Thus, application of spatial
technologies is an important step towards a better
understanding of public health issues and their
inherent complexities and for gaining insight into the
spatial distribution of health determinants (Higgs &
Gould, 2001). However, it is essential to expand the
use of this tool through online platforms or as part of
broader e-health initiatives.
For example, for decision-makers to identify
gaps in the provision of health facilities in a given
community, GIS could be utilised to examine the
effect of travel time to health facilities by mapping
catchment areas and travel zones. The impact of new
facilities or new transport routes can be examined in
hypothetical scenarios. By placing this information
in an online setting, the capacity to share
information in a variety of forms will improve
stakeholders’ involvement in decision-making,
horizontal knowledge sharing and simplicity of the
HEALTHINF 2011 - International Conference on Health Informatics
150

decision process (Dur, Yigitcanlar & Bunker 2009).
Testing this framework in a real case-study would
ascertain whether the DSS has a valuable impact on
health planners.
5 CASE STUDY:
THE LOGAN-BEAUDESERT
HEALTH COALITION
The Logan Beaudesert Health Coalition (LBHC) is a
partnership established to address the growing level
of chronic disease in the region. The initiative
intended to build on work that had preceded it,
enhancing existing services and infrastructure,
establishing formal partnerships and mechanisms to
improve the coordination of existing resources as
well as planning for additional services and
strategies. It was initiated with a view to improving
health capacity at multiple levels through improved
and responsive localised planning. The Coalition has
a central board committee which oversees six health
initiatives or working groups, each focusing on a
specific area identified as needing attention. These
working groups focus on the early years of life (0 to
8 years), multicultural health, prevention and
management of existing chronic disease, integration
between general practice and acute settings, efficient
management and transfer of health information and
health promotion. Each group has a leader or project
manager
and a selected group of key stakeholders
from multiple sectors or relevant organisations. The
working groups are responsible for facilitating
decisions, polices or strategies by providing
recommendations and information to the LBHC
board. The LBHC board coordinates and directs the
coalition as a ‘whole’. Thus, given its focus on
collaborative decision-making, the LBHC is an ideal
platform from which to develop and observe the
DSS and its potential role.
6 METHOD
The purpose of this study was to understand the
potential role of the DSS in improving the
collaborative health planning practice of the LBHC.
Both quantitative and qualitative data were collected
prior to the implementation of the DSS to explore
the decision-making strategies and experiences of
the coalition members. The quantitative data was
collected using a 31-item survey based on several
decision-making scales (Dean & Sharfman, 1993;
Flood et al, 2000; Bennet et al, 2010; Parnell & Bell,
1994). The items measured the following four
dimensions of decision-making outlined by Murray
(2006): Evidence-based decision-making (5 items);
Perceived consensus (4 items); Participation in
decision-making (3 items) and Perceived satisfaction
of decision-making (10 items), defined as our four
key variables. In addition, three process variables
were measured, including: Perceived importance of
decision-making (3 items); Perceived effectiveness
of decision-making (3 items); and Perceived equity
of decision-making (3 items). Forty participants
were required to rate the extent to which they agreed
with each item using a 7 point Likert scale, with
choices ranging from ‘not at all’ to ‘completely
agree’. The questionnaire was disseminated to the
members of LBHC both in ‘hard copy’ and an online
survey so that the participants could select their
preferred method of completion. Participants were
also asked to comment on their decision-making
processes and experiences within the LBHC to
provide context for the quantitative findings. Both
the quantitative and qualitative data will be collected
again once the DSS has been fully implemented,
thus allowing an evaluation of the implementation
process and DSS utility.
7 PRELIMINARY FINDINGS
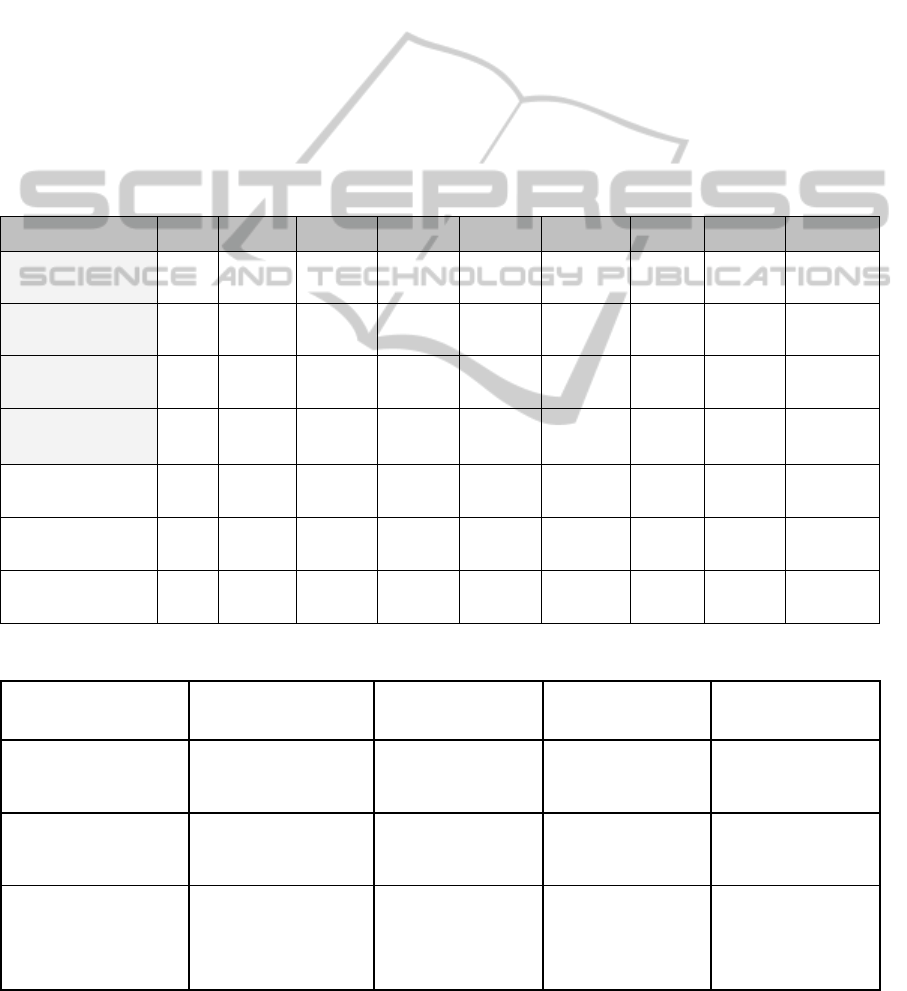
Table 1 provides the descriptive statistics for each of
the decision-making domains. The findings indicate
that, overall, satisfaction with information for
decision-making and perceived effectiveness of
decision-making were rated lowest of the seven
domains. Conversely, perceived participation of
decision-making and perceived equity of decision-
making were rated highest. To further examine
Murray’s (2006) four domains, one way Analysis of
Variance (ANOVA) and Post Hoc tests were
conducted using different groups within the LBHC
as independent variables. Participants were first
divided into clusters representing the different types
of initiatives that were auspiced by the LBHC. Three
clusters were constructed to represent a focus on
governance (the board and administration), health
promotion (the Early Years Team, Health Promotion
scholars and the Multicultural Initiative) and disease
management/service integration (the GP Liaison
team, Information Management Initiative and
Optimal Health Team). A One Way ANOVA test
showed that consensus and participation tended to be
higher for the board than the other teams, but the
differences were not significant.
THINKING SPATIALLY, ACTING COLLABORATIVELY - A GIS-based Health Decision Support System for
Improving the Collaborative Health-planning Practice
151
Participants were then grouped into two major
age groups: 1) 0-40; 2) 40+. A One Way ANOVA
revealed a significance difference in the
accumulated means for the following variables,
participation, consensus and satisfaction with
information. Evidence-based decision-making
showed a trend towards significance. Specifically,
the younger age group reported lower scores on all
four key variables.
When grouped according to their duration of
membership in the LBHC, no significant differences
were found on any variables. The tenure groups
were constructed as follows: those who were new to
the LBHC (less than 12 months), intermediate
members (12-24 months) and veterans (more than 24
months). One Way ANOVA showed no significant
difference in the accumulated means. However, new
members and the veterans tended to report higher
scores than the intermediate age group. We then
tested the difference between accumulated means on
our four key variables across gender groups, with no
significant differences. Males tended to report higher
scores than females, but only represented 30% of our
sample.
The qualitative data provided by members
revealed further detail that might explain the
quantitative findings. For instance, one participant
noted that, ‘Very few decisions have ever been made
by the Board - most decisions are made by a few
outside the meeting, and therefore there is no rigour
or transparency to the processes’. Another
participant commented on the relative absence of
decision-making: ‘I'm not sure if any actual
planning for the future is made, with the exception
Table 1: Means, Standard Deviations and Frequencies of Responses to the 7 Domains of Decision-Making.
Dimension
Mean Standard
deviation
Not at all A Little Some Moderately Often Mostly Completel
y
Perceivedevidence‐
baseddecision‐making
4.33 2.18 3
(1.8%)
18
(11.0%)
27
(16.6%)
40
(24.5%)
32
(19.6%)
35
(21.5%)
8
(4.9%)
Perceivedconsensusof
decision‐making
4.55 2.24 4
(3.2%)
14
(11.1%)
17
(13.5%)
27
(21.4%)
18
(14.3%)
29
(23.0%)
17
(13.5%)
Perceivedparticipation
indecision‐making
4.80 2.32 4
(3.8%)
9
(8.7%)
14
(13.5%)
14
(13.5%)
20
(19.2%)
21
(20.2%)
22
(21.2%)
Perceivedsatisfaction
withinformationfor
decision‐making
3.49 2.22 50
(14.9%)
55
(16.4%)
68
(20.3%)
55
(16.4%)
56
(16.7%)
50
(14.9%)
1
(.3%)
Perceivedimportance
ofdecision‐making
4.63 2.27 0
(0%)
9
(9.2%)
23
(23.5%)
17
(17.3%)
10
(10.2%)
24
(24.5%)
15
(15.3%)
Perceivedequityof
decision‐making
4.77 2.31 6
(7.2%)
3
(3.6%)
6
(7.2%)
9
(10.8%)
30
(36.1%)
23
(27.7%)
6
(7.2%)
Perceivedeffectiveness
ofdecision‐making
3.83 2.26 8
(8.2%)
13
(13.4%)
16
(16.5%)
24
(24.7%)
17
(17.5%)
18
(18.6%)
1
(1.0%)
Table 2: Comparison of selected four key variables with LBHC major age groups.
LBHC Affiliation by two
major groups
Perceived evidence-based
decision-making
Perceived consensus of
decision-making
Perceived participation of
decision-making
Perceived satisfaction with
information of decision-
making
0-40 - young
Mean = 3.9
Std. Deviation = 1.1
N = 11
Mean = 3.6
Std. Deviation = 1.4
N = 11
Mean = 3.7
Std. Deviation = 1.1
N = 11
Mean = 2.3
Std. Deviation = 1.5
N = 10
40+ veterans
Mean = 4.7
Std. Deviation = 0.8
N = 13
Mean = 5.0
Std. Deviation = 1.2
N = 13
Mean = 5.4
Std. Deviation = 1.4
N = 14
Mean = 4.5
Std. Deviation = 1.3
N = 13
Statistics details
DF = 1
F = 3.7
SIG = .066
*non-significant(trended
towards significant)
DF = 1
F = 5.9
SIG = .02
* significant
DF = 1
F = 9.6
SIG = .005
* significant
DF =1
F = 13.8
SIG = .002
* significant
HEALTHINF 2011 - International Conference on Health Informatics
152

of recent 'planning sessions'. The lack of control
over decisions made by the coalition was a recurrent
theme in the qualitative comments; ‘I thought a
decision had been made prior to our input’.
However, the majority of comments made by
coalition members revealed the difficulty associated
with making decisions in the absence of adequate
information.
‘[We] need to identify priority actions, need
to be more pro-evidence in our decision
making’.
‘There is a serious lack of information and
communication [to guide decision-making] ‘.
The value of evidence-based decisions was clear
throughout the data; ‘If the LBHC goes down the
pathway of prioritising strategic directions based on
evidence, inclusive decision making processes
(including community input), this will have great
potential to more appropriately address [the]
issues’.
Despite high scores on consensus and
participation, some members noted that problems
existed in relation to the sense of connectedness of
the coalition “as a whole” and that this had a
significant impact on decision-making.
8 DISCUSSION
AND FUTURE RESEARCH
The preliminary quantitative and qualitative findings
of this study confirm that overall there were low
levels of satisfaction with the decision-making
processes across the LBHC. However, some groups
within the LBHC were more satisfied than others
(i.e., those who were over 40 years). There was also
a tendency for LBHC board members, males, new
members and veterans to be more satisfied with
information and perceive higher levels of consensus,
participation and evidence-based decision-making.
The data suggested that the lack of satisfaction with
information for decision-making may be due to the
complete lack of evidence on which to base
decisions. This lack of evidence seemed to
contribute to a sense of disconnectedness between
the different elements of the LBHC. For example,
some elements in the LBHC perceived that the
decision-making processes were not being practiced
consensually and in a participatory manner. The data
indicated that within some groups (i.e., Board), there
were high levels of consensus and participation, but
that this may not occur across the whole LBHC.
Further, there was an overall sense that decisions
were ineffective, presumably because they were not
based on information or evidence.
Although not significant, there was some
diversity across the components of the LBHC. Males
tended to be more satisfied as did those who had
been members of the LBHC for either longer or
shorter periods. This finding indicates the likelihood
of an acculturation curve for members (i.e., new
members are enthusiastic, but become more critical
of decision-making over time and then eventually
resolve this situation in some way – either by
withdrawing or seeking other sources of
information). Age of members had an important
influence on the way decision-making was
perceived. It is possible that younger people could
be more demanding in terms of their need for
involvement in the decision-making processes,
whereas veterans are likely to have access to more
intrinsic sources of information based on years of
experience in the region. As a result, they may be
less demanding of the decision-making processes.
As for the variation across the LBHC, the tendency
towards significant differences between the sub-
groups of the LBHC indicates that there may be
considerable diversity in decision-making that may
require different approaches to planning.
In summary, our findings have shown that there
is some diversity in the way members of a LBHC
view decision-making. They have also highlighted
the need for a comprehensive information
framework and collaborative process to underpin
planning for healthy cities, thus enabling health
coalitions to make effective decisions that engage all
stakeholders equitably. The framework proposed in
this paper would not only encourage planners to
engage with evidence and information about the
entire range of health determinants, but would also
provide a platform for collaboration and shared
engagement in the decision-making process.
Questions about how the framework and method are
actually applied in local communities, the impact of
the DSS on decision-making and its ability to
facilitate collaborative-based health planning,
remain unanswered and form the basis of this
ongoing research. These important research
questions will be addressed in the near future.
ACKNOWLEDGEMENTS
This study is part of a broader ARC project named:
Coalitions for Community Health: A Community-
based Response to Chronic Disease. The authors
would like to acknowledge the investigators of this
THINKING SPATIALLY, ACTING COLLABORATIVELY - A GIS-based Health Decision Support System for
Improving the Collaborative Health-planning Practice
153

project, Elizabeth Kendall, Scott Baum, Heidi
Muenchberger and Tan Yigitcanlar.
REFERENCES
Bennett, C, Graham, ID, Kristjansson, E, Kearing, S. A.,
Clay, K. F. & O'Connor, A. M. (2010) Validation of a
Preparation for Decision Making Scale. Patient
Education and Counseling 78: 130-133 Elsevier.
Bishop, P. and Davis, G. (2001). Developing consent:
consultation, participation and governance. In Are You
Being Served? Eds. G. Davis and P. Weller. Sydney,
Allen & Unwin: 175–195.
Campbell, S. and Fainstein, S. S. (1996). Introduction: the
structure and debates of planning theory. In Readings
in urban theory, Eds. S. Campbell and S.S. Fainstein.
Oxford, Blackwell Publishing:1-16.
Cromley, E. K. and McLafferty, S. L. (2003). GIS and
public health. Health & Place 9(3): 279.
Dean J. R., J. W. and Sharfman, M. P. (1993). Procedural
rationality in the strategic decision-making process.
Journal of Management Studies 30(4): 587-609.
Duhl, L. J., & Sanchez, A. K. (1999). Healthy cities and
the city planning process. A Background
Documentation On Links Between Health And Urban
Planning, Copenhagen, WHO, Regional Office For
Europe.
Dur, F., Yigitcanlar, T. and Bunker, J. (2009). A decision
support system for sustainable urban development: the
integrated land use and transportation indexing model.
Proceedings of the Postgraduate Infrastructure
Conference. Brisbane, Australia, 26 March.
Queensland University of Technology.
Flood, P., Hannan, E., Smith, K., Turner, T., West, M., &
Dawson, J. (2000). Chief executive leadership style,
consensus decision making, and top management team
effectiveness. European Journal of Work &
Organizational Psychology 9(3), 401-420.
Flynn, B. C. (1996). Healthy cities: toward worldwide
health promotion. Annual Review of Public Health 17:
299-309.
Gudes, O., Kendall, E., Yigitcanlar, T., Pathak, V. and
Baum, S. (2010). Rethinking health planning: a
framework for organising information to underpin
collaborative health planning. Health Information
Management Journal 39 (2): 18-29.
Han J. H., Kendall, E., Sunderland, N., Gudes, O. and
Henniker, G. (2010) Chronic disease, geographic
location and socioeconomic disadvantage as obstacles
to equitable access to e-health. Health Information
Management Journal 39 (2): 30-36.
Healthy Cities Illawarra (2010). Working with the
community for a healthier, safer, greener and more
caring Illawarra. Wollongong: Illawarra city council.
Available at: http://www.healthycitiesill.org.au/
contactus.htm (Accessed 10 October 2010).
Higgs, G. and Gould, M. (2001). Is there a role GIS in the
'new NHS'? Health & Place 7(3): 247-59.
Mooney, G. and Fohtung, N.G. (2008). Issues in the
measurement of social determinants of health. Health
Information Management Journal 37(3): 26-30.
Murray, D. J. (2006). A critical analysis of communicative
planning theory as a theoretical underpinning for
integrated resource and environmental management.
Unpublished PhD thesis, Griffith University,
Queensland.
National Electronic Decision Support Taskforce. (2008).
Electronic Decision Support Systems Report.
Department of Health and Ageing. Canberra:
Australia.
NHHRC (2009). A healthier future for all Australians.
Canberra, ACT, National Health and Hospitals Reform
Commission.
Northridge, M. E., Sclar, E. D. and Biswas, P. (2003).
Sorting out the connections between the built
environment and health: a conceptual framework for
navigating pathways and planning healthy cities.
Journal of Urban Health 80(4): 556-568.
Parnell, J. A. and Bell, E. D. (1994). ‘The propensity for
participative decision making scale: A measure of
managerial propensity for participative decision
making.’ Administration & Society 25(4): 518-533.
Reeves, P. N. and Coile, R. C (1989). Introduction to
health planning. Arlington, VA: Information
Resources Press.
Reinke, W. A. (1972). Health planning: qualitative
aspects and quantitative techniques. Baltimore, MD:
Johns Hopkins University School of Hygiene and
Public Health, Department of Internet Health.
Schulz, A. and Northridge, M.E. (2004). Social
determinants of health: implications for environmental
health promotion. Health Education & Behaviour
31(4): 455-471.
Turban, E. (1993). Decision support and expert systems:
management support systems: Prentice Hall PTR
Upper Saddle River, NJ, USA.
Wave, V. (2009). mHealth for development: the
opportunity of mobile technology for healthcare in the
developing. United Nations Foundation and Vodafone
Foundation.
WHO (1997). Twenty steps for developing a healthy cities
project. WHO Regional Office of Europe.
WHO (1999). Health: creating healthy cities in the 21st
century. In The Earthscan reader in sustainable cities.
Ed. D, Satterthwaite. London, Earthscan: 137–172.
WHO (2010). Urban health Healthy Cities. Available at:
http://www.euro.who.int/en/what-we-do/health-
topics/environmental-health/urban-
health/activities/healthy-cities (Accessed 9 October
2010).
HEALTHINF 2011 - International Conference on Health Informatics
154
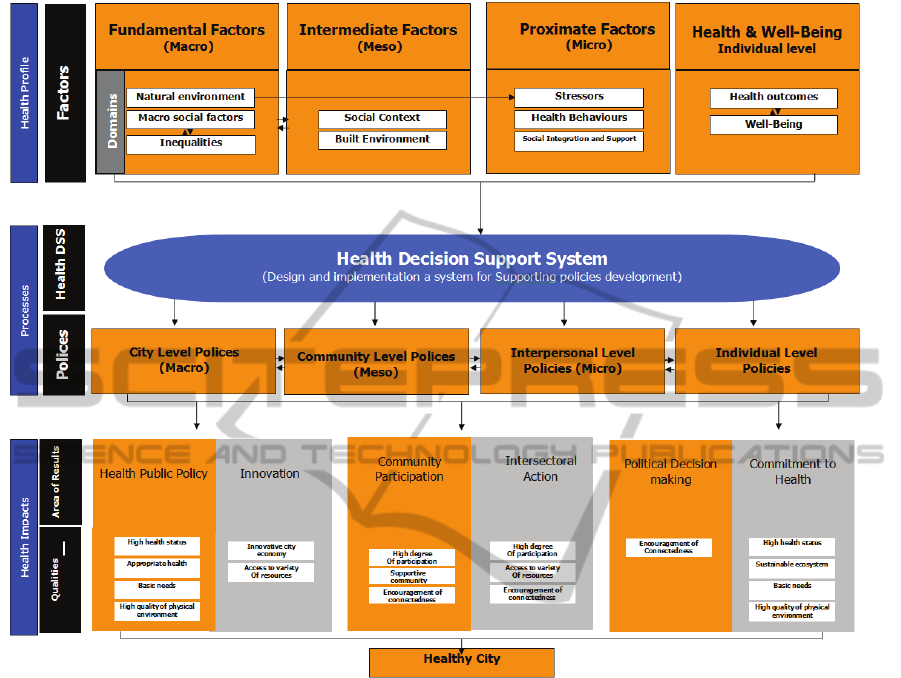
APPENDIX
Appendix: A conceptual framework for planning a healthy city (Modified after World Health Organization 1997; Schulz &
Northridge 2004).
THINKING SPATIALLY, ACTING COLLABORATIVELY - A GIS-based Health Decision Support System for
Improving the Collaborative Health-planning Practice
155
