
LIGHT TRANSMISSION THROUGH GAUZE PAD SOAKED
WITH BLOOD OR LIQUIDS TO DETECT VENOUS NEEDLE
DISLODGEMENT
Akihiro Takeuchi, Kai Ishida
Department of Medical Informatics, School of Allied Health Sciences, Kitasato University, Kitasato, Sagamihara, Japan
Graduate School of Medical Sciences, Kitasato University, Kitasato, Sagamihara, Japan
Yasuo Morohoshi, Toshihiro Shinbo, Minoru Hirose, Noriaki Ikeda
Department of Laboratory Animal Science, Kitasato University School of Medicine Kitasato, Sagamihara, Japan
Department of Clinical Engineering, School of Allied Health Sciences, Kitasato University, Kitasato, Sagamihara, Japan
Department of Medical Informatics, School of Allied Health Sciences, Kitasato University, Kitasato, Sagamihara, Japan
Keywords: Venous needle dislodgement (VND), Photo sensor, Light transmission, Gauze pad.
Abstract: Accidents during hemodialysis such as a large amount of blood loss are often caused by venous needle
dislodgement. To develop a bleeding sensor based on a photo sensor, we studied effects of liquids and
porcine blood on light transmission through a thin gauze pad. The photo sensor consisted of an ordinary
electrical circuit, a light emitting diode (lambda max = 645 nm), a photo diode, and a thin gauze pad placed
between the diodes. The light transmitted through the gauze pad soaked with liquids or porcine blood was
measured with a digital voltmeter. The liquids on a gauze pad, significantly increased the voltage (light
transmission) from 0.33 +/- 0.004 V (SD) to 0.63 +/- 0.02 V (minimum, by reverse osmosis water) and to
0.70 +/- 0.03 V (maximum, by 50% glucose). The porcine blood significantly decreased the voltage from
0.33 V to 0.21 +/- 0.02 V in Hct 40%, to 0.27 +/- 0.02 in Hct 30%, to 0.30 +/- 0.02 V in Hct 20%. We
confirmed that liquids significantly increased light transmission through the gauze pad, but porcine blood
decreased light transmission. This opposite response can be used to distinguish liquids from blood on a
gauze pad.
1 INTRODUCTION
Over the past three decades, hemodialysis has
evolved into a safe and less stressful procedure for
both patients and caregivers (Sarkar,
Kaitwatcharachai and Levin, 2005; Hawley,
Jefferies, Nearhos and Van Eps, 2008). However,
intradialytic complications still cause considerable
patient morbidity and rarely, mortality (Sarkar et al.,
2005). Venous needle dislodgment (VND) is one of
the most serious accidents that can occur during HD
(PMID9859033, 1998; Hawley et al., 2005; Van
Waeleghem, Chamney, Lindley and Pancírová,
2008). The FDA has some statistics on cases of fatal
blood losses but the known numbers are probably
too low to reflect the real figures (Ahlmén, Gydell,
Hadimeri, Hernandez, Rogland and Strömbom,
2008). Ahlmén et al. estimate the incidence of
venous-needle dislodgements of 0.1% is merely an
approximation over a short period (Ahlmén, et al.,
2008). Although certain devices monitoring venous
pressure (Hertz, Joensson, Sternby), pressure pulse
(Goldau, Fresenius Medical Care Deutschland
GmbH) and moisture (Pierratos and Lugonzo, 2009)
(DRI Sleeper® Dr. Page. Retrieved Aug 20, 2009)
have been developed, tested and patented, a “VND
sensor” has been requested by patients and medical
professionals (European Dialysis and Transplant
Nurses Association/European Renal Care
Association (EDTNA/ERCA, 2005) has produced
12 practice recommendations to help reduce the risk
of VND and detect blood leakage as early as
possible (Van Waeleghem et al., 2008). A device
that uses fiber optic technology to detect blood has
been approved (CE marked) as a Class I medical
174
Takeuchi A., Ishida K., Morohoshi Y., Shinbo T., Hirose M. and Ikeda N. (2010).
LIGHT TRANSMISSION THROUGH GAUZE PAD SOAKED WITH BLOOD OR LIQUIDS TO DETECT VENOUS NEEDLE DISLODGEMENT.
In Proceedings of the Third International Conference on Biomedical Electronics and Devices, pages 174-177
DOI: 10.5220/0002738801740177
Copyright
c
SciTePress

device with the intended purpose of detecting VND
in extracorporeal circuits (Ahlmén J et al., 2008;
Van Waeleghem et al., 2008). The device has also
been granted FDA approval and is now available for
sale in the United States. However, other detection
systems are still under development at the present
time (Van Waeleghem et al., 2008).
Although there was no observed event that led to
dislodgement of the needle in most reported
episodes (Sandroni, 2005), the oozing of blood has
commonly been noticed on a tape or small gauze at
the needle site in hemodialysis (Lindsay, Burton,
1972; Salaman, 1971; Sandroni, 2005). The oozing
may be due to a brittle vessel and skin in chronic
renal failure patients. The oozing decreases the
adhesiveness between the tape and skin and could
lead to needle dislodgement. A small piece of gauze
is used to absorb the oozing blood at a needle site
and to avoid bloody soiling of clothes and bed sheets.
We attempted to sense the small amount of blood
on a small gauze pad that covers the needle site. A
direct electronic sensor such as moisture or enuresis
detector is not suitable in Japan because they could
cause micro electrification. Processing an optical
fiber to a blood sensor is technically difficult for our
laboratory, and the fiber is already used in the
convenient device above. Although it is easy to
imagine that light transmission through gauze might
be changed by blood, we could not find a practical
report of light transmission affected by blood or
other liquids.
To detect an accidental bleed in hemodialysis, we
made a photo sensor module to measure light
transmitted through gauze pad and studied the
effects of blood and liquids on a light transmission.
2 METHODS
2.1 Light Sensory Module
The sensory module consists of a light emitting
diode (LED, lambda max = 645 nm, 55 mcd,
HLMP-Q105), a photo diode (PD, spectrum 600-
1050 nm, DIL-BPW34) on a simple circuit that is
commonly used in light/dark sensors (Figure 1). The
Figure 1: The circuit of photo sensor module.
PD changes its resistance depending on the intensity
of the light transmitted. The voltage across the
resistance R2 (12 k ohm) increases when the light is
bright and decreases when it is dark. The voltages
are measured with a digital voltmeter. The LED and
PD are attached at the edges of a plastic clip and
sealed with bond to avoid any short-circuits that
could be caused by the liquids. The voltages were
not changed by any background illumination such as
that from a desk lamp because the strong LED light
was shown directly through the gauze pad to the PD.
2.2 Gauze Pad and Test Medium
Loose weave pads was a piece of gauze (Blood Ban,
L size, Yutoku Pharmaceutical Industry, Ltd., Japan)
used after collecting blood or administering infusion
such as a “BAND-AID.”
Test mediums in the amount of 0.3 ml were
manually dropped in the center of the gauze pad
(Figure 2). The applied liquids were a reverse
osmosis water, physiological saline, and glucose in
water at 5%, 10%, 20%, 40% and 50%. Porcine
plasma and blood were also applied and tested in the
same manner. The hematocrits (40%, 30% and 20%)
were prepared by adding porcine plasma but not
saline. The porcine blood was obtained from a
slaughterhouse (Tokyo Shibaura Zoki Ltd., Tokyo
Japan).
2.3 Statistics
For each liquid, seven measurements were collected
and presented with a mean and SD. For each porcine
blood, five measurements were averaged as one
value. Nine values were collected for each blood
sample and presented with a mean and SD. They
were statistically compared with the control values
using unpaired Student’s t-test. A probability level
of P < 0.05 was considered to indicate statistical
significance.
LIGHT TRANSMISSION THROUGH GAUZE PAD SOAKED WITH BLOOD OR LIQUIDS TO DETECT VENOUS
NEEDLE DISLODGEMENT
175

Figure 2: Experiment of dropping porcine blood on a tight
weave pad thin gauze pad.
3 RESULTS
Mean voltage was 0.332 +/- 0.004 V under control
condition. Liquids and porcine plasma increased the
voltages from 0.332 +/- 0.004 V to 0.634 +/- 0.018
V (minimum, by a reverse osmosis water) and to
0.703 +/- 0.027 V (maximum, by 50% glucose)
(Figure 3). The light transmitted through the gauze
pad was increased by liquids or plasma. There was a
higher concentration of glucose the more the light
transmission increased. Porcine blood decreased the
voltage from 0.332 V to 0.214 +/- 0.019 V in 40%
Hct, to 0.271 +/- 0.023 in 30% Hct, to 0.304 +/-
0.019 V in 20% Hct. The higher the concentration of
Hct, the more the light transmission decreased.
4 DISCUSSION
Studies of incidents showed that the typical scenario
of VND episodes happened in apparently routine
treatments and with fully staffed units (Sandroni,
2005). Although a needle and needle tubing are
stabilized with an adhesive fabric and the “chevron”
technique (Van Waeleghem et al., 2008), VND
occurs in hemodialysis. In the present state, medical
staffs are required to find accidents as quickly as
possible.
Liquids or plasma increased light transmission
through gauze pad. It may be the same effect as
when light is seen through a wet shirt. A part of the
light from a light source, the LED, was scattered
outward in the gauze as a bulk scatter. The residuals
hit the PD. The liquids dropped on the gauze pad
could reflect the light traveling inward. The light
transmissions increased proportionally to the glucose
concentrations. The relationship is probably due to
the Beer-Lambert’s law.
Porcine blood clearly decreased the light
transmission through the gauze pad. The decreases
were related to their hematocrits. The absorbance of
light at a wavelength 645 nm was interpreted by a
higher concentration of haemoglobin. The opposite
response of light transmission caused by liquids or
blood may be used in theory to distinguish blood
from liquids such as sweat, infusion drip, urine,
saliva, or leaching solution. Although we have
attempted to develop a monitor tool to detect
bleeding in hemodialysis, the device may be used for
monitoring VND during a continuous intravenous
infusion for a relatively long time. In such a case,
even if venous blood flows and mixes at the needle
site, the infusion volume may be larger than that of
venous blood. It would be more desirable if the
device could quickly detect any change from the
control level rather than an absolute value of the
light transmission.
Although the optical device of Ahlmén et al.
(2008) can find a minute amount of blood (about 1
ml), it may be difficult to distinguish oozing from
bleeding. Our procedure may control the sensing
volume by an arbitrarily set gauze volume or
distance between the needle site and the sensor on a
gauze pad.
This study proved that the light was absorbed in
gauze pads with hemoglobin and that light
transmission increased in wet gauze pads without
hemoglobin. Although we should confirm that the
phenomenon is ordinary shown in other kinds of
gauze pad, more thin or thick, this fundamental
study will promote the development of simple
practical bleeding sensors to monitor hemodialysis
and continuous infusion. In a future plan, we will
consider a disposable or re-usable LED and PD
device to completely avoid any infection and short-
circuits, a power supply for four-hour hemodialysis
a day, three times a week, and how to alarm an event
to notify medical staffs.
5 CONCLUSIONS
We confirmed that liquids on a gauze pad
significantly increased light transmission through the
gauze pad, but porcine blood decreased light
transmission. These opposite effects of light
transmission through the gauze pad can be used to
distinguish liquids from blood on the gauze pad with
the bleeding sensor.
BIODEVICES 2010 - International Conference on Biomedical Electronics and Devices
176
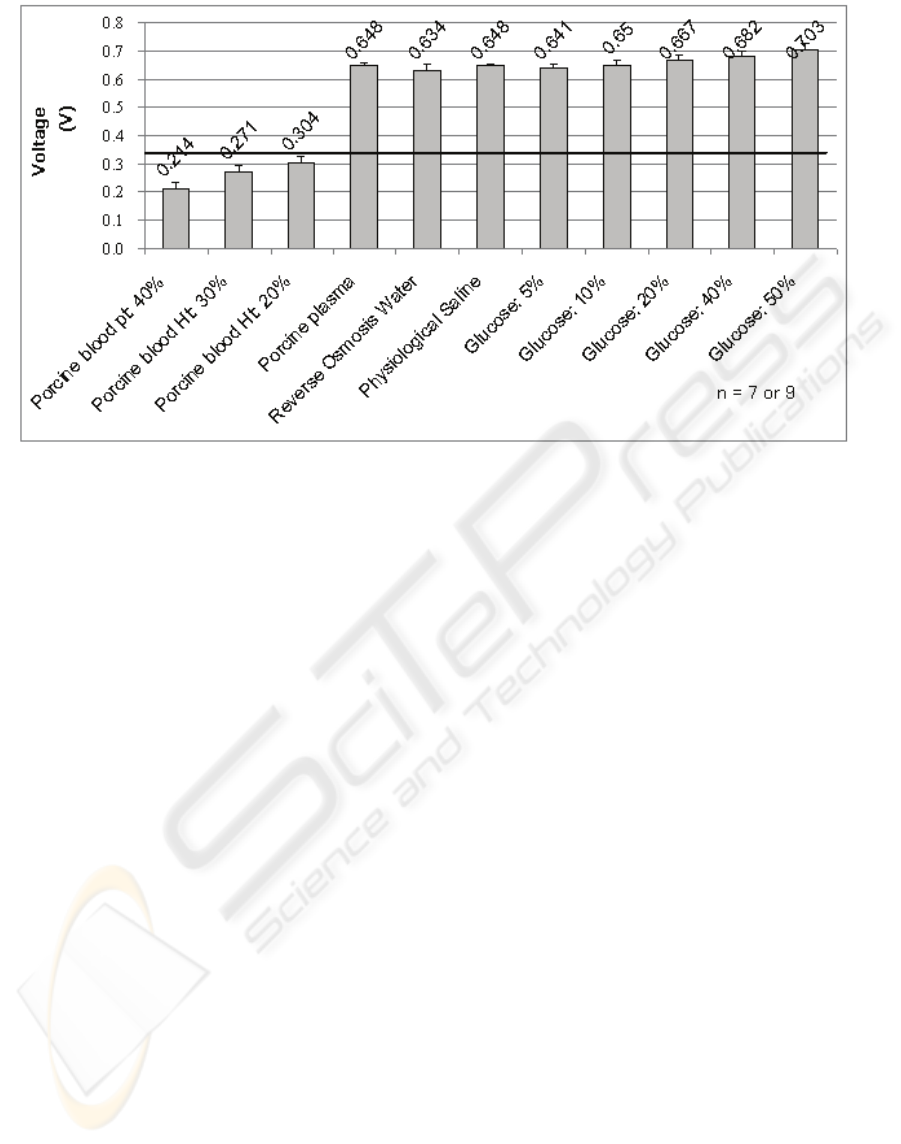
Figure 3: Voltages across R2 with porcine blood and liquids in the gauze pad. Horizontal line 0.332 V shows the value at
the control condition.
REFERENCES
Sarkar, S., R., Kaitwatcharachai C., Levin N. W., 2005.
Complications during Hemodialysis. In: Nissenson
AR, Fine RN, (eds.), Clinical Dialysis. 4th ed (pp.
237-272), New York, NY: Mcgraw-Hill.
Hawley, C., M., Jefferies, J., Nearhos J., Van Eps C., 2008.
Complications of home hemodialysis. Hemodial Int,
12(Suppl 1), S21-S25.
PMID9859033, 1998. Undetected venous line needle
dislodgement during hemodialysis. Health Devices, 27,
404-406.
Van Waeleghem, J., P., Chamney, M., Lindley, E., J.,
Pancírová, J., 2008. Venous needle dislodgement: how
to minimise the risks. J Ren Care, 34, 163-168.
Ahlmén, J., Gydell, K., H., Hadimeri, H., Hernandez, I.,
Rogland, B., Strömbom, U., 2008. A new safety
device for hemodialysis. Hemodial Int, 12, 264-267.
Hertz, T., Joensson, S., Sternby, J., inventors. Gambro, A.
B., assignee., 2008. Method and arrangement for
detecting the condition of a blood vessel access. US
patent 6090048.
Goldau, R., inventors. Fresenius Medical Care
Deutschland GmbH, assignee., 2008. Method and
device for monitoring a vascular access during a
dialysis treatment. US patent 6077443.
Pierratos, A., Lugonzo, P., 2009. Overnight Success
Provides International Inspiration, Nocturnal
Hemodialysis at Humber River Regional Hospital.
Retrieved Aug 20, 2009, from
http://www.longwoods.com/website/jobsite/HQ61Hu
mber.pdf.
DRI Sleeper® bedwetting treatment alarms by Dr. Page.,
2009. Retrieved Aug 20, 2009, from http://www.dri-
sleeper.com/.
2005/2 EDTNA/ERCA Journal Club Discussion
Summary., 2005. Retrieved Aug 20, 2009, from
http://www.edtnaerca.org/pages/education/journalclub
/summary2005_2.php.
Sandroni, S., 2005. Venous needle dislodgement during
hemodialysis: An unresolved risk of catastrophic
hemorrhage. Hemodial Int, 5, 102-103.
Salaman, J., R., 1971. Bleeding from dialysis shunt sites.
Br Med J, 2, 711.
Lindsay, R., M., Burton, J., A., 1972. Blood loss from
cannulation sites during haemodialysis. Scott Med J.,
17, 266-269.
LIGHT TRANSMISSION THROUGH GAUZE PAD SOAKED WITH BLOOD OR LIQUIDS TO DETECT VENOUS
NEEDLE DISLODGEMENT
177
