
DECISION SUPPORT AND IMAGE & SIGNAL ANALYSIS IN
HEART FAILURE
A Comprehensive Use Case
Sara Colantonio, Massimo Martinelli, Davide Moroni, Ovidio Salvetti
Inst. of Information Science and Technologies,ISTI-CNR, Pisa, Italy
Francesco Perticone, Angela Sciacqua
Univerity Magna Graecia, Catanzaro, Italy
Franco Chiarugi
Institute of Computer Science (ICS), Foundation for Research and Technology – Hellas (FORTH)
Heraklion, Crete, Greece
Domenico Conforti, Antonio Gualtieri, Vincenzo Lagani
University of Calabria, Cosenza, Italy
Keywords: Decision Support Theory, Echocardiographic Imaging Analysis, Signal Processing.
Abstract: The European STREP project HEARTFAID aims at defining an innovative platform of services able to
intelligently support clinical operators in the daily management of heart failure patients. The core of the
platform intelligence is a Clinical Decision Support System, developed by integrating innovative knowledge
representation techniques and hybrid reasoning methods, and including advanced tools for the analysis of
diagnostic data, i.e. signals and images. Aiming at showing how all these issues are combined in the
HEARTFAID platform, we present a comprehensive use case, centred on echocardiography workflow and
covering the clinical course leading from visit scheduling to therapeutic choices, highlighting the
intervention and the value added by the Clinical Decision Support System.
1 INTRODUCTION
Heart Failure (HF) is a complex clinical syndrome
resulting from any structural or functional cardiac
disorder which impairs the ability of the ventricle to
fill with or eject blood. In its chronic form, HF is
one of the most remarkable health problems for
prevalence and morbidity, especially in the
developed western countries, with a strong impact in
terms of social and economic effects. All these
aspects are typically emphasized within the elderly
population, with very frequent hospital admissions
and a significant increase of medical costs. Recent
studies and experiences have demonstrated that
accurate heart failure management programs, based
on a suitable integration of inpatient and outpatient
clinical procedures, might prevent and reduce
hospital admissions, improving clinical status and
reducing costs.
The European project HEARTFAID (“A
knowledge based platform of services for supporting
medical-clinical management of the heart failure
within the elderly population'” — IST-2005-027107)
aims at defining efficient and effective health care
delivery organization and management models for
the “optimal” management of the care in the field of
cardiovascular diseases.
The HEARTFAID platform (HFP) has been
conceived as an integrated and interoperable system,
able to guarantee an umbrella of services that range
from the acquisition and management of raw data to
the provision of effective decisional support to
288
Colantonio S., Martinelli M., Moroni D., Salvetti O., Perticone F., Sciacqua A., Chiarugi F., Conforti D., Gualtieri A. and Lagani V. (2008).
DECISION SUPPORT AND IMAGE & SIGNAL ANALYSIS IN HEART FAILURE - A Comprehensive Use Case.
In Proceedings of the First International Conference on Health Informatics, pages 288-295
Copyright
c
SciTePress

clinicians. All the functionalities and services
supplied by the entire HFP can be further grouped
into data, decision and end-users macro “contexts”.
The former is devoted to the collection and
management of information, which consists of
biomedical data, acquired from biomedical devices
and structured/unstructured information such as
clinical reports collected during patient
hospitalisation and outpatient visits and within a
homecare program by telemonitoring patients’
conditions. The decision context includes a
knowledge-based Clinical Decision Support System
(CDSS) whose main goal is supporting the HF
health care operators, by making more effective and
efficient all the processes related to diagnosis,
prognosis, therapy and health care personalization of
the HF patients. The latter context provides the
doorway to a multitude of end-user utilities and
services, such as accessing an electronic health
record, querying the CDSS, applying advanced
models and methods for the extraction of new
knowledge, and so forth.
The CDSS represents the core of HFP and has
been carefully designed by combining innovative
knowledge representation formalisms,
robust and
reliable reasoning approaches, based on Machine
Learning and inference methodologies, and
innovative methods for diagnostic images analysis
and biomedical signals processing (VV.AA., 2007).
This paper aims at showing how all these issues
are combined within a comprehensive use case,
centred on an echocardiography workflow and
covering the clinical course leading from visit
scheduling to therapeutic choices, highlighting the
intervention and the value added by the CDSS.
In the following sections, we will briefly review
the related literature, then introduce the
HEARTFAID CDSS and its main functionalities,
and, finally, describe the use case and CDSS
interventions.
2 DECISION SUPPORT AND
DATA PROCESSING IN
HEARTFAID
The development of computerized applications for
supporting health care givers is an old but still alive
quest, started more than 45 years ago, in the early
1960s, and with ascending and descending periods
of interest and growth (Greenes, 2007).
A plethora of CDSS has already evolved with
different platforms and architectures, encompassing
a variety of services, from information retrieval and
reporting, scheduling and communications, to cost-
effectiveness, error prevention, safety, and
improvement of health care quality. The most
common realizations include electronic
medical/patient records (Poissant et al., 2005),
computerized alerts and reminders, clinical
guidelines formalizations (GEM, 2003), provider
order entries (Park et al., 2005), diagnostic support,
clinical result interpretation, adverse event
monitoring, shared patient-doctor decision-making
(Wirtz et al., 2006).
The primary task for developing effective CDSS
is to select the corpus of pertinent knowledge and/or
collect and process data to create pertinent
knowledge which is relevant for bringing the health
care to effect. Knowledge representation just
concerns understanding, designing, and
implementing ways of formally coding the
knowledge necessary for deriving other knowledge,
planning future activities, solving problems that
normally require human expertise. Representing
knowledge requires the selection of a suitable
language or formalism and the definition of a
Knowledge Base (KB) built by formalizing clinical
experts’ know-how and guidelines. Usually, the
formalism is symbolic and the KB contains
statements or expressions of one of the following
formalisms: (i) rule based; (ii) frame based; (iii)
network based; and (iv) logic based (Helbig, 2006).
Workflow based representation is also becoming
well-known, especially for modelling guidelines
(Boxwala et al., 2004). Moreover, in recent years
ontologies are emerging as a powerful knowledge
representation formalism which is conceptually
equivalent to the frame based and to first order logic
approach (Bayegan et al., 2002).
The KB is exploited by a reasoning engine
which processes available information for
formulating new conclusions and answering
questions. Inferential reasoning is employed for
inferring new knowledge from the KB by deduction,
induction or abduction.
In some cases, making a decision requires an
investigation on the hidden, complex, often non-
linear correlations among data, together with high-
level analytical processing functions. In such cases,
the knowledge needed for the solution should be
acquired directly from data (inductive knowledge)
and stored in a model (e.g. Artificial Neural
Networks, Support Vectors Machines), able to
induce sub-symbolic knowledge by data-driven
processing. Computational models are also useful
for representing uncertain knowledge, as Bayesian
Networks and Fuzzy theory.
HF routine practice presents several aspects in
which an automatic, computer-based support could
have a favourable impact. Some attempts to support
HF clinical operators have been presented, such as
DECISION SUPPORT AND IMAGE & SIGNAL ANALYSIS IN HEART FAILURE - A Comprehensive Use Case
289

an Electronic Patient Record (Bosmans et al., 2000)
or computerized guidelines (Dassen et al., 2003).
More complex decision support systems have been
developed for suggesting the most appropriate
therapy (e.g. Perlini et al., 1990).
Within HEARTFAID, a careful investigation
about the needs of HF practitioners and the effective
benefits assured by decision support was performed:
four problems have been identified as highly
beneficial of HEARTFAID CDSS point-of-care
intervention. They can be referred as macro domain
problems and listed up as: (i) HF diagnosis, (ii)
prognosis, (iii) therapy planning, and (iv) follow-up.
Further detailed decision problems were identified
for specifying these macro domains, focusing as
much as possible on the medical users’ needs;
explicative examples are:
severity evaluation of heart failure;
identification of suitable pathways
planning of adequate, patient’s specific therapy;
analysis of diagnostic exams
early detection of patient’s decompensation.
An accurate analysis highlighted that the needed
corpus of knowledge mainly consisted of domain
know-how. Nevertheless, the solution of some of
these problems seemed still debated in the medical
community, due to the lack of validated and assessed
evidences. In such cases, computational models
appeared the best solution for modelling the decision
making extracting knowledge directly from available
data. Moreover, specific processing algorithms were
designed for analyzing diagnostic examinations. In
this perspective, HEARTFAID CDSS was designed
for combining different models of reasoning, as will
be described in the next sections.
2.1 Significance of Signal Acquisition
and Analysis in HF
Electrocardiography (ECG) is one of the very basic
examinations performed in the evaluation and
assessment of HF. According to ESC (2005)
guidelines, the negative predictive value of normal
ECG to exclude left ventricular systolic dysfunction
exceeds 90%.
The most common ECG examinations are the
“Resting ECG” and the “Holter ECG”. While the
latter is more commonly used for the discovery of
rhythm abnormalities and the computation of the
Heart Rate Variability (HRV), the former is more
commonly used for the evaluation of morphological
abnormalities in the PQRST shape.
In both examinations, the first step to be
performed is the QRS detection with the
identification of the time occurrences of each heart
beat. This series of data allows for the evaluation of
the heart rate and is preparatory to the beat
classification for the discrimination between normal
and abnormal beats. This task is usually performed
in the “Holter ECG” reading stations as a starting
point for the arrhythmias’ classification and for the
evaluation of the NN series (time intervals between
consecutive normal beats) that is the input for the
HRV evaluation. In case of “Resting ECG”
examination (typical duration is 10 seconds), the
evaluation of the normal beats allows the normal
beat averaging with the construction of a more
noise-free reference beat that can be used for a better
evaluation of wave durations and amplitudes.
Wave durations and amplitudes are paramount in
the evaluation of the “Resting ECG” (usually with
12 leads) parameters of high significance for the HF
patients like ST depression, QRS and QT durations,
Sokolow-Lyon index for left ventricular
hypertrophy, presence of left or right branch bundle
block and presence of pathological Q waves.
2.2 Significance of Imaging Techniques
and Image Processing in HF
Imaging techniques offer invaluable aid in the
objective documentation of cardiac function,
allowing for the computation of parameters relative
to chamber dimensions, wall thickness, systolic and
diastolic function, regurgitations and pulmonary
blood pressure.
According to ESC (2005), chest X-ray and
echocardiography should be included in the HF
initial diagnostic work-up. Further,
echocardiography will be regularly repeated to
monitor in an objective way the changes in the
clinical course of a HF patient. Additional
techniques, like nuclear imaging and cardiac
magnetic resonance, may be also considered for
particular patients, since they have not been shown
to be superior to echocardiography in the
management of most HF population.
Thus, echocardiography —and in particular 2-D
TransThoracic Echocardiography (TTE) for its
portability and versatility— is the key imaging
technique for the practical management of HF.
The most important measurement performed by
TTE is Left Ventricle Ejection Fraction (LVEF),
which permits to distinguish patients with cardiac
systolic dysfunction from patients with preserved
systolic function. LVEF is given by the normalized
(non-dimensional) difference between left ventricle
End-Diastolic Volume (EDV) and the End-Systolic
volume (ESV). Among different models for the
computation of such volumes, the American Society
of Echocardiography (Lang et al., 2005) suggests the
HEALTHINF 2008 - International Conference on Health Informatics
290

use of the so-called Simpson’s rule, by which the
left ventricle is approximated by a stack of circular
(or elliptical) disks whose centres lie in the major
axis. Simpson’s method, therefore, relies on left
ventricle border tracing. It is well-known that
manual border tracing, besides being time-
consuming, is prone to inter- and intra- observer
variability, and thus is unable to provide a
satisfactory and reproducible measurement of
LVEF.
Image processing techniques may relieve this
problem, by providing automated or, at least, semi-
automated methods for tracing contours of relevant
structures found in an image, an issue called image
segmentation in the specific literature. However, the
segmentation problem for ultrasound images is by
no means trivial, due mainly to low signal to noise
ratio, low contrast, and image anisotropy and
speckle noise (Noble and Boukerroui, 2006).
3 A SIGNIFICANT SCENARIO
HEARTFAID CDSS was designed after a careful
analysis of the problems to be faced and the
expectations of the medical users.
A complete use case was defined for guiding the
development activity of CDSS by considering many
of the integrated services of the platform.
More in detail, we are considering a 65 years old
patient, already enrolled in the HFP, former smoker,
suffering from hypertension for several years. The
patient was enrolled in the HFP six months ago and,
in particular, the telemonitoring services offered by
the platform were activated. At the baseline visit, the
patient referred a slight limitation of physical
activity, since he felt comfortable at rest but ordinary
activity resulted in fatigue and dyspnoea. For these
reasons, the patient was assigned to NYHA class II.
Anamnesis data were also collected, from which it is
known that the patient had an acute myocardial
infarction five years before and he underwent to
aorto-coronary bypass. The patient had a post
ischaemic dilated cardiomyopathy with associated
systolic dysfunction.
The TTE test (performed at baseline evaluation)
showed an LVEF equal to 40%, ESV and EDV
being respectively 114 ml and 190 ml. The left
ventricle end-diastolic diameter was 6.0 cm. The
pharmacological treatment consisted in ACE-
inhibitor, beta-blockers, spironolactone, aspirin and
statin. Neither pulmonary nor systemic congestion
signs were present. Blood examinations of renal
function and electrolytes were normal. During these
six months, the patient has been telemonitored. In
particular, the pharmacological therapy has been
followed with care and no relevant changes have
been detected by the platform.
Suddenly, the patient observes a worsening of
his symptoms, with a marked limitation of physical
activity. After he fills in a periodic questionnaire
suggested by the platform based on Minnesota
questionnaire, the changes in the symptoms are
automatically detected and considered relevant. A
medical visit is suggested by the CDSS, accepted by
the referent physician and immediately scheduled.
At the visit, the NYHA class changes from II to
III. No variations in the signs are observed by the
cardiologist, apart from a slight worsening of blood
pressure (150/90 mmHg) and an increase of 10
beats/min in the heart rate. An ECG is performed
also to confirm the heart rate increment.
The cardiologist, supported by the CDSS,
decides however to evaluate other parameters by
echocardiography. During the TTE examination, the
sonographer acquires images and images sequences
according to a protocol specified by the platform.
Finally the images and the parameters manually
evaluated by the sonographer are stored in the
platform image archive. The reviewing cardiologist
visualizes the echocardiographic images and the
estimated parameters. Left ventricle volume and
ejection fractions are computed again by automatic
methods, exploiting the available image sequences.
These values are compared with the historical data
of the patient. EDV increases to 210 ml, ESV
increases to 145 ml, EF decreased from 40% to 30%.
Mild tricuspidal insufficiency is Doppler-
detected by its regurgitation. By tricuspidal
regurgitation extent, the pressure gradient (mmHg)
between right ventricle and right atrium is measured.
Pulmonary pressure is then estimated. With this aim,
the subcostal view is taken into account, so as to
determine Inferior Vena Cava (IVC) diameter and its
collapsibility index. The pulmonary pressure is
estimated to be 40 mmHg, by using a lookup table
with entries consisting in the tricuspidal gradient,
IVC diameter and collapsibility index. Since this
value indicates a slight pulmonary congestion, the
CDSS suggests the physician to integrate the
pharmacological therapy with diuretics, for example
loop diuretics or thiazides. Further, since there are
no up-to-date information about the renal function
and electrolytes, the CDSS suggests to start with a
safe diuretic dosage and to perform blood
examinations, which are scheduled for few days
later. The physician opts for a loop diuretics therapy,
for quicker beneficial effects.
Back to his home, the patient is monitored in the
subsequent days. In particular control of weight,
urine output, blood pressure, symptoms are
scheduled daily. Blood examinations are scheduled
seven days after the beginning of the new treatment.
DECISION SUPPORT AND IMAGE & SIGNAL ANALYSIS IN HEART FAILURE - A Comprehensive Use Case
291

The results of such blood examinations are uploaded
to the platform.
An up-titration table for the diuretics is compiled
by the CDSS, considering in particular symptoms
and electrolytes balance, creatinine clearance, blood
pressure, weight slope and urine output. The CDSS
also suggests to control weight and urine output
daily and to schedule blood examinations weekly. A
visit is also suggested in one month, to appreciate
the response to the therapy. The physician reviews
this program and decides to approve it. After
approval, the up-titration table for diuretics is
automatically sent to the patient.
One week after, telemonitoring evidences
persistence of symptoms; the patient is thus required
to continue the up-titration program for diuretics.
During the subsequent weeks symptoms get better
until the visit. At that visit, the patient refers that
symptoms are relieved. NYHA class is moved back
to II. However, the CDSS suggests the physician to
explore the possible origins of the change in the
symptoms reported in the previous visit (i.e. the
probable cause of heart failure decompensation). In
particular, with the aim of controlling the ischemic
disease, a stress test is scheduled.
3.1 Methods
The CDSS was defined for an overall support of HF
management, facing the main decisional problems of
diagnosis, prognosis, therapy and follow-up, by
using patients’ heterogeneous information (e.g.,
actual status, anamnesis, clinical history, diagnostic
parameters, and clinicians’ evaluation).
Ontologies combined with rules were chosen as
representation formalism, because of the more
suitable and up-to-date methodology for formalizing
the declarative and procedural knowledge derived
from the guidelines and the experts’ know-how.
Actually, ontologies constitute a logic-based
representation which also assures easy re-use and
sharing of knowledge. Moreover, the rule based
approach appeared the more appropriate both to
complete possible representation lacks of ontological
model and to involve more effectively the experts in
the elicitation process. An inference engine was then
devised for the corresponding inferential reasoning
processes, by induction and deduction on the
formalized knowledge for assessing patients’ status,
formulating diagnosis and prognosis, assisting
therapy planning, and monitoring patients.
Computational reasoning models were included
for those difficult HF decision problems, such as
prognosis assessment and early detection of patient’s
decompensation.
The HEARTFAID CDSS architecture was
designed according to a multilevel conceptualization
scheme for distinguishing among
the knowledge level, corresponding to all the
information needed by the system for performing
tasks, e.g. data, domain knowledge, computational
decision models;
the processing level, consisting of the system
components that are responsible for tasks
accomplishment by using the knowledge level;
the end-user application level, including the system
components whose functionalities are specifically
defined for interacting with the user.
More in detail, the CDSS architecture consists of
the following components (Figure 1):
Domain Knowledge Base, consisting of the domain
knowledge, formalized from the guidelines and of
the clinicians’ know-how;
Model Base, containing the computational decision
models, signals and images processing methods
and pattern searching procedures;
Meta Knowledge Base, composed by the strategy
knowledge, i.e. about the organization of CDSS
tasks.
Brain, the system component endowed with the
reasoning capability, which is divided into the meta
and object level;
Explanation Facility, providing a means to explain
conclusions taken.
The Brain was modelled by functionally
separating a meta level, devoted to task
accomplishment and organisation, and an object
level, responsible for actually performing tasks, by
reasoning on the computational and domain
knowledge. A Strategy Controller was inserted for
performing the meta level functionalities, by
orchestrating the two components of the object level,
i.e. the Inference Engine and the Model Manager.
Moving from the design to the development
activity, the use case is being used as a real scenario
for implementing the above architecture.
Figure 1: The general view of the HEARTFAID CDSS
architecture – dashed arrows correspond to reference to
the ontologies, while the others denote a direct
communication.
HEALTHINF 2008 - International Conference on Health Informatics
292

The required CDSS interventions consist in the
following services, listed in order of occurrence in
the workflow:
interpretation of telemonitored data and
assessment of patient’s status;
visit scheduling;
suggestion of new diagnostic examinations;
analysis of imaging examinations;
interpretation of diagnostic findings;
suggestion of therapy changes.
The necessary pieces of knowledge have been
identified as mainly symbolic and an elicitation
process has been performed for their formalization
in the Domai1n KB. Specific algorithms for
extracting a number of useful parameters from the
echo images have been developed and inserted into
the Model Base.
In particular, the use case highlights the
interventions of other components of HFP which
hold important roles in assuring the effectiveness of
the support services, e.g. the agenda for scheduling
new visits or examinations. Actually, HFP was
conceived for consciously distributing the work load
among the various components. A sketch of the
platform with the components that interact with the
CDSS is shown in Figure 2.
An EHR module was inserted for suitably
organizing, visualizing and managing patients’ data,
stored into the platform Repository. In particular, a
dedicated Repository for storing examination images
was conceived in accordance to the DICOM
standard. An Agenda module was included for
managing patients’ care planning, e.g., scheduling
new visits, prescribing new examinations and so
forth. The User Interface was designed as a
fundamental component, responsible for all the
interactions and communications with the users.
The different components of the platform were
seen as resources, by virtualizing the operations
required for their management. When involved, the
different components are dynamically integrated for
supplying sophisticated but much flexible
applications. The responsible for guaranteeing
integration and interoperability among all the HFP
components was defined as the platform
Middleware, which includes all the adapters
necessary for the virtualization. For simplifying the
provision of different services, a Service Controller
(SC) was comprised for managing platform events
and invoking the other components.
Figure 2: A sketch of HFP with the components that
interact with the CDSS.
In this perspective, the CDSS component was
designed as a resource able to offer a number of
functionalities and to interact with the other
resources for performing its tasks. Each decision-
making problem has to be translated into a request
or a class of requests committed to the CDSS, which
is then activated on-demand. The system handles
every request according to a specific policy encoded
in the Meta KB, interacting, when necessary, with
the other platform components.
A brief (and partial), discursive description about
how the scenario has been mapped onto a workflow
of HFP services is useful for understanding its
implementation.
Description of the Mapping into the HFP.
The patient answers a questionnaire through his
web-based user interface and sends the information
to the HFP that checks eventual missing values.
Then the Service Controller stores this information
into the repository, gets historical data and
opportunely invokes the specific CDSS service
responsible for handling the request.
The CDSS analyzes data and answers supplying
the current patient’s status, i.e. worsening of
symptoms, and a set of suggested actions the
clinician should undertake, i.e. schedule a new visit,
change the NYHA class or change the therapy and
so forth. Then the SC stores CDSS results into the
repository.
When the doctor on duty logs in the HFP, the list
of patients is displayed ordered by their severity
status and the timestamp of the last related event.
Once the patient is selected, the change in his status
is shown along with the list of suggested actions, for
instance as a list of operations that can be selected.
He then approves the schedule of the visit and the
SC forwards the request to the Agenda component
that opportunely records it and informs the patient.
During the visit, the physician inserts his
observations into the patient’s record and decides to
approve the change of the NYHA class: he selects
the corresponding action within the list and the SC
DECISION SUPPORT AND IMAGE & SIGNAL ANALYSIS IN HEART FAILURE - A Comprehensive Use Case
293
takes care of registering the change in the patient’s
record. An ECG is then performed acquired by the
platform and processed with QRS detection and
classification algorithms in order to produce noise-
free reference beats for all the 12 leads. The
availability of graphical tools for the signal display
and measurements (ruler) allows the cardiologist for
an accurate and reliable evaluation of the significant
morphological parameters. Then the information
obtained by the ECG is inputted and a request is sent
by the SC to the CDSS, which suggests performing
an echocardiography as displayed in the
recommended actions list.
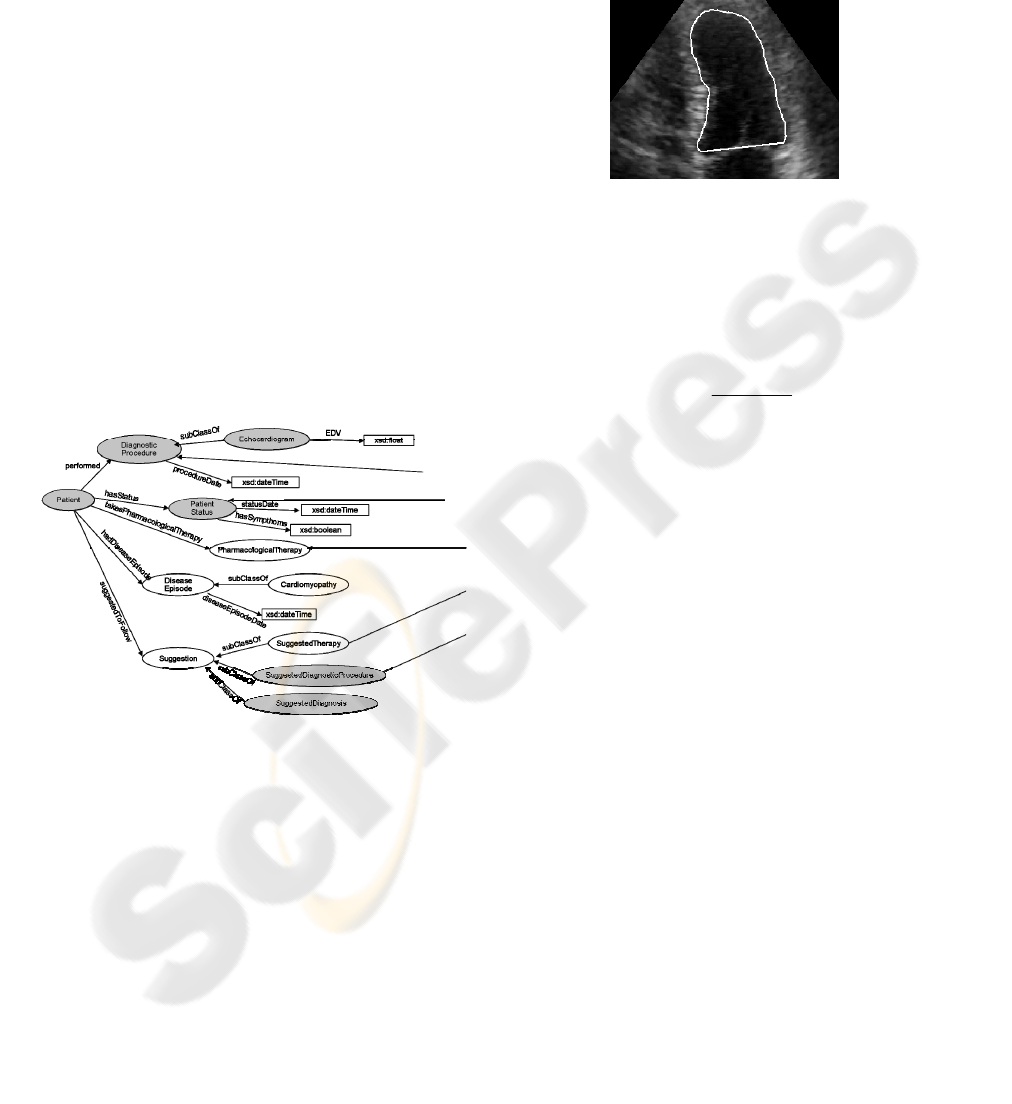
Inference on Patients’ Data. In order to include
information derived from the use case, starting from
a preliminary ontology mainly corresponding to a
structured terminology of the domain, we began to
develop a new ontology by inserting relevant
properties, classes and relations for a coherent and
comprehensive formalization, also in accordance to
standard medical ontologies, such as the Unified
Medical Language System (UMLS, 2007). An
excerpt of this new ontology is shown in Figure 3.
Figure 3: Some relevant classes and properties of the
ontology.
A careful elicitation activity was performed for
formalizing a set of rules, founded on the developed
ontology and to be encoded in the KB. An elicited rule
which is used for therapy suggestion is: “If a patient has
Left Ventricle Ejection Fraction <= 40% and he is
asymptomatic and is assuming ACE Inhibitors or ARB)
and he had a myocardial infarction then a suggestion for
the doctor is to give the patient Betablockers”.
Echocardiography Images Analysis. A prototype
module for the computation of LVEF has been
developed (Barcaro et al., 2007). The module is able
to process an apical-view sequence of the heart (the
so-called two- and four-chamber views) in order to
identify the left ventricle cavity in every frame of the
sequence. This segmentation stage is accomplished
augmenting a variational formulation of level set
methods with mimetic criteria for contour
initialization (see Figure 4).
Figure 4: Segmented left ventricle cavity at end-systole.
After segmentation, the left ventricle volume is
computed as a function of time by applying
monoplane Simpson's method. Then ESV and EDV
are regarded as the minimum and maximum
respectively of the volume time-course. Finally
LVEF is obtained by the simple formula:
EDV ESV
LVEF
EDV
−
=
.
4 RESULTS AND CONCLUSIONS
A number of tools and instruments are available for
developing the CDSS according to the design
specifications. The key factors that were taken into
account for defining an up-to-date system were
accordance to standards, efficiency and robustness.
We investigated several technologies, with
particular attention to the Semantic Web field, since
it offers various tools for building ontological
models, knowledge bases and reasoning on them.
Moreover, the platform was conceived for web
applications developed in Java. For selecting the
appropriate tools, we carefully analyzed the W3C
recommendations along with the performance,
compatibility and maintenance of the same tools.
As to the knowledge representation formalism,
we selected the Web Ontology Language (OWL,
2007) for defining the ontologies, since it is the
actual de-facto standard semantic markup language
for this task.
The ontology has been built using the two editors
Protégé and Swoop. For defining the rules of the
KB, we chose SWRL (2007), the Semantic Web
Rule Language combining OWL and Rule Mark-up
Language, which is a submission to W3C that
extends the set of OWL axioms to include Horn-like
HEALTHINF 2008 - International Conference on Health Informatics
294

rules. For realizing the reasoning component, Jena
(McBride, 2001) was selected as a Java
programmatic environment that includes OWL, a
language for querying ontologies, SPARQL (2007),
and a rule-based inference engines. In particular, for
improving the reasoning capability of the latter, we
also used Bossam (2007) and Pellet (2007). An
example of the rules we are developing in SWRL is
shown in Figure 5 as it has been defined in Protégé.
Figure 5: A rule developed in SWRL.
Prototypical methods for processing the echo
images were realized implementing the various
procedures in Matlab.
Future activities consist in finalizing the platform
implementation by concluding the realization of the
Domain KB, the algorithms contained in the Model
Base and the Brain, in particular of its meta level for
integrating all the object models and the interface.
ACKNOWLEDGEMENTS
This research work is supported by the European
Community, under the Sixth Framework
Programme, Information Society Technology – ICT
for Health, within the STREP project HEARTFAID
(IST-2005-027107), 2006-2009.
REFERENCES
Barcaro, U., Moroni, D., Salvetti, O. (2007) Left ventricle
segmentation in ultrasound sequences for the
automatic computation of ejection fraction. In
OGRW07 Open Gern Russ Work on Pat Rec & Im An.
Bayegan, E. Nytro, O. Grimsmo, A. (2002). Ontologies
for knowledge representation in a computer-based
patient record. In ICTAI 2002, 14th IEEE Int. Conf. on
Tools with Artificial. IEEE.
Bosmans, J.E., Dassen, W.R.M., van der Velde, E.T.,
Dijk, W.A., Spruijt, H.J., Baljon M.H. (2000).
Towards ICT Support for Treatment of Congestive
Heart Failure. Computers in Cardiology, 27, 641-644.
Bossam (2007) http://bossam.wordpress.com/
Boxwala, A.A., Peleg, M., Tu, S. et al. (2004) GLIF3: a
representation format for sharable computer-
interpretable clinical practice guidelines. J. Biomed
Inform., 37(3), 147-161.
Dassen, W.R.M., Gorgels, A.P.M., Berendsen, A., Dijk,
W.A., de Clercq, P.A., Hasman, A., Baljon M.H.
(2003). Guideline Assessment and Implementation in
Congestive Heart Failure. Computers in Cardiology,
30, 331-334.
ESC (2005) Swedberg, K. et al., “Guidelines for the
diagnosis and treatment of Chronic Heart Failure: full
text (update 2005)”, European Heart J, 45 pages.
GEM (2003) E2210-02 Standard Specification for
Guideline Elements Model (GEM) Book of Standards
Volume: 14.01. ASTM International.
Greenes, D. (2007). Clinical Decision Support: The Road
Ahead. Academic Press.
Helbig, H. (2006) Knowledge Representation and the
Semantics of Natural Language, Springer, Berlin,
Heidelberg, New York.
Lang, R.M. et al., (2005). Recommendation for Chamber
Quantification.. J Am Soc Echocardiogr, 18, 1440-
1463.
McBride, B. (2001) Jena: Implementing the RDF Model
and Syntax Specification. In WWW2001, Semantic
Web Workshop.
Noble, J.A., & Boukerroui, D. (2006). Ultrasound image
segmentation: a survey. In IEEE Trans. Med. Imag.,
25, 987-1010.
OWL (2007) http://www.w3.org/TR/owl-features/
Park, R.W., Shin, S.S., Choi, Y.I., Ahn, J.O., Hwang, S.C.
(2005). Computerized physician order entry and
electronic medical record systems in Korean teaching
and general hospitals: results of a 2004 survey. J Am
Med Inform Assoc. 12(6):642-7.
Pellet (2007) http://pellet.owldl.com/
Perlini, S. et al. (1990) Treatment of chronic heart failure:
an expert system advisor for general practitioners.
Acta Cardiol., 45(5), 365-78.
Poissant, L., Pereira, J., Tamblyn, R. Kawasumi, Y.
(2005). The impact of electronic health records on
time efficiency of physicians and nurses: a systematic
review. J Am Med Inform Assoc. 12 (5), 505-16.
SPARQL (2007) http://www.w3.org/TR/rdf-sparql-query/
UMLS (2007). http://www.nlm.nih.gov/research/umls/
SWRL (2007) http://www.w3.org/Submission/SWRL/
VV.AA. (2007). Functional Specifications of Data
Processing and Decision Support Services.
Deliverable D15, HEARTFAID IST-2005-027107.
Wirtz, V., Cribb, A., Barber, N. (2006). Patient–doctor
decision-making about treatment within the
consultation—A critical analysis of models. Social
Science & Medicine. 62, 1, 116-124.
DECISION SUPPORT AND IMAGE & SIGNAL ANALYSIS IN HEART FAILURE - A Comprehensive Use Case
295
