
A BPM-BASED MOBILE U-HEALTH SERVICE FRAMEWORK
Dongsoo Han, In-Young Ko, Sungjoon Park, Minkyu Lee
School of Engineering, Information and Communications University,119, Munjiro, Yuseong-gu, Daejeon, Korea
Suntae Jung
Samsung Electronics, 416, Maetan-dong,Youngtong-gu, Suwon, Kyounggi-do, Korea
Keywords: e-Health, u-Health service platform, ontology, mobile, BPM.
Abstract: The integration of mobile bio-sensors and cellular phones opens a new horizon for healthcare service.
Mobile u-health service, which usually incorporates mobile bio-sensor attached cellular phones, provides
users real time healthcare services at the right time in the right manner. While the u-health services may
look different from the service point of view, they often share many common features at various levels such
as the service structure, unit service, and data levels. Thus, it is necessary to have a common platform on
which various u-health services can be developed by effectively sharing and reusing the common features
and services rather than developing the services independently from the scratch. In this paper, we propose a
mobile u-health platform that provides core functions and facilities to develop mobile u-health services.
Main elements of the platform include the u-health ontology and common data structures, and Business
Process Management (BPM) based service integration framework. The platform provides commonly
reusable features and functions in developing u-health services. According to the early evaluation, our
platform turned out to have strength in terms of service flexibility, accessibility, evolvability, reusability,
adaptability, interoperability and guideline provision for developing u-health services.
1 INTRODUCTION
The integration of mobile bio-sensors and cellular
phones opens a new horizon for healthcare service.
It enables us to provide various healthcare services
in mobile environment. Actually, couple of mobile
u-health services are developed and announced to
the public. But, currently available mobile u-health
services are very limited in terms of scopes and
types of the services. This situation will be changed
as more mobile bio-sensors become available and
the number of mobile u-healthcare users increases.
Meanwhile, due to the lack of commonly
available mobile u-health service development and
running platform, current mobile u-health services
are usually developed in ad hoc and separate manner.
Although u-health services may look different from
the service point of view, they often share many
common features at various levels such as the
service structure, unit service, and data levels. Thus,
it is necessary to have a common platform on which
various u-health services can be developed by
effectively sharing and reusing the common features
and services rather than developing the services
independently from the scratch.
In this paper, we propose a mobile u-health
platform that provides core functions and facilities to
develop mobile u-health services. Main elements of
the platform include the u-health ontology and
common data structures, and Business Process
Management (BPM) based service integration
framework. The platform provides commonly
reusable features and functions in developing u-
health services.
The platform has several unique features. First,
the platform interprets and treats mobile u-health
service as service process and it extends BPMS to
healthcare service. As a consequence, the platform
can provide functions and facilities of general
Business Process Management System (BPMS). In
regard with the u-health service process, we define a
typical mobile u-health service process template and
deploy the process template on the platform. Second,
the platform is equipped with a very unique matrix
based patient group identification method. The
method is quite useful in mobile environment in
which less precise bio-signals data is frequently
gathered from a large number of users. Third, the
platform provides several advanced features and
functions by incorporating ontology technologies in
110
Han D., Ko I., Park S., Lee M. and Jung S. (2008).
A BPM-BASED MOBILE U-HEALTH SERVICE FRAMEWORK.
In Proceedings of the First International Conference on Health Informatics, pages 110-117
Copyright
c
SciTePress

defining mobile u-health services and disease
inferring processes.
We implemented the prototype of the proposed
platform and evaluated the prototype based on the
various software design criteria. According to the
early evaluation, our platform turned out to have
strength in the aspects of service flexibility,
accessibility, evolvability, reusability, adaptability,
interoperability and guideline provision for
developing u-health services.
2 RELATED WORK
Konstantas et al. (Konstantas et al., 2006) have
presented a Java-based service platform for remote
monitoring of patients. They collect patient data
using medical sensors integrated into the system
which captures six different bio-signals: ECG, HRV,
pulse oximetry, temperature, marking, respiration,
and motion/activity. The captured bio-signals are
delivered to remote healthcare experts for analysis.
However, the system does not provide any means to
manage the health care process between the experts
and the patients.
There were some attempts to use a workflow
management system or Business Process
Management System (BPMS) for the integration of
the Patient Record Manager (PRM) module and the
Personal Organizer (PO) system in healthcare
support (Pappas et al., 2002). Healthcare and
emergency response organizations are the users of
such solutions. One of the drawbacks of a healthcare
system without BPM is insufficient handling of
incomplete task definitions (Broens et al., 2005).
Oliver et al. (Oliver and Flores-Mangas, 2006)
have designed and developed MPTrain, a mobile
phone based system that utilizes the effects of music
in physical exercises. MPTrain enables users to
more easily achieve their exercise goals by
constantly monitoring their physiology such as HRV,
and by selecting/playing music with specific features
that make the users speed up, slow down or keep the
pace to maximize the exercise results.
The work done by Jovanov et al. (Jovanov et al.,
2003) is closely related to the healthcare monitoring.
They capture HRV to quantify the levels of stress for
a group of individuals undergoing military training.
They collect HRV data of military personnel prior to,
during and after training and assess their stress
levels and predict their stress resistance.
However, none of the work support a systematic
approach in developing mobile u-health services by
using a common u-health service platform like the
one described in this paper.
3 MOBILE U-HEALTH SERVICES
A mobile u-health service system is a total system
that enables u-health services to be coherently
provided to the users. The system integrates various
components such as bio-sensors, cellular phones,
associated software, and devices that are essential
for u-health services. In this section, we describe the
core components that constitute mobile u-health
services.
We have identified the main categories of the
core components that play essential roles in
providing u-health services. Bio-data gathering and
management, bio-data analysis, and knowledge
extraction and decision support are the service
categories that we identified based on the steps or
roles involved in the u-health service process.
3.1 Bio-data Gathering and
Management
A mobile u-health service starts its function with
periodically or randomly gathering input data i.e.
capturing the bio-signal data from users. We use
some bio-sensors that are wearable by the users or
imbedded into cellular phones. Thus, the bio-sensor
devices and cellular phones, which act as a gateway
between the bio-sensors and the u-health server, are
the essential components for gathering input data.
Besides, questionnaires that can be provided via
cellular phones are necessary to obtain information
that cannot be gathered from bio-sensors. The
physical symptoms that a user experiences, the
location of the user, and the weather information are
examples of such information that need to be
obtained directly from the users by using the
questionnaires. We have developed a generic
questionnaire composer to accommodate various
symptoms and environmental information in making
questionnaires.
Our mobile u-health service platform provides
the sensing modules and questionnaire interfaces
independently from the core functionality of u-
health services. This improves the reusability of the
sensing modules and questionnaires for different
healthcare services.
3.2 Bio-data Analysis
Since huge amount of bio-data need to be gathered
and analyzed in mobile u-health services, it is
essential to have an efficient data structure that
allows the system to effectively store and manage
bio-data. We investigated that a matrix is one of the
good candidates for storing and analyzing a large
A BPM-BASED MOBILE U-HEALTH SERVICE FRAMEWORK
111
quantity of data. We devised a bio-signal and
symptom combination matrix, in which the
appearances of bio-signal and symptom combination
pairs of a normal user group and those of a patient
user group are registered. We call the matrix as the
Disease Combination Appearance Probability
(DCAP) matrix. Two DCAP matrices are created,
one for normal groups, and another for patent groups.
The accumulated data in DCAP matrices becomes
the basis of the next step of the u-health service
process, the knowledge extraction and decision
support.
3.3 Knowledge Extraction and Decision
Support
Once a large amount of bio-data is accumulated,
knowledge extraction and decision support for
diagnosis can be provided by using data mining
technology. Sometimes, we can use well established
health indices to diagnose certain diseases to support
some u-health services. However, in many cases,
new health indices may need to be developed by
performing machine learning or pattern recognition
based on the accumulated data.
For the accumulation and management of bio-data
and information obtained from questionnaires, we
have developed data ontology. Based on this data
ontology, symptom, disease and bio-signal data can
be archived in a structured manner. Some additional
information such as a weight value to represent the
degree of association between each input data and a
certain disease type is assigned to the data ontology.
Note that the weight values are defined not by users
but by domain experts. The data ontology grows as
new services and/or disease information are
incorporated, and this contributes to make our
platform evolvable.
One assumption that we made in identifying
health indices is that diseases can be diagnosed
based on the combination of bio-signals and
symptom information. Another assumption is that
bio-signals and symptom data of normal and patient
groups can be obtained in some way. If the
difference between the data gathered from the
normal group and the patient group is obvious, the
interrelation patterns between bio-signals and
symptoms provide good criteria to classify users into
the two groups. A statistical equation is devised
based on the DCAP matrices to discern a normal
group from a patient group. Once bio-signals and
symptoms of a disease or a service are stored in
DCAP matrices, (Eq. 1) is used to compute the
probability for a person who has the CP(p) bio-
signals and symptom pairs to belong to the patient
group of the disease. X(p) and Y(P) denote weight
vectors of bio-signals and symptoms respectively.
We leave the detailed explanation to our previous
work and we do not delve into the details in this
paper.
P(p ∈ Patient Group │CP(p)) =
∑∑
∑∑
==
==
⋅
⋅
m
i
n
u
n
v
v
uiu
m
j
j
i
pY
pDCAPpY
pX
pX
11
1
,
1
)]
)(
)()(
(
)(
)(
[
(Eq. 1)
4 MOBILE U-HEALTH SERVICE
SCENARIO
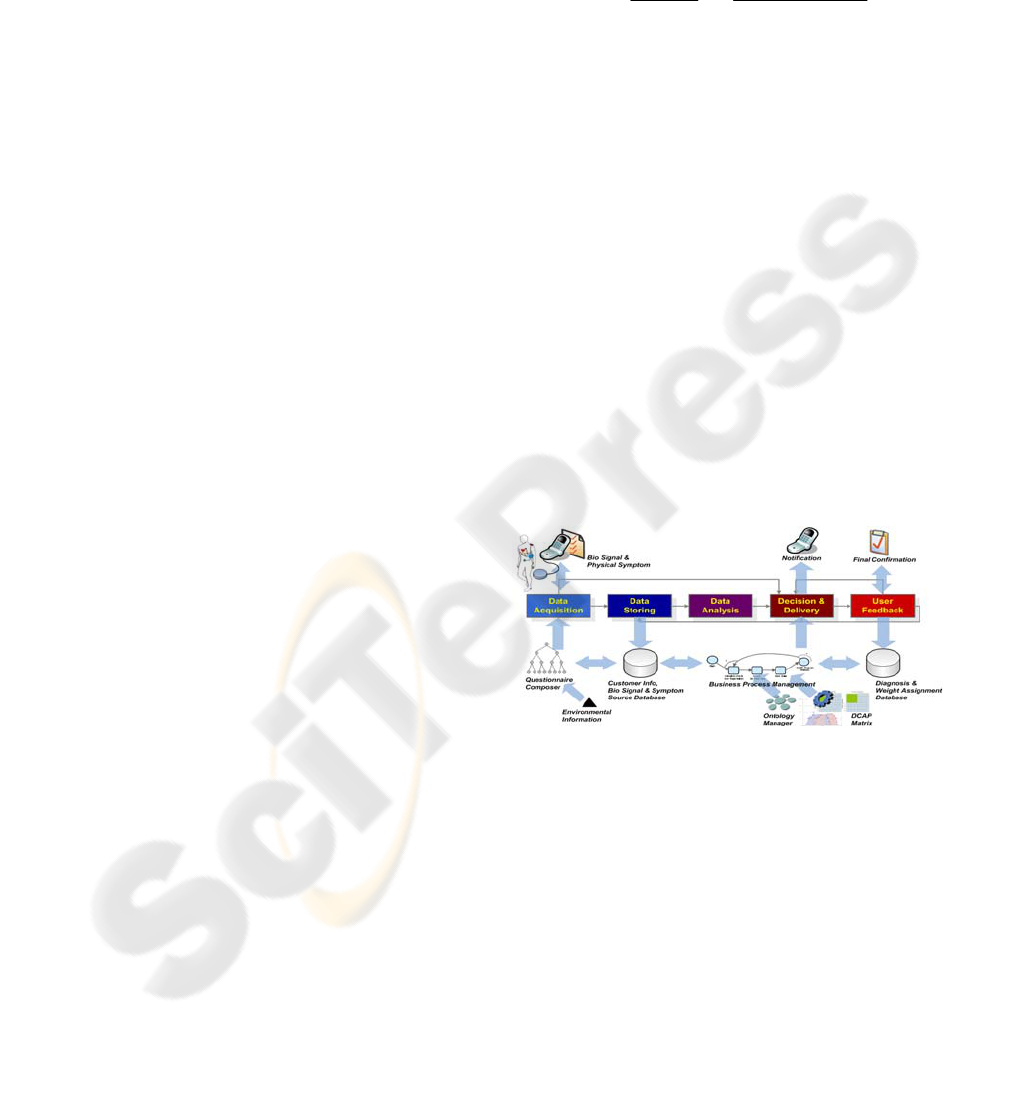
Fig. 1 illustrates the generic service scenario for
mobile u-health services. In the first step of the
service scenario, users fill out questionnaires to
provide information about physical symptoms and
their environments, which cannot be obtained from
bio-sensors. The sensors embedded in cellular
phones capture necessary bio-signal and relay the
data to the u-health server.
After gathering bio-data from questionnaires and
sensors, a mobile u-health service process is initiated
by an associated BPM engine. The next activity of
the scenario process is to store the relayed data to a
database so that the history of bio-data of a person
can be persistently kept for further analyses.
Figure 1: Mobile u-health service scenario process.
In the data analysis and decision support steps,
the data ontology manager, which keeps
semantically structured data for a specific set of
diseases, plays a key role in identifying potential
diseases based on the symptoms and bio-signals. For
each symptom and bio-signal, the data ontology
manager assigns a weight value that represents the
degree of association between the symptom or bio-
signal and a certain disease.
The final diagnosis decision is made by (Eq. 1).
The computed probability is delivered to the user to
show whether the user belongs to the patient group
or not. One of the unique features of our approach is
the user feedback mechanism. Using the feed back
HEALTHINF 2008 - International Conference on Health Informatics
112

mechanism, users can send their feed back on
analysis results (the diagnosed diseases) as the
response to the system. Based on this feedback data,
the system adjusts weight values of corresponding
symptoms and bio-signals to provide more
personalized services.
The u-health service scenario itself, and the data
ontology and the DCAP matrix components are
independent from any specific u-health services.
Therefore, the platform we designed is considered to
be a general platform. In other words, the u-health
service scenario and its supporting components can
be used for a variety of u-health services. A mobile
u-health service for specific disease can be
implemented by extending the service scenario.
Please see Section 6 for more details.
5 PLATFORM ARCHITECTURE
The mobile u-health service platform is a
middleware that enables the integration of diverse
services by using BPM. It serves as the hub to
integrate techniques and functions that are
associated with mobile u-health services, and
provides an environment to develop and run the u-
health services. Fig. 2 illustrates the architecture of
the platform that shows the major components and
the connections to the surrounding elements in the u-
health service framework.
Since cellular phones play the role of a gateway
between bio-sensors and servers, mobile message
handling is essential for the platform. The mobile
message handling module relays all the messages
from bio-sensors to the server. Not only the bio
signal data but also service request messages are
delivered by the message handling module.
Sometimes, it contributes to filter out some noise
signals from the received messages.
The bio-data delivered to a server is stored and
managed by the huge temporal data management
module. The bio-data is stored in diverse forms so
that various services can utilize the data to perform
their functions.
Data mining and pattern recognition techniques
are used to identify health index from the
accumulated bio-data. Also, an external or internal
expert system may refer to the data as feedback
information. In order to support this, the database
schema of the temporal database needs to be
designed to satisfy the requirements of data mining
or pattern recognition techniques and expert systems.
Online Services
Mobile E
Mobile E
-
-
Health Platform
Health Platform
Patient
Medical Info
E-Health
Information
Medical
Knowledge
Ontology
Expert
System
Expert
Expert
System
System
Cell p ones
PDAs
E- health Cards
Sensors
E
E
-
-
Health Process
Health Process
Management
Management
Mobile Message
Mobile Message
Handling
Handling
Dynamic Service
Dynamic Service
Coordination
Coordination
User
User
Management
Management
Huge Temporal
Huge Temporal
Database Management
Database Management
Data Mining/
Data Mining/
Pattern Recognition
Pattern Recognition
E
E
-
-
Health Process
Health Process
E
E
-
-
Health Portal
Health Portal
Patients
Clinicians
Exercise Management
Exercise Management
Stress Management
Stress Management
Weight Management
Weight Management
ECG/MCG E
ECG/MCG E
-
-
Health
Health
Management
Management
Blood Sugar
Blood Sugar
Mang
Mang
.
.
Fatigue Management
Fatigue Management
User Applications
User Applications
Expert
System
Expert
Expert
System
System
Expert
Systems
Expert
Expert
Systems
Systems
Sleeping Management
Sleeping Management
Figure 2: Mobile u-health service platform architecture.
As explained in Section 4, in order to develop a
mobile u-health service on the service platform, the
u-health service should be defined in a form of
process containing steps like bio-data gathering,
storing, analysis, and result reporting. The u-health
process block in Fig. 2 denotes a set of mobile u-
health processes derivable from the u-health service
scenario process explained in Section 4.
The u-health process definition tool allows
developers to easily define new mobile u-health
services. Mobile u-health services defined in a form
of process are controlled and enacted by the u-health
process management module. The u-health process
management module provides not only the
enactment function but also monitoring and
administration functions for u-health processes.
The mobile u-health management module and u-
health process definition tool play a key role in
making the platform evolvable. When a new mobile
u-health service process is defined, reusable process
templates, steps, and data structures are identified
and registered to the server for later use. The
management module ties together a set of u-health
services into a group by specifying execution
dependencies and the dataflow between the services.
There may be also some constraints that prevent a
particular service to be initiated until some other
services finish their functions.
The user management module is essential for
providing personalized service to individual users.
The user management module stores user profile
information such as age, gender, and occupation.
Since a user is a participant in a mobile u-health
process as well, this module is closely connected to
the participant information in the u-health process
management module.
The dynamic service coordination module
executes a service process by initiating and
synchronizing services during runtime. It also
ensures reliable u-health service execution by
A BPM-BASED MOBILE U-HEALTH SERVICE FRAMEWORK
113
replacing one service with an alternative one when a
fault occurs in the service or the user's requirements
are changed. Data mining and pattern recognition
functions may need to be developed for specific u-
health services. Whenever such functions become
available, they are placed on the data mining/pattern
recognition module. An expert system engaged with
a u-health service may need to access the functions
in the data mining/pattern recognition module to get
a decision making support.
Mobile u-health services are accessible not only
from mobile devices, but also through a Web
browser. Web users can connect to a healthcare Web
portal, and access their health information. The
healthcare portal also provides useful services such
as registering user information, composing
questionnaires, and browsing expert advices.
Especially, the Web portal allows users to access
services that cannot be provided through mobile
devices due to the limitations of the devices such as
the small screen size, and memory and processor
constraints.
6 IMPLEMENTATION
6.1 Mobile u-Health Modeling Tool
We have implemented a prototype of the u-health
process modeling tool that allows application
developers to semi-automatically compose mobile u-
health services.
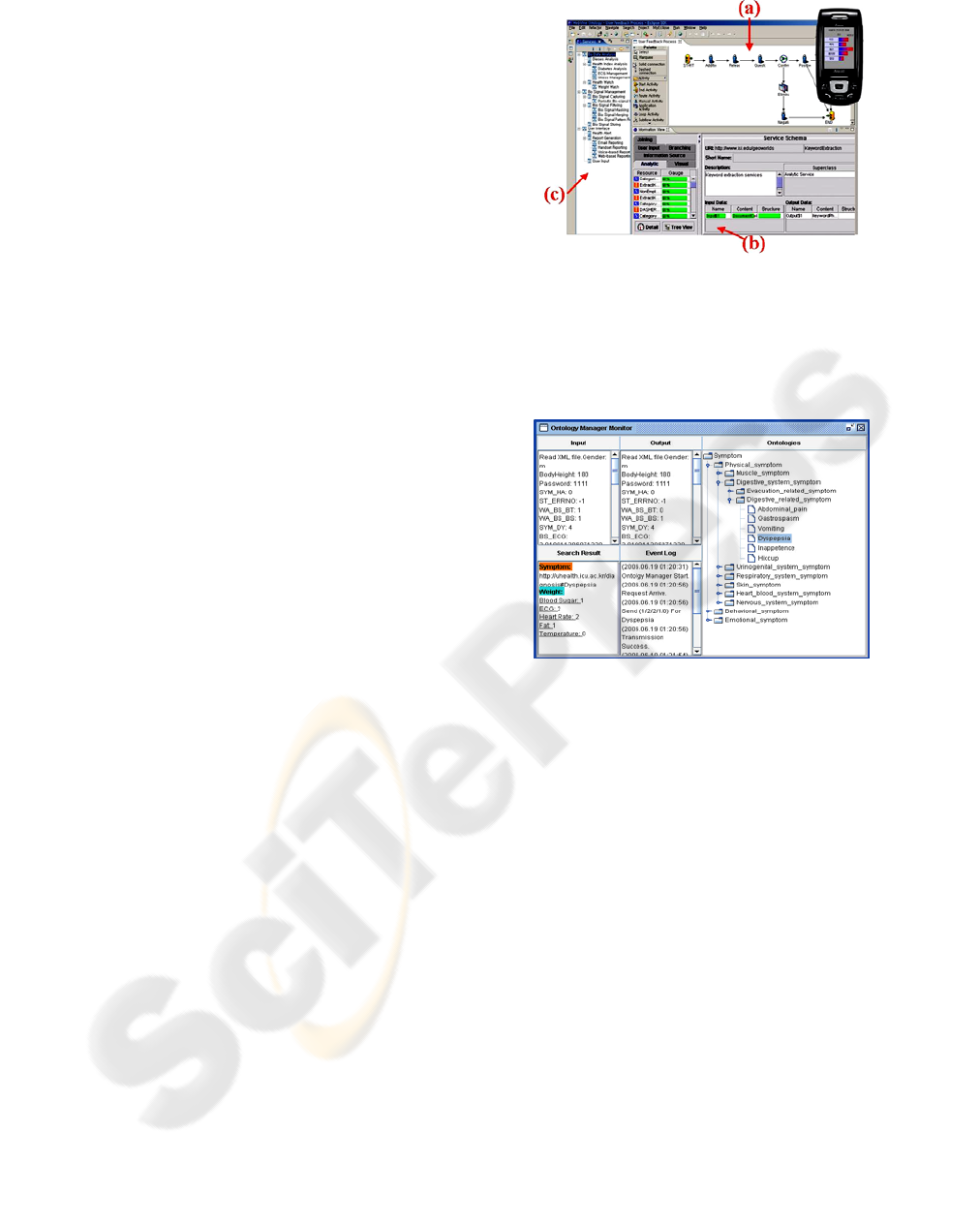
Fig. 3 shows the prototype of our mobile u-
health process modeling tool. The tool is
implemented in Java™ on Eclipse Foundation's
Eclipse™ platform. Part (a) of Fig. 3 shows the
canvas of the visual business process editing tool.
The tool graphically shows the basic u-health service
process template, and allows application developers
to specialize and extend the process to meet their
requirements. In the course of defining the process,
the process modeling tool recommends a set of
candidate services that can be used to implement
each step of the process, and are interoperable with
other services that are already put in the process. It
also automatically inserts adapters and converters
when it finds some syntactic and semantic
mismatches between services in the process. Part (b)
of the modeling tool is the service recommendation
tool that shows a list of candidate services for each
step in a process. When a user marks a service in a
service process, the tool lists the services that are
interoperable with the marked service. Part (c) of Fig.
3 is the ontology-hierarchy browser that allows
developers to browse through the service hierarchy.
Figure 3: Prototype of the service composition tool - (a)
Visual business process editing tool; (b) Service
recommendation tool; (c) Ontology-hierarchy browser.
6.2 Mobile u-Health Ontology
Manager
Figure 4: Ontology manager interface.
As explained earlier, in our platform, u-health data
such as symptoms, diseases, and bio-signals, are
systematically managed by constructing their
ontology. In addition, services are classified and
managed based on their functional ontology. The
ontology manager allows experts to easily manage
the u-health ontology. Fig. 4 shows the user
interface of the ontology manager. By using the tool,
experts can browse, add, remove, and search u-
health ontology.
6.3 Mobile u-Health DCAP Matrix
In our u-health service platform, the interrelation
patterns are identified in the learning and diagnosis
stage based on the patterns that is constructed in the
prediction stage. In the learning stage, interrelation
patterns of bio signal data and physical symptoms of
the normal and patient groups are identified. We
assume that enough learning data for the
identification of interrelations is available for this
stage.
HEALTHINF 2008 - International Conference on Health Informatics
114

In the learning stage, interaction frequencies of
bio-signals and physical symptoms from the normal
and patient groups are counted and registered in the
Combination Interaction (CI) matrices. Each CI
matrix contains combination patterns of specific bio-
signals and physical symptoms of the normal or
patient group with frequency scores. We integrated
both CI matrices into the DCAP matrix. In the
DCAP matrix, each element has a probability which
means how likely the combination pattern of the
element can be shown in a patient group. In the
prediction stage, bio signals and physical symptoms
of an unidentified person are submitted to the
prediction system. Then, the prediction system
determines how likely the person can be categorized
into the patient group. Since the DCAP matrix is
constructed based on the CI matrix, we can easily
figure out which bio-signal and physical-symptom
combinations contribute to a certain diagnosis. In
Fig. 5-(b), shaded areas are corresponding bio-signal
and symptom combination elements, and a
probability, ranging from 0 to 1, is calculated by
using (Eq. 1).
The DCAP matrix enables diverse forms of bio-
signals and physical symptoms to be used for
analyses. As shown in Fig. 5-(a), users can compare
their position in the matrix with those of others. In
addition, when we use the DCAP matrix, finding
primary bio-signal and physical symptom pairs that
contribute for the user to be classified into the
patient group is relatively easy. As a result, the
prediction system can show the causes of a certain
disease to users in a comprehensive manner. The
more clinical data is accumulated in the platform,
the more services the platform can provide in the
future.
Figure 5: Disease combination appearance probability
matrix – (a) Disease distribution chart for a learning set;
(b) Test result for a user health condition by the DCAP
matrix.
6.4 Mobile Client
Due to the diverse types and characteristics of bio-
sensors and various application scenarios, there are
many different requirements imposed on mobile u-
health systems. As a mobile gateway, a mobile
device is responsible for collecting data from sensors
by periodically sensing the human body.
Once a communication link is established, bio-
data and functions are delivered to the u-health
server using the wireless interface. The interface
sends and receives XML messages to and from BPM.
An XML message can a flexible structure to
facilitate transmission of different data types and
formats generated based on various bio-signals and
physical symptoms. By parsing the XML message,
the server classifies bio-data into several types and
then the server responds with the results of classified
bio-data in an XML message.
After forwarding bio-data to the server, the
application changes its state to the stand-by state
until it receives a response message from the server.
No event or signal can be pushed to the client
asynchronously. A process polling mechanism is
used to continuously pull the event of clients'
requests to the decision support step of the u-health
service process. When the server process is
completed, the result is delivered to the client.
Figure 6: WIPI Application Mounted on KTF Emulator &
Samsung Anycall SPH-V8900.
Once the client receives the probability of a
disease, the result is graphically displayed on the
mobile device. Figure 6 shows a graph displayed on
a cellular phone after receiving the results from the
server. If the user does not agree with the results,
he/she can send a feedback to the server to revise
his/her own weight vectors. The DCAP matrices are
updated if the feedback data is sufficiently
accumulated.
A BPM-BASED MOBILE U-HEALTH SERVICE FRAMEWORK
115
7 EVALUATION
We considered some quality attributes in designing
the mobile u-health service platform, which is a
large-scale service platform. We think that flexibility,
accessibility, evolvability, reusability, adaptability
and interoperability are the essential requirements
for large-scale service platforms.
Table 1: Evaluation of the Mobile u-Health Service
Platform.
Core Com-
ponents
Design
Goals
Bio-data
gathering and
management
Bio-data analysis
Decision
support
WI
PI
Web
Portal
Ontol
-ogy
DCAP
Matrix
BPM
Flexibility
○
△
○
○ ○
Accessibility
○ ○ × ×
△
Evolvability
N/A N/A
○ ○
△
Reusability
△
○ ○
△
○
Adaptability
△ △ △
○ ○
Interoperability
○ ○
△ △
○
Remarks: ○: Supported, ×: Not Supported, △ : Insufficient,
N/A: Not Applicable
Table 1 summarize these quality attributes and
explain how the core components of our service
platform contribute to satisfy those requirements.
The following sub-sections discuss the design
rationales of our platform to make it satisfy each of
the quality attributes.
7.1 Flexibility
There are some reasons why the mobile u-health
service platform needs to be flexible. Different sets
of bio-sensors such as ECG, HRV, and temperature
sensors need to be supported for different u-health
services. Furthermore, some of the sensors may need
to be replaced with other types depending on the
mobile-device types and some other constraints. In
addition, the functionality provided by the platform
or the user interface on a mobile device may need to
be customized for a specific user group. Also, the
bio-signals and symptoms that the healthcare server
handles may need to be changed based on the
disease types to cover by specific u-health services.
In order to support flexibility, we have
developed a Web-based questionnaire composer. It
can easily accommodate new questionnaires or
updates of questionnaires for new u-health scenarios.
In addition, since we use the BPM process modeling
tool for the definition of u-health service processes,
we can easily update the defined process when a
change is required. This enables the platform to be
used for a variety of u-health services with different
scenarios. The ontology-based data management and
the DCAP matrix are the features that improve
flexibility of our platform as well. The structure of
ontology and DCAP matrix can be dynamically
changed based on users' feedback information.
7.2 Accessibility
The multi-channel approach, which makes users'
health information accessible via both mobile and
Web-based interfaces, supports a good access
environment that enables the benefits of hybrid
accessibility. In the healthcare service environment,
a real-time and mobile disease-checking function
can be supported using mobile devices whereas the
in-depth analysis of the disease can be provided on
the Web. This makes the users to access their health
information in various degrees of detail.
7.3 Evolvability
As discussed in Section 3, the data ontology evolves
as new data and feedback information from users are
accumulated. In addition, the DCAP matrices used
in our u-health service platform are also evolvable.
According to the feedback on the analysis results,
the DCAP matrices appropriately change their
values for more precise and personalized analyses.
7.4 Reusability
The BPMS-based service development mechanism
makes service components reusable for various
types of u-health services. In other words, when a
new mobile u-health service is defined with the u-
health process definition tool, developers can reuse
various service components, and other assets in
different abstraction levels. Process templates,
activities, applications pertaining to an activity, and
data structures are the reusable assets in our platform.
When we consider that most u-health service
processes shares the basic u-health service scenario
described in Section 4, many components of a u-
health service process can be reusable by other u-
health processes. Since our platform is based on
BPMS, it is competitive in supporting reusability.
7.5 Adaptability
The circumstances and environment surrounding
mobile u-health services are ever changing. New
bio-sensors, which produce new forms of signals or
HEALTHINF 2008 - International Conference on Health Informatics
116

signals never handled before, may become available,
and new service scenarios may be developed. For
example, a mobile u-health service may be
developed to handle only a single type of sensor. But
sometime it may need to handle multiple sensors in a
bundle. Then, the implementation of the u-health
service needs to be modified to cope with the
changes. Since our platform maintains a property
file that keeps the descriptions about the sensor
types, the platform can adapt to the change more
efficiently. This property file enables multiple
sensors to be linked to a mobile device and to
transmit the sensor data over a single wireless link to
the u-health server.
When hospitals and insurance companies are
engaged with the mobile u-health service scenario
described in Section 4, the u-health service scenario
needs to be extended. Such kind of environmental
change circumventing u-health services may be
frequent in real situations. Since u-heath services are
defined in the form of processes using the BPMT
tool in our platform, they can adapt to such changes
more efficiently by adding new service components
and/or by replacing some of the service components
with alternative ones.
7.6 Interoperability
One of important criteria for designing the mobile u-
health service platform is interoperability. BPMS is
usually equipped with facilities for supporting
interoperability. Since our platform is based on
BPMS, the facilities of BPMS for interoperability
can be shared in the mobile u-health service
platform. The remote applications and systems can
be integrated with u-health services in our platform
without any extra work. The Web Services API for
BPMS and the Web portal provide an easy way of
exchanging information between processes.
8 CONCLUSIONS
In this paper, we have identified several core
components of the u-health service scenario process,
and described the overall architecture of the mobile
u-health platform. We have also developed essential
functions and facilities that allow service developers
to effectively use the core components to develop
various mobile u-health services with less effort.
Our mobile u-health service platform is very
unique in that it adopts BPMS as its underlying
platform, and u-health services are designed as
service processes. The standard u-health service
process provides a guideline to u-health service
developers. They can specialize and/or extend the
service process template to develop their own u-
health services. Six design goals are identified for
the mobile u-health platform, and we have tried to
achieve them in our BPMS-based u-health service
platform.
One of the lessons that we learned while
working with the mobile environment is that
different trade-offs need to be made for different
circumstances. For example, we need to consider
resource limitations on mobile devices,
communication bandwidth, and constraints on user
interfaces to make a trade-off between different
quality of services for different environments and
different user groups.
There are also some pending works to be done to
make the platform more secure and reliable. We are
currently investigating how to support the features of
managing personal healthcare data securely, and
enhancing the performance by compressing
messages exchanged between mobile devices and
the u-health server.
REFERENCES
D. Konstantas, R. Bults, A. Van Halteren , K. Wac, V.
Jones, I. Widya, R. Herzog, B. Streimelweger,
“Mobile Health Care: Towards a commercialization of
research results”, In proceedings of 1st European
Conference on eHealth - ECEH06 -Fribourg,
Switzerland, pp.12 – 13, October 2006.
Pappas, C. Coscia, E. Dodero, G. Gianuzzi, V.
Earney, M., “A Mobile E-Health System Based on
Workflow Automation Tools”, Computer-Based
Medical Systems. Proceedings of the 15th IEEE
Symposium on pp.271 – 276, June 2002.
Broens, T.H.F., van Halteren, A.T., van Sinderen, M.J.,
Wac, K.E. “Towards an application framework for
context-aware m-health applications”, In: EUNICE
2005 "Networked Applications". 11th open European
Summer School, pp.6-8 July 2005.
N. Oliver , F. Flores-Mangas, “MPTrain: a mobile, music
and physiology-based personal trainer”, ACM
International Conference Proceeding Series; Vol.159,
pp.21 – 28, 2006.
E. Jovanov, D. Raskovicl, A. 0. Lords, P. Cox, R. Adharni,
F. Andrasik, "Stress monitoring Using a Distributed
Wireless Intelligent Sensor System“, in IEEE
Engineering in Medicine and Biology Magazine, pp.
49-55, May/June 2003.
A BPM-BASED MOBILE U-HEALTH SERVICE FRAMEWORK
117
