
CLINICAL PRACTICAL GUIDELINE EDITOR
Clinical Practical Guideline-based Decision Support Tool
Plavčak Aleš
MIPS programska oprema d.o.o., Cesta k Tamu 7, 2000 Maribor, Slovenia
Keywords: Decision-support systems, medical informatics, clinical practice guidelines, knowledge modelling.
Abstract: According to quick growth of information and complexity of medicine, the development of informatics in
medicine is in full bloom. Medical decision support systems have been developed to help choose the
appropriate medical treatment procedures, ensure the quality of health care and enable the control of
resources. Clinical Practical Guidelines have greatly contributed to the accelerated development. Many
different modelling methods and tools have been developed for executing guidelines. Here, the three of
many applicable guideline modelling techniques are represented in greater scope. Also, a new technique of
representing the clinical knowledge has been designed, taken from the studies of already existing models.
The implementation of the application for editing, browsing and executing clinical guidelines has been
implemented as well. The application is capable of generating recommendations for a specific clinical state
and evaluation of the already existing health care process. This paper covers the general presentation of
informatics in medicine and the techniques for modelling of medical knowledge which nowadays represents
a gateway for prosperous development, and paves the way for broader use and implementation.
1 INTRODUCTION
The experiences of individual physicians, opinions
of professors in medical schools, medical textbooks,
clinical journals and clinical trials have guided the
practice of medicine for most of this century, so the
standardization is not necessarily obligatory, but
strongly recommendable. The medical community
has always standardized medical care to some
degree in order to provide what it thought was the
best care, to efficiently use resources, to satisfy
patients, and to withstand third party scrutiny.
The idea of studying which treatments work best
is nothing new, although systematic treatment
procedures are a novelty in many branches of
medicine. It is well known what the right things to
be done are, but we have to make it happen, so here
is methodology and computer based decision
support systems to assist practitioners and patients in
making decisions about appropriate management of
specific clinical conditions.
Our use of computers has been driven not only
by the increasing need to manage large amounts of
information, but also by the imperative to make
evidence based and cost effective decisions on a
daily basis. Furthermore, there is accumulating
evidence to prove that computer aided medical tools
address the growing information needs of the busy
clinician and improve healthcare processes as well
as patient outcomes. In turn, this has led to the rapid
proliferation of a variety of clinical decision support
system (CDSS). A computerised CDSS is a
computer based tool using explicit knowledge to
generate patient specific advice or interpretation. It
is now universally agreed that conforming to state-
of-the-art guidelines are the best way to improve the
quality of CDSS.
Nowadays the basic of developing a CDSS is a
clinical practice guideline (CPG) that is a subject
discussed by number of researchers who are trying
to develop different technologies for delivering
computerized guidelines in clinical care. The new
research movement could revolutionise the health
care industry by improving quality and reducing
costs, say the experts that are studying, developing
and evaluating CPGs. Above is depicted a newly
proposed design and implementation of application
for modelling, executing and evaluating CPG.
112
Ale
ˇ
s P. (2008).
CLINICAL PRACTICAL GUIDELINE EDITOR - Clinical Practical Guideline-based Decision Support Tool.
In Proceedings of the First International Conference on Health Informatics, pages 112-118
Copyright
c
SciTePress

2 KNOWLEDGE MODELLING
Medical experts are increasingly expected to always
make the best decision. This is difficult. The
amount of medical information in the world is
increasing, yet then capacity of a human brain is not.
Computers have the ability to help deal with all this
information, so generally speaking, computers are
better than humans at managing loads of information
and solving complex problems.
To be effective, these tools should have access to
the patient's medical record, use standard medical
vocabularies, have clear semantics, and facilitate
knowledge maintenance and sharing. In addition to
that they need to be sufficiently expressive in order
to explicitly capture the design of the rational
process and outcome intentions of the guideline's
author, while at the same time they must enable the
attending physician to use their own preferred
methods to achieve a certain degree of flexibility
during the application runtime.
The level of standardization in today’s
guidelines is relatively new. When predicated on
sound medical and scientific data, these guidelines
can lessen provider variability in treatment and
diagnosis. Better standardization allows better
measurement of resources used and assessment of
benefits obtained. These guidelines can be
particularly effective when applied to high-
prevalence, high-cost diseases or conditions.
2.1 Clinical Practice Guidelines
CPGs are developed to reduce inappropriate
variations in practice, to improve health care quality,
and to help control costs. Although the importance
of guidelines is widely recognized, health care
organizations typically pay more attention to
guideline development than to guideline
implementation for routine use during care process.
The American Medical Association calls them
“practice parameters” and defines them as
“...strategies for patient management developed to
assist physicians in clinical decision making.” As
already mentioned, they should not be rigid and
static; rather, they should be flexible and dynamic
road maps aimed at reducing clinically significant
and unexplained variations in patient care process.
“CPG are systematically developed statements,
based on best evidence, intended to assist
practitioners and patients in making decisions about
appropriate management of specific clinical
conditions” (Institute of Medicine, 1990). This
definition emphasizes the decision-making aspect of
clinical practice guidelines.
Samson Tu and Mark Musen have identified five
principle tasks that computerised guidelines and
guideline representation methods should be capable
of supporting: making decisions, sequencing actions,
setting goals (e.g. specific patient states) to be
achieved, interpreting data, refining actions (i.e.
breaking up into sub-components).
But not all of them are able to fulfil all the
principles. They cover many methods and
demonstrate the use of different representation
formalisms and computational techniques.
2.2 Guideline Modelling Methods
Based on a literature search of computer-based
guideline specific representation models, three
published research projects were included in this
review and represent the base for developing a CPG
support tool. Arden Syntax was chosen for its
simplicity and represents a pioneering achievement
for guidelines. PROforma is an easy understandable
and flexible language for encoding medical
knowledge. GLIF represents a complex guideline
modelling method and has well defined object-
orientated design.
2.2.1 Arden Syntax
Arden Syntax is a standard, formal procedural
language that represents medical algorithms in
clinical information systems as Medical Logic
Modules (MLMs), and uses rule-based specification
for encoding medical knowledge. It is the first
standard for representing medical knowledge. An
MLM is a hybrid between a production rule (i.e. an
"if-then" rule) and a procedural formalism. Each
MLM is invoked as if it were a single-step "if-then"
rule, but then it executes serially as a sequence of
instructions, including queries, calculations, logic
statements and write statements.
Arden was developed for embedding MLMs into
proprietary clinical information systems. It was
specially designed to support clinical decision
making. An individual MLM should contain
sufficient logic to make a single medical decision.
Sequencing tasks can be modelled by chaining a
sequence of MLMs. MLMs have been used to
generate clinical alerts and reminders,
interpretations, diagnoses, screening for clinical
research studies, quality assurance functions, and
administrative support.
CLINICAL PRACTICAL GUIDELINE EDITOR - Clinical Practical Guideline-based Decision Support Tool
113
2.2.2 PROforma
PROforma is a formal executable logic language for
describing clinical and other processes in terms of
the decisions and other tasks that a physician needs
to carry out to achieve its goals. It is capable of
capturing the structure and content of a CPG in a
form that can be interpreted by a computer. The
language represents the basis for a method and a
technology for developing and publishing executable
CPGs. PROforma combines the features of formal
specification languages as known in software
engineering with the features of knowledge
representation languages as known with artificial
intelligence.
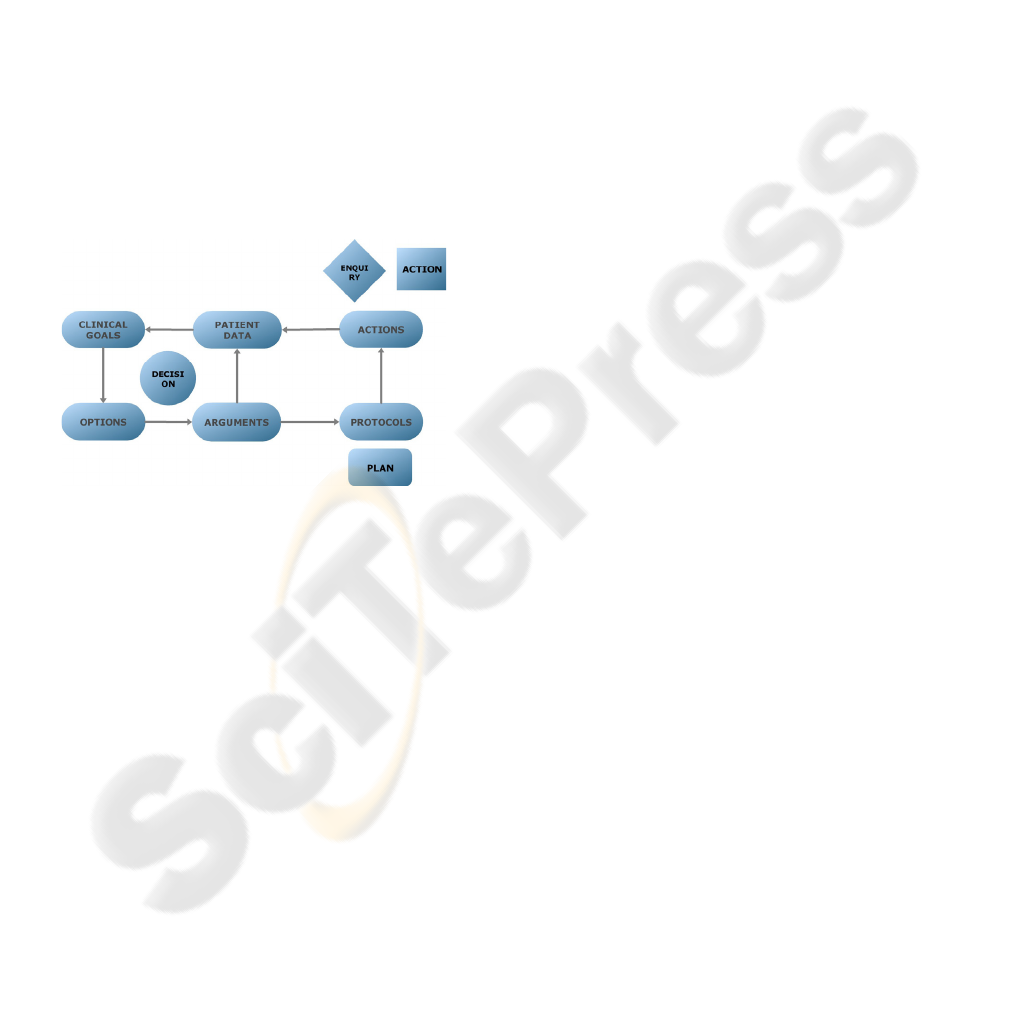
The PROforma language structure is based on a
simple but versatile clinical process model known as
the domino model shown in “Figure 1”. This model
derives from a variety of empirical studies of clinical
decision-making and the development of aids to
support patient management.
Figure 1: The relationship between the domino model of
clinical process and PROforma tasks.
The left side of the diagram represents decision-
making and the right the plan enactment. Given a set
of beliefs, an agent may set certain goals and various
solutions to these goals. With multiple options, such
as alternative diagnoses or treatments, the agent
must consider the arguments for and against these
alternatives and make decisions based on the validity
of each of the arguments. The domino model
describes a relationship between actions, decisions,
beliefs, plans, goals and candidate solutions, and the
inference and processes linking them.
A further result was a reconstruction of the
domino model into a minimal set of executable
generic tasks: enquiries, decisions, plans and actions
as shown in “Figure 1”. Tasks are formal software
objects that can be composed into networks
representing CPGs or other processes, and it is from
these tasks and the logical construct associated with
each task, that the PROforma language is derived.
2.2.3 GLIF
GLIF is a computer-interpretable language for
modelling and executing clinical practice guidelines.
GLIF supports sharing of computer-interpretable
clinical guidelines across different medical
institutions and system platforms. It has a formal
representation and defines the ontology for
representing guidelines, as well as a medical
ontology for representing medical data and concepts.
GLIF2 enables guideline modelling as a
flowchart of structured steps, representing clinical
actions and decisions. GLIF’s guideline class also
specifies maintenance information, the intention of
the guideline, eligibility criteria, and didactics. The
GLIF guideline instance syntax, which was based on
a separately developed language, specifies the
format of text files which contain GLIF-encoded
guidelines. These files are used for sharing and
interchange. However, the attributes of structured
constructs are defined as text strings that can not be
parsed, and such guidelines can not be used for
computer-based execution that requires automatic
collaboration.
In the year 2000 a new version of GLIF was
introduced (GLIF3), an evolving revision of GLIF
that attempted to overcome several of GLIF2’s
limitations. The GLIF3 model is object-oriented. It
consists of classes, their attributes and the
relationships among the classes which are necessary
to model clinical guidelines. The model is described
using Unified Modelling Language (UML) class
diagrams.
2.2.4 Approach to Guideline Modelling
We were trying to examine the increasing sets of
resources to obtain sufficiently amount of
knowledge that is needed to design development
tools and technique for building healthcare
application that comply with the highest possible
quality, safety and ethical standards.
To build an effective tool for capturing medical
knowledge in a systematic and executable way
among other criteria the following should be
satisfied: access to the patient's record, use of
standard medical vocabulary, clear semantics,
knowledge maintenance and sharing, sufficient
expressiveness to explicitly capture clinical
processes of the guideline's author and leave
flexibility during application runtime.
The primary goal of this project was to design an
open source decision support application for
decision-making between health professionals and
patients.
propose
solution
define
problem
arguments
commitment
data
acquisition
task
management
commitment
HEALTHINF 2008 - International Conference on Health Informatics
114
2.3 Guideline Evaluation and Design
We have designed a machine interpretable guideline
model as a sample of application that can improve
inappropriate variations in practice, health care
quality and to help control the costs. The guideline
model was preceded by the profound study of the
above mentioned guideline modelling methods. It
includes an analysis of the literature and three
published research projects concerning
computerized specific representation models. We
have tried to overcome the problematic of
representing clinical knowledge in computerised
manner by modelling clinical knowledge with CPGs.
In achieving our goals we have followed the
Stanford team dimensions: organization of guideline
plan components, goals/ intentions, model of
guideline actions, decision model, expression/
criterion language, data interpretation, medical
concept model, patient information model.
These dimensions capture the essence of
modelling the logic of computer-interpretable
guidelines. The first four represent the core
guideline components, and the last four link the
guideline model to the patient data.
For identifying key elements of our CPG model
the following elements were chosen:
Action specifies clinical actions that are to be
performed during the patient’s care process. These
clinical actions can include diagnostic or therapeutic
procedures that need to be performed in a treatment
process, if an action step is triggered. Actions were
modelled merely in a descriptive manner.
Enquiry describes the patient’s temporary physical
state. It contains the list of the attributes which are
necessary for evaluating the patient at the temporary
point of treatment. It looks into a patient’s medical
record and retrieves the values of the attributes
described in the enquiry list, or asks the user for the
required data.
Decision controls the flow of a guideline. It
contains a group of candidates and a group of
arguments for an individual candidate. Arguments
are described by given weight. It supports inference
in propositional and predicate logics, together with
certain non-classic logic for reasoning and control of
the guideline flow.
Plan components represent actions, decisions,
enquiries, or hierarchical decomposed sub-plans of
the guideline and their relationships. Plans merge
together individual atomic tasks (decisions, actions
and enquiries) or sub-plans into logical groups,
control complexity and enable control of grouped
elements.
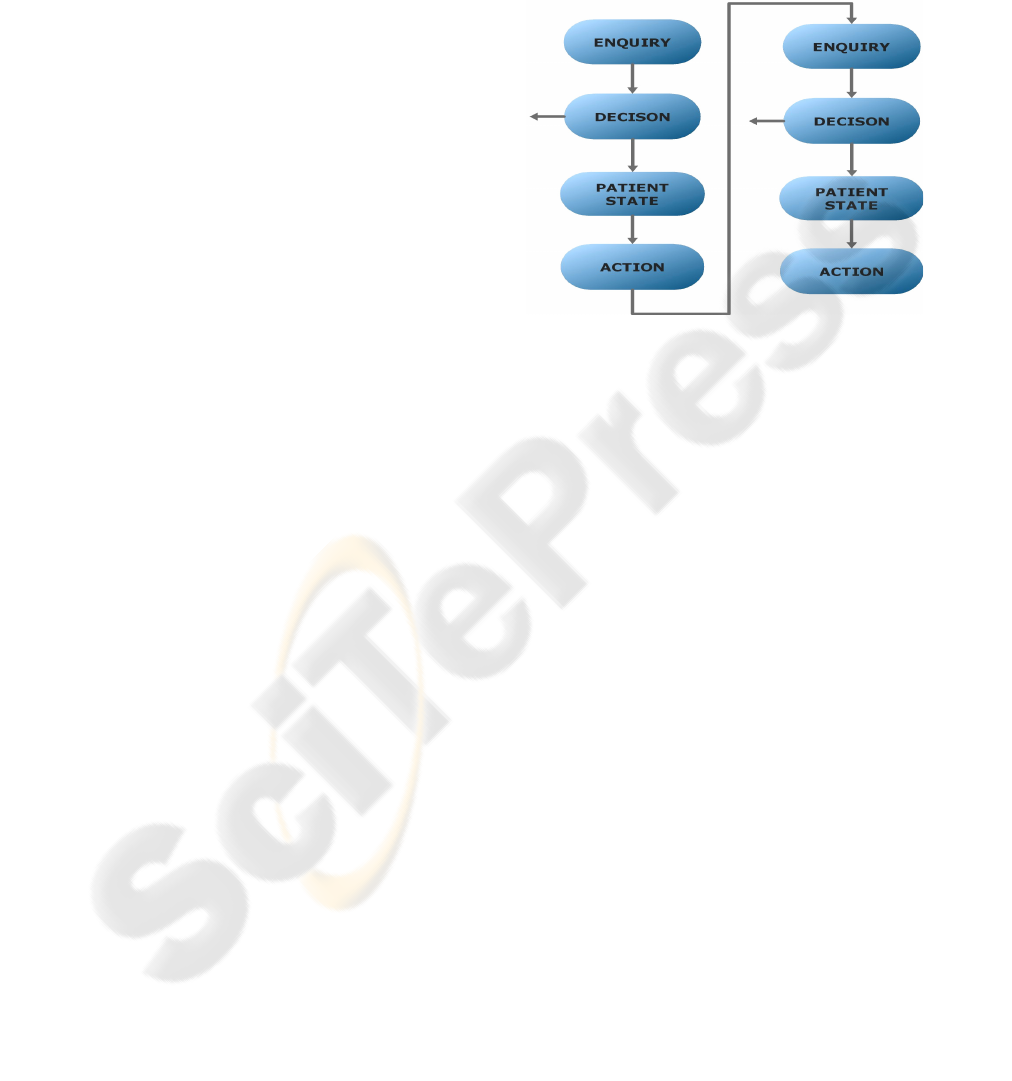
Basic tasks that a guideline needs to satisfy are
shown in “Figure 2”. Data needed at the specific
point of guideline execution is acquired by Enquiry.
Based on defined values we can make decisions that
evaluate patient’s temporary physical state. Actions
are defined for specific patient state, and are
executed as needed.
Figure 2: Logical flow of a guideline.
Constructs organization and decision model
clearly defines goals of guideline and appropriate
actions. The goal of a guideline flow is to choose an
appropriate medical procedure for treatment of
specific patient’s state, by either excluding possible
variations, or by choosing an optimal treatment
process. Our decision support model supports the
following features: each task can interrupt the
guideline execution, some tasks are optional and can
be ignored at execution time, some tasks need user
interaction and have to be confirmed, all tasks can
define preconditions that have to be fulfilled in order
to execute that task, execution of each task brings
system into a new state and sets new conditions, all
tasks can have cycle execution, decision model can
execute alternative tasks in parallel by excluding
preconditions of each task, decision model is non-
deterministic and uses arguments rules that can
choose more than one candidate among available
alternatives, expression language is represented
using mathematical expressions which, when
evaluated, give logical result True or False.
A guideline can be viewed in two abstract levels:
Conceptual level represents guideline as a flow
chart, and is used for browsing and navigation
through constructs. It represents a clear and simple
overview of a guideline.
Executable level represents guidelines in full
consistency and completeness. Definitions of
enquiries items, clinical action and flow of the
algorithm are specified at this level.
CLINICAL PRACTICAL GUIDELINE EDITOR - Clinical Practical Guideline-based Decision Support Tool
115
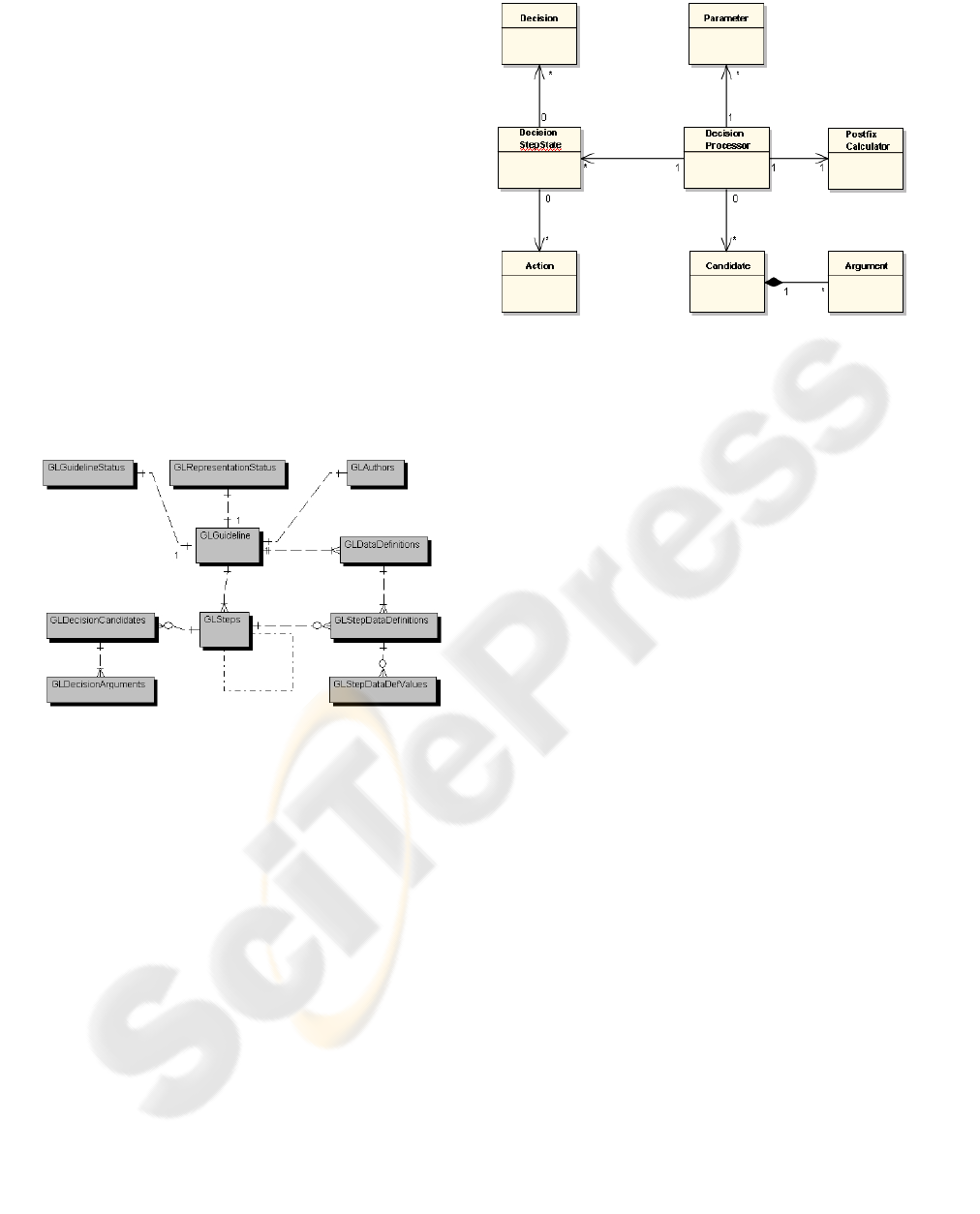
2.3.1 Database Support
Our model uses a support of relational database that
is easy extendable and enables transformation or
different representation of data. We have built an
entity relational database diagram (ERD) with
minimal set of entities as shown in “Figure 3”.
Starting-point of a guideline is the “GLGuideline”
entity that describes general information about
intention and its temporary state. For the moment we
have four general tasks of guideline, the common
attributes of which are collected in the “GLSteps”
entity. Future extensions with additional type of
tasks are easily deployable. Decision specific
attributes are described with candidates and
pertaining arguments. Enquiry specific attributes are
described with predefined attributes and their
pertaining values. All schedules that represent
possible selection are modelled with separate
entities.
Figure 3: ERD diagram.
2.3.2 UML Design
We present a conceptual object oriented design of
our application that capture the structure of
guideline-based decision support tool in “Figure 4”.
The “DecisionProcessor” is a controller class that
represents business logic and enables iteration
through guideline steps. For evaluation of our
expressions parameters and arguments are needed.
“Candidate”, “Argument” and “Parameter” are
persistent classes. Postfix calculator can evaluate an
expression with given arguments and parameters.
The “DecisionStepState” enables the monitoring of
each state of execution. Chosen actions and
evaluated decisions are represented with classes
“Action” and “Decision”. In this sub-section a brief
description of actual design is stated, so basically a
more complex model was implemented.
Figure 4: Conceptual class diagram.
2.3.3 Decision Model
The guideline modelling methods use a variety of
decision models. The decision models ranges from
simple if…then….else or switching constructs to
complex models such as decision trees. Our model
uses a decision tree, and selection among elements is
modelled by mutually exclusive preconditions that
depend on result of a decision task. The model uses
argumentation rules for/against/choice for selection
among alternatives. A none-deterministic choice is
possible, where more than one alternative may be
justifiable for a patient.
Expression language that defines preconditions,
post conditions, cycles and candidates is defined as a
complex expression containing operators, functions
and variables. Operators are arranged into formula
lexicon, term lexicon and unary lexicon. Each of
these describes the operators available at certain
parser priority. We have included 12 function
lexicons which cover a wide range of standard
functions, string functions, and other complex
functions. Also, 2 operator lexicons are included.
We have implemented more than 20 operators and
more than 200 functions in an expression parser that
is easily extendable with additional lexicon, or a new
operator or function.
2.3.4 Constructing Guideline
We have implemented an information system based
on CPG for modelling clinical knowledge. The
result of this implementation is a graphical composer
for creating machine interpretable guidelines. Those
guidelines are fully implemented on executable level
and can be executed to obtain appropriate clinical
actions. The main window of the guideline editor is
shown in “Figure 5”. Top node of the tree represents
HEALTHINF 2008 - International Conference on Health Informatics
116
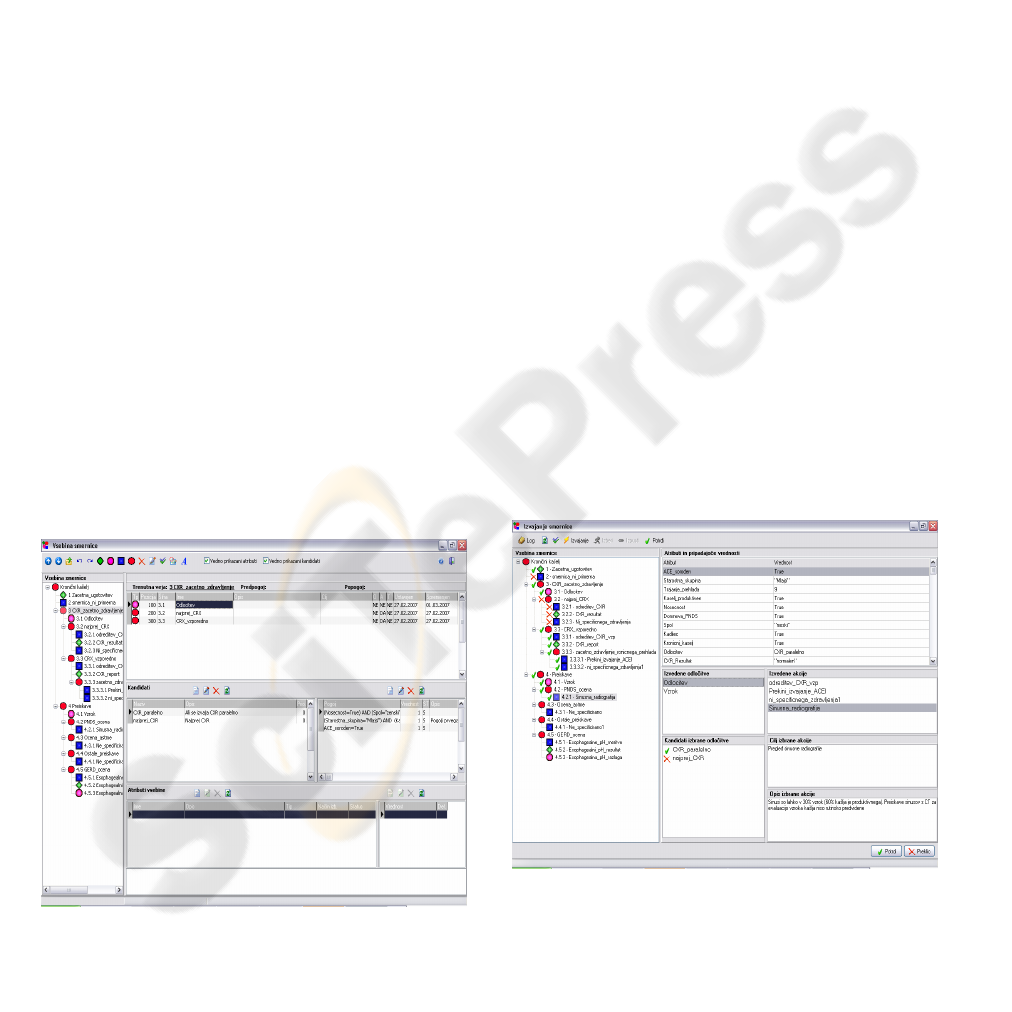
a main task that specifies information unrelated to
the health knowledge, and is used for maintenance,
change control, version control and other basic
information of the entire guideline.
The enquiry element is used for acquisition of
attributes that are needed at execution level of a
guideline. Attributes are described as optional or
mandatory, and their selection mode can be single or
multiple. They can be predefined, and each of them
ca be encapsulated within a specific attribute type.
Action task of a guideline is an important aspect,
but in this project it has been modelled as simple
textual description, and it is anticipated to be
executed outside of the information system.
Decision uses a well defined decision processor
with a rich mathematical expression language.
Augmentation rules are used to choose one or more
appropriate candidates. For each of them, we can
specify a multiple arguments that, when evaluated,
give logical result True or False. Each argument has
a given weight. A selection control can be set to
numeric mode or selective mode with the following
rules:
Rules that strictly exclude the alternative
Rules that argue against the alternative
Rules that argue for the alterative
Rules that confirm or express strong
preference for the alternative
A decision can also act as enquiry, in case it
requires additional data for its execution.
Execution of tasks depends on their predefined
precondition. Each executed task can inject a new
condition into algorithm flow.
Figure 5: Guideline composer.
3 EXECUTING GUIDELINES
This subsection represents execution of guidelines
modelled with our guideline composer. As a test of
guideline execution, two guidelines were composed
and executed for the purposes of testing. The first
was treatment of chronic cough taken from the
studies of PROforma, and the other one the
determination and classification of hypertension
disease taken from textual format using a book
“Evidence based guidelines” and transformed into
executable form.
At this point a guideline is represented at the
executable level. The guideline execution is shown
in “Figure 6”. The left side of the picture shows a
guideline content in execution process which
provides the overview about which elements are
chosen and which rejected. A user can also see a
diary of events and check guideline for errors.
During the runtime some occurrences need a user
conformation which enables an interaction in
guideline execution process. Also some tasks are
optional and are to be confirmed or rejected. The
left-top part of the “Figure 6” shows guideline
attributes and their values which are valid at a
moment. Also, chosen decisions and their evaluated
candidates are shown for each execution step. In the
right-bottom part appropriate actions are shown,
together with their description and intention.
The intention of executing CPGs with this
application is to obtain regularity of CPGs or to
confirm already valid health care process.
Figure 6: Guideline execution.
CLINICAL PRACTICAL GUIDELINE EDITOR - Clinical Practical Guideline-based Decision Support Tool
117

4 CONCLUSIONS
Growth of information about appropriate clinical
treatment is enormous and makes its appropriate use
in practice impossible. The purpose for building
decision support systems for treatment process is to
enable easy access to clinical knowledge. That is
what should be the lead force for developing an
appropriate and standardized CDSS.
By studying some of the many methods for
representing clinical knowledge, guideline
modelling and execution tools were developed. One
of the most important aspects when developing a
decision support tool is sharing information among
other institutions which leads to a need to build a
centralized data storage. For this purpose a relation
database model has been developed and
implemented. Model is flexible and fully extendable
for further development. Application itself uses a
multi user application server that enables sharing
medical knowledge among users and institutions.
For building a clinical guideline with composer a
simple and easy understandable guideline constructs
were implemented that are understandable to a
person with none or poor computer knowledge.
Design of the application is object orientated
and, if needed, extendable with other construct.
Expression/criterion language uses a reach postfix
mathematical parser. Among many already
implemented operators and functions, it is possible
to develop as many as needed user defined lexicons
and inject them into the parser. This leads to a very
flexible and adaptable expression language that can
be used for complex decision making.
A newly proposed design represents an
innovation in that it uses relational database support
and a reach mathematical expression language
parser which enables an infinitive and complex
decision modelling.
For now, the application’s primary goal is to
build clinical practice guidelines and execute them
in patient care process in order to obtain
recommendable actions. Further development could
lead to inductive learning, the statistical evaluation
of effectiveness and appropriateness of guidelines by
testing their regularity in a specific care procedure.
REFERENCES
Wyatt, J., Spiegelhalter, D. 1991. Field trials of medical
decision-aids: potential problems and solutions,
Proceedings of the 15th Symposium on Computer
Applications in Medical Care.
Osheroff, J., Bankowitz, R., 1993. Physicians’ use of
computer software in answering clinical questions.
Bull Med Library Association.
Hunt, D., Haynes, B., Segal, H., et al., 1998, Effects of
computer-based clinical decision-support systems on
physician performance and patient outcomes, JAMA,
280:1339–46.
Fox, J., Bury, J., Humber, M., Sutton, D., Integrating
Bayesian inference into the PROforma language,
Advanced Computation Laboratory, Imperial Cancer
Research Fund, London
Bury, J., Fox, J., Sutton, D., The PROforma guideline
specification language: progress and prospects.
Peleg, M., Boxwala, A.A., Ogunyemi, O., Zeng, Q., Tu,
S.W., Lacson, R., Bernstam, E., Ash, N., Mork, P.,
Ohno-Machado, L., Shortliffe, E.H., Greenes, R.A.,
GLIF3: The Evolution of a Guideline Representation
Format,1 Stanford Medical Informatics, Stanford
University School of Medicine, Decision Systems
Group, Harvard Medical School, Brigham &
Women’s Hospital, Department of Medical
Informatics, Columbia University
Sordo, M., Ogunyemi, O., Boxwala, A.A., Greenes, A.R.,
Tu, S.W., GELLO: An Object-Oriented Query and
Expression Language for Clinical Decision Support,
Decision Systems Group, Brigham & Women’s
Hospital, Harvard Medical School, Section of Medical
Informatics, Stanford University School of Medicine,
Stanford.
Peleg, M., Boxwala, A., Modeling Clinical Guidelines in a
Sharable and Computer-interpretable Way:
Development, Implementation, and Use Requirements
Instructors, Stanford Medical Informatics, Stanford
University School of Medicine, Decision Systems
Group, Harvard Medical School, Brigham &
Women’s Hospital, Boston, MA.
Tu, S.W., Campbell, J., Musen, A.M., The Structure of
Guideline Recommendations: A Synthesis, Stanford
Medical Informatics, Stanford University School of
Medicine, Stanford, University of Nebraska Medical
Center, Nebraska Health Systems, Omaha
Plavčak, A., 2007. Clinical Decision Support System,
Diploma work.
HEALTHINF 2008 - International Conference on Health Informatics
118
