
Role of Artificial Intelligence of Things (AIoT) in Covid-19 Pandemic: A
Brief Survey
Venkatesh K. Pappakrishnan
1
, R. Mythili
2
, V. Kavitha
2
and N. Parthiban
2
1
Palo Alto Networks, CA, U.S.A.
2
Department of Computer Science and Engineering,
SRM Institute of Science and Technology, Kattankulathur, Tamilnadu, India
Keywords:
AIoT, Healthcare 4.0, COVID-19, IoT, AI, Smart Healthcare.
Abstract:
Digital twins, Internet of Things (IoT) and Artificial Intelligence (AI), plays a proactive role in numerous
ways during a pandemic such as COVID-19 by allowing us to make informed decisions using real-time data.
According to World Health Organization (WHO), COVID-19 is an infectious disease caused by Severe Acute
Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) that predominantly spreads through body fluids, leading
to a mild-to-severe respiratory illness. Considering the global health crisis due to COVID-19 and novelty of
the SARS-CoV-2 virus due diligence is required in vaccine preparation and human trials. At the early stages
of the pandemic, due to lack of complete knowledge on the virus, there are two main objectives: (1) treat
patients as effectively as possible and (2) control the spread of the disease. IoT devices in healthcare empower
the healthcare industry in identifying potential carriers of COVID-19 and quarantine. Even though IoT plays
a major role in healthcare 4.0, decision making capabilities are limited due to the type of the algorithms and
decision making paradigms used. Using AI, we will be able to identify critical medical conditions earlier
and take necessary steps. Artificial Intelligence of Things (AIoT) implementation has the potential to greatly
reduce the mortality rate allowing us in early identification of high-risk patients, monitoring the spread of the
disease, methods to limit the spread, predict mortality risk by analyzing patient’s health history, remote or
in-home treatments to reduce hospital occupancy, and other techniques to significantly control the spread and
treat the patients effectively.
1 INTRODUCTION
Artificial Intelligence (AI) has gained a lot of trac-
tion recently and has been widely adopted and rev-
olutionizing various fields including healthcare, re-
tail, banking, financial services, marketing, travel,
real estate, logistics, and food technology (Hall and
Pesenti, 2017). Internet of Things (IoT) is a group
of interconnected devices that are programmed to
act individually or collectively with the knowledge
gained through all the interconnected devices (Ini-
tiative et al., 2015). IoT devices typically contain
sensors to collect useful data, processor and mem-
ory units, internet capability, and part of a network
of millions of similar devices (Atzori et al., 2010).
The collected data are either processed locally using
edge computing which can efficiently handle a small
amount of data within a limited bandwidth which pro-
vides us enhanced security mechanisms (local), low-
latency, and faster responsiveness or using fog com-
puting. The fog computing is a decentralized archi-
tecture where the computing is performed at the fog
node which is located within the LAN providing the
same advantages as edge computing in terms of data
security and latency. The intelligence still remains
close to the source of the data. However, when heavy
data processing and computation is required due to
the volume and velocity of the data, then cloud com-
puting is the best alternative which comes at the cost
of high latency, high cost, and possible data secu-
rity issues (Armbrust et al., 2010). Recently, more
focus is given to edge computing especially for IoT
applications due to high responsiveness, improved
performance, and better data security compared to
fog and cloud computing architectures (Hassan et al.,
2018). AIoT (Artificial Intelligence of Things) is
the combination of AI’s computational power and
IoT’s collective interoperability that pushes the limits
on the intelligence of smart devices by empowering
them to perform highly challenging tasks which are
Pappakrishnan, V., Mythili, R., Kavitha, V. and Parthiban, N.
Role of Artificial Intelligence of Things (AIoT) in Covid-19 Pandemic: A Brief Survey.
DOI: 10.5220/0010461502290236
In Proceedings of the 6th International Conference on Internet of Things, Big Data and Security (IoTBDS 2021), pages 229-236
ISBN: 978-989-758-504-3
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
229

technically impossible with current IoT architectures
(Ghosh et al., 2018; Poniszewska-Maranda and Kacz-
marek, 2015; Gonz
´
alez Garc
´
ıa et al., 2019). AIoT has
been widely adopted in different sectors such as retail,
healthcare, automobile, home appliances, etc (Ghosh
et al., 2018).
Industrial revolution 4.0 (I4.0) is the integration
of technologies from different sectors such as IoT,
AI, Big Data, 5G, etc (Lampropoulos et al., 2019).
There are four major components in I4.0: Cyber
Physical System (CPS), IoT, resource availability, and
cognitive computing. Information and Communica-
tion Technology (ICT) is the integration of infor-
mation through telecommunication and the compo-
nents in the ICT are computing, communications, and
entertainment that helps in exchange of information
through digital electronic media. Health-CPS is des-
ignated for patient-centric healthcare applications and
services which is based on cloud computing and big
data analytics (Zhang et al., 2015). Healthcare 4.0 is
an integral component of Industry 4.0 where differ-
ent domains of the industries are integrated through
personalization and virtualization. It revolves around
the idea of how a centralised health care system such
as hospitals, provide a decentralized patient-friendly
health care services using innovative research fields of
computer science such as IoT, AI, big data, robotics
and so on (Javaid and Haleem, 2019; Javaid and
Haleem, 2018; Ekstrand et al., 2018).
Figure 1: Components of Healthcare 4.0 (H4.0).
Figure 1 shows different components in H4.0
which are borrowed from I4.0 with applications tai-
lored to the healthcare industry. As everyone is con-
nected through digital technologies, ICT helps in im-
proving healthcare for individuals and larger com-
munities (Thilakarathne et al., 2020). ICT monitors
and controls every component in the system includ-
ing hardware such as sensors and actuators. All the
components should follow a predetermined procedure
and require constant monitoring and periodic mainte-
nance.
In H4.0, patients’ data are continuously collected
using various sensors and stored in a cloud infras-
tructure for data analysis and predictive modeling. In
IoT based health care systems, sensors connected to
micro-controllers (eg. arduino) and integrated chips
(eg. raspberry pi) monitor health statistics and vi-
tal parameters such as body temperature, pulse rate,
respiratory rate, blood glucose level, and ECG (Ku-
mar et al., 2017). For effective communication, wire-
less technologies currently used in IoT are: (1) wide
area cellular technologies such as GSM, LTE and 5G,
(2) short range technologies such as ZigBee, Z-wave,
WiFi and Bluetooth, and (3) low power technologies
such as LoRa and Sigfox are used (Qadir et al., 2018).
This paper is organised as follows: In section 2
we discuss the pandemic evolution and the challenges
faced. In section 3 we present existing work related
to AI and IoT in the field of healthcare. In section 4
we discuss the technologies currently available for di-
agnosis and monitoring of patients. In section 5 we
discuss the process flow of telemedicine using AIoT,
remote health monitoring, and telematics. This is fol-
lowed by applications and benefits of AIoT during
pandemics. In section 6 we briefly discuss the secu-
rity challenges of personal health data and finally in
section 7 we summarize all the important findings.
2 PANDEMIC OVERVIEW AND
CHALLENGES
Infectious diseases are classified into endemic, epi-
demic, and pandemic based on geographic spread and
scale of the people infected. A pandemic is usu-
ally triggered by a zoonotic transmission of pathogens
from animals to humans (Belay et al., 2017). This is
due to the fact that human’s immune system are not
evolved to fight pathogens from other species, espe-
cially the ones that are from uncommon environmen-
tal conditions known to humans.
The following are the common challenges faced
during a pandemic (Madhav et al., 2017):
• Lack of preparedness after the initial outbreak
as the developing countries have limited financial
and technical resources.
• Shortage in essential medical necessities such as
gloves, masks, syringes, etc. Unavailability of an-
tiviral agents and vaccines.
• Insufficient number of healthcare workers and
lack of training in specialized areas for effective
control of the infection in the early stages.
• Economic downfall including short-term fiscal
shocks and longer-term negative impact to the
economic growth.
IoTBDS 2021 - 6th International Conference on Internet of Things, Big Data and Security
230
• Slowdown in social and economic growth due to
pandemic mitigation plans from every country.
• High morbidity and mortality rates due to poor
public health resources and population density
(Oshitani et al., 2008).
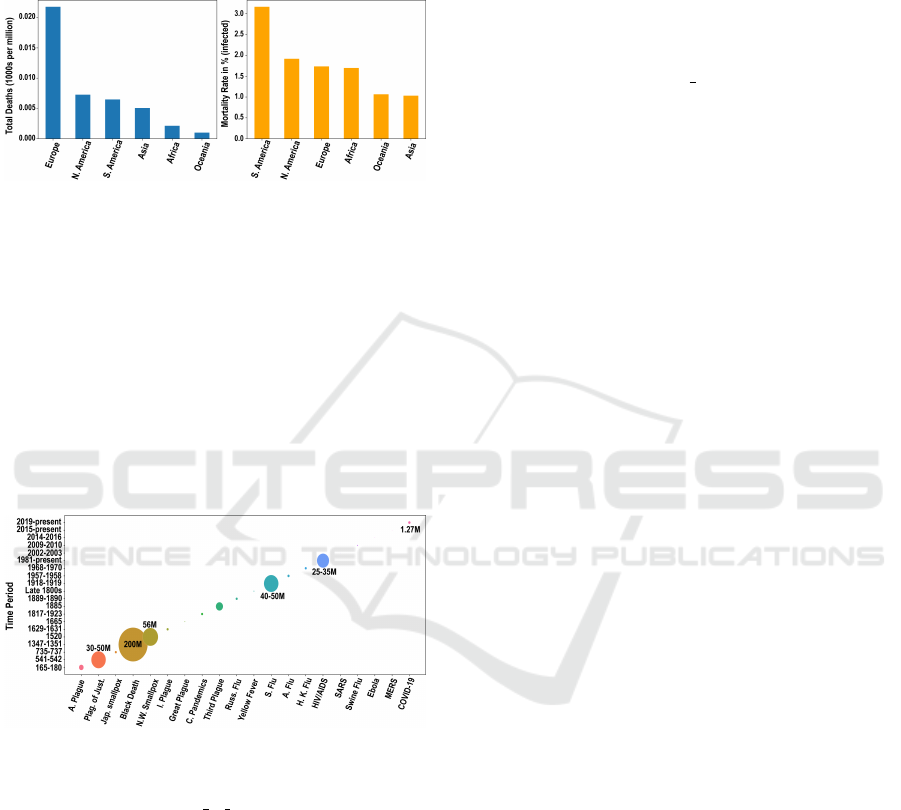
Figure 2: (a) Total deaths and (b) mortality in per-
centage across different continents (data source: https://
ourworldindata.org/coronavirus-data).
Mortality rate and total deaths of the COVID pa-
tients are continuously tracked and periodically pub-
lished for the public by various organizations and uni-
versities including WHO and John Hopkins Univer-
sity. Europe has been critically affected in terms of
total deaths followed by N. America and other con-
tinents (Figure 2 (a)) and in terms of mortality rate,
which considers only infected patients, S. America
has been severely affected with over 3% mortality rate
(Figure 2 (b)).
Figure 3: Impact of pandemics (death count)
during different time periods (data sources:
https://www.worldometers.info/coronavirus/, https:
//en.wikipedia.org/wiki/List of epidemics).
Figure 3 depicts the death count during each pan-
demic that are known to us. One of the recent pan-
demics that has been making a significant impact is
HIV/AIDS with over 35M deaths and this is mainly
due to the nature of the virus itself and lack of tech-
nological advancements to predict and control the
spread during that period. The COVID-19 has al-
ready claimed over 1.27M lives across the world as of
Nov 2020 (Organization et al., 2020) and continues to
climb. Recent technological advancements allows us
to accelerate the research and development of the vac-
cine for SARS-CoV-2 compared to the technologies
we had during HIV/AIDS outbreak. According to the
WHO, there are currently more than 60 COVID-19
vaccine candidates in clinical development and over
170 in pre-clinical development.
For COVID-19 two types of vaccines are de-
veloped by three major pharmaceutical companies:
Pfizer-BioNTech COVID-19 Vaccine (pfizer, BioN-
Tech) (Tanne, 2020), Moderna COVID-19 Vaccine
(Morderna) (Cohen, 2020), and Serum Institute of In-
dia (Covishield ChAdOx1 nCoV19). The vaccines
show promising results based on initial human tri-
als and released to public. However, the side effects
and the effectiveness of the vaccine still needs fur-
ther study. Although, various hospitals are pioneer-
ing in smart healthcare and forge ahead for better and
advanced treatments, there still prevails various chal-
lenges in this sector (Zhu, 2019; Gastaldi and Corso,
2012).
3 RELATED WORK
Pardeshi et al., explains the process remote moni-
toring of patients remotely, data storage techniques,
data processing, and data transmission methods along
with the hardware and the software required for the
successful monitoring of the patients (Pardeshi et al.,
2017). Remote monitoring system is used for keeping
track of non-critical patients from their home with-
out the need for hospital occupancy. Islam et al., dis-
cusses the advances imposed in the IoT industry and
various industrial implementations of healthcare solu-
tions along with a detailed explanation of a collabora-
tive security model to address the security issues (Is-
lam et al., 2015). Rodrigues et al., discusses products,
services, and features of IoHT technology (Rodrigues
et al., 2018). Smart clothing based health care system
has been introduced as Wearable 2.0 to support bed-
ridden patients with accurate monitoring of health
statistics (Chen et al., 2017). To improve the energy
efficiency of the IoT devices, ARM micro controllers
are used for collecting real-time data. Pang et al.,
discusses the advancement in automation, biomedi-
cal industry, and health analytics and identifies the
research gap and industrial demands to set direction
on future research (Pang et al., 2018). Assisted liv-
ing for the elderly people can be achieved using AIoT;
Genni an intelligent IoT application designed as a per-
sonal assistant using wearable technology for moni-
toring vital signs such as heart rate, blood pressure,
sleep hours, etc., and integrate them in a distributed
data management framework for demonstrating data
interoperability and data accessibility (Serrano et al.,
2018). In spite of strong security measures to protect
Role of Artificial Intelligence of Things (AIoT) in Covid-19 Pandemic: A Brief Survey
231

patients medical e-records, security breaches may still
occur due to various unique techniques followed by
the hackers. The security challenges include privacy
and confidentiality of the patients data. According to
Ermakova et al., due to the privacy concerns, patients
are still skeptical and less likely to prefer cloud envi-
ronments for storing their medical records (Ermakova
et al., 2013; Kuo et al., 2014). AIoT is currently used
for cardiac disease detection and analysis of electro-
cardiogram (ECG) signals. Convolution Neural Net-
work (CNNs) are used for arrhythmia classification
(Lin et al., 2019).
4 DIAGNOSIS AND
MONITORING OF COVID-19
PATIENTS
According to the WHO, the most common symp-
toms of COVID-19 are fever, dry cough and tired-
ness and the less common symptoms are aches and
pains, sore throat, diarrhoea, conjunctivitis, headache,
etc. Severe symptoms include difficulty in breath-
ing, chest pain, loss of speech or movement (Chamola
et al., 2020). For effective identification, the diag-
nosis needs to be scaled up to test millions of po-
tential patients with symptoms which is critical dur-
ing a pandemic. For scaling up, the challenges in-
clude availability of the medical kits, trained health
care workers, and health care facility. IoT would
tackle the challenge by integrating the medical de-
vices with the in-built sensors, algorithms and mo-
bile health applications. AI, virtual healthcare man-
agement, and telemedicine reduces the manual inter-
ventions in considerable way thereby protect the front
line workers. The image sensing such as CT scans
and X-ray detect and classifies the abnormalities ob-
served. This intelligent classification will enhance the
automation process, less intervention of the physician
with the patients. The performance of analytics helps
in monitoring the spread of COVID-19. The com-
plexity in handling the applications has been reduced
and the technology is easy to adapt. Although there
are several challenges, AI and IoT would help us op-
timize logistics of medical kits and required equip-
ment to reduce shortage during critical times, improve
the accuracy of the diagnosis, efficient and effective
data collection required for gain better understand-
ing of the disease and in developing accurate algo-
rithms or models. There are sensors that help us in
pure data collection and others that allow us to con-
tinuously monitor the patients for taking necessary
actions. Here we have listed sensors and devices in
the table 1 that are known to be quite helpful so far
in the early detection of COVID-19 symptoms and
monitoring of affected patients. The contact trac-
ing applications developed by various countries are
COVIDSafe (Australia), Stopp Corona (Austria), e-
Tabib (Azerbaijan), Corona Tracer BD (Bangladesh),
CoronApp (Colombia), Smittestop (Denmark), Stop-
Covid (France), Corona-Warn-App (Germany), Aar-
ogya Setu app (India), and HaMagen (Israel).
5 AIoT FOR COVID-19
AIoT holds a tremendous potential in addressing
the limitations of IoT in H4.0. A typical process
of AIoT system involves three main components:
telemedicine, remote data gathering, and algorithm.
The telemedicine segment includes both the sensors
for recording data or monitoring health of patients
and the actuators to act physically based on the signal
either from health care practitioner (semi-automated
system) or the algorithm directly (fully-automated
system). The collected data is pre-processed and
stored in distributed storage system and the data can
be processed in batch mode or streaming mode for
model building and prediction. During every batch or
cycle, the data collected is used for predicting the next
behavior. The algorithm could be re-trained periodi-
cally like every 3-6 months using last n days of data
or the entire data set.
5.1 Contact Tracing and Tracking
Contact tracking is the process of monitoring a person
who has been exposed to the disease in-order to alert
his contacts to curtail the transmission of the disease
(Thayyil et al., 2020). The contact tracing and track-
ing API have been developed by Google and Apple
and they provide a GUI platform for building trac-
ing apps using which a user can participate in digi-
tal contact-tracing. For instance, if two people meet
for five minutes or more, an identifier is exchanged
between their phones via Bluetooth. Later, if one of
them is tested positive for COVID–19, an alert noti-
fication is send to the other person’s phone who has
come in contact with him. Privacy is preserved as
user’s location and other details are not shared. Trac-
ing and tracking of patients and their health statistics
is discussed in detail in (Nazirun et al., 2017).
IoTBDS 2021 - 6th International Conference on Internet of Things, Big Data and Security
232

Table 1: Types of Sensors.
SENSOR MEASURES / MONITORS COMPANY
Temperature Body temperature Analog devices, Mitsumi, Melexis
Pressure Blood pressure Sensata Technologies, IFM Efector,
Keller America
Airflow Breathing rate HydraCheck, RCM Industries, Inc.,
ERDCO Engineering Corporation
Oxygen Oxygen level Honeywell, Unimed, Cubic
Electrocardiogram Heart rate NeuroSky, Eko Devices, Inc. , Cognionics
Accelerometers Movement of body First Sensor Inc., Baumer Group, Colibrys SA
Biosensors Level of cholesterol InnovoGENE Biosciences, Biodot, Aryballe
5.2 Telehealth, Remote Health
Monitoring, and Telematics
With ever increasing number of COVID-19 patients
across the globe, automation of healthcare workers’
duties will be of great deeds (Alwashmi, 2020). This
would reduce medical expenditures and in-facility
congestion. Remote Patient Monitoring (RPM), also
called home-care telehealth, allows patients to per-
form a routine check up, send real-time data to the
medical practitioner, and receive medicines through
home delivery (Avitall et al., 2001). RPM technol-
ogy with the introduction of biosensors makes health
care accessible to remote areas requiring timely ac-
tion. The WHO describes the synergy of telehealth
and telemedicine as telematics, a term for information
technology based health care activities. Telemedicine
Figure 4: Remote Health monitoring.
involves distance learning component wherein con-
sultation of the case management can also be per-
formed between the physicians at different geolo-
cations. The prescription and drug management is
also enhanced by tracking and delivering drugs to
the concerned client and to analyze the side effects
of the same, if any (Organization et al., 2019). In
telemedicine although the doctors can check the ex-
ternal features for diagnosis, however there are still
challenges that exist including checking of the heart
beat, blood pressure, etc. In this scenario, wearables
play a vital role to monitor heart rate and blood pres-
sure and abnormalities could be diagnosed in earlier
stages. The factors influencing the telemedicine de-
ployment are the installation space, network availabil-
ity, proper management of sensors and wearables, and
proper adherence to the health care polices and digi-
tal infrastructure. The incident rate for COVID-19 is
increasing exponentially; in such a scenario reverse
quarantine would be the best possible monitoring sys-
tem in near future (Raveendran and Jayadevan, 2020).
Figure 4 shows remote health monitoring system that
collects the medical health data using the sensors and
actuators from one place and transmit it to the cloud
infrastructure and can be used for decision making
and analytics to the physicians or healthcare providers
for medical assessment or medicine recommenda-
tions. Here is a list of telemedicine apps developed by
companies worldwide: Mfine (Novocura Tech), eSan-
jeevaniOPD (C-DAC, India), Practo (Practo), Doc-
Clocker (Fast Pathway), and CMED Health (CMED).
5.3 AI and IoT Applications in
Pandemic and beyond
• Early Warning System: BlueDot, an AI based
company detected and notified to its users an out-
break of pneumonia cases (Wuhan, China) as dig-
ital smoke signal even before it was officially de-
clared by WHO. The AI VFusion platform by Vi-
vace Health Solutions is reliable in identifying
Acute Respiratory Distress Syndrome (ARDS).
• Tracking the Spread of Virus: AI-based
Healthmaps integrate data sources from Google
and other social media platforms. The data are
then sent to epidemiologist for the detection of
early sign of a possible outbreak. Healthmaps in
the Boston Children’s Hospital first recognizes the
kind of pneumonia attacking a group of people.
• Contact Tracing: Geo-location data are used to
identify people coming in close contact with each
other and notify them directing to isolate them-
Role of Artificial Intelligence of Things (AIoT) in Covid-19 Pandemic: A Brief Survey
233

selves if one of them is infected.
• Prediction of Virus Protein Structure: Deep-
Mind, a company developed a method to predict
the virus protein structures using AlphaFold AI
system (Alimadadi et al., 2020). They have re-
leased AlphaFold, a deep learning library that use
neural networks for predicting how the proteins
that make organisms crinkle or curve on the basis
of their genome. This predicts the receptor shape
in the cells of the living being. By learning its
shape drug development becomes easier.
• Early Detection and Diagnosis: AI and digital-
imaging are used together with the COVID-19 de-
tection neural network (COVNet) algorithm to de-
tect positive cases using the chest computed To-
mography (CT) images (Li and Xia, 2020). XG-
Boost machine learning based model to predict
survival rates of the COVID-19 affected patients
using blood samples data.
• Robots: Robots are deployed to respond to imme-
diate needs in hospitals such as delivery of food,
medications and equipment, to cleanse and ster-
ilise tools, and to aid medical practitioners. Asi-
mov Robotics, a robotic service provider com-
pany based in India, assist patients with their
needs to minimize the risk of health-care work-
ers. UVD Robots, emit powerful UV light that
can disinfect surfaces (Chamola et al., 2020).
• Drones: Drones are deployed for crowd surveil-
lance and to avoid gathering of people in large
groups. In India, drones are used to monitor
body temperature using an array of infrared (IR)
sensors and supply commodities, medical kits,
food supplies, and collect samples from people
for COVID-19 diagnosis (Anggraeni et al., ; Mo-
hammed et al., 2020).
5.4 Advantages of AIoT during a
Pandemic
AI allows us to minimize the workforce required to
achieve a task which is critical during a pandemic.
Chatbots, a NLP based AI application, is vital in
spreading general awareness to the public. Viola-
tion of rules in areas with restricted movements can
be monitored efficiently using unarmed aerial vehi-
cles (UAV), real-time monitoring using closed cir-
cuit television (CCTV) reduces the incident rate of
COVID-19. Medical fraternities are moving towards
e-learning to abridge the gap in medical workforce
(Jecker et al., 2020; Tang et al., 2020). ML algo-
rithms, a subset of AI system helps in the following
ways to handle such pandemics:
• Screening of Individuals: Using CNNs people
with illness, sweating, and discoloration can be
detected using thermal scanning face cameras.
Wearable rings are used at the University of Cali-
fornia to track health statistics of people.
• Chatbots for Diagnostic: Chatbots can be pro-
grammed to feed patients with a questionnaire
about their symptoms as a part of self triage,
hence reducing the risk of infection to other
health-care workers.
• Risk Prediction: Health risk of a patient can be
determined using various factors such as age, gen-
eral hygiene, and social interactions.
• Bio Medical Knowledge Graphs: Using NLP,
entities of drugs and proteins are connected to-
gether as structured graphs. Similarly, customised
BenevolentAI knowledge graph is used to find
the connection between COVID-19 and Barici-
tinib (Richardson et al., 2020).
6 SECURITY CHALLENGES OF
DATA
Health records are continuously monitored and
recorded using telemonitoring facilities, there exists a
potential security threat (Singh et al., 2020). Tamper-
ing of data, unauthorized access of personal informa-
tion of the patients, sensitive and confidential infor-
mation breach, Distributed Denial of Service (DDoS)
are possible as the records are most likely placed in a
centralized server. A poorly configured central server
in terms of network security, all the sensitive content
could be compromised and data would be leaked. To
limit the security threats, it is important to highest
privileges to only few individuals who are qualified
to handle. By limiting the number people with broad
privileges we could greater reduce the chances of be-
ing hacked (Tarouco et al., 2012). According to Anas-
tasios Arampatzis, most of the healthcare threats are
done using hidden HTTPS and Domain Name Server
(DNS) tunnels, ransomware, and BOTNET. Neces-
sary privacy policies need to be adhered to protect
against unauthorized access to health records. Tele-
health sector must be provided with enhanced authen-
tication, authorization and accountability (Williams
and McCauley, 2016). Data integration and consis-
tency is an another major challenge. A proper envi-
ronment has to be provided in-order to integrate large
sets of data and to make them readily available for
accessing and analyzing at any given point of time.
According to TrapX report, some hospitals are prone
IoTBDS 2021 - 6th International Conference on Internet of Things, Big Data and Security
234

to medical device hijacking which is also called med-
jacking. A different scenario includes radiology im-
age storage system connected to the main server gets
compromised and the sensitive contents are leaked. In
another scenario attackers could use a vulnerability in
drug pumps to control the hospital’s network.
7 SUMMARY
Healthcare 4.0 integrated with AI would greater help
in lowering the mortality rate during a pandemic such
as COVID-19. We specifically discussed the role of
IoT with various sensors to monitor health remotely
and how AI would further improve the capabilities
in terms of accurate detection of the disease, trac-
ing and tracking of infected/potential patients, etc.,
allowing us to proactively handle the situation. The
need for digital intervention in healthcare and sup-
porting structures has also been discussed along with
the security challenges in protecting patients medical
records. Finally, we have proposed ideas and listed
relevant works on AIoT in healthcare and how it could
be used to improve the current healthcare system even
beyond 4.0.
REFERENCES
Alimadadi, A., Aryal, S., Manandhar, I., Munroe, P. B., Joe,
B., and Cheng, X. (2020). Artificial intelligence and
machine learning to fight covid-19.
Alwashmi, M. F. (2020). The use of digital health in
the detection and management of covid-19. Interna-
tional Journal of Environmental Research and Public
Health, 17(8):2906.
Anggraeni, S., Maulidina, A., Dewi, M. W., Rahmadianti,
S., Rizky, Y. P. C., Arinalhaq, Z. F., Usdiyana, D.,
Nandiyanto, A. B. D., and Al-Obaidi, A. S. M. The
deployment of drones in sending drugs and patient
blood samples covid-19. Indonesian Journal of Sci-
ence and Technology, 5(2):18–25.
Armbrust, M., Fox, A., Griffith, R., Joseph, A., Katz, R.,
Konwinski, A., Lee, G., Patterson, D., Rabkin, A.,
Stoica, I., and Zaharia, M. (2010). A view of cloud
computing. Commun. ACM, 53:50–58.
Atzori, L., Iera, A., and Morabito, G. (2010). The internet of
things: A survey. Computer networks, 54(15):2787–
2805.
Avitall, B., Peterson, B., Kletch, J., Griswold, E. B., and
Moran, P. (2001). Remote health monitoring system.
US Patent 6,171,237.
Belay, E. D., Kile, J. C., Hall, A. J., Barton-Behravesh,
C., Parsons, M. B., Salyer, S., and Walke, H.
(2017). Zoonotic disease programs for enhancing
global health security. Emerging infectious diseases,
23(Suppl 1):S65.
Chamola, V., Hassija, V., Gupta, V., and Guizani, M.
(2020). A comprehensive review of the covid-19 pan-
demic and the role of iot, drones, ai, blockchain, and
5g in managing its impact. IEEE Access, 8:90225–
90265.
Chen, M., Ma, Y., Li, Y., Wu, D., Zhang, Y., and Youn, C.-
H. (2017). Wearable 2.0: Enabling human-cloud in-
tegration in next generation healthcare systems. IEEE
Communications Magazine, 55(1):54–61.
Cohen, J. (2020). Vaccine designers take first shots at covid-
19.
Ekstrand, C., Jamal, A., Nguyen, R., Kudryk, A., Mann,
J., and Mendez, I. (2018). Immersive and interac-
tive virtual reality to improve learning and retention
of neuroanatomy in medical students: a randomized
controlled study. CMAJ open, 6(1):E103.
Ermakova, T., Fabian, B., and Zarnekow, R. (2013). Se-
curity and privacy system requirements for adopting
cloud computing in healthcare data sharing scenarios.
Gastaldi, L. and Corso, M. (2012). Smart healthcare digi-
talization: Using ict to effectively balance exploration
and exploitation within hospitals. International Jour-
nal of Engineering Business Management, 4(Godi
ˇ
ste
2012):4–9.
Ghosh, A., Chakraborty, D., and Law, A. (2018). Artificial
intelligence in internet of things. CAAI Transactions
on Intelligence Technology, 3(4):208–218.
Gonz
´
alez Garc
´
ıa, C., N
´
u
˜
nez Vald
´
ez, E. R., Garc
´
ıa D
´
ıaz,
V., Pelayo Garc
´
ıa-Bustelo, B. C., and Cueva Lovelle,
J. M. (2019). A review of artificial intelligence in the
internet of things. International Journal of Interactive
Multimedia and Artificial Intelligence.
Hall, W. and Pesenti, J. (2017). Growing the artificial in-
telligence industry in the uk. Department for Digital,
Culture, Media & Sport and Department for Business,
Energy & Industrial Strategy. Part of the Industrial
Strategy UK and the Commonwealth.
Hassan, N., Gillani, S., Ahmed, E., Yaqoob, I., and Imran,
M. (2018). The role of edge computing in internet of
things. IEEE communications magazine, 56(11):110–
115.
Initiative, I. I. et al. (2015). Towards a definition of the
internet of things (iot)(revision-1).
Islam, S. R., Kwak, D., Kabir, M. H., Hossain, M., and
Kwak, K.-S. (2015). The internet of things for health
care: a comprehensive survey. IEEE access, 3:678–
708.
Javaid, M. and Haleem, A. (2018). Additive manufactur-
ing applications in medical cases: A literature based
review. Alexandria Journal of Medicine, 54(4):411–
422.
Javaid, M. and Haleem, A. (2019). Industry 4.0 applications
in medical field: a brief review. Current Medicine
Research and Practice, 9(3):102–109.
Jecker, N. S., Wightman, A. G., and Diekema, D. S. (2020).
Prioritizing frontline workers during the covid-19
pandemic. The American Journal of Bioethics, pages
1–5.
Kumar, S. P., Samson, V. R. R., Sai, U. B., Rao, P. M., and
Eswar, K. K. (2017). Smart health monitoring system
Role of Artificial Intelligence of Things (AIoT) in Covid-19 Pandemic: A Brief Survey
235

of patient through iot. In 2017 international confer-
ence on I-SMAC (IoT in social, mobile, analytics and
cloud)(I-SMAC), pages 551–556. IEEE.
Kuo, K.-M., Ma, C.-C., and Alexander, J. W. (2014). How
do patients respond to violation of their information
privacy? Health Information Management Journal,
43(2):23–33.
Lampropoulos, G., Siakas, K., and Anastasiadis, T. (2019).
Internet of things in the context of industry 4.0: An
overview. International Journal of Entrepreneurial
Knowledge, 7(1):4–19.
Li, Y. and Xia, L. (2020). Coronavirus disease 2019 (covid-
19): role of chest ct in diagnosis and management.
American Journal of Roentgenology, 214(6):1280–
1286.
Lin, Y.-J., Chuang, C.-W., Yen, C.-Y., Huang, S.-H., Huang,
P.-W., Chen, J.-Y., and Lee, S.-Y. (2019). Artificial
intelligence of things wearable system for cardiac dis-
ease detection. In 2019 IEEE International Confer-
ence on Artificial Intelligence Circuits and Systems
(AICAS), pages 67–70. IEEE.
Madhav, N., Oppenheim, B., Gallivan, M., Mulembakani,
P., Rubin, E., and Wolfe, N. (2017). Pandemics: risks,
impacts, and mitigation.
Mohammed, M., Hazairin, N. A., Al-Zubaidi, S., AK, S.,
Mustapha, S., and Yusuf, E. (2020). Toward a novel
design for coronavirus detection and diagnosis system
using iot based drone technology. International Jour-
nal of Psychosocial Rehabilitation, 24(7):2287–2295.
Nazirun, N. N. N., Shakhih, M. F. M., Ren, P. C., Zaini,
M. A. A., Nordin, N., Empaling, S., Amran, D. I., and
Supriyanto, E. (2017). User acceptance analysis of
hospital asset management system. In 2017 Interna-
tional Conference on Robotics, Automation and Sci-
ences (ICORAS), pages 1–5. IEEE.
Organization, W. H. et al. (2019). Who guideline: recom-
mendations on digital interventions for health system
strengthening: web supplement 2: summary of find-
ings and grade tables. Technical report, World Health
Organization.
Organization, W. H. et al. (2020). Covid-19 weekly epi-
demiological update, 24 november 2020.
Oshitani, H., Kamigaki, T., and Suzuki, A. (2008). Major
issues and challenges of influenza pandemic prepared-
ness in developing countries. Emerging infectious dis-
eases, 14(6):875.
Pang, Z., Yang, G., Khedri, R., and Zhang, Y.-T. (2018).
Introduction to the special section: convergence of
automation technology, biomedical engineering, and
health informatics toward the healthcare 4.0. IEEE
Reviews in Biomedical Engineering, 11:249–259.
Pardeshi, V., Sagar, S., Murmurwar, S., and Hage, P.
(2017). Health monitoring systems using iot and rasp-
berry pi—a review. In 2017 international conference
on innovative mechanisms for industry applications
(ICIMIA), pages 134–137. IEEE.
Poniszewska-Maranda, A. and Kaczmarek, D. (2015). Se-
lected methods of artificial intelligence for internet of
things conception. In 2015 Federated Conference on
Computer Science and Information Systems (FedC-
SIS), pages 1343–1348. IEEE.
Qadir, Q. M., Rashid, T. A., Al-Salihi, N. K., Ismael, B.,
Kist, A. A., and Zhang, Z. (2018). Low power wide
area networks: a survey of enabling technologies, ap-
plications and interoperability needs. IEEE Access,
6:77454–77473.
Raveendran, A. and Jayadevan, R. (2020). Reverse quaran-
tine and covid-19. Diabetes & Metabolic Syndrome:
Clinical Research & Reviews, 14(5):1323–1325.
Richardson, P., Griffin, I., Tucker, C., Smith, D., Oechsle,
O., Phelan, A., and Stebbing, J. (2020). Baricitinib
as potential treatment for 2019-ncov acute respiratory
disease. Lancet (London, England), 395(10223):e30.
Rodrigues, J. J., Segundo, D. B. D. R., Junqueira, H. A.,
Sabino, M. H., Prince, R. M., Al-Muhtadi, J., and
De Albuquerque, V. H. C. (2018). Enabling tech-
nologies for the internet of health things. Ieee Access,
6:13129–13141.
Serrano, M., Dang, H. N., and Nguyen, H. M. Q. (2018).
Recent advances on artificial intelligence and internet
of things convergence for human-centric applications:
internet of things science. In Proceedings of the 8th
International Conference on the Internet of Things,
pages 1–5.
Singh, R. P., Javaid, M., Haleem, A., and Suman, R. (2020).
Internet of things (iot) applications to fight against
covid-19 pandemic. Diabetes & Metabolic Syndrome:
Clinical Research & Reviews.
Tang, Y.-W., Schmitz, J. E., Persing, D. H., and Stratton,
C. W. (2020). Laboratory diagnosis of covid-19: cur-
rent issues and challenges. Journal of clinical micro-
biology, 58(6).
Tanne, J. H. (2020). Covid-19: Fda panel votes to approve
pfizer biontech vaccine.
Tarouco, L. M. R., Bertholdo, L. M., Granville, L. Z., Ar-
biza, L. M. R., Carbone, F., Marotta, M., and De San-
tanna, J. J. C. (2012). Internet of things in healthcare:
Interoperatibility and security issues. In 2012 IEEE
international conference on communications (ICC),
pages 6121–6125. IEEE.
Thayyil, J., Kuniyil, V., and Cherumanalil, J. M. (2020).
Covid-19: digital contact tracing technologies and
ethical challenges. International Journal of Commu-
nity Medicine and Public Health, 7(7):2854.
Thilakarathne, N. N., Kagita, M. K., Gadekallu, T. R., and
Maddikunta, P. K. R. (2020). The adoption of ict pow-
ered healthcare technologies towards managing global
pandemics. arXiv preprint arXiv:2009.05716.
Williams, P. A. and McCauley, V. (2016). Always con-
nected: The security challenges of the healthcare in-
ternet of things. In 2016 IEEE 3rd World Forum on
Internet of Things (WF-IoT), pages 30–35. IEEE.
Zhang, Y., Qiu, M., Tsai, C.-W., Hassan, M. M., and
Alamri, A. (2015). Health-cps: Healthcare cyber-
physical system assisted by cloud and big data. IEEE
Systems Journal, 11(1):88–95.
Zhu, X. (2019). Case vi: Children’s hospital of shanghai: A
pioneer in smart healthcare. In Emerging Champions
in the Digital Economy, pages 195–210. Springer.
IoTBDS 2021 - 6th International Conference on Internet of Things, Big Data and Security
236
