
Acceptance of Telemedical Consultations in Nursing Homes: First
Insights & Outlook
Julia Offermann-van Heek
1a
, Anne Kathrin Schaar
1b
, Jörg Christian Brokmann
2c
and
Martina Ziefle
1d
1
Human-Computer Interaction Center, RWTH Aachen University, Campus-Boulevard 57, 52074 Aachen, Germany
2
Emergency Department, University Hospital RWTH Aachen, Pauwelsstraße 30, 52074 Aachen, Germany
Keywords: Telemedicine, Telemedical Consultations, Acceptance, Nursing Homes, Geriatric Patients.
Abstract: Rising numbers of older people and people in need of care pose tremendous challenges for care institutions.
Due to a lack of medical personnel, residents of nursing homes (geriatric patients) are frequently hospitalized
although it is not medically necessary and causes a deterioration of health in many cases. Telemedical
consultations in nursing homes represent one approach to relief and support care personnel in emergency and
medically uncertain situations aiming at a reduction of unnecessary hospitalizations of geriatric patients. For
a successful implementation of these consultations and related innovative processes, the patients’ and as well
as other stakeholders’ (caregivers, doctors, relatives) perspectives and acceptance are important. Thus, a
systematic investigation and adjustment of the requirements is of immense importance. This paper introduces
the Optimal@NRW approach for a cross-sectoral care structure that aims at an avoidance of unnecessary
hospital admissions by implementing telemedical infrastructure in nursing homes. A first scenario-based
acceptance evaluation of telemedical consultations provides insights into the people’s attitudes and allows to
outline an acceptance research agenda as well as next steps within the project.
1 INTRODUCTION
In Europe and worldwide, national health systems are
under pressure. Even before Covid-19 many countries
were confronted with shortages of medical personnel
and limited financial resources as well as an
increasing number of old people entering the care
system as a result of demographic change (Schmidt et
al., 2013; Abbing et al., 2016). The increasing number
of people with need for professional care burdens the
health system and calls for new innovative solutions.
One critical aspect that is of particular importance
refers to acute medical emergency situations of
people in nursing homes. These situations often cause
hospitalization as a result of a rescue service,
especially during the weekend and outside the
consulting hours of physicians (Ouslander &
Berenson, 2011). In this context, it is important to
point out that hospitalization of older people supports
a
https://orcid.org/0000-0003-1870-2775
b
https://orcid.org/0000-0002-8643-6213
c
https://orcid.org/0000-0002-1745-6130
d
https://orcid.org/0000-0002-6105-4729
an increase of a delirium or secondary diseases
(Marcantonio, 2017). This fact has a double negative
impact: On the one hand, unnecessary hospital stays
are an immense financial burden for the health
system. On the other hand, immobilization and a high
mortality rate come along with the necessity to
discuss social implications and questions about a
dignified end of life. In sum, the necessity for
innovative approaches including all relevant
stakeholders to foster resilient, sustainable, and
accepted approaches is without controversy. Digital
measure such as telemedicine could offer relief.
However, a success of telemedicine is no self-starter
at all. How telemedicine can be implemented in
nursing homes, how old structures can be
reorganized, and how acceptance of all stakeholders
involved can be fostered need special attention,
research, and implementation work.
This paper steams from the research project
“Optimal@NRW” that proposes an approach for a
36
Offermann-van Heek, J., Schaar, A., Brokmann, J. and Ziefle, M.
Acceptance of Telemedical Consultations in Nursing Homes: First Insights Outlook.
DOI: 10.5220/0010444000360045
In Proceedings of the 7th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2021), pages 36-45
ISBN: 978-989-758-506-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

systematic implementation of a telemedical
infrastructure in German nursing homes that is
accompanied by a fundamental reorganization of
intersectoral emergency care.
The focus of this paper is put on the acceptance of
telemedical consultations in nursing homes with
special attention to nursing home residents and their
relatives. In this respect, the paper is structured as
follows: Section 1 starts with a short state of the art of
telemedical applications (section 1.1) in general and
leads over to a presentation of technology acceptance
research (section 1.2) with focus on health-related
technologies and telemedical applications (section
1.3). Following that, section 2 presents the research
project and its aim to illustrate the research context of
the presented study. Afterwards, section 3 presents
first insights from a scenario-based questionnaire
study with focus on future users’ and their relatives’
attitude towards telemedical consultations in nursing
homes. Section 4 contains the discussion and presents
a roadmap for future research on the acceptance of
telemedical consultations in nursing homes. The
paper closes with a short conclusion (see section 5).
1.1 Telemedicine and eHealth
Digital measures offer possible solutions to address
the main challenges in the healthcare sector, such as
shortages of medical personnel and lack of financial
resources. The ubiquitous presence of the Internet in
combination with modern sensor technology, for
example, open up innovative monitoring concepts for
the private space or nursing facilities. Since 2005
eHealth is a central element within the work of the
World Health Organization (WHO) (Al-Shorbaji,
2013). From that moment on, there was a clear
endorsement to the value of information and
communication technologies (ICT) for health and
their socioeconomic benefits in healthcare.
Moreover, since that time there has been immense
progress and innovation in the field of eHealth (and
thus also telemedicine). For the professional medical
sector, we can see two different levels of telemedical
advantages: One the one hand, within the field of
doctor-patient communication and, on the other hand,
in the context of communication between medical
professionals, e.g., in the field of tele-intensive care
(Amkreutz, et al. 2020) or tele-emergency care
(Felzen et al., 2019; Czaplik, et al 2014).
Telemedicine and eHealth concepts are currently
being developed and tested in numerous national and
international research projects. National and
international research funding systematically
supports the development and research of eHealth and
networked. A few of them are mentioned here to
illustrate the broad range of approaches and research
activities: The PAAL project, an EU project, for
example aims at a development of different video-
sensor-, and speech-based systems supporting older
and frail people in their everyday life (Flórez-
Revuelta et al., 2018). Other projects, such as the
BMBF project AIDA, focus on the medical care of
residents in nursing homes. In this context, the aim is
to use telemedicine to ensure adequate care for
elderly people in nursing homes, despite the
increasing lack of resources. At the same time, it is to
be examined whether telemedical measures are
suitable for reducing unnecessary hospital admissions
(Ohligs et al 2020). However, even though research
projects such as the ones described here are promising
it is still difficult to make the move from the project
phase into the standard care of the national health
insurance funds. In addition to these financial aspects,
the acceptance of the involved stakeholders (nurses,
patients, physicians) is an important aspect, which,
just like ethical and legal aspects, is necessary for the
successful and sustainable introduction of concepts
(see section 1.3).
1.2 Technology Acceptance
Due to the fundamental digitalization technology
acceptance and use is a crucial topic in these days.
Since the 1980ies technology acceptance is part the
research agenda in different disciplines (e.g., business
economics, psychology, social sciences).
With focus on different acceptance subjects,
objects and contexts technology acceptance research
is focused on the willingness to use technology as
well as using conditions and human factors as a
potential influencing factor on acceptance. The most
successful acceptance models like TAM (Davis,
1989) and UTAUT (Venkatesh et al., 2003) steam
from the late 1980ies and are focused on the adoption
ICT in the working context. In the context of these
models, factors like the perceived ease of use or
perceived usefulness were identified to be good
predictors for the behavioral intention to use a special
technology. Up to today these models emboss
acceptance research and were transferred to other
technical domains (e.g., medical technology, or
energy) and innovative approaches from the field of
ICT. Acceptance research is often challenged to
research the status quo at the beginning of these
phases, when no interaction with technical artefacts
has yet happened and only theoretical deliberations
were made. In these cases, adequate methodological
approaches are needed to gain resilient information.
Scenario-based approaches (see section 3) are one
suitable measure. Derived from the computer
sciences, which uses scenario-based methods to
integrate the perspective of future users into the
Acceptance of Telemedical Consultations in Nursing Homes: First Insights Outlook
37

software design process, scenario-based surveys are
today also used in other fields of research, such as
technology acceptance research. The next section
focuses on the acceptance of (tele)medical
applications as one sensitive area in acceptance
research.
1.3 Acceptance of eHealth and
Telemedical Technologies
Within the field of technology acceptance research
medical or health-related technology (such as
telemedical technologies) are playing a special role.
The sensitive circumstances of their application
require a review of existing models and acceptance
factors. Most studies on the acceptance of
telemedicine or other eHealth applications focus on
the acceptance of medical professionals. In this
context, it could be revealed that the classical
technology acceptance models like TAM and
UTAUT (see section 1.2) also have a prediction for
the medical use context (Holden & Karsh, 2010).
Nevertheless, there is a lack of adequate
standardization of acceptance factors and testing of
their robustness. According to Holden and Kars
(2010), it must be assumed that factors such as social
influence have other reference points (e.g., patients or
relatives) than in the area of ICT in the work context.
From several research projects and studies, we know
different factors that have been proven to be relevant
for the acceptance of medical technologies (human
factors, system related factors, and context factors):
Human factors: Age (e.g., Ziefle & Wilkowska,
2010), gender, expertise with (medical) technologies
(Ziefle & Wilkowska, 2010), perceived locus of
control over technology (Burde & Blankerts, 2002),
but also health status (Calero Valdez & Ziefle, 2015)
and care experience (Offermann-van Heek & Ziefle,
2018) were revealed to be relevant factors in the field
of human factors.
System related factors: As relevant system
factors, the perceived ease of use and usefulness (e.g.,
Brauner, 2016) as well as perceived costs as classical
technology acceptance factors are of importance. In
addition to that, perceived system security as well as
privacy and data security (Wilkowska, 2015) were
revealed be play an important role in the context of
the acceptance of medical technologies. In the case of
telemedical technologies, teleconsultation
presentations types (e.g., display size) can also have
an important influence on the evaluation by patients
(Beul et al., 2011). When examining such
technologies, it is therefore of particular importance
to make mutually influencing aspects measurable in a
differentiated manner in order to examine which
factors are ultimately decisive for acceptance.
Context factors: The relevant contextual factors
arise directly from the framework conditions of
technology use. In the case of medical technology or
telemedicine, this can be the living environment, the
clinical context, or further social conditions, for
example acceptance or rejection of family or doctors
(e.g., Brauner, 2016).
2 RESEARCH AIM & PROJECT
As described above, a specific challenge of
demographic change is the provision of adequate
geriatric care in nursing homes or home environments
of geriatric patients. Telemedicine is a promising
approach to tackle the existing challenges, but so far
there are no solutions that have been rolled out on a
large scale. A widespread use would require the
implementation and standardization of technical
means, the proof of medical evidence, cost coverage
by the health insurance companies as well as the
acceptance of the involved stakeholders. This is
precisely where the Innovation Fund project
Optimal@NRW comes in. The Optimal@NRW
project represents a new intersectoral approach to
provide acute care and support for geriatric persons in
need of care by means of an implementation of an
early warning system and the integration of
telemedical consultation systems in 25 nursing homes
and outpatient care within the region of Aachen in
Germany. To realize this goal the project is focused
on restructuring the emergency care infrastructure for
nursing homes as well as improving the collaboration
between the involved stakeholders (emergency
service, emergency department, general practitioners,
care personnel, etc.). According to this goal, a central
emergency number provided by the Association of
Statutory Health Insurance should act as a virtual hub
for the care of geriatric patients. The concrete
approach of the project involves that the participating
nursing homes first contact the doctor's call center
(116 117) when a medical problem arises. Then, the
call center is responsible for an initial medical
assessment and decides whether the respective
general practitioner can be involved or if a
teleconsultation with the “virtual digital desk” (which
means the medical experts from the emergency
department at the University Hospital RWTH
Aachen) should be conducted. In addition, mobile
care assistants are introduced within the project, who
can also support the care personnel and provide
services that can be delegated by doctors – especially
ICT4AWE 2021 - 7th International Conference on Information and Communication Technologies for Ageing Well and e-Health
38

if the general practitioner is not available at that time.
Applying these processes, the central project goals
refer to the avoidance of inadequate hospital
admissions in outpatient-sensitive hospital cases and
improved medical care at the nursing homes and in
outpatient care.
During the project, an evaluation of the efficacy
of the implemented structure and processes will be
carried out in a cluster-randomized study. Besides
this health economic evaluation and concrete medical
questions, one central focus of the project relates to
user-related acceptance, perceptions, requirements,
and wishes. Thereby, all relevant stakeholders (i.e.,
residents of nursing homes, relatives of residents, care
personnel, general practitioners, emergency
department, emergency services etc.) have to be
considered in order to identify and evaluate the user
requirements and acceptance with regard to the usage
of telemedical consultations in nursing homes
holistically. The study (see section 3) in this paper
represents the first (scenario-based) step of the user-
related acceptance evaluation.
3 FIRST STUDY INSIGHTS
Within this paper, we like to present first insights
from the previously described project. For this
purpose, the applied online survey, the acquired
sample as well as exemplary results are presented in
the following.
3.1 Online Survey
In the initial phase of the project – in which the
technology is still being configured, requirements
must be identified, and processes coordinated, a first
scenario-based study was conducted to initially
evaluate the use of telemedical technology in nursing
homes from the perspective of younger and older
adults being predominantly not affected by care
themselves. For this purpose, an online survey was
conceptualized focusing on two different self-
developed scenarios: the participants were asked to
put themselves in situations that 1) the telemedical
consultations are used for a family member who lives
in a nursing home, and 2) that they will live
themselves in a nursing home in a few years and the
telemedical technology is used for them.
In the first part of the online survey, the
participants indicated demographic information (i.e.,
age, gender, educational level, living situation).
Afterwards, the participants stated if they suffer from
a chronic disease and if they are in need of support
and care. In addition, the participants were also asked
if they had previous professional or private
experience in care (each as yes/no answer options).
Subsequently, the participants were informed in
detail about the projects’ idea, concept, and
functionality of integrating telemedical consultations
in nursing homes. Thereby, an exemplary situation
was described. In this context, it was explained in
which way telemedical technology can be used and
be beneficial for both, residents and personnel in
nursing homes, by preventing unnecessary hospital
admissions and the associated, frequently occurring
deterioration in the health status of geriatric patients
(e.g., delirium).
Following this explanation, the participants were
asked to empathize with the first scenario – imaging
that telemedical consultations are integrated in a
nursing home a family member is living in. Thus, the
participants should evaluate the usage of telemedical
consultations from a perspective of a relative of a
nursing home resident. Overall, 13 items were used
for the evaluation of the telemedical consultations
(see Figure 1). In more detail, the general attitude
towards the technology (3 items), the behavioral
intention to use the technology (3 items), and the
perception of potential advantages (4 items) as well
as potential barriers (3 items) of using telemedical
consultations in nursing homes were assessed.
In a second step, the participants were asked to
imagine that some years have passed and they
themselves live in a nursing home. Hence, they
should therefore evaluate the use of telemedical
consultations for themselves. Here, the participants
evaluated the same statements again from their “own”
perspective (being a resident in a nursing home).
Aiming for a comparison of both scenarios, all
participants evaluated both scenarios, while
participants who evaluated only one scenario and
filled out the onine survey incompletely were
excluded from statistical analyses.
At the end of the online survey, the participants
were asked to evaluate (yes/no answer options) two
final statements (“Telemedicine enriches care in
nursing homes” and “Telemedicine replaces human
attention in nursing homes”) from both introduced
perspectives (i.e., relative vs. resident),
3.2 Participants
Overall, N = 118 participants filled out the online
survey in November and December 2020 in
Germany. The mean age of the participants was 36.58
years (SD = 15.12; min = 21; max = 79) and the
sample consisted of a higher proportion of female
Acceptance of Telemedical Consultations in Nursing Homes: First Insights Outlook
39

(70.3%, n = 83) compared to male participants
(29.7%; n = 35). Overall, the sample’s educational
level was comparably high as the majority (60.2%, n
= 71) indicated to hold a university degree, 22.9% (n
= 27) a university entrance certificate, and 8.5% (n =
10) a PhD. In contrast, only 8.5% (n = 10) of the
participants indicated lower education levels, i.e.
diverse secondary school certificates.
Asked about their current living situation, the
majorities of the participants reported to live together
with another person (49.2%, n = 53) or together with
several people (32.2%, n = 38), while only a small
proportion (18.6%, n = 22) lived alone.
Referring to health-related characteristics, the
participants assessed their health status as very good
(26.3%, n = 31), good (47.5%, n = 56), and rather
good (22.3%, n = 24), while only (5.9%, n = 7)
indicated lower assessments. In addition, 25.4% (n =
30) of the participants reported to suffer from a
chronic disease (e.g., hypertension), and only 1.7% (n
= 2) indicated to be in need of care.
As last person-related characteristics, the
participants were asked for their previous experience
in care. Thereby, 15.3% (n = 18) reported to be
professionally experienced in care, whereas 27.1% of
the participants indicated private passive experience
in the sense that a person in their close environment
is in need of care. Beyond that, 21.2% (n = 25) of the
participants reported to have active experience in
care, as they have already been the caregiver for a
person needing care in their close environment.
3.3 Results
In a first step and apart from descriptive statistics,
repeated measure ANOVAs were calculated in order
to investigate the influence of the different
perspectives (a relative of a resident in a nursing
home vs. a resident in a nursing home) – on the
evaluations of telemedical consultations in nursing
homes. In a second step, (multivariate) analyses of
variance were applied to examine whether the
evaluations were influenced by individual
characteristics of the sample. Finally, it was
investigated to what extent the evaluations of
telemedical consultations relate with each other. For
this purpose, bivariate correlation analyses were
calculated. In the following, means (M) and standard
deviations (SD) are reported for descriptive analyses.
For the omnibus significance of analyses of variance,
the F-Tests were taken from the Pillai values,
Pearson’s coefficient are reported for correlations,
and the level of statistical significance (p) was set at
a conventional level of 5% (* = p < .05; ** = p < .01).
3.3.1 Two Perspectives on the Evaluation of
Telemedical Consultations in Nursing
Homes?
The results regarding the evaluations of telemedical
consultations in nursing home differing both
described perspectives are presented in Figure 1.
Thereby, means above the mean of the scale (3.5)
indicate the agreement, while means below 3.5
rejection of an item.
Starting with the overall acceptance, telemedical
consultations in nursing homes were evaluated to be
equally useful (n.s.), and the usage of innovative
technologies in nursing homes was desired
independent from both investigated perspectives
(n.s.). Compared to that, the item “I find the system
meaningful” was confirmed significantly more from
the perspective of a relative (M = 4.74, SD = 0.92)
compared to the perspective of a resident (M = 4.54,
SD = 1.05; F(1,115)=6.211, p < .05).
Beyond the general acceptance, the participants
also evaluated a more concrete facet of acceptance in
terms of an intention to use telemedical consultations
in nursing homes. Thereby, both perspectives equally
rejected to “do not want to use the system” (n.s.) and
agreed with the statement that they “can imagine
using the system in the future” (n.s.). Instead, the
most concrete statement “I would like to use it” was
evaluated more affirmative from the perspective of a
relative (M = 4.46, SD = 1.06) compared to the
perspective of a resident (M = 4.23, SD = 1.20;
F(1,116)=4.993, p < .05).
Among potential barriers of using telemedical
consultations, the item “I would prefer personal
contact” was confirmed most from both perspectives
(n.s.) and, thus, revealed the most relevant aspect.
Further, both perspectives (n.s.) confirmed to “would
not have any concerns that data is transmitted
securely”. As a last barrier, both perspectives (n.s.)
showed rejections with regard to the statement “I feel
that the technology is not mature”.
Moving to perceived benefits and motives to use
telemedical consultations, the results show the
descriptive tendency that all four items were
evaluated more affirmatively from the resident’s than
from the relative’s perspective. In particular, the item
“[My relative / I] would feel safe” was even evaluated
significantly more positive from the perspective of a
resident (M = 4.26, SD = 0.90) compared to the
perspective of a relative (M = 3.99, SD = 0.98;
F(1,114)=6.972, p < .01).
In addition to the evaluations, the participants
assessed two final statements also from both
perspectives. In accordance with the non-varying
evaluations of the barriers, the statement
ICT4AWE 2021 - 7th International Conference on Information and Communication Technologies for Ageing Well and e-Health
40
Figure 1: Evaluation of telemedical consultations in nursing homes from two different perspectives.
“Telemedicine replaces human attention in
nursing homes” was evaluated almost the same
(F(1,115)=.498; n.s.) from both perspectives –
relative: yes 12.8% (n = 15), no 87.2% (n = 102);
resident: yes 13.0% (n = 12), no 87.0% (n = 104). In
line with the tendency of a higher evaluations from
the relative perspective (e.g., meaningfulness), the
statement “Telemedicine enriches care in nursing
homes” was also evaluated more confirmatively
(F(1,114)=7.799; p < .01) from the relative’s (yes
94.8% (n = 109), no 5.2% (n = 6)) compared to the
resident’s perspective (yes 86.2% (n = 100), no
13.8% (n = 16)).
3.3.2 Influence of Individual Factors on the
Evaluation of Telemedical
Consultations
For both scenario perspectives, MANOVA analyses
did not reveal significant omnibus effects for the
included demographic characteristics, i.e., age,
gender, and educational level. Further, also the living
situation and health-related characteristics of the
participants did not influence the evaluations of
telemedical consultations in nursing homes in
general. The same appeared for both facets of private
experience in care.
In contrast, professional experience in care
influenced the evaluations of telemedical
consultations in nursing homes significantly within
the relative’s scenario perspective (F(13,98)=2.218;
p<.05): in particular, professionally experienced
participants (M = 4.41, SD = 1.18) showed higher
agreements to the statement “My relative would feel
safe” (F(1,111)=4.114; p < .05) compared to
inexperienced participants (M = 3.89, SD = 0.93).
Further, they (M = 3.71, SD = 1.61) showed lower
confirmations of the statement “I would prefer
personal contact for my relative” (F(1,111)=4.228)
compared to inexperienced participants (M = 4.33,
SD = 1.05). Interestingly, these effects were not
apparent for the own perspective of a resident in a
nursing home.
3.3.3 Relevant Relationships
In order to analyze die extent of relationships within
the evaluations of telemedical consultations,
correlation analyses were conducted. Therefore,
overall scores for the participants’ general
acceptance, their intention to use telemedical
consultations as well as their evaluations of perceived
benefits and barriers were created for the relative’s
and the resident’s perspectives. The results are
presented in Figure 2.
Acceptance of Telemedical Consultations in Nursing Homes: First Insights Outlook
41
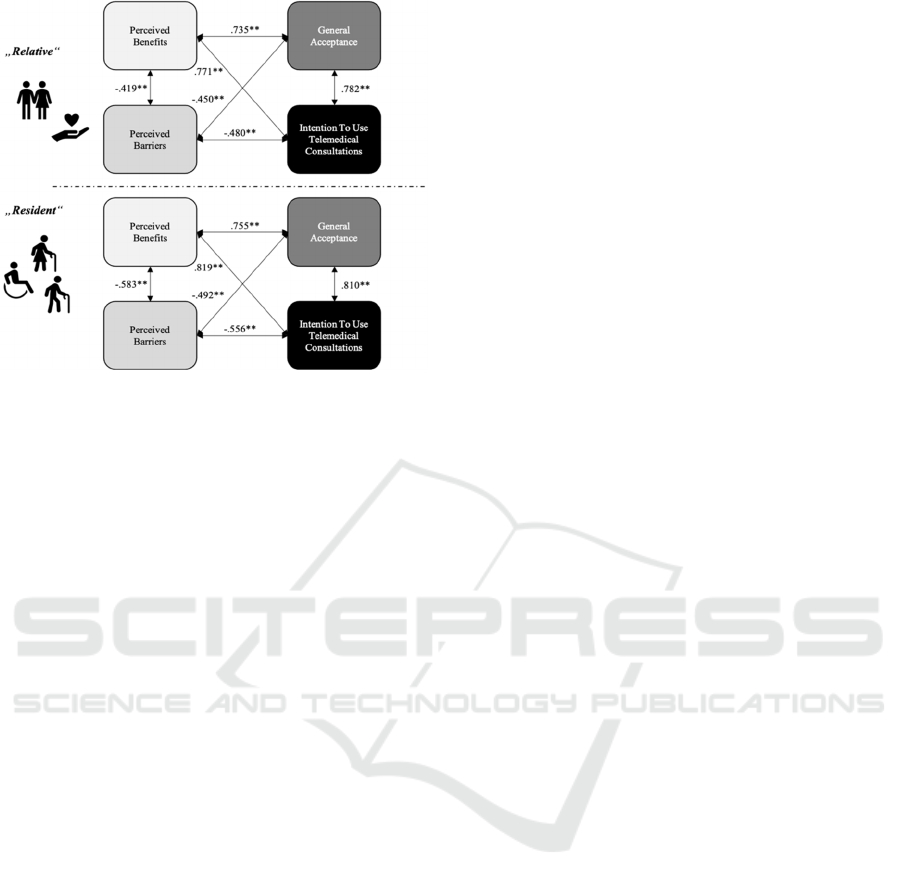
Figure 2: Relationships regarding the evaluation of
telemedical consultations from two perspectives.
Starting with the relative’s perspective on using
telemedical consultations in nursing homes, strong
relationships showed up between the participant’s
general acceptance and intention to use (r = .782; p <
.01). Further, also the perceived benefits correlated
strongly with the general acceptance (r = .735; p <
.01) and the intention to use telemedical consultations
(r = .771; p < .01).
Considering the perceived barriers, comparably
lower, moderate (negative) relationships appeared
with regard to perceived benefits (r = -.419; p < .01),
general acceptance (r = -.450; p < .01), and the
intention to use (r = -.490; p < .01).
Moving to the resident’s perspective, even
stronger relationships were apparent. General
acceptance and the intention to use correlated
strongly (r = .810; p < .01) and also the perceived
benefits showed strong relationships with general
acceptance (r = .755; p < .01) and the intention to use
telemedical consultations in nursing homes (r = .819;
p < .01). However, the differences are most noticeable
in terms of perceived barriers: in comparison, the
perceived barriers correlated (more) strongly
negatively with the perceived benefits (r = -.583 p <
.01), general acceptance (r = -.492 p < .01), and the
participants’ intention to use (r = -.556 p < .01).
4 DISCUSSION
Overall, this paper aimed at an introduction of a
current research project focusing on the integration of
telemedicine in nursing homes in order to relief
caregivers, and to reduce the probability of
inadequate hospital admissions. Focusing on the
communication science perspective the results of a
first scenario-based study were presented. In the
following, the findings of this study are discussed,
allowing to outline a research roadmap which
indicates relevant further steps within the project for
the technology acceptance part.
4.1 Key Insights & Limitations of a
First Study
Inquiry of the Involved Stakeholders: In general,
the study revealed rather similar evaluations with
regard to using telemedicine in nursing homes from
both perspectives – the perspective of a relative of a
nursing home resident and being the nursing home
resident him- or herself. These similar evaluations
could be caused by the scenario-based approach. In
this regard, the gap between (reported) attitudes and
the actual behavior of people is well known (Ajzen &
Fishbein, 1980). Therefore, affected stakeholders
(i.e., in particular nursing home residents, their
relatives and caregivers) should be directly addressed
in future studies.
Considering Diverse Stakeholders: Despite the
overall rather similar evaluations, single significant
differences with regard to the different perspectives
were apparent: on the one hand, perceived
meaningfulness and a concrete intention to use
telemedicine in nursing homes were higher from a
relative’s perspective than from a nursing home
resident’s perspective; on the other hand, the
perceived benefit in terms of higher felt safety was
more acknowledged from the nursing home resident’s
than the relative’s perspective. These (within a
scenario-based study gained) differences indicate the
importance of considering diverse stakeholders in
future research on the acceptance of integrating
telemedicine in nursing homes. This procedure
addresses different aspects: On the one hand, the
results obtained here are to be tested for their
resilience. On the other hand, other perspectives (e.g.,
those of the nursing staff) and any interactions
between the stakeholders are to be brought into focus.
Contrasting Professional and Non-professional
Stakeholders: With regard to the impact of
individual factors on the evaluations of telemedicine
in nursing homes the study did not reveal any effects
of demographic characteristics, such as age, gender,
or educational level. Here, it should be considered
that the study’s sample was comparably small,
reached rather young participants, contained a higher
proportion of female than male participants, and
reached predominantly participants being less
experienced in care. Changes in the evaluation
patterns can be expected when the opinions of older
ICT4AWE 2021 - 7th International Conference on Information and Communication Technologies for Ageing Well and e-Health
42

participants (e.g., Wilkowska, 2015; Brauner, 2016)
and also care-experienced participants are
investigated. Therefore, future studies should aim at
reaching broader and more balanced samples in order
to integrate all relevant stakeholders equally and
adequately. In line with previous research on the
acceptance of assisting technologies in care (e.g.,
Offermann-van Heek & Ziefle, 2018), effects of
professional experience on the evaluations of using
telemedicine in nursing homes were identified in the
present study. Here, professionally experienced
participants saw a greater advantage in increased
safety by using telemedicine in nursing homes and
showed lower concerns of a loss of personal contact.
These effects were only apparent within the scenario
including the perspective of a relative of a nursing
home resident, which makes sense as this perspective
is close to a professional caregiver’s perspective.
These insights confirm the relevance of integrating all
affected stakeholders within research on the
acceptance of using telemedicine in nursing homes
since perceived (dis)advantages may differ
depending on the respective stakeholders’
perspectives.
Investigating Interrelations between
Acceptance, Requirements, and Perceived
(dis)Advantages: In line with previous research on
the acceptance of assisting technologies in older age
(e.g., Peek et al., 2014, Offermann-van Heek et al.,
2019) the results showed that the acceptance and
intention to use telemedicine in nursing homes are
connected with the perception of potential
technology-related advantages and disadvantages.
Beyond that, the relationships were even stronger for
the perspective of a nursing home resident compared
to the perspective of a relative of a nursing home
resident. Hence, future research should also
investigate the interrelations between acceptance,
requirements, and perceived (dis)advantages
depending on the perspective of all affected
stakeholders.
Holistic Evaluation of User Requirements:
Another aspect refers to the fact that only few aspects
were part of this first study, and, therefore, this study
has certainly not included all relevant aspects
holistically. As mentioned above, future studies
should address all relevant stakeholders in order to
identify relevant requirements as well as perceived
(dis)advantages of using telemedicine in nursing
homes. Only this way, it can be ensured that all
“user”-relevant requirements and wishes are
considered within the adaption and integration of
telemedicine in nursing homes.
4.2 Investigating Acceptance of
Telemedicine in Nursing Homes in
the Future
Based on the identified insights of a first scenario-
based study focused on potential users’ attitude
towards telemedicine in nursing homes within the
Optimal@NRW project, concrete strategies for
further steps of the user-centered investigations can
be derived:
From the user-centered communication science
perspective, a major focus must be put on
acceptance research and respective assessments of
“real” interactions with telemedical systems in
addition to a usage of scenario-based analyses.
Analyzing direct interactions within telemedical
consultations enables to identify appearing problems,
(initial) reactions, and relevant process flows between
the different involved stakeholders (i.e., care
personnel, doctors, emergency services, patients) and
also in the field of human-technology interaction. In
addition, scenario-based approaches support the
understanding and identify existing opinions and
mental models regarding care in nursing homes,
process flows, or general attitudes before
telemedicine is integrated in the involved nursing
homes.
A further major, user-centered task refers to the
integration of all relevant stakeholders in all phases
of the project (before telemedicine is implemented,
during the different interaction phases, and at the end
of the project). As the results of the present study
suggest significant differences in the acceptance of
telemedicine depending on different user
perspectives, it is necessary to talk to the "real"
stakeholders and to systematically survey the real
perspectives within all steps of the project. This way,
all relevant user requirements can be identified and
validated for the diverse stakeholders.
To realize acceptance research within the project
successfully, a combination of qualitative and
quantitative methodological approaches is
necessary. Thereby, interviews will be conducted in
particular at the beginning of the project to identify
the status quo regarding relevant process flows,
communication requirements as well as wishes,
attitudes, and needs of all involved stakeholders. Only
on the basis of these qualitative studies and analyses
a holistic quantification of the results using (online)
surveys is usefully realizable considering the
different stakeholders and their specific
characteristics.
Finally, the mix of summative and comparative
acceptance analyses enables to identify changing
Acceptance of Telemedical Consultations in Nursing Homes: First Insights Outlook
43

acceptance parameters over time as well as to
determine influencing characteristics of the
stakeholders (e.g., age, gender, experience), which
may also vary over the different project phases.
5 CONCLUSIONS
This paper presented a first scenario-based
acceptance study with focus on future users’ attitude
towards the use of telemedicine in nursing homes. on
the attitude of potential users Focusing on a user-
centered and technology acceptance related
perspective is one focus addressed within research
project “Optimal@NRW”. Overall, the project aims
at a sustainable implementation of telemedicine in
nursing homes and outpatient care in order to avoid
inadequate hospital admissions of geriatric patients.
The results of this particular presented study highlight
the importance of integrating all involved
stakeholders into all further project phases in order to
do justice to user-specific requirements. Beyond that,
the study’s insights enable to outline research tasks
within a research roadmap, that will be pursued in the
acceptance research part of the project.
ACKNOWLEDGEMENTS
The authors thank all participants for their openness
to share opinions on telemedical consultations and
processes. Furthermore, the authors want to thank
Vanessa Petring for research assistance. This work
was funded by the German joint federal committee
“Innovationsfond” (grant number: 01NVF19015).
Regarding the acceptance-related issues, this work
based on the project “Privacy Aware and Acceptable
Lifelogging services for older and frail people”
(16SV7955).
REFERENCES
Abbing, H. R., 2016. Health, healthcare and ageing
populations in Europe, a human rights challenge for
European health systems. European Journal of Health
Law, 23(5), 435-452.
Ajzen I, Fishbein M., 1980. Understanding Attitudes and
Predicting Social Behavior, Englewood Cliffs, NJ:
Prentice-Hall.
Al-Shorbaji, N., 2013. The World Health Assembly
resolutions on eHealth: eHealth in support of universal
health coverage. Methods of Information in Medicine,
52(06), 463-466.
Amkreutz, J., Lenssen, R., Marx, G., Deisz, R., & Eisert,
A., 2020. Medication safety in a German telemedicine
centre: Implementation of a telepharmaceutical expert
consultation in addition to existing tele-intensive care
unit services. Journal of Telemedicine and Telecare,
26(1-2), 105-112.
Beul, S., Ziefle, M., & Jakobs, E. M. (2011, May). Users'
preferences for telemedical consultations: Comparing
users' attitude towards different media in technology-
mediated doctor-patient-communication. In 2011 5th
International Conference on Pervasive Computing
Technologies for Healthcare (PervasiveHealth) and
Workshops (pp. 614-620). IEEE.
Brauner, P. M., 2016. Serious Games for Healthcare in
Ambient Assisted Living Environments: A Technology
Acceptance Perspective. Apprimus Verlag.
Burde, W., & Blankertz, B., 2006. Is the locus of control of
reinforcement a predictor of brain-computer interface
performance? TU Berlin. http://doc.ml.tu-
berlin.de/publications/publications/BurBla06.pdf.
Calero-Valdez, A., & Ziefle, M., 2015. Older Users’
Rejection of Mobile Health Apps a Case for a Stand-
Alone Device? In International Conference on Human
Aspects of IT for the Aged Population, pp. 38-49.
Springer, Cham.
Czaplik, M., Bergrath, S., Rossaint, R., Thelen, S.,
Brodziak, T., Valentin, B., Hirsch, F., Beckers, S.K., &
Brokmann, J. C., 2014. Employment of telemedicine in
emergency medicine. Methods of Information in
Medicine, 53(02), 99-107.
Davis, F. D., 1989. Perceived usefulness, perceived ease of
use, and user acceptance of information technology.
MIS Quarterly, 319-340.
Felzen, M., Beckers, S. K., Kork, F., Hirsch, F., Bergrath,
S., Sommer, A., Brokmann, J.C., Czaplik, M., &
Rossaint, R. (2019). Utilization, Safety, and Technical
Performance of a Telemedicine System for Prehospital
Emergency Care: Observational Study. Journal of
Medical Internet Research, 21(10), e14907.
Flórez-Revuelta, F., Mihailidis, A., Ziefle, M., Colonna, L.,
& Spinsante, S. (2018, September). Privacy-Aware and
Acceptable Lifelogging services for older and frail
people: The PAAL project. In 8th International
Conference on Consumer Electronics-Berlin (ICCE-
Berlin) (pp. 1-4). IEEE.
Holden, R. J., & Karsh, B. T., 2010. The technology
acceptance model: its past and its future in health care.
Journal of Biomedical Informatics, 43(1), 159-172.
Marcantonio, E. R., 2017. Delirium in hospitalized older
adults. New England Journal of Medicine, 377(15),
1456-1466.
Offermann-van Heek, J., & Ziefle, M., 2018. They Don’t
Care About Us! Care Personnel’s Perspectives on
Ambient Assisted Living Technology Usage: Scenario-
Based Survey Study. JMIR Rehabilitation and Assistive
Technologies, 5(2), e10424.
Offermann-van Heek, J., Wilkowska, W., Brauner, P., &
Ziefle, M. (2019). Guidelines for Integrating Social and
Ethical User Requirements in Lifelogging Technology
Development. In: 4th International Conference on
ICT4AWE 2021 - 7th International Conference on Information and Communication Technologies for Ageing Well and e-Health
44

Information and Communication Technologies for
Ageing Well and e-Health (ICT4AWE 2018).
SCITEPRESS.
Ohligs, M., Stocklassa, S., Rossaint, R., Czaplik, M., &
Follmann, A., 2020. Employment of Telemedicine in
Nursing Homes: Clinical Requirement Analysis,
System Development and First Test Results. Clinical
Interventions in Aging, 15, 1427.
Ouslander, J. G., & Berenson, R. A., 2011. Reducing
unnecessary hospitalizations of nursing home residents.
New England Journal of Medicine, 365(13), 1165.
Peek, S. T., Wouters, E. J., Van Hoof, J., Luijkx, K. G.,
Boeije, H. R., & Vrijhoef, H. J., 2014. Factors
influencing acceptance of technology for aging in
place: a systematic review. International Journal of
Medical Informatics, 83(4), 235-248.
Schmidt, S., Hendricks, V., Griebenow, R., & Riedel, R.
2013. Demographic change and its impact on the
health-care budget for heart failure inpatients in
Germany during 1995–2025. Herz, 38(8), 862-867.
Venkatesh, V., Morris, M. G., Davis, G. B., & Davis, F. D.,
2003). User acceptance of information technology:
Toward a unified view. MIS Quarterly, 425-478.
Wilkowska, W., 2015. Acceptance of eHealth technology
in home environments: Advanced studies on user
diversity in ambient assisted living. Apprimus Verlag.
Ziefle, M., & Wilkowska, W., 2010. Technology
acceptability for medical assistance. In 2010 4th
International Conference on Pervasive Computing
Technologies for Healthcare (pp. 1-9). IEEE.
Acceptance of Telemedical Consultations in Nursing Homes: First Insights Outlook
45
