
Proposed Use of a Conversational Agent for Patient Empowerment
Marco Alfano
1,4 a
, John Kellett
2b
, Biagio Lenzitti
3c
and Markus Helfert
1d
1
Lero, Maynooth University, Maynooth, Co. Kildare, Ireland
2
Department of Emergency Medicine, Hospital of South West Jutland, Esbjerg, Denmark
3
Dipartimento di Matematica e Informatica, Università di Palermo, Palermo, Italy
4
Anghelos Centro Studi sulla Comunicazione, Palermo, Italy
Keywords: Digital Health, Patient Empowerment, Conversational Agent, Tailored Health Communication, Artificial
Intelligence, Big Data.
Abstract: Empowerment is a process through which people acquire the necessary knowledge and self-awareness to
understand their conditions and treatment options, make informed choices and self-manage their health
conditions in daily life, in collaboration with medical professionals. Conversational Agents in healthcare
could play an important role in the process of empowering a person but, so far, they have been seldom been
used for this purpose. This paper presents the basic principles and preliminary implementation of a
conversational health agent for patient empowerment. It dialogues with the user in a “natural” way, collects
health data from heterogeneous sources and provides the user with specific and relevant information. This
allows a person/patient to create his/her own opinion on health matters in the most complete and objective
way, and, therefore, it facilitates the empowerment process.
1 INTRODUCTION
Technological innovations are accelerating disruption
in consumer health and wellbeing but there is still a
disconnect between current healthcare, focused on
disease management, and the needs of empowered
people whose focus is on comprehension and
management of their health (Snowdon, 2020). An
empowered person/patient 1. has the necessary
knowledge and self-awareness to understand his/her
conditions and treatment options, 2. can make
informed choices (i.e. decide), and 3. can self-
manage his/her health conditions in daily life (i.e.
act), in collaboration with medical professionals
(European Health Parliament, 2017; WHO, 2016;
Alfano et al., 2019a; Alfano et al., 2019b). Few
applications exist for person/patient empowerment
and they often work as silos (Snowdon, 2020).
Artificial Intelligence (AI) in healthcare can play
an important role in the process of empowering a
person (Kondyalkis et al., 2013; Iatraki et al. 2018).
AI, however, often empowers machines rather than
a
https://orcid.org/0000-0001-7200-9547
b
https://orcid.org/0000-0002-4741-9242
c
https://orcid.org/0000-0003-2664-7788
d
https://orcid.org/0000-0001-6546-6408
people (e.g., self-diagnosis apps tend to be substitute
doctors and keep patients as passive recipients,
Davenport and Kalakota, 2019; Jiang et al., 2017; Fast
and Horvitz, 2017). Moreover, AI-driven healthcare
applications are used in separated contexts, use
different data, and work as silos (Herrero et al. 2016).
Finally, the existing virtual assistants are mainly used
for self-diagnosis (decide) and self-
monitoring/management (act). Although they
represent, in principle, the second and third step of the
empowerment process, the first step (understanding)
is unaddressed and, therefore, do not provide genuine
empowerment (Magyar et al., 2019; Herrero et al.,
2016).
How can AI be used to empower people and help
them to better comprehend health information, make
informed decisions and self-manage their health and
wellbeing in collaboration with their healthcare
professionals?
This paper presents the basic principles and
preliminary implementation details of a
conversational health agent for patient empowerment
Alfano, M., Kellett, J., Lenzitti, B. and Helfert, M.
Proposed Use of a Conversational Agent for Patient Empowerment.
DOI: 10.5220/0010414408170824
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 5: HEALTHINF, pages 817-824
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
817

that facilitates the comprehension of health
information so that a person can create his/her own
opinion on health matters in the most complete and
objective way, using the most accurate and
appropriate information available. This is the first of
the three empowerment steps and the precondition for
the other two (i.e., making informed and conscious
health decisions, together with medical professionals,
and actively manage their health and well-being).
The paper is organized as follows. Section 2
illustrates the background and motivation of the
research. Section 3 presents the principles of the
conversational health agent for patient empowerment.
Section 4 presents the details of the initial
implementation of the agent. Sections 5 presents
some conclusions and future work.
2 BACKGROUND AND
MOTIVATION
2.1 Review of the Literature
Conversational agents or chatbots are computer
programs that simulate conversations with users.
These AI systems, also known as relational agents,
inform the user by generating an easily
comprehended dialogue.
We have made a preliminary analysis of the
literature and we found only a limited number of
studies linking person/patient empowerment to
conversational agents: Issom et al. (2020) evaluated
the information provided by a chatbot designed to
help patients with Sickle-Cell Disease to prevent
vaso-occlusive pain. Denecke et al. (2018a; 2018b)
reported an AI-driven self-anamnesis mobile
application in music therapy; a conversational user
interface is chosen to simulate the patient-therapist
conversation but there is no direct empowering action
towards the patient.
We also searched for studies that connect AI or
machine learning with patient empowerment and
conversational agents used in healthcare. Ni et al.
(2020) propose a model that predicts human physical
activity status from sequential lifelogging data
collected from wearable sensors. It can be used as a
decision support tool to provide real-time monitoring,
statistical analysis, and personalized advice. Yadav et
al. (2020) present an AI-driven mobile application
used to predict cases of Anaemia and Thalassemia.
However, this application has been designed for use
by a doctor, nurse, or a health worker, and not by a
patient. The VASelfCare project (Magyar et al 2019)
aimed to develop a conversational agent to facilitate
the self-care of older adults with type 2 diabetes
mellitus (T2D) by improving medication adherence
and lifestyle changes (i.e., physical activity and diet).
The counselling step is tailored through diverse pre-
existing levels of knowledge, by means of a rule-
based decision system. The conversational agent
used reinforcement to learn appropriate behaviour
based on users’ preferences. Herrero et al. (2016)
developed a portable personalised decision support
system to empower individuals on insulin therapy to
self-manage their condition. The blood glucose levels
are collected by the sensors and are managed by a
Case-Based Reasoning (CBR) module to provide
personalised insulin recommendations, while a
second Model-Based Reasoning (MBR) module is
used to maximise users’ safety. You and Gui (2020)
conducted a review and interview study of eleven AI-
enabled chatbot-based symptom checker (CSC) apps.
They found that users perceive the current CSC apps
to lack support for a comprehensive medical history,
flexible symptom input, comprehensible questions,
and diverse diseases and user groups.
Although limited, the review of the current
literature shows:
● Conversational agents are mostly created for a
specific condition.
● Empowerment is almost never addressed directly
and, when it is, only some aspects are considered.
● Comprehension of the health
information/conditions is the least addressed step
of empowerment.
● Little user information is used to provide tailored
content to the user.
● The origin of the provided content is often
unknown and does not use all the information
that is available, for example, on-line (Alfano et
al. 2020b; Alfano et al. 2019c).
● User requirements, such as language level or
information quality (Alfano et al. 2020a; Alfano
et al. 2020b), are not considered.
Therefore, conversational agents currently focus on
specific conditions and mainly deal with self-
diagnosis or self-management of health/conditions.
Almost no agent deals with person empowerment by
considering the user characteristics and requirements,
and then providing him or her with up-to-date and
high-quality customized information.
2.2 Tailored Health Communication
Tailored health communication is the process of
adapting information to the specific characteristics of
an individual (Kamel Ghalibaf et al., 2019). Since it
is more personally relevant, it is more likely to be
read, understood, and acted on (Lustria et al., 2013;
Noar et al., 2011). The process of tailoring health
messages is the same as a tailor uses to make a
Scale-IT-up 2021 - Workshop on Scaling-Up Healthcare with Conversational Agents
818

custom-fit garment according to the customer’s
measurements and their preferred fabric,colour, and
style. Likewise, tailored health communication
considers the user’s needs, interests, and concerns, to
create appropriate “to fit” health information (Bol,
Smit, & Lustria, 2020; Kreuter et al., 2000).
Interpersonal communication has the potential to
be the most customized “tailored” type of
communication, provided all participants understand,
know, and listen to each other. Patients often complain
that discussions with their doctor are unsatisfactory
because they are frequently interrupted and not
listened to (Snyder, 2008; Schouten & Meeuwesen,
2006). Ideally, for any health-related communication
to be empowering it should support an attentive
conversational dialogue with the user to assess his or
her health needs and ensure any information provided
is appropriate and comprehensible (Cheung et al.,
2019); this applies both to traditional inter-personal
and conversational agents.
2.3 Rationale for Tailored Health
Information and Patient
Empowerment
Although provision of tailored health information is
often aimed at a change in behaviour (e.g., smoking
cessation, dietary change, and physical activity),
person empowerment already represents, by itself, a
behavioural change (when it is seen as an outcome
other than a process) because it provides a person
with skills and “power” to make informed decisions,
self-manage health and carry out further lifestyle
changes as needed.
Petty and Cacioppo’s Elaboration Likelihood
Model (Petty and Cacioppo, 1981) provides a
rationale for this approach (Kreuter et al., 1999):
1. by tailoring materials, superfluous
information is eliminated
2. the information that remains is more
personally relevant to the message recipient
3. the message recipient will pay more
attention to information he or she perceives
to be personally relevant
4. information that is attended to is more likely
to have an effect than that which is not
5. when attended to, information that
addresses the unique needs of a person will
be useful in helping him or her decide and
act upon the decision.
In addition, we believe the information provided
to the user must be objective and factual and must not
contain any kind of bias and opinion, unless explicitly
required. In this way, a user will be able to create his
or her own opinion without being influenced (even
indirectly) by biased information.
3 CONVERSATIONAL HEALTH
AGENTS FOR PATIENT
EMPOWERMENT
The requirements of a conversational health agent
that empowers users to understand health
information, make informed decisions, self-manage
their health and wellbeing, and interact better with
healthcare professionals are:
It dialogues with the user in the most “natural”
way.
It collects health data from heterogeneous
sources (health information, health status,
empowerment level, needs, etc.) and can
understand, process, and combine them.
It provides tailored information that is specific
and relevant to patients.
It provides a person/patient with up-to-date
health information that is easy to understand and
directly actionable.
The information provided to the user is objective
and factual and does not contain any kind of bias
and opinion, unless explicitly required.
It explains the principles on how information is
selected in terms that a person/patient can
understand, thus increasing his/her trust and
acceptance.
On the input side, we assume that a user makes a
query (clearly defined or undefined) about complaints
or diseases. The system understands/establishes the
user query and related subqueries in terms of:
Complaints - re. definition, causes, related
diseases, remedies.
Diseases - re. presentation, related complaints,
causes, treatment, prognosis, course of disease/
range of severity.
Moreover, the user provides further information
(either directly or indirectly) that is going to be used
as explicit tailoring criteria for the answer:
Current health status (e.g., symptoms and/or
conditions).
Background health status (e.g., sex, age, gait,
BMI, comorbid illness).
Lifestyle information (e.g., sleep, drugs, meal
composition, alcohol consumption, hormonal
cycles).
Dynamic health indicators (e.g., vital signs
monitoring, physical activity monitoring, stress
level).
Empowerment level (health literacy,
motivation, gaining control).
Proposed Use of a Conversational Agent for Patient Empowerment
819
Health and wellbeing needs (e.g., urgent health
improvement, elective quality of life).
Notice that, beside the explicit tailoring criteria, we
also consider some implicit tailoring criteria such as
the language level, to provide the user with
information he/she can easily understand (Alfano et
al., 2020a; Alfano et al., 2020c; Alfano et al., 2018),
and the information quality, in terms of selection of
authoritative sources and factual (unbiased)
information (Alfano et al., 2020b; Alfano et al.,
2019a).
Possible external sources of health information
are:
Semantic Web (e.g., health-lifesci.schema.org).
UMLS Metathesaurus.
Specialized Websites.
World Wide Web (selected sources).
Other health information repositories.
We also consider internal information that comes
from the user’s previous data and from data related to
other users (appropriately anonymized).
The system provides a primary output in terms of:
Tailored health information on complaints
(Definition, Causes, Related diseases,
Remedies).
Tailored health information on diseases
(Presentation, Treatment, Prognosis, Course of
disease/ Range of severity).
It also provides a secondary output in terms of:
Suggested available options (based on a
threshold mechanism) on talking to a doctor or
going immediately to a hospital (Wasingya-
Kasereka, 2020).
Connection with relevant healthcare services
and professionals.
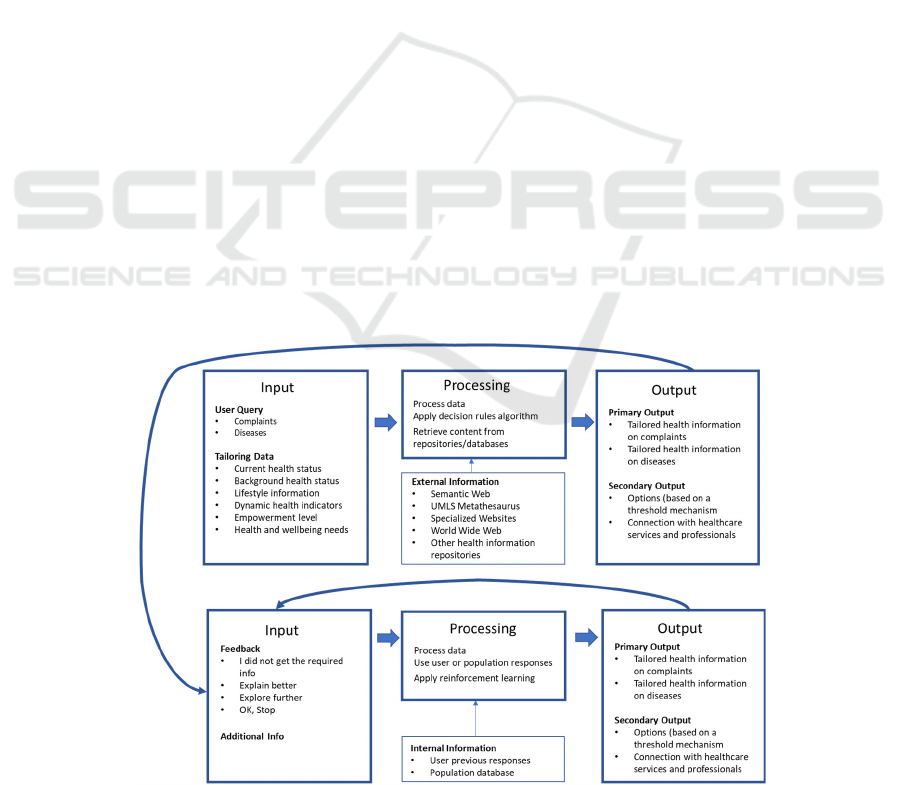
The overall process of the conversational agent is
summarised in Fig. 1 and works as follows:
1. The conversational agent receives the user
input (query and tailoring data) through a
dialogue interface.
2. The conversational agent processes the data,
applies a decision rule algorithm, using the
tailoring data, and retrieves the proper
content from external repositories/databases.
3. The conversational agent
provides the user
with a primary and secondary output.
4. The user provides one of the following
responses to the conversational agent:
o Not OK, I did not get the required
info.
o Partially OK, Explain better.
o OK, Explore further.
o OK, Stop.
For the first three responses, the user can
provide additional information to better
specify his/her further request.
The system will then process the initial and
new data (if present) and the user’s previous
responses (or responses of other users with a
similar profile) and use a reinforcement
learning algorithm to provide the new output.
5. The conversational agent provides the user
with a new primary and secondary output and
goes to step 4.
Figure 1: Summary of the process of the conversational health agent for person/patient empowerment.
Scale-IT-up 2021 - Workshop on Scaling-Up Healthcare with Conversational Agents
820

4 INITIAL IMPLEMENTATION
The implementation of a conversational health agent
for patient empowerment is currently being piloted.
4.1 Complaints and Diseases
There are only a finite number of symptoms and signs
of a disease. For our implementation we have used the
common complaints listed in a classic text
(MacBryde CM, Blacklow RS, 1970):
Pain
Gastro-intestinal complaints
Feverishness
Cough
Breathlessness
Faints or fits
Insomnia
Anxiety
Dizziness
Palpitations
Weakness
Loss of vision
Impaired hearing
Bleeding
The number of diseases considered in our first “proof
of concept” iteration has been confined to:
A. the ten conditions most associated with in-
hospital death (Kellett and Deane, 2007):
o Infection
o Heart failure
o Myocardial infarction
o Chronic obstructive lung disease
o Cancer
o Diabetes
o Kidney disease
o Stroke
o Dementia
B. The commonest diagnoses in primary care
(Finley CR et al, 2018):
o Upper respiratory tract infection
o Asthma
o Otitis media
o Tonsillitis
o Urinary tract infection
o Hypertension
o Arthritis
o
Dyspepsia
o Depression
1
https://schema.org/
2
https://health-lifesci.schema.org/
3
http://webdatacommons.org/
4
http://commoncrawl.org
o Dermatitis
o Tuberculosis
4.2 Creation of Repository of
Schema.org and Health-lifesci
Structured Data
We have started the creation of a repository of health
information by exploiting the semantic information
available in the World Wide Web and, in particular,
that provided by schema.org
1
, an initiative funded by
some major Web players, that aims to create,
maintain, and promote schemas for structured data on
the Internet. For the present work, we consider the
health-lifesci extension
2
that contains 80 types, 162
properties and 125 enumeration values related to the
health/medical field.
We have performed an analysis of the health-
lifesci elements using the data made available by the
Web Data Commons initiative
3
(Meusel, 2014. The
Web Data Commons contain all Microformat,
Microdata and RDFa (Resource Description
Framework in Attributes) data extracted from the
open repository obtained by the Web Common
Crawl
4
. The whole dataset contains about 2.5 billion
pages and almost 1 billion pages contain structured
data. The dataset consists of 44 billion RDF n-quads
5
.
These are sequences of RDF terms in the form {s, p,
o, u}, where {s, p, o} represents a statement about
semantic data consisting of subject, predicate, object,
and {u} represents the Uniform Resource Identifier
(URI) of the document from which the statement has
been extracted.
From the whole dataset, we have extracted the
subset containing health-lifesci.schema.org elements
and the schema.org elements associated with each
URI that contains health-lifesci.schema.org elements.
Since the queries (direct or indirect) from the
users are about complaints and diseases, we have
initially identified the corresponding health-
lifesci.schema.org types (with the corresponding
explanation). For what concerns the complaints, we
have selected the MedicalSignOrSymptom
6
type. For
what concerns the diseases, we have selected the
MedicalCondition
7
type. Moreover, according to the
user query and tailoring data, defined in Section 3, we
have selected the following properties and types
(explanations are taken from health-
lifesci.schema.org):
name, i.e., the name of the item.
5
https://www.w3.org/TR/n-quads/
6
https://schema.org/MedicalSignOrSymptom
7
https://schema.org/MedicalCondition
Proposed Use of a Conversational Agent for Patient Empowerment
821
description, i.e., a description of the sign,
symptom, or condition.
signOrSymptom, i.e., a sign or symptom of the
condition.
MedicalCause, i.e., the causative agent(s) that
are responsible for the pathophysiologic process
that eventually results in a medical sign,
symptom, or condition.
possibleTreatment, i.e., a possible treatment.
drug, i.e., a drug or medicine used in the
treatment.
expectedPrognosis, i.e., the likely outcome in
either the short term or long term of the medical
condition.
stage, i.e., the stage of the condition, if
applicable. It is used in the course of the disease.
epidemiology, i.e., the characteristics of
associated patients, such as age, gender, race, etc.
They are used for tailoring the information.
riskFactor, i.e., a modifiable or non-modifiable
factor that increases the risk of a patient
contracting this condition, e.g., age, coexisting
condition. It is used for tailoring the information.
code, i.e., a medical code for the entity, taken
from a controlled vocabulary or ontology such as
ICD-9, DiseasesDB, MeSH, SNOMED-CT, etc.
It is used for connecting the schema.org data to
other vocabularies such as the ones related to the
Unified Medical Language System (UMLS)
8
.
The health-lifesci.schema.org types and properties
allow us to provide users with complete information
about both complaints and diseases. In terms of
tailoring, the system is presently limited to the current
and background health status. We are in the process
of adding further tailoring data to our repository and
in particular:
Lifestyle information
Dynamic health indicators
Empowerment level
Health and wellbeing needs
4.3 User Interfaces
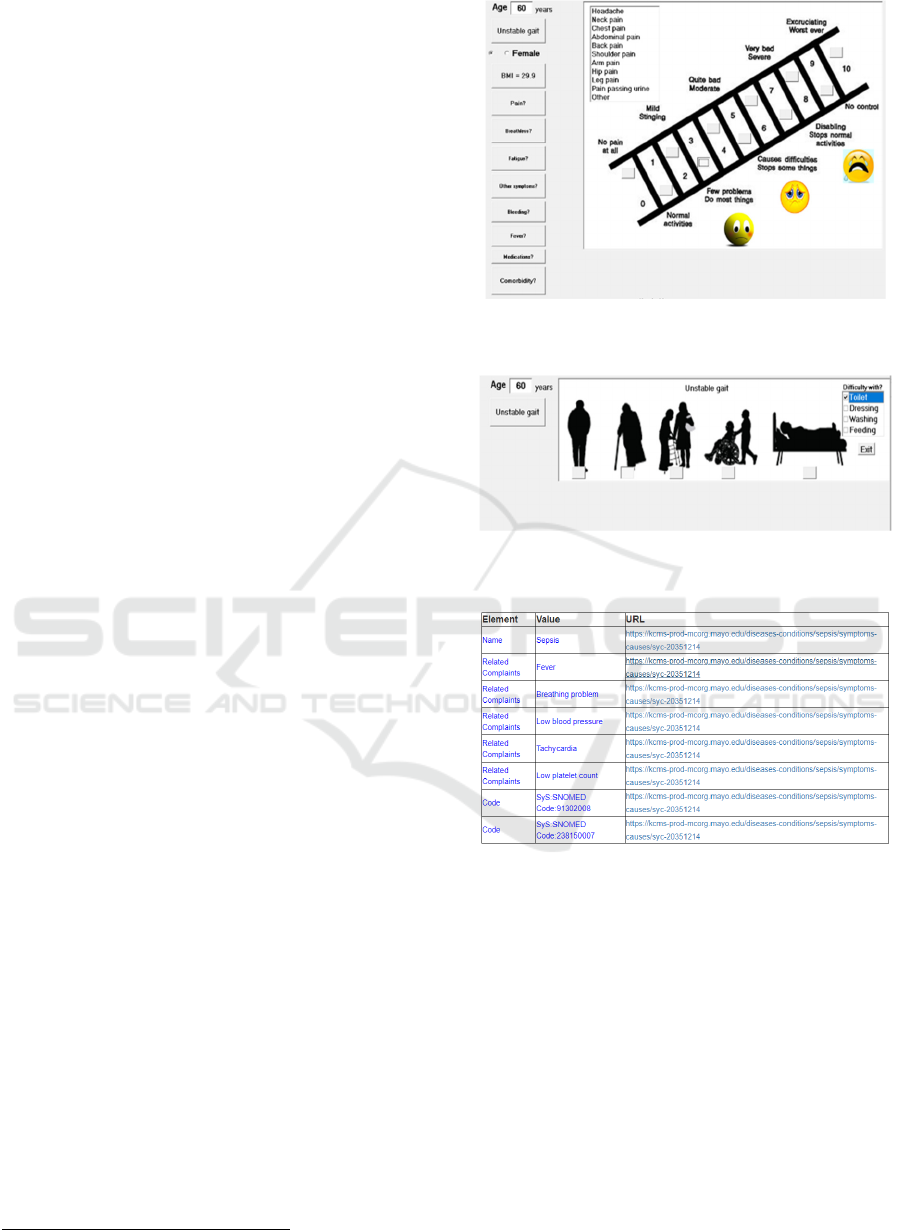
Pilot interfaces have been developed that allow the
user to insert his/her health information in a
conversational way so that the system can create a
profile to tailor the user’s query (Fig. 2 and 3).
Once the user has inserted all the information, the
conversational agent processes the data, applies a
decision rule algorithm, using the tailoring data, and
retrieves the proper content from the schema.org
database (Fig. 4).
8
https://www.nlm.nih.gov/research/umls/index.html
Figure 2: User interface for collecting current health status
(e.g., complaint).
Figure 3: User interface for collecting background health
status (e.g., gait information).
Figure 4: Preliminary output of the conversational agent for
the sepsis disease.
Given that the present repository, as seen in Section
4.2, does not contain all the data that allow a complete
tailoring of information, the conversational agent
only uses the subset of information that allows such
tailoring.
5 CONCLUSIONS
Our overall objective is that anyone anywhere,
regardless of educational level or health literacy, will
have instant access to health information they
Scale-IT-up 2021 - Workshop on Scaling-Up Healthcare with Conversational Agents
822

understand, which will empower them to decide the
wisest interventions, if any, for their immediate and
future wellbeing. In this paper, we presented the
principles and preliminary implementation of a
conversational agent for patient empowerment that
allows the user to specify his or her requests (either
explicitly or implicitly) in terms of complaints and
diseases and receives tailored health results for his or
her understanding and empowerment.
To our best knowledge, this is the first attempt to
create a conversational agent for patient
empowerment (with a specific focus on
comprehension) for general complaints and diseases.
Moreover, the system is making a novel effort to mix
data that come from different fields and are usually
used separately. We are at the initial stage of the
implementation phase and in the process of
completing the health information repository by using
other sources (such as the UMLS) and adding further
tailoring data. We are also implementing the machine
learning and selection mechanism that will provide
the user with high-quality tailored information in a
language that the user can easily understand. We are
also implementing the quality/accuracy mechanism
for the provided information (Alfano et al. 2020b).
We plan to simulate different user typologies to test
the system in all its different aspects and then run
some tests with real users to evaluate its efficacy and
fine-tune it.
ACKNOWLEDGEMENTS
This work was supported, in part, by Science
Foundation Ireland grant 13/RC/2094 and by the
European Union’s Horizon 2020 research and
innovation programme under the Marie Skłodowska-
Curie grant agreement No 754489.
REFERENCES
Alfano, M., Lenzitti, B., Taibi, D., Helfert, M. (2020a)
Language Complexity in On-line Health Information
Retrieval.. In: Ziefle M., Maciaszek L. (eds) Information
and Communication Technologies for Ageing Well and
e-Health. ICT4AWE 2019. Communications in
Computer and Information Science, vol 1219. Springer,
Cham
Alfano, M., Lenzitti, B., Taibi, D., Helfert, M. (2020b).
Tailored Retrieval of Health Information from the Web
for Facilitating Communication and Empowerment of
Elderly People. In Proceedings of the 6th International
Conference on Information and Communication
Technologies for Ageing Well and e-Health - Volume 1:
ICT4AWE, ISBN 978-989-758-420-6, pages 205-216.
DOI: 10.5220/0009576202050216.
Alfano, M., Lenzitti, B., Lo Bosco, G., Muriana, C., Piazza,
T., Vizzini, G. (2020c). Design, Development and
Validation of a System for Automatic Help to Medical
Text Understanding. International Journal of Medical
Informatics, Elsevier.
DOI:https://doi.org/10.1016/j.ijmedinf.2020.104109
Alfano, M., Lenzitti, B., Taibi, D., Helfert, M.. (2019a).
Provision of tailored health information for patient
empowerment: An initial study. In CompSysTech '19
Proceedings of the 20th International Conference on
Computer Systems and Technologies (pp. 213-220).
Alfano M., Lenzitti B., Taibi D., Helfert M. (2019b) ULearn:
Personalized Medical Learning on the Web for Patient
Empowerment. In: Herzog M., Kubincová Z., Han P.,
Temperini M. (eds) Advances in Web-Based Learning –
ICWL 2019. ICWL 2019. Lecture Notes in Computer
Science, vol 11841. Springer, Cham.
Alfano, M., Lenzitti, B., Taibi, D., Helfert M., (2019c).
Facilitating access to health Web pages with different
language complexity levels. Proc. of the 5th Inter.
Conference on Information and Communication
Technologies for Ageing Well and e-Health (ICT4AWE
2019), 2-4 May 2019, Heraklion-Crete.
Alfano, M., Lenzitti, B., Lo Bosco, G., and Taibi, D., (2018).
Development and Practical Use of a Medical
Vocabulary-Thesaurus-Dictionary for Patient
Empowerment. Proc. of ACM International Conference
on Computer Systems and Technologies
(CompSysTech’18), 13-14 September 2018, Ruse.
Bol, N., Smit, E. S., & Lustria, M. L. A. (2020). Tailored
health communication: Opportunities and challenges in
the digital era. Digital Health, 6, 1–3.
https://doi.org/10.1177/2055207620958913
Cheung, K. L., Durusu, D., Sui, X., & de Vries, H. (2019).
How recommender systems could support and enhance
computer-tailored digital health programs: A scoping
review. Digital Health, 5, 1–19.
https://doi.org/10.1177/2055207618824727
Davenport T, Kalakota R. The potential for artificial
intelligence in healthcare. Future Healthc J. (2019).
6(2):94-98. doi: 10.7861/futurehosp.6-2-94.
Denecke, K., Pöpel, A., Hochreutener, S. L., & May, R.
(2018a). Talking to ana: A mobile self-Anamnesis
application with conversational user interface. ACM
International Conference Proceeding Series, 2018-
April, 85–89.
https://doi.org/10.1145/3194658.3194670
Denecke K, Hochreutener SL, Pöpel A, May R. Self-
Anamnesis with a Conversational User Interface:
Concept and Usability Study. Methods Inf Med.
(2018b).57(5-06):243-252. doi: 10.1055/s-0038-
1675822.
European Health Parliament. (2017). Patient empowerment
and centredness.
Fast, E., & Horvitz, E. (2017). Long-term trends in the
public perception of artificial intelligence. 31st AAAI
Conference on Artificial Intelligence, AAAI 2017,
January 1986, 963–969.
Proposed Use of a Conversational Agent for Patient Empowerment
823

Finley CR, Chan DS, Garrison S, Korownyk C, Kolber MR,
Campbell S, Eurich DT, Lindblad AJ, Vandermeer B,
Allan GM. What are the most common conditions in
primary care? Systematic review. Canadian Family
Physician 2018;64:832-840
Herrero, P., López, B., & Martin, C. (2016). PEPPER:
Patient Empowerment Through Predictive Personalised
Decision Support. Artificial Intelligence for Diabetes.
1st ECAI Workshop on Artificial Intelligence for
Diabetes at the 22nd European Conference on Artificial
Intelligence (ECAI 2016), 8–10.
Iatraki, G., Kondylakis, H., Koumakis, L., Chatzimina, M.,
Kazantzaki, E., Marias, K., & Tsiknakis, M. (2018).
Personal Health Information Recommender:
implementing a tool for the empowerment of cancer
patients. Ecancermedicalscience, 12, 1–11.
https://doi.org/10.3332/ecancer.2018.851.
Issom, D. Z., Rochat, J., Hartvigsen, G., & Lovis, C. (2020).
Preliminary evaluation of a mHealth coaching
conversational artificial intelligence for the self-care
management of people with sickle-cell disease. Studies
in Health Technology and Informatics, 270, 1361–1362.
https://doi.org/10.3233/SHTI200442
Jiang F, Jiang Y, Zhi H, et al. (2017). Artificial intelligence
in healthcare: past, present and future. Stroke and
Vascular Neurology 2017;2: e000101. doi:10.1136/svn-
2017-000101.
Kamel Ghalibaf A, Nazari E, Gholian-Aval M, et al. (2019)
Comprehensive overview of computer- based health
information tailoring: a systematic scoping review. BMJ
Open; 9:e021022. doi:10.1136/ bmjopen-2017-021022
Kellett, J., & Deane, B. (2007). The diagnoses and co-
morbidity encountered in the hospital practice of acute
internal medicine. European Journal of Internal
Medicine, 18(6), 467–473.
https://doi.org/10.1016/j.ejim.2007.02.019
Kondyalkis, H., Koumakis, L., & Tsiknakis, M. (2013).
Smart Recommendation Services in Support of Patient
Empowerment and Personalized Medicine. In
Multimedia Services in Intelligent Environments. Smart
Innovation, Systems and Technologies (Vol. 24).
Springer Cham. https://doi.org/10.1007/978-3-319-
00372-6.
Kreuter, M., Farrell, D., Olevitch, L., & Brennan, L. (2000)
Tailoring health messages: customizing communication
with computer technology. Mahwah New Jersey:
Lawrence Erlbaum Associates. Available at:
https://www.popline.org/node/174671.
Kreuter MW, Farrell D, Olevitch L, Brennan L. Tailoring
Health Messages: Customizing Com- munication Using
Computer Technology. Mahwah, NJ: Lawrence
Erlbaum, 1999.
Lustria, M. L. A., Noar, S. M., Cortese, J., Van Stee, S. K.,
Glueckauf, R. L., & Lee, J. (2013). A meta-analysis of
web-delivered tailored health behavior change
interventions. Journal of Health Communication, 18(9),
1039–1069.
https://doi.org/10.1080/10810730.2013.768727
Magyar, G., Balsa, J., Cláudio, A. P., Carmo, M. B., Neves,
P., Alves, P., Félix, I. B., Pimenta, N., & Guerreiro, M.
P. (2019). Anthropomorphic virtual assistant to support
self-care of type 2 diabetes in older people: A
perspective on the role of artificial intelligence.
VISIGRAPP 2019 - Proceedings of the 14th
International Joint Conference on Computer Vision,
Imaging and Computer Graphics Theory and
Applications, 1(Visigrapp), 323–331.
https://doi.org/10.5220/0007572403230331.
MacBryde CM, Blacklow RS, eds. Signs and Symptoms:
Applied Pathologic Physiology and Clinical
Interpretation. 5th edn. Philadelphia: Lippincott, 1970.
Meusel, R., Petrovski, P., and Bizer, C. 2014. The
WebDataCommons Microdata, RDFa and Microformat
Dataset Series. Proc. of the 13th International Semantic
Web Conference (ISWC14), Springer-Verlag New York,
USA, 277-292.
Ni, J., Chen, B., Allinson, N. M., & Ye, X. (2020). A hybrid
model for predicting human physical activity status from
lifelogging data. European Journal of Operational
Research, 281(3), 532–542.
https://doi.org/10.1016/j.ejor.2019.05.035
Noar, S. M., Grant Harrington, N., Van Stee, S. K., &
Shemanski Aldrich, R. (2011). Tailored Health
Communication to Change Lifestyle Behaviors.
American Journal of Lifestyle Medicine, 5(2), 112–122.
https://doi.org/10.1177/1559827610387255.
Petty RT and Cacioppo JT. (1981). Attitudes and
Persuasion: Classic and Contemporary Approaches.
Dubuque, IA:Wm C. Brown, 1981.
Schouten BC, Meeuwesen L. (2006). Cultural differences in
medical communication: A review of the literature.
Patient Education and Counseling 64, 21–34
Snowdon, A. (2020). Digital health: A Framework for
Healthcare Transformation. In HIMSS.
https://doi.org/10.1038/d41586-019-02869-x.
Snyder U. (2008). The doctor-patient relationship II: not
listening. Medscape J Med; 10: 294.
Yadav S. et al. (2019) Suśruta: Artificial Intelligence and
Bayesian Knowledge Network in Health Care –
Smartphone Apps for Diagnosis and Differentiation of
Anemias with Higher Accuracy at Resource
Constrained Point-of-Care Settings. In: Madria S.,
Fournier-Viger P., Chaudhary S., Reddy P. (eds) Big
Data Analytics. BDA 2019. Lecture Notes in Computer
Science, vol 11932. Springer, Cham.
https://doi.org/10.1007/978-3-030-37188-3_10.
You, Y. & Gui, X. (2020). Self-Diagnosis through AI-
enabled Chatbot-based Symptom Checkers: User
Experiences and Design Considerations.
Wasingya-Kasereka, L., Nakitende, I., Nabiryo, J.,
Namujwiga, T., & Kellett, J. (2020). Presenting
symptoms, diagnoses, and in-hospital mortality in a low
resource hospital environment. QJM: An International
Journal of Medicine, May, 1–7.
https://doi.org/10.1093/qjmed/hcaa169
World Health Organization. (2016). Framework on
integrated, people-centred health services: Report by the
Secretariat. World Health Assembly, (A69/39), 1–12.
Scale-IT-up 2021 - Workshop on Scaling-Up Healthcare with Conversational Agents
824
