
To What Scale Are Conversational Agents Used by Top-funded
Companies Offering Digital Mental Health Services for Depression?
Aishah Alattas
1a
, Gisbert W. Teepe
2b
, Konstantin Leidenberger
3c
, Elgar Fleisch
1,2,3 d
,
Lorraine Tudor Car
4,5 e
, Alicia Salamanca-Sanabria
1f
and Tobias Kowatsch
1,2,3 g
1
Future Health Technologies, Singapore-ETH Centre, Campus for Research Excellence and Technological Enterprise
(CREATE), Singapore
2
Department of Management, Technology, and Economics (D-MTEC), ETH Zurich, Zurich, Switzerland
3
Institute of Technology Management (ITEM), University of St. Gallen, St. Gallen, Switzerland
4
Family Medicine and Primary Care, Lee Kong Chian School of Medicine, Nanyang Technological University Singapore,
Singapore
5
Department of Primary Care and Public Health, School of Public Health, Imperial College London, London, U.K.
lorraine.tudor.car@ntu.edu.sg, alicia.salamanca@sec.ethz.ch, tkowatsch@ethz.ch
Keywords: Conversational Agent, Depression, Mental Health, Venture Capital, Top-funded.
Abstract: There is strong support in the literature for the use of conversational agents (CAs) in digital mental healthcare
along with a recent increase in funding within digital mental health, indicating the fast growth of the industry.
However, it is unknown to what extent CAs are leveraged in these digital interventions for depression. The
aim of this study is to therefore explore the scale of CA use in top-funded digital mental health companies
targeting depression and describe what purposes they are used for. Companies were identified through
searching venture capital databases and screened for the presence and purpose of use of CAs in their
interventions for depression. It was found that only 7 out of the 29 top-funded companies used a CA in their
intervention. The most common purpose of CA use was education, followed by assistance, training and
onboarding. None of the interventions used CAs for elderly assistance, diagnosis or prevention. These results
indicate that the industry uptake of CAs in digital interventions for depression within top-funded companies
is low. Future work can look into using CAs in areas which this analysis found they are not currently used
such as in tailoring to different target populations and in preventing depression.
1 INTRODUCTION
Conversational agents (CAs), also known as chatbots,
are computer programs that use techniques from
artificial intelligence and machine learning to mimic
humanlike verbal, written and visual behaviours to be
able to converse and interact with human users
(Vaidyam et al., 2019). The first well-established CA,
ELIZA, was designed in 1966 and programmed to
emulate a Rogerian psychotherapist via typed text
a
https://orcid.org/0000-0003-4777-900X
b
https://orcid.org/0000-0002-2264-9797
c
https://orcid.org/0000-0003-3304-6673
d
https://orcid.org/0000-0002-4842-1117
e
https://orcid.org/0000-0001-8414-7664
f
https://orcid.org/0000-0002-2756-5592
g
https://orcid.org/0000-0001-5939-4145
(Weizenbaum, 1966). Presently, over fifty years later,
the use of CAs is widespread in healthcare and has
been used in multiple points in the continuum of care
such as in prevention through the modification of
lifestyle behaviours, diagnosis and detection, and
treatment and monitoring for a multitude of health
conditions (Tudor Car et al., 2020; Schachner et al.,
2020; Berube et al., 2020).
Since the days of ELIZA, interest in CAs have
fluctuated; however, the boom in technological
Alattas, A., Teepe, G., Leidenberger, K., Fleisch, E., Car, L., Salamanca-Sanabria, A. and Kowatsch, T.
To What Scale Are Conversational Agents Used by Top-funded Companies Offering Digital Mental Health Services for Depression?.
DOI: 10.5220/0010413308010808
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 5: HEALTHINF, pages 801-808
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
801

advancements together with the increasing focus on
mental health in the past twenty years has seen a
significant amount of research in the use of CAs
particularly in mental health conditions (Gaffney et
al., 2019). This is owing to the utility of CAs in
bridging the gap in the perceived trade-off between
barriers to receiving standard face-to-face therapies
for mental illness such as waiting lists, costs,
geography and stigma and the often static nature of
self-guided digital mental health interventions that do
not respond dynamically to individual needs and
preferences (Miner et al., 2016). In this way, CAs
have the potential to create a therapeutic alliance with
the user, which is a key feature of the overall
effectiveness of therapy on patient outcomes such as
symptom severity, treatment compliance and patient
satisfaction, without the involvement of a human
therapist (Lopez et al., 2019).
In a recent review in the mental health setting,
CAs were used for a variety of purposes including
therapy, training, screening, self-management,
counselling, education and diagnosing (Abd-alrazaq
et al., 2019). Another review reported on the
effectiveness of CAs for mental health applications
which showed that they are effective in reducing
levels of depression, anxiety and perceived stress as
well as increasing levels of self-esteem and
psychological wellbeing (Tudor Car et al., 2020). In
terms of user experience, ratings of engagement,
satisfaction, acceptance and helpfulness were in
favour of the use of CAs in these mental health
applications (Tudor Car et al., 2020). Moreover, it has
also been found that the risk of harm from the use of
CAs in mental health is extremely low, with only 1 in
759 participants reported to have a related adverse
event incident (Vaidyam et al., 2019). This particular
incident involved a patient with schizophrenia
developing paranoia and refusing to continue using a
CA intended to promote antipsychotic medication
adherence after a few days, which highlights the
caution that may need to be taken when using CAs in
those with psychotic presentations (Bickmore et al.,
2010).
While mental health disorders in general account
for a large proportion of global disease burden,
depressive disorders are a particular area of concern
as they are the third leading cause of all-age years
lived with disability after low back pain and headache
disorders (James et al., 2018). Depression is
estimated to affect an estimated over 300 million
people worldwide and can greatly impair functioning
and quality of life both through the direct effects of
depressive symptoms as well as through its
association with poor physical health outcomes,
resulting in increased morbidity and mortality (Liu et
al., 2020). Furthermore, latest figures report an
almost 50% increase in the global incident cases of
major depressive disorder worldwide over the past
thirty years, calling for urgent action to actively
intervene and control its occurrence and exacerbation
(Liu et al., 2020).
The manifestation and expression of depression is
complex, with a large amount of heterogeneity both
between and within individuals depending on the
different contexts and challenges faced at different
times. Longitudinal studies have shown that those
experiencing depression may spend up to almost 40%
of their time being asymptomatic, and that even when
symptomatic, patients had a mean of 1 symptom
severity level fluctuation per year with more
fluctuations being associated with poorer function
and quality of life (Vergunst et al., 2013).
Currently, most digital health interventions
targeting depression are modelled to be able to
manage acute symptoms, but do not consider these
important time and context specific aspects that can
alter the experience, and therefore required
intervention for depression (Kornfield et al., 2020).
This mismatch has been cited as a possible reason for
the high levels of dropouts and non-adherence rates
to digital interventions for depression, presenting an
opportunity for the adaptive nature of CAs to
accommodate the temporal dynamics that are at play
in efforts to increase retention and consequently
effectiveness levels of such tools.
Although the evidence base for CAs in mental
health has seen a steady increase over the past two
decades with promising results on their ability to
provide effective, engaging and scalable digital
mental health interventions, little is known on their
actual uptake in the industry. In 2019 alone, venture
capital companies invested a record high of 637
million US Dollars in over 60 mental health
companies, a notable proportion of which went
specifically into digital mental health (Shah and
Berry, 2020). In fact, the latest reports show that a
new record in the deal volume in digital mental health
companies was reached with 68 deals in the third
quarter of 2020 alone (CB insights, State of
Healthcare Q3’20 Report). It thus piques an interest
in the extent to which these new, highly-funded
companies are leveraging CAs in their digital mental
health interventions.
This paper aims to explore the scale at which CAs
are used by top-funded digital mental health
intervention companies and describe what purposes
they are used for. To gain a deeper insight, the scope
of analysis will be narrowed down to those top-
Scale-IT-up 2021 - Workshop on Scaling-Up Healthcare with Conversational Agents
802
funded companies with a main focus on targeting
depression, seeing its high prevalence, burden and
potential for CA technology to enhance therapeutic
approaches in this area. On top of this, the literature
also indicates depression as the most commonly
targeted disorder in the use of CAs in mental health
(Gaffney et al., 2019 ; Abd-alrazaq et al., 2019).
2 METHOD
2.1 Companies
Companies were searched using two venture capital
databases, Crunchbase Pro and PitchBook, which
have been identified to be among the most
comprehensive and accurate of the commonly used
venture capital databases in academic reports and
articles as well as used by investors (Retterath and
Braun, 2020). The search terms (Depression OR
Mental Health) AND (Health care OR Apps OR
Digital health OR Big Data OR Artificial
Intelligence) were entered into Crunchbase Pro and
(Depression OR Mental Health) AND (Digital
Health OR Application Software OR Big Data OR
Artificial Intelligence & Machine Learning OR
Mobile) entered into PitchBook to identify the
companies that were relevant to the field of digital
mental health through October 24, 2020. The
differences in search terms between the two venture
capital databases are a reflection of the specific
verticals that exist on their search options. A filter to
only include the companies that received more than a
million US dollars was also applied when searching
in both databases in order to limit the amount of
companies returned that would not be eventually
included in our list of top-funded digital mental health
companies.
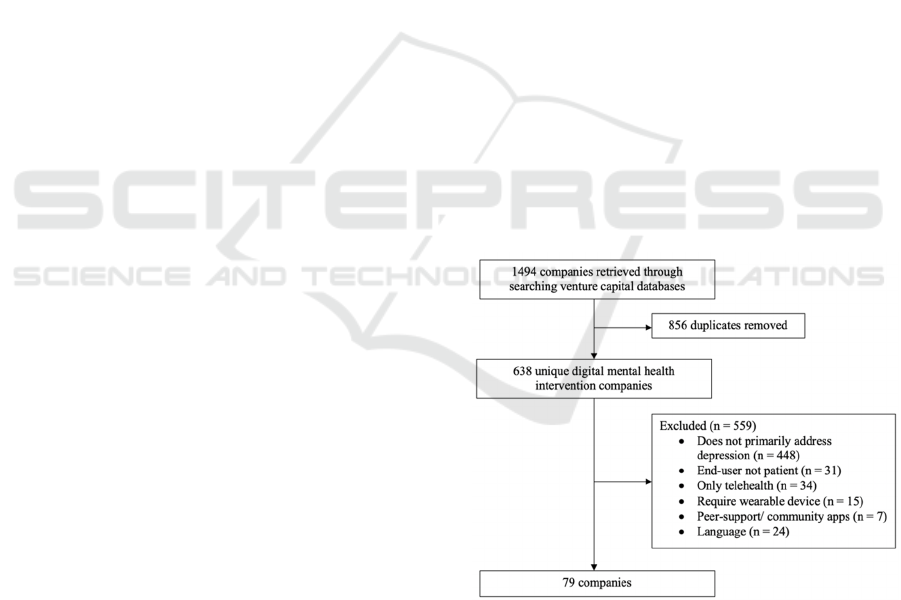
Figure 1 represents the company selection process
based on an inclusion and exclusion criteria defined a
priori. We excluded companies that did not primarily
address depression, that is, for example, companies
offering general health and wellness interventions in
terms of diet and exercise which make
unsubstantiated claims to be able to improve mood
and help with depression. We also excluded
companies where the end-user is not the “patient”,
where patient can be defined as the individual who
will receive intervention for depressive symptoms.
Hence, digital mental health solutions targeted at
healthcare providers for managing their caseload
remotely were excluded as the sphere of this study
focuses on the use in CAs in the therapeutic
engagement with individuals with depression.
For similar reasons, companies that only
offered telehealth services such as triaging and
matching between service users and service providers
without any additional active components were
excluded. Here, we take the definition of “active
components” from the multiphase optimisation
strategy which states a component is “active” if there
is empirical evidence of its therapeutic effectiveness
via measures including but not limited to statistical
significance or effect size (Collins et al., 2007). Other
excluded companies were those that required the use
of a wearable device as this technology has been cited
as being a barrier to the use of digital health
interventions due to factors such as comfort, design,
battery life and connectivity issues (Loncar-Turukalo
et al., 2019), although companies in which the use of
a wearable device was an optional add-on feature
remained included. Those that were purely peer
support or forum platforms and those that were not
available in the English language were also excluded.
The final list of companies was validated on their
credibility, potential utility and validity as an
intervention for depression by two experts with
extensive industry and academic experience in the
field of digital mental health. This was done to ensure
that the major players within the digital mental health
field were not overlooked, while remaining focussed
on the specific area of depression that is being
investigated in this study.
Figure 1: Flow chart of the company selection process.
2.2 Conversational Agent (CA)
A CA was coded to be present in the digital mental
health intervention if there was evidence of the use of
a dialogue system that processes and automatically
responds to human language via text, speech or visual
stimuli. For those interventions that could be
To What Scale Are Conversational Agents Used by Top-funded Companies Offering Digital Mental Health Services for Depression?
803
accessed, the presence or absence of a CA was
established through direct use of the platform and for
those interventions that were unable to be accessed,
this was established through reviewing the
information provided by the intervention company on
their website as well as in peer-reviewed literature.
To determine the purposes that the CAs are used for,
we have coded our findings based on an adapted
version of a taxonomy of CAs in health proposed by
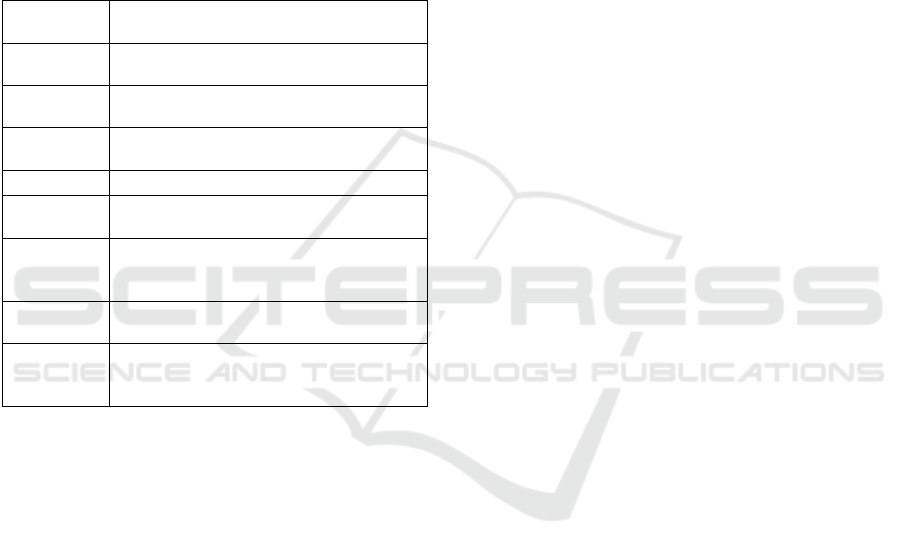
Montenegro et al (Montenegro et al., 2019). Table 1
provides a description of the coded CA uses.
Table 1: Coding framework used to classify the purpose of
use of CAs present in digital mental health interventions.
Purpose of
use of CA
Description
Assistance The CA provides assistance to increase
or improve a behaviou
r
Training The CA trains the user in a health related
b
ehaviou
r
Elderly
assistance
The CA improves a health condition in
the elderly population
Diagnosis The CA gives a mental health diagnosis
Education The CA provides information to increase
mental health literac
y
Prevention The CA aims to prevent the onset, a
deterioration or a relapse of a mental
health condition
Onboarding The CA is used to facilitate the
onboarding process
Questions
and
services
The CA is used for a support purpose
such as technical support or answering
frequently asked questions
2.3 Analysis
The list of digital mental health companies to be
included in our analysis, the presence or absence of a
CA and the purposes that they serve in their
respective interventions were evaluated
independently by two authors (AA and KL) based on
predefined criteria. Any disagreements were resolved
through a discussion and eventual consensus between
the two authors, or brought up to a third author for
adjudication (GWT) where necessary.
3 RESULTS
Out of the 79 companies extracted from the venture
capital databases that met our inclusion and exclusion
criteria, we analysed the 30 top-funded companies as
they accounted for 97.6% of the total funding in all
79 companies, giving a representative and
comprehensive insight into the pattern of common
features present in these interventions. During our
analysis, one of the companies had put a temporary
halt on the intervention being made available on the
market until further notice and was excluded. This
resulted in the final list consisting of 29 top-funded
digital mental health companies.
7 of the 29 interventions (24%) used a CA,
with the most common purpose of use being
education, which was seen in 6 of the 7 (86%) of
interventions that used a CA. This was closely
followed by assistance, training and onboarding
which were each seen in 5 of the 7 (71%)
interventions that used a CA. Only 1 (14%)
intervention used a CA for questions and services.
None of the interventions used CAs for the purposes
of elderly assistance, diagnosis or prevention. Besides
the one intervention that used a CA solely for
onboarding purposes, the other 6 out of 7
interventions used a CA for multiple purposes. The
combination of purposes of use of CA of assistance,
training and education were prevalent in 5 of the 6
interventions that used a CA for multiple purposes.
Table 2 shows a list of the 7 digital mental health
intervention companies that use a CA, a description
of the intervention they offer and how the CA is used.
4 DISCUSSION
4.1 Principal Findings
The results of this analysis indicate that the scale at
which conversational agent and chatbot technology is
utilised by the 29 top-funded digital mental health
intervention companies is rather low at 24%. Some
parallels can be drawn with previous reviews of the
features of CAs in mental health, particularly that
training was reported to be a common use of CAs in
digital mental health interventions and that mental
health diagnosis was reported to be on the rarer side
of CA usage purpose, or in the instance of this
exploratory analysis, not used for this purpose at all
(Abd-alrazaq et al., 2019). Differences were also
seen, one being that while education was the most
common use of CAs in this analysis, other reviews
report education to be among the least common use
of CAs in mental health (Abd-alrazaq et al., 2019). It
should be noted however that this difference is only
striking with regards to ranking and that looking at
absolute values, the difference becomes much less
stark with this study reporting 6 interventions that use
CAs for education and the other reporting 4 (Abd-
alrazaq et al., 2019).
Scale-IT-up 2021 - Workshop on Scaling-Up Healthcare with Conversational Agents
804
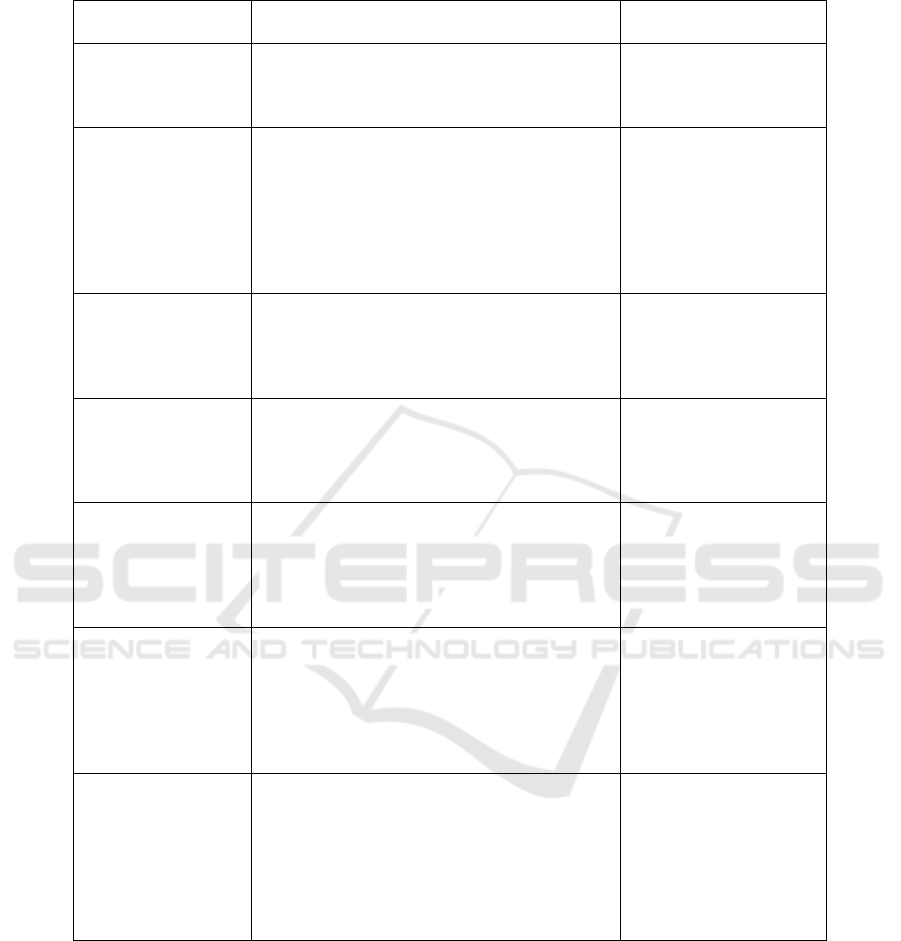
Table 2: Description of intervention and CA use of the 7 out of 29 top-funded digital mental health intervention companies
for depression.
Top-funded
com
p
anies
Description Purpose of CA
Happify The Happify platform provides engaging
activities and games that target overcoming
negative thoughts, stress and life’s challenges
for better overall mental health.
Assistance,
Training,
Education,
Woebot Woebot is an artificial intelligence based chat
tool that is used as a delivery mechanism for a
suite of clinically-validated therapy programs
including psychoeducation, mood monitoring
and in-the-moment guidance that target
behavioural health domains such as sleep, grief
and financial worry as well as clinical domains
like depression, anxiety and substance abuse.
Assistance,
Training,
Education,
Onboarding
Unmind Unmind is a workplace mental health platform
that aims to empower employees to measure,
understand and improve their mental wellbeing
through self-guided programs and in-the-
moment exercises.
Education,
Onboarding,
Questions and Services
Shine Shine describes itself as a daily self-care app
rooted in Acceptance Commitment Therapy
which provides daily meditations, journaling,
mood tracking and the option to connect to an
online communit
y
of users.
Assistance,
Training,
Education
My Online Therapy The My Online Therapy platform offers
matching services with a clinical psychologist
relevant to users’ specific needs, symptoms and
circumstances, video or chat therapy with the
matched therapist and evidence-based self-care
tools.
Onboarding
Wysa Wysa is an artificial intelligence based chat tool
that “will listen and ask the right questions to
help you figure things out”. The platform also
includes self-care tool packs that users can
choose based on specific issues they are facing
such as mood, anxiety, trauma, body image,
slee
p
and loneliness.
Assistance,
Training,
Education,
Onboarding
Youper Youper is an artificial intelligence based therapy
platform that supports users’ mental health
anytime and anywhere through “talking to
Youper like texting a therapist or caring friend”.
Users start by completing a Mental Health
Checkup to personalize Youper to their needs.
There are options to set daily check ins and track
and monitor symptom reduction.
Assistance,
Training,
Education,
Onboarding
4.2 Target Population
Interestingly, the finding that none of the chatbots
were used for the purpose of elderly assistance
mirrors the landscape of a lack of interventions for
depression targeted towards geriatric populations,
despite the high prevalence, poor prognosis and
unique features that contribute to depression in this
demographic such as age related diseases and frailty,
loss of freedom and social isolation (Parkar, 2015).
This brings up a discussion on target populations,
where with the exception of 1 of the companies using
a CA targeted towards employees, the other 6
companies are not targeted towards any specific
demographic.
It is well-established that the factors influencing
the aetiology, expression and prognosis of depression
differ in different populations such as in women
(Albert, 2015), adolescents (Cheung et al., 2018) and
dependent on different cultural backgrounds (Haroz et
To What Scale Are Conversational Agents Used by Top-funded Companies Offering Digital Mental Health Services for Depression?
805

al., 2017). Individually-tailored internet-based or
computerised cognitive behavioural therapy for
depression where users navigate by selecting among
pre-defined response options through which
subsequent content is tailored has been shown to be
effective in reducing depressive symptoms in
naturalistic community settings (Twomey et al.,
2017). CAs can build upon this evidence as a useful
tool to tap into these differences than exist between
populations, to give tailored intervention for
depression that meets individuals unique contexts and
needs in a way that also addresses the benefits of
communicating digitally in a human-like manner.
4.3 Therapeutic Application
The combination of assistance, training and education
that emerged as a core set of purposes that featured in
the CAs in this study can also be thought of as key
elements in popular, evidence-based psychotherapies
for depression in face-to-face and remote virtual
settings such as cognitive behavioural therapy and
mindfulness. This is in that these psychotherapeutic
paradigms are largely focused on education in terms
of psychoeducating individuals on the consequences
of certain habitual patterns of thoughts, feelings and
behaviours, training them to notice these patterns and
providing assistance in implementing techniques to
change maladaptive patterns into more adaptive ones
that can help alleviate symptoms of depression and
improve functioning (Beck, 2011)( Segal and
Teasdale 2018). Indeed, reviews have supported that
it is common for chatbots in mental health to be used
to deliver therapeutic components rooted in cognitive
behavioural therapy, mindfulness and other therapies,
which also aligns with our findings (Tudor Car et al.,
2020; Gaffney et al., 2019).
The finding that none of the CAs were used for
prevention purposes is also in line with the current
landscape, where the prevention of depression has
been largely neglected in comparison to detection and
treatment (Ormel et al., 2019). Reports have
identified reasons for this lack of focus on prevention
to be due to lack of targeting of proximal
determinants of depression such as negative
affectivity, low self-control and poor social and
problem-solving skills as well as prevention of
depression not being structurally and socially
embedded (Ormel et al., 2019). These barriers are
areas that CAs can potentially help to overcome, for
example, in targeting proximal determinants that
exist in the general population, structurally
embedding prevention strategies at national levels
through ease and cost-effectiveness of scalability and
socially embedding through the relatability that
comes with CA communication styles.
In relation to communication styles, although the
mimicking of human-like conversation is widely
reported as a benefit that CAs posses, evidence exists
that may reflect otherwise, especially when sensitive
information is being disclosed such as would be
within mental health and depression. Specifically, not
only was it reported that face-to-face interviews
garnered less accurate responses that are higher in
social desirability compared to the same questions
presented via CA, but that CAs that gave more
relevant and tailored responses to user input also
increased socially desirable response bias compared
to CAs that gave generic responses regardless of user
input (Schuetzler et al., 2018). Other studies have also
supported this notion through findings more relevant
to mental health in that participants who were told
that they were talking to a computer displayed more
intense expressions of sadness than those who were
told that the CA was controlled by a human (Lucas et
al., 2014).
These insights should be taken into consideration
when CAs are being used for therapeutic applications
for depression as it may not serve users in terms
wellbeing and therapeutic outcomes to compromise
on the accuracy of their input in the interest of
tailoring efforts. The key in this instance would be to
determine the minimum amount of tailoring required
for users to develop a therapeutic alliance with the CA
without the CA reaching conversational capability
levels that are too high and thus elicit less accurate
socially desirable responses (Schuetzler et al., 2018).
Miner et al., (2017) has concisely described these
considerations as gaining a better understanding of
users’ “imagined audience” when discussing mental
health with CAs which is highly unclear as opposed
to a traditional in-person consultation where there is
a concrete, visible audience to which the service
users’ impressions and expectations are attached.
4.4 Limitations
The interpretation of the findings of this investigation
into the extent of use of CAs in top-funded digital
mental health companies with interventions targeting
depression should be taken with caution as there is a
high level of variability in the operationalisation of
the terms used to classify the purposes for use of CAs.
For example, Abd-alrazaq et al. (2019) makes a
distinction between CAs that provide therapy versus
training, based on whether the CAs function is rooted
in an established therapeutic paradigm for the former
rather than general skills training such as social skills
Scale-IT-up 2021 - Workshop on Scaling-Up Healthcare with Conversational Agents
806

or job interview skills for the latter. The same was
seen in a review of embodied CAs in clinical
psychology conducted by Provoost et al. (2017),
where in addition to social skills training, the specific
framework of cognitive behavioural therapy was in a
category of its own. A reasonable explanation for
such differences could be that these two reviews
included interventions for autism, of which many are
more focused specifically on social skills training
compared to depression which does not necessitate
such a distinction.
Additionally, the scope of this observational
investigation only focuses on the purpose of use of
CAs in digital mental health interventions targeting
depression. It does not account for the many other
different aspects of CAs that work together and can
influence how effective their integration is on clinical
and user experience outcomes. These include design
characteristics such as whether or not the CA is
embodied, duration of interaction with the CA, its
speech and/or textual output, personality and
aesthetic features like resemblance to human figures
versus other non-human characters (Stal et al., 2020;
Scholten et al., 2017). Existing randomised-
controlled trials tend to look at each of these features
in isolation from the others, which may not be able to
capture the full picture of what makes a CA effective
for a certain person with a certain condition at a
certain time. Making use of optimisation approaches
such as factorial trials, micro-randomised trials or
system identification experiments can be useful in
answering such questions, in order to maximise the
effectiveness and reach of the unique benefits that
CAs can bring to digital mental health interventions
(Hekler et al., 2020).
4.5 Conclusions
Although numerous reviews have provided
compelling support for the added benefits that
integrating a CA into digital mental health
interventions for depression can bring, industry
uptake, at least at the level of top-funded companies,
seems to be relatively low. Despite this, due to the
nascency and the rapidly evolving nature of the field
of digital therapeutics for depression and CA
technology, one could expect the scale at which these
CA tools are implemented to increase over the
coming years, especially with trends such as the
increased number of people who solely use
technology without any in-person visits to address
mental health concerns (Miner et al., 2017). Identified
areas where CAs can be of particular benefit include
in addressing the differing needs that exist in the
intervention of depression between different
demographic groups as well as addressing intra-
individual fluctuations through tailoring and in
preventing depression through targeting its proximal
determinants and embedding prevention structurally
and socially through ease of dissemination.
Future research should look into the establishment
of a taxonomy for categorising the purpose of use of
CAs depression in order to facilitate communication
and comparison. Another important aspect is in
integrating different elements of CA design features
to address a wider scope of determining the efficacy
of CAs in digital interventions. Emerging digital
interventions for depression would benefit from a
collaborative approach between research and
industry, using best practices from each sector to
leverage on the potential that CAs may have on digital
mental health therapeutics. In this regard, the level of
rigor that is encompassed within research settings
combined with industry business models that allow
for rapid and vast dissemination of products lends
itself well to using iterative design processes to
investigate, conceptualise and ultimately create
solutions that can meet the needs of underserved
populations.
REFERENCES
Abd-Alrazaq, A. A., Alajlani, M., Alalwan, A. A., Bewick,
B. M., Gardner, P., & Househ, M. (2019). An overview
of the features of chatbots in mental health: A scoping
review. International Journal of Medical Informatics,
132, 103978.
Albert, P. (2015). Why is depression more prevalent in
women? Journal of Psychiatry & Neuroscience, 40(4),
219–221.
Beck, J. (2011). Cognitive behavior therapy: basics and
beyond. The Guilford Press.
Bickmore, T. W., Puskar, K., Schlenk, E. A., Pfeifer, L. M.,
& Sereika, S. M. (2010). Maintaining reality: Relational
agents for antipsychotic medication adherence.
Interacting with Computers, 22(4), 276–288.
Bérubé, C., Schachner, T., Keller, R., Fleisch, E.,
Wangenheim, F. V., Barata, F., & Kowatsch, T. (2020).
Voice-based Conversational Agents for the Prevention
and Management of Chronic and Mental Conditions: A
Systematic Literature Review (Preprint).
CB Insights. (2020). State of Healthcare Q3’20 Report.
Cheung, A. H., Zuckerbrot, R. A., Jensen, P. S., Laraque,
D., Stein, R. E., & GLAD-PC STEERING GROUP.
(2018). Guidelines for Adolescent Depression in
Primary Care (GLAD-PC): Part II. Treatment and
Ongoing Management. Pediatrics, 141(3).
Collins, L. M., Murphy, S. A., & Strecher, V. (2007). The
Multiphase Optimization Strategy (MOST) and the
Sequential Multiple Assignment Randomized Trial
To What Scale Are Conversational Agents Used by Top-funded Companies Offering Digital Mental Health Services for Depression?
807

(SMART). American Journal of Preventive Medicine,
32(5).
Gaffney, H., Mansell, W., & Tai, S. (2019). Conversational
Agents in the Treatment of Mental Health Problems:
Mixed-Method Systematic Review. JMIR Mental
Health, 6(10).
Haroz, E., Ritchey, M., Bass, J., Kohrt, B., Augustinavicius,
J., Michalopoulos, L., … Bolton, P. (2017). How is
depression experienced around the world? A systematic
review of qualitative literature. Social Science &
Medicine, 183, 151–162.
Hekler, E., Tiro, J. A., Hunter, C. M., & Nebeker, C. (2020).
Precision Health: The Role of the Social and Behavioral
Sciences in Advancing the Vision. Annals of
Behavioral Medicine, 54(11), 805–826.
James, S. L., Abate, D., Abate, K. H., Abay, S. M.,
Abbafati, C., Abbasi, N., … Murray, C. J. L. (2018).
Global, regional, and national incidence, prevalence,
and years lived with disability for 354 diseases and
injuries for 195 countries and territories, 1990–2017: a
systematic analysis for the Global Burden of Disease
Study 2017. The Lancet, 392(10159), 1789–1858.
Kornfield, R., Zhang, R., Nicholas, J., Schueller, S. M.,
Cambo, S. A., Mohr, D. C., & Reddy, M. (2020).
"Energy is a Finite Resource": Designing Technology
to Support Individuals across Fluctuating Symptoms of
Depression. Proceedings of the 2020 CHI Conference
on Human Factors in Computing Systems.
Liu, Q., He, H., Yang, J., Feng, X., Zhao, F., & Lyu, J.
(2020). Changes in the global burden of depression
from 1990 to 2017: Findings from the Global Burden of
Disease study. Journal of Psychiatric Research, 126,
134–140.
Loncar-Turukalo, T., Zdravevski, E., Silva, J. M. D.,
Chouvarda, I., & Trajkovik, V. (2019). Literature on
Wearable Technology for Connected Health: Scoping
Review of Research Trends, Advances, and Barriers.
Journal of Medical Internet Research, 21(9).
Lopez, A., Schwenk, S., Schneck, C. D., Griffin, R. J., &
Mishkind, M. C. (2019). Technology-Based Mental
Health Treatment and the Impact on the Therapeutic
Alliance. Current Psychiatry Reports, 21(8).
Lucas, G. M., Gratch, J., King, A., & Morency, L.-P.
(2014). It’s only a computer: Virtual humans increase
willingness to disclose. Computers in Human Behavior,
37, 94–100.
Miner, A. S., Milstein, A., & Hancock, J. T. (2017). Talking
to Machines About Personal Mental Health Problems.
Jama, 318(13), 1217.
Miner, A., Chow, A., Adler, S., Zaitsev, I., Tero, P., Darcy,
A., & Paepcke, A. (2016). Conversational Agents and
Mental Health.
Proceedings of the Fourth International
Conference on Human Agent Interaction - HAI '16.
Montenegro, J. L. Z., Costa, C. A. D., & Righi, R. D. R.
(2019). Survey of conversational agents in health.
Expert Systems with Applications, 129, 56–67.
Ormel, J., Cuijpers, P., Jorm, A. F., & Schoevers, R. (2019).
Prevention of depression will only succeed when it is
structurally embedded and targets big determinants.
World Psychiatry, 18(1), 111–112.
Parkar, S. (2015). Elderly Mental Health: Needs. Mens
Sana Monographs, 13(1), 91.
Provoost, S., Lau, H. M., Ruwaard, J., & Riper, H. (2017).
Embodied Conversational Agents in Clinical
Psychology: A Scoping Review. Journal of Medical
Internet Research, 19(5).
Retterath, A., & Braun, R. (2020). Benchmarking Venture
Capital Databases. Available at SSRN.
Schachner, T., Keller, R., & Wangenheim, F. v. (2020).
Artificial Intelligence-Based Conversational Agents for
Chronic Conditions: Systematic Literature Review.
Journal of Medical Internet Research, 22(9).
Scholten, M. R., Kelders, S. M., & Gemert-Pijnen, J. E. V.
(2017). Self-Guided Web-Based Interventions:
Scoping Review on User Needs and the Potential of
Embodied Conversational Agents to Address Them.
Journal of Medical Internet Research, 19(11).
Schuetzler, R. M., Giboney, J. S., Grimes, G. M., &
Nunamaker, J. F. (2018). The influence of
conversational agent embodiment and conversational
relevance on socially desirable responding. Decision
Support Systems, 114, 94–102.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2018).
Mindfulness-based cognitive therapy for depression.
The Guilford Press.
Shah, R. N., & Berry, O. O. (2020). The Rise of Venture
Capital Investing in Mental Health. JAMA Psychiatry.
Stal, S. T., Kramer, L. L., Tabak, M., Akker, H. O. D., &
Hermens, H. (2020). Design Features of Embodied
Conversational Agents in eHealth: a Literature Review.
International Journal of Human-Computer Studies,
138, 102409.
Tudor Car, L., Dhinagaran, D. A., Kyaw, B. M., Kowatsch,
T., Joty, S., Theng, Y.-L., & Atun, R. (2020).
Conversational Agents in Health Care: Scoping Review
and Conceptual Analysis. Journal of Medical Internet
Research, 22(8).
Twomey, C., O’Reilly, G., & Meyer, B. (2017).
Effectiveness of an individually-tailored computerised
CBT programme (Deprexis) for depression: A meta-
analysis. Psychiatry Research
, 256, 371–377.
Vaidyam, A. N., Wisniewski, H., Halamka, J. D.,
Kashavan, M. S., & Torous, J. B. (2019). Chatbots and
Conversational Agents in Mental Health: A Review of
the Psychiatric Landscape. The Canadian Journal of
Psychiatry, 070674371982897.
Vergunst, F. K., Fekadu, A., Wooderson, S. C., Tunnard, C.
S., Rane, L. J., Markopoulou, K., & Cleare, A. J.
(2013). Longitudinal course of symptom severity and
fluctuation in patients with treatment-resistant unipolar
and bipolar depression. Psychiatry Research, 207(3),
143–149.
Weizenbaum, J. (1966). ELIZA—a computer program for
the study of natural language communication between
man and machine. Communications of the ACM, 9(1),
36–45.
Scale-IT-up 2021 - Workshop on Scaling-Up Healthcare with Conversational Agents
808
