
Neuroelectrostimulation from Natural Electricity to Multifactorial
Systems: A Review
Vladimir Kublanov
1a
, Konstantin Retyunskiy
2b
, Timur Petrenko
1c
and Mikhail Babich
1d
1
Ural Federal University, Yekaterinburg, Russian Federation
2
Belgorod State University, Belgorod, Russian Federation
Keywords: Neuroelectrstimulation, Neuropsychiatric Diseases, Neurorehabilitation, Electrical Stimulation, Transcranial,
Cranial, Spinal, Cervical Nerve Formations, Polyfactorial, Homeostatic Regulation.
Abstract: The article discusses the problem of the neuropsychiatric health deterioration in the face of new challenges to
humanity: the complication of the scientific and technical environment and the technosphere, social relations
in society against the background of an increase in the duration of a person's active life, as well as the relevance
of the development of neurorehabilitation technologies for restoring human health in these conditions. The
paper presents a review of the evolution of the technology of transcutaneous neuroelectrostimulation from
ancient times to modern technologies, transcranial electrical stimulation, electrical stimulation of cranial
nerves, spinal cord and neck nerve structures. The prospects of a mobile hardware and software system for
polyfactorial neurostimulation and its potential for use in personalized medicine are considered. Possibilities
of promising medical technologies for homeostatic regulation, capable of modulating autonomic processes,
influencing motor control and cognitive functions are discussed.
1 INTRODUCTION
In the 21st century, a person lives in a dynamically
developing scientific and technical environment, the
complication of the technological sphere, social
relations in society against the background of an
increase in the duration of an active life. The
consequence of these processes are new global
problems and challenges that did not exist before -
overpopulation, globalization, hyper information
environment, man-made disasters, interethnic
conflicts, local wars. In such conditions, the load,
especially on the neurological and mental health of a
person, increases significantly, leading to its
exhaustion, chronic stress and, as a result, to
depressive disorder and personality deformation with
complete loss of ability to work and life guidelines.
According to the World Health Organization,
today diseases of the central nervous system have
come out on top among diseases leading to disability
among young people in developed countries. At the
a
https://orcid.org/0000-0001-6584-4544
b
https://orcid.org/0000-0003-1302-483X
c
https://orcid.org/0000-0001-7328-9894
d
https://orcid.org/0000-0001-7077-6611
same time, all areas of human health suffer, limiting
his adaptive capabilities throughout his life. Increased
funding is required to restore health. health care
(WHO, 2016).
The global pandemic of the coronavirus infection
COVID-19 has raised these problems. According to a
WHO study, the COVID-19 pandemic has increased
the demand for neurological and mental health
services: bereavement, isolation, loss of income and
fear for the future disrupt mental health, exacerbate
existing problems. A high level of social stress pushes
people to abuse substances and alcohol. Meanwhile,
there is convincing evidence that the coronavirus has
a neurotoxic effect, leading to impaired perception,
delirium, asthenia, depression. People with pre-
existing mental, drug addiction and neurological
disorders are more vulnerable to coronavirus
infection - they are at high risk of severe outcomes
and even death (WHO Survey, 2020).
Under these conditions, there is a demand for non-
invasive medical technologies for
Kublanov, V., Retyunskiy, K., Petrenko, T. and Babich, M.
Neuroelectrostimulation from Natural Electricity to Multifactorial Systems: A Review.
DOI: 10.5220/0010394302210230
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 1: BIODEVICES, pages 221-230
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
221

neurorehabilitation, capable of restoring psycho-
neurological disorders formed as a result of
depression, stroke, brain and spinal cord trauma or
progressive degenerative and hereditary diseases
(Parkinson's disease, motor neuron disease, etc.).
2 ORGANIZATION PRINCIPLES
OF NEUROPROTECTIVE
THERAPY
Modern approaches to the treatment of neurological
dysfunctions are based on neuroprotective therapy,
which enhances the activity of nervous tissue and its
structural restoration in response to emerging
pathogens. New neurostimulation techniques should
enhance the brain's natural ability to repair damage,
form new functional pathways, facilitate the recovery
process, as well as increase and accelerate functional
neurorehabilitation, improve and optimize the
treatment of acquired brain damage, as well as the
patient's ability to learn. Regardless of the nosological
form of the disease, modern technologies of
neurorehabilitation combine natural therapeutic
factors, drug and non-drug therapy, as well as other
methods aimed at restoring impaired functions
(Doidge, 2007).
Of the specific neuroprotectors, the most studied
and have a strong evidence base are pharmacological
drugs. To date, a large group of drugs that were
effective in the experiment, in clinical therapy were
not so effective because of side effects, in their
severity commensurate with clinical (Tamburin et al.,
2019). The described situation is especially
unfavorable in those cases when the treatment, along
with the existing disease, "interferes" with the natural
course of the regulatory, adaptive processes of the
central nervous system, acting as stress factors.
With non-drug therapy, in which targeted
stimulation is provided by non-thermal physical
signals and fields, side effects problems can be
virtually eliminated (Nudo et al., 2001).
The key link in non-drug technologies for the
restoration of functional disorders of the brain is the
use of the brain's ability to significant functional
restructuring, which triggers the mechanisms of
neuroplasticity when restoring and compensating for
disturbed functions (Egiazaryan & Sudakov, 2007).
When creating modern medical devices and
technologies, the achievements of cybernetics,
medical physics, instrumentation, microelectronics
and information technologies are applied.
3 PERCUTANEOUS
NEUROELECTROSTIMULATI-
ON
Since prehistoric times, people have tried to
understand natural phenomena and use their
capabilities. So, according to the evidence of
numerous artifacts and written sources, even in
ancient times, amber and some species of fish were
used for treatment, capable of generating electrical
discharges. Amber was used to prevent tonsillitis and
other diseases of the throat, and amber, crushed and
mixed with Attic honey, was used for low vision, in
the treatment of delusional conditions. For diseases of
the stomach, amber was recommended to be
consumed either in the form of a finely ground
powder, or with water and mastic. In many ancient
cultures, doctors recommended that their patients
wear stones in the form of amulets and talismans for
health, protection and good luck (von der Emde G,
1999). Persian philosopher and physician Avicenna
(Abu Ali Hussein ibn Abdallah ibn Sina, 980 - 1037).
in his encyclopedia of medical knowledge "Canon of
Medicine" mentions amber as a remedy for many
diseases at any age.
The Roman physician Scribonius Largus, who
lived from 1 to 50 AD, was the first to suggest using
the "strikes" of stingrays for medical purposes: he
advised standing on live rays to relieve headaches and
treat gout. Other physicians of that time also advised
to relieve pain with live rays in the treatment of
several diseases - from epilepsy to rectal prolapse.
There is also a description in the Russian chronicles
of the XIV century, which tells about outlandish fish
placed in a barrel, which, by their touch, caused a
healing effect in humans.
Scientists in medieval Europe studied the
phenomenon of electric fish ("animal electricity"). It
should be noted here the works of G. Cavendish, D.
Walsh, L. Galvani and A. Volta, the results of which
formed the applied direction in medicine - medical
physics, which became an integral part of medical
science. Today we know that electric current is one of
the key phenomena in medical physics, primarily
because the functioning of the human nervous system
is provided by neurons that can generate and transmit
electrical impulses. Therefore, for a living organism,
electric current is a "familiar" physical phenomenon,
and it is widely used in the treatment process.
If we restrict ourselves only to non-invasive
percutaneous solutions, then the following groups are
known from an extensive variety of medical devices
used for neuroelectrostimulation.:
NDNSNT 2021 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
222

1. Transcranial electrical stimulation - provides
regulation of the cerebral blood supply system and
stimulation of the cerebral cortex. The therapeutic
effects in this case are associated with selective ionic
conductivity and systemic-selective biochemical
transformations in the brain tissues. Depending on the
characteristics of the current used in this case, the
following stimulation methods are distinguished
(Mutz et al., 2019):
1.1. Anode transcranial electrical stimulation
(known as "Transcranial direct current stimulation,
tDCS") uses direct electrical current to stimulate. The
function of the active electrode in this case is
performed by the anode, which is located in the
projection of the cortical region to be stimulated,
while the reference electrode is usually located in the
area not associated with the studied brain processes
(forehead, crown, or not on the head). This is a purely
neuromodulation method: the current generated
during tDCS does not induce an action potential but
is maintained at subthreshold levels in order to affect
only cortical excitability. tDCS alters the spontaneous
activity of neural networks without causing
suprathreshold membrane depolarization and
generation of neuronal electrical impulses (Nitsche et
al., 2008). tDCS induces long-term effects that persist
after the end of stimulation due to modulation of
inhibitory intracortical and corticospinal neurons
(Liebetanz et al., 2002). Since a constant electric field
affects all polar molecules, and most
neurotransmitters and receptors in the brain have
electrical properties, tDCS can also affect neuronal
function, causing long-term neurochemical changes.
In this case, tDCS modulates not only the activity of
single neurons, the induced activity of neurons, but
also spontaneous oscillations of neurons, causes not
only long-term changes in the evoked motor
potentials, but also affects the somatosensory and
visual evoked potentials and can affect the state of the
cerebellum (Ardolino et al., 2005). In a study using
functional magnetic resonance imaging, it was found
that tDCS of the primary motor cortex in healthy
volunteers leads to a significant increase in resting-
state cerebral blood flow during and after stimulation.
In this case, cerebral blood flow increases linearly
with increasing current strength (Shigematsu et al.,
2013). tDCS leads to significant changes in the
regional connections of the brain in the default mode
network, frontal-parietal neural networks in the
stimulation and associative areas. Similar changes
were observed in studies involving patients with
Parkinson's disease: strengthening of connections in
neural networks by default is associated with
improved working and semantic memory, and
activation of the frontal and parietal regions is
associated with attention and working memory.
Strengthening of connections in frontal-parietal
neural networks was observed after cognitive training
(Pereira et al., 2012; Wirth et al., 2011). It was found
that tDCS can restore disturbed functional
connections in regulatory systems, which is due to an
improvement in interneuronal, interstructural and
intersystem interactions. The restructuring of the
central functional mechanisms continues after the end
of stimulation, which indicates the activation of self-
regulation mechanisms and, consequently, an
improvement in homeostasis (Lewis et al., 2009). The
effectiveness of using tDCS in medical practice
primarily depends on the choice of current parameters
and the correct positioning of the electrodes on the
head, depending on the type of restored cognitive
function.
1.2. Cathode transcranial electrical stimulation,
Cathode CS, uses direct or alternating electric current
for stimulation, and the cathode acts as an active
electrode. It has been experimentally established that
СathtCS activates the protective mechanisms of the
brain. Only sagittally directed current (location of the
electrodes forehead - occiput or forehead - mastoid
processes) can reach the structures of the protective
mechanisms of the brain. With this position of the
electrodes, the current to the structures of the
protective mechanisms of the brain (the ventral nuclei
of the hypothalamus, the central gray matter of the
midbrain, the nucleus of the suture) flows through the
cisternal and intraventricular pathways. With the
bilateral arrangement of the electrodes (mastoid
process - mastoid process), no current flows to the
structures of the protective mechanisms of the brain.
СathtCS influences endorphinergic mechanisms,
which leads to a significant increase in the
concentration of beta-endorphin in the structures of
the brain stem, dorsal horns of the spinal cord, in the
cerebrospinal fluid and blood, as well as met-
enkephalin in the cerebrospinal fluid. The maximum
increase in the concentration of beta-endorphin is
observed when using rectangular current pulses with
a duration of 3.5 ms and a frequency in the range from
60 to 80 Hz. At the same time, the level of serotonin
in the cerebrospinal fluid also increases (Gabis et al.,
2003).
1.3. Transcranial alternating current stimulation,
tACS, uses amplitude modulated alternating current,
usually sinusoidal, to stimulate. It was found that in
the case of tACS, frequency, intensity and phase are
the main factors influencing the effectiveness of
stimulation. In contrast to tDCS, tACS does not
change the excitability of neurons, but their
Neuroelectrostimulation from Natural Electricity to Multifactorial Systems: A Review
223

transmembrane potential and polarization change.
This leads to an increase in the number of neurons
participating in the formation of the exogenous
frequency: it is assumed that this is due to the fact that
the alternating current participating in the stimulation
process excites endogenous neuronal oscillations,
possibly by increasing the oscillation power or the
index of phase synchronization between excitatory
and endogenous oscillations (Neuling et al., 2012).
This ability to engage neurons in a specific area of the
brain to excite them at a predetermined frequency
allows researchers to identify key frequencies
associated with different types of behavior, and to
identify causal relationships between them. The
specific parameters of these changes depend on the
task, area and state of the brain and are believed to
reflect the structural and functional characteristics of
the activity of neural networks that mediate local and
distributed cortical functions and their cognitive
manifestations. Currently, the most problematic issue
of tACS is the choice of stimulating current
parameters: amplitude and frequency.
1.4. Transcranial random noise stimulation, tRNS,
uses an alternating electrical current with noise-like
amplitude modulation to stimulate. The method was
developed relatively recently. Compared to tDCS,
CattCS and tACS, tRNS is the most effective method
for increasing the excitability of the motor cortex
(Battleday et al., 2014). Based on the results of
physiological and pharmacological studies, several
theories have been proposed to explain the
mechanisms underlying tRNS. According to one of
the proposed theories, broadband amplitude
modulation, formed according to a pseudo-random
law in the tRNS signal, provides a quasi-resonant
effect in target neurons, which increases the
sensitivity of neurons to external influences.
However, it is suggested that the mechanism of action
of tRNS is based on repeated subthreshold
stimulations, which can prevent homeostasis of the
system and potentiate task-related neural activity (van
der Groen & Wenderoth, 2016). To date, relatively
few studies have been published on the effect of tRNS
on functional processes in brain tissues. But the
available evidence shows that tRNS can modulate
cognitive processes, including connectivity. And this
testifies to the great prospects of this direction in
solving problems using neuroelectrostimulation in
neurology and psychiatry.
2. Electrical stimulation of the cranial nerves,
which are input channels directly to the brain. The
effect of neurostimulation in this case is determined
by the effect on the structures of the brain stem, which
leads to the activation of the reticular formation, the
release of neurotransmitters and the suppression of
epileptiform patterns of the cerebral cortex. The most
elaborated solutions in this direction are realized with
the help of translingual neurostimulation and
electrical stimulation of the trigeminal nerve (Bach-
y-Rita, 2004). Medical devices for translingual
Neurostimulation, TLNS, and medical techniques for
their use, known as Cranial Electrical Stimulation
(Cranial Nerve NonInvasive NeuroModulation, CN-
NINM), were developed by a group of scientists from
the University of Wisconsin-Madison (USA). The
ideologist of this trend was the outstanding American
neurophysiologist Paul Bach-y-Rita, known for his
pioneering work in the field of neuroplasticity. Using
the tongue as a target for stimulation can be beneficial
for many applications. The anterior dorsal surface of
the tongue is an area of human skin with a unique
pattern of innervation. Relatively thin, in comparison
with other areas of the skin, the epithelium of the oral
cavity is saturated with mechanical and taste
receptors, as well as free nerve endings. It is uniquely
suited for electrotactile stimulation because, in the
protected environment of the mouth, on the dorsal
surface of the tongue, there is no stratum corneum or
protective layer of skin, such as on the hands and feet,
and sensory receptors are located either on the surface
or close to it. The tongue is constantly washed with
an electrolyte solution (saliva), which has a constant
acidity and temperature. Two main nerves from the
tongue deliver information flows directly to the
brainstem: the lingual nerve, which is a branch of the
mandibular section of the trigeminal nerve (CN-V),
and the chorda tympani, the terminal branch of the
intermediate nerve extending from the facial nerve
(facial nerve, CN-VII). Currently, several
modifications of the PoNS ™ (Portable
Neurostimulator) device have been developed, which
implements the TLNS technology. TLNS technology
was originally developed for modulating neural
networks in neurorehabilitation tasks. Further studies
have shown the possibility of its use for restoring
balance and posture in patients after peripheral
vestibular disorders, as well as for the treatment of
infantile cerebral palsy, imbalance in patients with
multiple sclerosis, restoration of gait in patients with
Parkinson's disease, multiple sclerosis, after TBI and
stroke, restoration of some parameters of cognitive
functioning, such as the ability of a person to quickly
switch attention from one task to another (multi-
tasking), concentration of attention, memory (Paltin
et al., 2017).
The target of trigeminal nerve stimulation
technology, TNS, is the supraorbital nerve, which is
the superior ophthalmic branch of the trigeminal
NDNSNT 2021 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
224

nerve. TNS increases blood flow to areas of the brain
that are associated with the regulation of attention,
emotion, and behavior (Generoso et al., 2019). It has
been found that this stimulation also has an
anticonvulsant effect. These results and data from
pilot clinical trials provide an optimistic view of this
technology in the treatment of epilepsy, depression,
post-traumatic stress disorder and attention deficit
hyperactivity disorder (ADHD).
3. Electrostimulation of the spinal cord - ensures
the restoration of the functioning of the descending
and ascending neural networks of the spinal cord,
which control postural and locomotor functions: this
effect stimulates the primary sympathetic neurons
and interneurons of the spinal cord involved in the
regulation of autonomic functions (Gerasimenko et
al., 2015a). A breakthrough in the development of
spinal cord electrical stimulation technology was
created by fundamental research carried out by
scientists at the I.P. Pavlov Institute of Physiology of
the Russian Academy of Sciences under the
leadership of Yu. P. Gerasimenko. In these studies,
direct experimental evidence was presented for the
existence of a neural spinal network in humans, a
generator of stepping movements, which forms a
locomotor activity program and provides stereotyped
rhythmic coordinated activity of the muscles of each
limb, interlimb coordination, as well as coordination
of the activity of the muscles of the limbs and trunk
for movement in space. The possibility of replacing
activating and controlling supraspinal influences on
stepping generators by means of electrical stimulation
of the spinal cord and pharmacological effects has
been shown. The knowledge gained made it possible
to develop an original electrical stimulator BioStim-5
(Gerasimenko et al., 2015b), as well as a technique
for transcutaneous electrical stimulation of the spinal
cord, which combines the ability to determine the
place of installation of stimulating electrodes through
which single pulses of a rectangular shape are
supplied, and directly stimulate the spinal cord with
modulated impulses of different frequencies and
shapes simultaneously several segments and roots of
the spinal cord. The most important difference of this
device from others is that it implements the
technology of multisegmental stimulation. The
BioStim-5 electrostimulation device allows you to
speed up the rehabilitation process, increase the
amplitude and improve the coordination of the
evoked movements, which is achieved through
synchronous stimulation of various parts of the spinal
cord, carried out simultaneously with natural
physiological stimulation.
4. Electrostimulation of the neck nerve structures
- provides correction of the activity of the
suprasegmental and segmental parts of the autonomic
nervous system by means of exposure to the
projection of the cervical ganglia of the sympathetic
part of this system (V. S. Kublanov, 2008). The
principles of organizing technical means for
stimulating the cervical ganglia of the sympathetic
division of the autonomic nervous system were
proposed in the early 90s of the last centuries and
implemented in the device "Corrector of the activity
of the sympathetic nervous system
SYMPATHOCOR-01" (V. Kublanov et al., 2018).
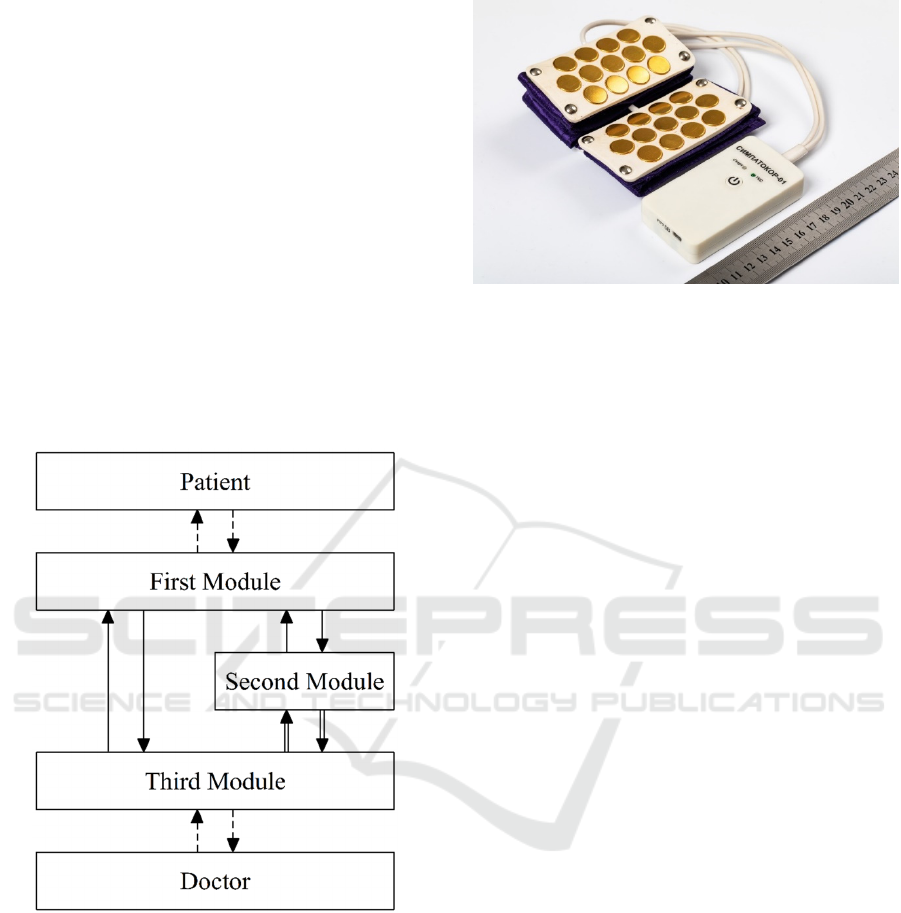
The SYMPATHOCOR-01 device is structurally
made in the form of a monoblock, consisting of two
multi-element electrodes (ME) and an electronic unit,
and has a mass of 1500 g. 13 electrodes are placed on
the cuff of each ME. The appearance of the device
and the layout of its electrodes on the patient's neck
during the treatment are shown in Fig. 1. Between two
MEs, a spatially distributed field of monopolar
positive current pulses is formed, the vector of which
is projected into the target area for stimulation - the
cervical region of the sympathetic trunk, represented
mainly by the upper and middle nodes (ganglia) and
the inter-nodal branches connecting them (Kublanov
et al., 2017).
Figure 1: The appearance of the SYMPATHOCOR-01
device (a) and the layout of its electrodes on the patient's
neck during the treatment procedure are shown (b).
For implementing the algorithm for correction of
the activity of the sympathetic nervous system,
alternation of modes of stimulation and its absence is
used. A typical version of the cyclogram of such an
algorithm looks like this: the patient's functional rest
a
b
Neuroelectrostimulation from Natural Electricity to Multifactorial Systems: A Review
225

for 5 minutes. - stimulation in the projection of the
left cervical ganglia of the sympathetic nervous
system - no stimulation for 5 minutes. - stimulation in
the projection of the right ganglia of the sympathetic
nervous system - functional rest of the patient for 5
minutes.
An information indicator of the processes
corrected with such a dynamic correction of the
activity of the sympathetic nervous system is the
index of vagosympathetic interaction (autonomic
balance), defined as the ratio LF / HF, where LF is the
activity of the low-frequency component of the heart
rate variability spectrum in the frequency range from
0.15 to 0.04 Hz, HF - activity of the high-frequency
component of this spectrum in the frequency range
from 0.4 to 0.15 Hz.
The device is effectively used in the treatment of
vegetative-vascular dystonia, migraine, headache,
tension pain, autonomic dysregulation syndrome,
headache, hyperhidrosis syndrome, orthostatic
hypotension syndrome and postural tachycardia,
neurosis-like syndromes and neuropathies of various
origins, vestibulopathic syndrome, for effective
replacement of invasive insults, treatment of
depression, tic disorders, attention deficit
hyperactivity disorder, hypertension, sensorineural
hearing loss, vasomotor rhinitis, degenerative
diseases of vision and atrophy of the optic nerve,
glaucoma, computer vision syndrome and asthenopia,
incurable epilepsy with attention deficit hyperactivity
disorder in children disorders, Korsakov's (amnestic)
psychosis, panic attacks, anxiety disorders (Petrenko
et al., 2020).
4 POLYFACTOR ELECTRIC
STIMULATION
The technology of polyfactorial electrical stimulation
should provide an effect on three levels of human
nervous regulation: peripheral, autonomic and
central, and be able to combine it with other
technologies. To do this, it is necessary to implement
in a medical device:
1. Possibility of choosing for
neuroelectrostimulation of several local zones of the
neck (targets), the projections of which correspond
not only to the cervical ganglia of the sympathetic
nervous system, but also to targets anatomically
associated with various parts of the brain.
2. Control of the structure of the field of current
pulses and its biotropic parameters is adequate to
pathophysiological changes in the central and
autonomic nervous systems.
3. Compactness and mobility of its
implementation due to the use of new circuit and
technical solutions using microcontrollers and
electrical radio products of a high level of system
integration, as well as modern materials and
technologies that made it possible to implement it in
a compact and mobile device.
4. New hardware and software solutions for
neuroelectrostimulation both for individual and group
use in the treatment process using one control unit.
5. The functions of modern information
technology that will allow it to be used in
personalized medicine.
Modern capabilities of electronic instrumentation
and information technology allow these requirements
to be implemented using a mobile hardware and
software system, consisting of three autonomous
functionally complete modules, which must perform
the following tasks:
• the first module provides the formation of a field
of monopolar rectangular voltage pulses between two
MEs, the installation of stimulation targets, field
structure and biotropic parameters of spatially
distributed pulses of this field;
• the second module is a specialized patient
interface and provides data transmission for the first
module, which are necessary for selecting a
stimulation target, changing the structure of the
voltage pulse field and setting the values of biotropic
parameters of pulses, as well as collecting
information about the patient, his clinical data and
functional parameters of the central and vegetative
nervous systems, as well as control data of the
neurorehabilitation process and transfers them to the
third module;
• the third module is a specialized interface of the
doctor and provides analysis of data about the patient,
his clinical state and functional parameters of the
central and autonomic nervous systems, as well as
data from the control of the neurorehabilitation
process; transmitting data to the second module for
selecting the stimulation target, the structure of the
voltage pulse field and the values of the biotropic
parameters of the pulses; provides the second module
with information for managing the treatment process
(turning on / off the first module, changing the
parameters of the stimulation procedure cyclogram),
as well as comments about the patient and the course
of the treatment process.
To implement the functions of the second module,
it is required to perform certain computational
procedures when generating commands and the
NDNSNT 2021 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
226
structure of a spatially distributed field of current
pulses and parameters of pulses of this field. These
tasks can be solved using a mobile wearable computer
(smartphone, tablet or personal computer), which will
perform the functions of a specialized interface of a
polyfactorial electrostimulation device.
The third module can be implemented as a web
application located on a server with access to the
Internet.
Information between the first and second modules
is transmitted via a telemetric communication
channel Bluetooth Low Energy (BLE): for this
purpose, transceivers built into the first and second
modules are used. Information between the second
and third modules is transmitted via the Internet. The
block diagram of the polyfactorial electrostimulation
device is shown in Fig. 2. General view of the first
module of the polyfactorial electrostimulation device
is shown in Fig. 3.
Figure 2: Block diagram of a polyfactorial
electrostimulation device.
The proposed approach for the implementation of
a polyfactorial electrostimulation device made it
possible to make it compact and mobile with the mass
of the first module less than 200 g.
Figure 3: General view of the first module of polyfactorial
electrostimulation device.
The projections of the cervical ganglia of the
sympathetic nervous system (target 1), the vagus
nerve (target 2), the carotid plexus (target 3), the
cervical spinal plexus (target 4), the accessory nerve
(target 5) and branches of the glossopharyngeal nerve
(target 6).
It is known that several interconnected systems
are involved in ensuring the functional processes of
the brain: neural networks, neuroglia, cerebral
membranes, the cerebrospinal fluid system and the
blood supply system. The latter is a complex
multiparameter biophysical structure with cross-
links, the control of which is provided by neurogenic,
humoral, metabolic and myogenic regulatory circuits.
These circuits are in dynamic interaction and their
activity is aimed at providing physical homeostasis,
determined by the balance of the process of filtration
of water from the blood into the brain tissue under the
action of hydrostatic pressure in the arterial segment
of the capillary and its absorption in the venous
segment of the capillary under the action of oncotic
pressure of blood plasma, and chemical homeostasis
internal environment of the brain.
To implement homeostatic regulation during
polyfactorial neuroelectrostimulation in an
electrostimulation device, it is possible to correct not
only the vegetative balance, but also the very low-
frequency component of the VLF of the heart rate in
the frequency range from 0.04 to 0.003 Hz. VLF
reflects the functional state of the brain in
psychogenic and organic pathology and is also a
sensitive indicator of metabolic processes control and
reflects well the energy deficit states of the brain.
One of the possible algorithms for the
implementation of this task is shown in Fig. 4.
Neuroelectrostimulation from Natural Electricity to Multifactorial Systems: A Review
227
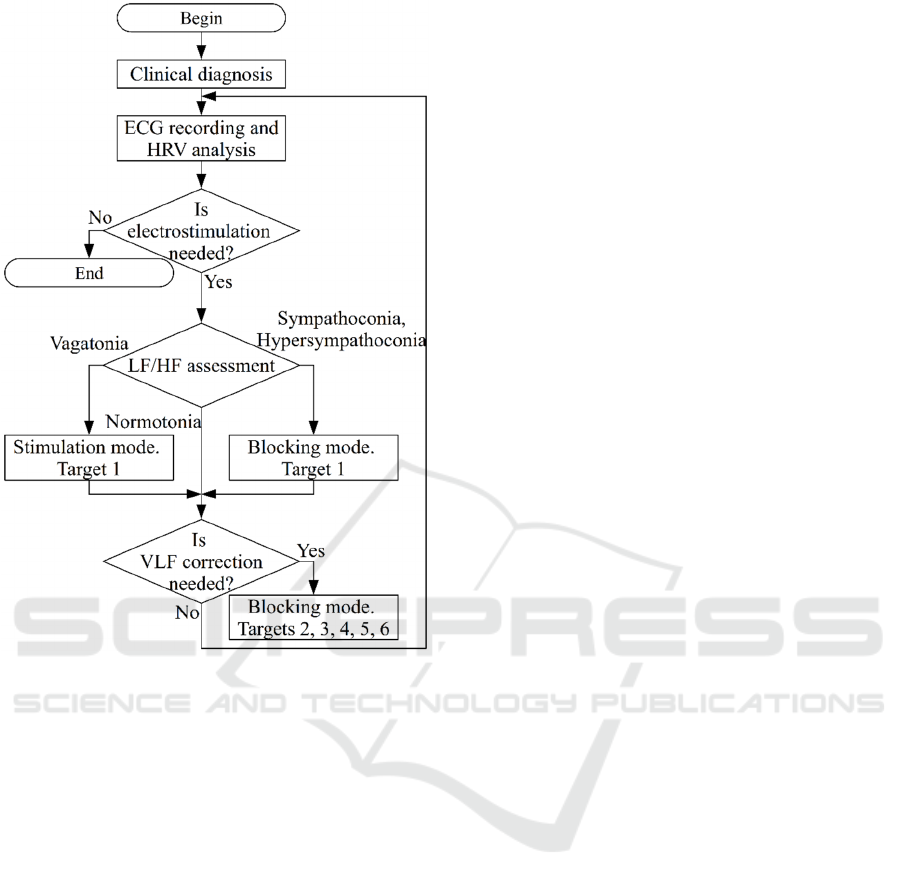
Figure 4: Algorithm for the implementation of
polyfactorism.
The algorithm consists of two stages:
1. At the first stage, target 1 is selected for
stimulation and the LF / HF vegetative balance
indicator is adjusted using the dynamic correction of
the activity of the sympathetic nervous system
technology.
2. At the second stage, one of the targets (2, 3, 4,
5 or 6) or their combination is selected for
stimulation, depending on the leading pathological
process of the central nervous system. In this case,
stimulation occurs through the reticular formation,
thalamic structures and cerebral cortex, and affects
both the vascular tone of the cerebral arteries and the
autonomic nuclei of the spinal cord. The low-
frequency component of the VLF spectrum is an
indicator of changes in the activity of the
suprasegmental cerebral pathways.
The proposed system of neuroelectrostimulation
is capable of fully modulating autonomic processes,
influencing motor control and cognitive functions.
5 CONCLUSIONS
An analysis of the electrostimulation technologies
considered in this work shows that, since ancient
times, the criteria for the formation of these
technologies were based on knowledge about the
processes occurring in the human body. Our
understanding of physiological regulation has
evolved over time from the Greek idea of the balance
of fluids in the body to the concept of homeostasis
and the theory of controlling regulatory processes at
the cellular, tissue and organ levels. Homeostasis has
become the central unifying concept of physiology
and is defined as a self-regulating process through
which a living organism can maintain internal
stability while adapting to changing external
conditions. The health and vitality of the body is the
result of homeostatic regulation of the internal
environment.
When creating new technologies for
neurorehabilitation, other approaches are possible
today, but their foundation should remain the
homeostatic mechanisms of the whole organism,
determined by the coordinated interaction of the
autonomic, immune and endocrine systems, which
support most of the stable states of the organism.
We must proceed from the fact that it is
impossible to create one technology, a panacea for
treatment: the human body is too complex, and its
regulatory mechanisms are diverse. Further research
and testing are needed. And, of course, the results of
the implementation of polyfactorial
neuroelectrostimulation considered in the work are
another step in the movement from natural electricity
to multifactorial systems.
ACKNOWLEDGEMENTS
The reported study was funded by RFBR according
to the research project № 18-29-02052.
REFERENCES
Ardolino, G., Bossi, B., Barbieri, S., & Priori, A. (2005).
Non-synaptic mechanisms underlie the after-effects of
cathodal transcutaneous direct current stimulation of
the human brain. The Journal of Physiology, 568(Pt 2),
653–663.
https://doi.org/10.1113/jphysiol.2005.088310
Bach-y-Rita, P. (2004). Tactile sensory substitution studies.
Annals of the New York Academy of Sciences, 1013, 83–
91. https://doi.org/10.1196/annals.1305.006
NDNSNT 2021 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
228

Battleday, R. M., Muller, T., Clayton, M. S., & Cohen
Kadosh, R. (2014). Mapping the mechanisms of
transcranial alternating current stimulation: A pathway
from network effects to cognition. Frontiers in
Psychiatry, 5, 162.
https://doi.org/10.3389/fpsyt.2014.00162
Doidge, N. (2007). The Brain That Changes Itself: Stories
of Personal Triumph from the Frontiers of Brain
Science (1 edition). Viking.
Egiazaryan, G. G., & Sudakov, K. V. (2007). Theory of
Functional Systems in the Scientific School of P.K.
Anokhin. Journal of the History of the Neurosciences,
16(1–2), 194–205.
https://doi.org/10.1080/09647040600602805
Gabis, L., Shklar, B., & Geva, D. (2003). Immediate
influence of transcranial electrostimulation on pain and
beta-endorphin blood levels: An active placebo-
controlled study. American Journal of Physical
Medicine & Rehabilitation, 82(2), 81–85.
https://doi.org/10.1097/00002060-200302000-00001
Generoso, M. B., Taiar, I. T., Garrocini, L. P., Bernardon,
R., Cordeiro, Q., Uchida, R. R., & Shiozawa, P. (2019).
Effect of a 10-day transcutaneous trigeminal nerve
stimulation (TNS) protocol for depression
amelioration: A randomized, double blind, and sham-
controlled phase II clinical trial. Epilepsy & Behavior,
95, 39–42. https://doi.org/10.1016/j.yebeh.2019.03.025
Gerasimenko, Y., Gorodnichev, R., Moshonkina, T.,
Sayenko, D., Gad, P., & Reggie Edgerton, V. (2015).
Transcutaneous electrical spinal-cord stimulation in
humans. Annals of Physical and Rehabilitation
Medicine, 58(4), 225–231.
https://doi.org/10.1016/j.rehab.2015.05.003
Gerasimenko, Y., Gorodnichev, R., Puhov, A.,
Moshonkina, T., Savochin, A., Selionov, V., Roy, R.
R., Lu, D. C., & Edgerton, V. R. (2015). Initiation and
modulation of locomotor circuitry output with multisite
transcutaneous electrical stimulation of the spinal cord
in noninjured humans. Journal of Neurophysiology,
113(3), 834–842.
https://doi.org/10.1152/jn.00609.2014
Kublanov, V., Aftanas, L., Petrenko, T., Danilenko, K.,
Maria, R., Efimtcev, A., Babich, M., Dolganov, A., &
Sokolov, A. (2018). Investigation of the Neuro-
electrostimulation Mechanisms by Means of the
Functional MRI: Case Study: Proceedings of the 11th
International Joint Conference on Biomedical
Engineering Systems and Technologies, 319–324.
https://doi.org/10.5220/0006712203190324
Kublanov, V., Babich, M., & Dolganov, A. (2017).
Principles of Organization and Control of the New
Implementation of the “SYMPATHOCOR-01” Neuro-
electrostimulation Device. 276–282.
http://www.scitepress.org/DigitalLibrary/Publications
Detail.aspx?ID=KKCrNxrMQJs=&t=1
Kublanov, V. S. (2008). A hardware-software system for
diagnosis and correction of autonomic dysfunctions.
Biomedical Engineering, 42(4), 206–212.
Lewis, C. M., Baldassarre, A., Committeri, G., Romani, G.
L., & Corbetta, M. (2009). Learning sculpts the
spontaneous activity of the resting human brain.
Proceedings of the National Academy of Sciences of the
United States of America, 106(41), 17558–17563.
https://doi.org/10.1073/pnas.0902455106
Liebetanz, D., Nitsche, M. A., Tergau, F., & Paulus, W.
(2002). Pharmacological approach to the mechanisms
of transcranial DC-stimulation-induced after-effects of
human motor cortex excitability. Brain: A Journal of
Neurology, 125(Pt 10), 2238–2247.
https://doi.org/10.1093/brain/awf238
Mutz, J., Vipulananthan, V., Carter, B., Hurlemann, R., Fu,
C. H. Y., & Young, A. H. (2019). Comparative efficacy
and acceptability of non-surgical brain stimulation for
the acute treatment of major depressive episodes in
adults: Systematic review and network meta-analysis.
BMJ (Clinical Research Ed.), 364, l1079.
https://doi.org/10.1136/bmj.l1079
Neuling, T., Rach, S., Wagner, S., Wolters, C. H., &
Herrmann, C. S. (2012). Good vibrations: Oscillatory
phase shapes perception. NeuroImage, 63(2), 771–778.
https://doi.org/10.1016/j.neuroimage.2012.07.024
Nitsche, M. A., Cohen, L. G., Wassermann, E. M., Priori,
A., Lang, N., Antal, A., Paulus, W., Hummel, F.,
Boggio, P. S., Fregni, F., & Pascual-Leone, A. (2008).
Transcranial direct current stimulation: State of the art
2008. Brain Stimulation, 1(3), 206–223.
https://doi.org/10.1016/j.brs.2008.06.004
Nudo, R. J., Plautz, E. J., & Frost, S. B. (2001). Role of
adaptive plasticity in recovery of function after damage
to motor cortex. Muscle & Nerve, 24(8), 1000–1019.
https://doi.org/10.1002/mus.1104
Paltin, D., Tyler, M., & Danilov, Y. (2017). Cognitive
enhancement exciting discovery using trans-lingual
neuro-stimulation. Journal of Neurology and
Neurorehabilitation Research, 02(01).
https://doi.org/10.35841/neurology-
neurorehabilitation.2.1.34-40
Pereira, J. B., Ibarretxe-Bilbao, N., Marti, M.-J., Compta,
Y., Junqué, C., Bargallo, N., & Tolosa, E. (2012).
Assessment of cortical degeneration in patients with
Parkinson’s disease by voxel-based morphometry,
cortical folding, and cortical thickness. Human Brain
Mapping, 33(11), 2521–2534.
https://doi.org/10.1002/hbm.21378
Petrenko, T., Kublanov, V., Retyunskiy, K., &
Sherstobitov, R. (2020). Possibilities of Applying Non-
invasive Multichannel Electrical Stimulation
Technology for Treatment Neuropsychiatric Diseases:
Proceedings of the 13th International Joint Conference
on Biomedical Engineering Systems and Technologies,
421–426. https://doi.org/10.5220/0009377304210426
Shigematsu, T., Fujishima, I., & Ohno, K. (2013).
Transcranial direct current stimulation improves
swallowing function in stroke patients.
Neurorehabilitation and Neural Repair, 27(4), 363–
369. https://doi.org/10.1177/1545968312474116
Tamburin, S., Smania, N., Saltuari, L., Hömberg, V., &
Sandrini, G. (2019). Editorial: New Advances in
Neurorehabilitation. Frontiers in Neurology,
10, 1090.
https://doi.org/10.3389/fneur.2019.01090
Neuroelectrostimulation from Natural Electricity to Multifactorial Systems: A Review
229

van der Groen, O., & Wenderoth, N. (2016). Transcranial
Random Noise Stimulation of Visual Cortex:
Stochastic Resonance Enhances Central Mechanisms of
Perception. The Journal of Neuroscience: The Official
Journal of the Society for Neuroscience, 36(19), 5289–
5298. https://doi.org/10.1523/JNEUROSCI.4519-
15.2016
von der Emde G. (1999). Active electrolocation of objects
in weakly electric fish. The Journal of Experimental
Biology, 202(# (Pt 10)), 1205–1215.
WHO (2016). Disease burden and mortality estimates.
World Health Organization. Retrieved November 25,
2020, from
http://www.who.int/healthinfo/global_burden_disease/
estimates/en/
WHO survey (2020). COVID-19 disrupting mental health
services in most countries. Retrieved November 25,
2020, from https://www.who.int/news/item/05-10-
2020-covid-19-disrupting-mental-health-services-in-
most-countries-who-survey
Wirth, M., Jann, K., Dierks, T., Federspiel, A., Wiest, R., &
Horn, H. (2011). Semantic memory involvement in the
default mode network: A functional neuroimaging
study using independent component analysis.
NeuroImage, 54(4), 3057–3066.
https://doi.org/10.1016/j.neuroimage.2010.10.039
NDNSNT 2021 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
230
