
Towards Customized Medicine with Open-source Applications in
Developing Countries: Foot Drop and Transtibial Prosthesis
Livingston D. Castro Valladares
1 a
, Juan Lam
´
an
1
, Xavier Riccio
1
, David Aucancela
1
,
Francis R. Loayza
1 b
and Gilbert Sotomayor
2
1
Facultad de Ingenier
´
ıa en Mec
´
anica y Ciencias de la Producci
´
on, Escuela Superior Polit
´
ecnica del Litoral,
Guayaquil, Ecuador
2
Hospital de Especialidades Teodoro Maldonado Carbo, Guayaquil, Ecuador
gsotomay dr@hotmail.com
Keywords:
Biomechanics, Ankle-foot-orthosis, Transtibial Prosthesis, 3D-printing.
Abstract:
Alterations in the normal gait can be enhanced to improve patients’ quality of life. Although several devices
improve these conditions, the technology to diagnose and create solutions is expensive. The present work
focuses on developing a methodology to use free software and hardware to create solutions. The process starts
gathering and analyzing the patient’s clinical data; then analyze the human motion kinematics of the patient,
so it is possible to customize and manufacture either an orthotic or prosthetic device. With the aim of imple-
menting the methodology, two cases of study are presented in this work. The patient with foot drop presented
an angular difference between the ankle and the toe of 10.10
◦
± 4.76
◦
, which was corrected throughout the
spring-like behavior of the material used for the 3D printing process. Further, the prosthetic device was a
design with an ankle joint that allows the plantarflexion and dorsiflexion angles of 30° and 25°, respectively.
Therefore, this methodology allows the diagnosing of the angular difference between joints during the normal
gait and how to create either orthotic or prosthetic devices to reduce them. Hence, the present work aims to
open doors towards the customization of medicine and rehabilitation, especially in developing countries.
1 INTRODUCTION
The foot drop is a gait abnormality commonly as-
sociated with several causes such as weakness of
the plantar flexors or the dorsiflexor muscles, lesion
of the peroneal nerve, spinal cord trauma, abnor-
mal anatomy, and neurological dysfunction (Stewart,
2008). A patient uses an orthosis or prosthesis as an
extension of their body to help to improve the gait.
This interaction and its complexity can be seen as a
biomechanical system that needs to be attended by
physical therapists and engineers during the rehabil-
itation process. Hence, it is necessary to develop
methodologies for the rehabilitation process that con-
sider the entire biomechanical interaction and the or-
thosis or prosthesis (Bedotto, 2006; Stewart, 2008).
Among the alternatives to improve this condi-
tion, the use of the ”L” shaped foot-up ankle sup-
port (ankle-foot orthosis AFO) has proved to be a
non-surgical resourceful option (Lenhart and Sumar-
a
https://orcid.org/0000-0002-6253-3553
b
https://orcid.org/0000-0002-6283-3679
riva, 2008; Bedotto, 2006; Stewart, 2008). Another
method uses a cuff placed around the ankle, a top-
side spring, and hook installed under the shoelaces.
The hook connects to the ankle cuff and lifts the shoe
when the patient walks. We can also find complex
mechanical solutions using a passive actuator com-
posed mainly of a gas spring and a cam to lift the foot
(Rodriguez et al., 2018), or using superelastic springs
based on nickel-titanium alloys (Amerinatanzi et al.,
2017; Rodriguez et al., 2018).
On the other hand, another lower limb disabil-
ity condition is transtibial amputation. This proce-
dure is performed to fully remove the lower limb (be-
low the knee) damaged due to trauma, congenital dis-
ease, or diseases like diabetes. Most commercial-
ized transtibial prostheses are energetically passive,
whose main disadvantages are nonsymmetrical gait
patterns and walking at lower speeds. Additionally,
the metal ankle joints provide a characteristic weight
to the prosthesis, which produces around 20% to 30%
more metabolic energy consumption for the amputees
(Au et al., 2009). In this line, some solutions based
762
Valladares, L., Lamán, J., Riccio, X., Aucancela, D., Loayza, F. and Sotomayor, G.
Towards Customized Medicine with Open-source Applications in Developing Countries: Foot Drop and Transtibial Prosthesis.
DOI: 10.5220/0010393507620767
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 5: HEALTHINF, pages 762-767
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reser ved

on powered transtibial prostheses are actually gaining
popularity. However, its main disadvantages are the
high price and the requirement of an additional source
of energy. Other little-explored alternatives for the
fabrication of transtibial prostheses are those based on
additive manufacturing. In this line, the development
of new materials and the feasibility to elaborate com-
plex forms makes them a promising technology.
Healthcare is moving towards the philosophy of
being predictive, preventive, personalized, and partic-
ipatory, which is commonly known as P4 medicine
(Hood, 2008). This is achieved by digitalizing med-
ical information and processing this information in
real-time (Flores et al., 2013; Morley and Vellas,
2017; Pulciani et al., 2017). Thus, it may be possi-
ble to improve patients with lower limb disabilities by
implementing patient-centered methodologies (Creyl-
man et al., 2013; Salles and Gyi, 2012; Salles and
Gyi, 2013). For the design and manufacturing of pros-
thesis and orthosis, the computer-aided design (CAD)
and modern manufacturing techniques appeal to a
particular interest like the 3D printing techniques, due
to their versatility to create complex geometries that
may not be feasible with other manufacturing tech-
niques (Telfer et al., 2012; Dombroski et al., 2014;
Jin et al., 2015; Baronio et al., 2016). Although the
cost of these technologies can be a considerable re-
striction, especially in developing countries, it may
be possible to overcome these difficulties with open
source technologies (de Souza et al., 2017; Loayza
et al., 2018; Tack et al., 2016).
This work aims to develop a methodology to cus-
tomize the design and manufacture of orthotic and
prosthetic devices for patients with foot drop and
transtibial amputation. Besides, the entire method-
ology is developed with free software and hardware.
The present study was carried out in collaboration
between the ESPOL Polytechnic University and the
Teodoro Maldonado Carbo Hospital (hTMC), from
Guayaquil, Ecuador.
2 MATERIALS AND METHODS
The methodology implemented in this work considers
the next steps: 1.) Patients clinical data, 2.) Human
motion kinematics, 3.) Data analysis, 4.) Customized
design, and 5) Implementation and Validation.
2.1 Patients Clinical Data
The first patient was a 45-year-old man with a height
of 1.65 m and 88.6 kg of weight. The patient presents
a foot drop at his right foot, which was diagnosed as
an alteration in the nervous systems by an expert trau-
matologist (GS). Besides, we recruited a control sub-
ject to obtain the motion kinematics data: a 24- year-
old male volunteer with a height and weight of 1.64
m and 73 Kg, respectively. The second patient, a 60-
year-old man, 72kg. of weight and 1.68 m. height,
presents a transtibial amputation of 15 cm. below the
right knee, this due to complications produced by dia-
betes type II. Patients and control subjects signed the
informed consent approved by the university review
board.
2.2 Human Motion Kinematics
The analysis of the human motion kinematics plays
an important role in characterizing the normal gait of
the patient. This analysis was performed only for the
patient with foot drop. We used motion capture tech-
nology to obtain the motion parameters of the subject.
Human motion measures were assessed during multi-
ple trials of treadmill walking of the foot drop patient
and the control subject. Walking speeds were initially
determined by the patient at speeds that he felt com-
fortable walking with running shoes at 0.5 m/s, with
increments and decrements from 1.0 m/s to 2.0 m/s.
Normal speed was 1.0 m/s because, for speeds of 1.5
m/s and 2.0 m/s, the patient had to hold on the tread-
mill to be able to walk.
Previous to the AFO customized design, we as-
sess the patient motion kinematics to obtain the angle
and force required for the design and the conventional
shoe measurements. To assess the influence of the
AFO on the behavior of the lower limb joint angle, the
patient performed two walking trials with four mark-
ers placed along each leg: at the hip, the kneecap,
the heel, and at the toe. These markers were placed
carefully at each joint as a reference for further cal-
culus and analysis. During the first trial, used as a
control, the subject walked without the AFO and us-
ing his conventional shoes. For the second trial, the
patient wore the AFO on the left foot. The data ac-
quisition was performed using an iPhone 8 camera of
1080 pixels located over a tripod at a 2 m distance
from the treadmill. The camera was recording at 60
frames per second (FPS) for both legs. The recordings
were made on both sides of the subject to get a bet-
ter perspective of the movements of both legs. Each
recording of the elapsed time for each leg was of 20
seconds, equivalent to approximately ten gait cycles.
2.3 Data Analysis
For the data analysis, we used the software Tracker®
(Tracker video analysis and modeling tool) and
Towards Customized Medicine with Open-source Applications in Developing Countries: Foot Drop and Transtibial Prosthesis
763

Python®. The software tracker® let us analyze the
regular gait video, display the markers, and discretize
the positions within the recording time. Python was
used for the corresponding analysis and plotting re-
sults. For each recording (6 previous and 6 wearing
the AFO), we measured each angular position of the
joint, frame by frame. The measured data was plot-
ted to select a time window of 10 gait cycles after re-
viewing it for a constant period (Figure 1). Further,
each gait cycle was split out, and then we obtained
the average and standard deviation for each angular
data point of each joint, previously checking for its
normal distribution. Finally, the average of the angu-
lar position and its corresponding standard deviation
of the data points were plotted by using Python® as
is shown in Figure 2. to obtain the average values
of the angles and standard deviation and calculate the
necessary angular compensation of the foot drop in
reference to the healthy foot.
2.4 Customized Design of the Orthosis
With the dimensions of the leg and the food, it is
possible to adapt an orthotic device to the anthropo-
morphic characteristics of the patient. The orthotic
device dimensions were defined with the CAD soft-
ware, which allows parametrizing and easily making
changes. The manufacture of the design was executed
with a 3D printer (Creality®, model CR-3040s). The
orthosis was divided into six parts, where five of them
work as rigid components printed with PLA at 40% of
triangles infill, at 200
◦
C, 0.2 mm resolution, 1.2 mm
wall thickness and 8 hours of print time. The flexi-
ble component, which works as spring-like behavior,
was 3D printed with TPU at 50% infill at 235ºC, 0.2
mm resolution, 0.8 mm wall thickness, and 10 hours
of print time. All components were designed using
FreeCad and then exported as STL format.
2.5 Orthosis Implementation and
Validation
Once the device was implemented, the gait of the
gait was recorded to process the information in the
tracker® analysis software and plot the data obtained
in Python® to compare the three cases: foot drop
without orthosis, foot drop with the orthosis, and the
healthy subject.
2.6 Prosthesis Design
king anthropometric measures of the left leg. This lets
us design the prosthesis according to their anthropo-
metric measurements.
The prosthesis was divided into two elements:
the foot and the shank joined via a bolted joint at
the ankle. According to the requirements, the com-
plete shank, including the socket, was designed to be
printed as a rigid component with PLA or ABS. The
foot, instead, including the ankle, was designed to be
printed as a flexible component. The idea was to take
advantage of the flexibility of the material to provide
an adequate rotation at the joints, of both the toes and
the ankle, as well as vertical cushioning.
To design both components, we used Blender soft-
ware version 2.8. The shank was designed as a solid
element down to the socket base, as shown in figure
5A. The prosthetic right foot was designed base on the
anatomy of the left foot. To give it flexibility and ro-
tation in the ankle and toe joints, like a flexible hinge,
some groves were made in both sides of the instanta-
neous center of rotation, as shown in figure 5B. These
flexible hinges were tested in the first design under
the working condition with the weight of the patient.
After several tests, we found that the flexible hinges
deteriorated only at the ankle joint, due to the verti-
cal load. After two additional iterations and tests, the
final design of the flexible joint at the ankle was the
incorporation of two S-like springs that can work as
tendons and ligaments attached to the shank, as shown
in figure 5B-2.
Before printing the final foot, we estimated the
printing parameters according to (Mutlu et al., 2016).
Additionally, we performed two experiments to esti-
mate the percent of infill. For that, we created a foot
part that includes only the flexible knee joint. Then,
this part was printed twice with two different infill set-
tings: 50% and 20%. Further, those parts were sub-
jected to rotational deformation with the application
of different torsion loads.
The manufacture of the components of the pros-
thesis was performed with the 3D printer (Creality®,
model CR-3040s) with the following parameters: the
shank was printed in one piece with PLA, and 30% of
triangles infill at 200ºC, 0.4 mm resolution, 1.2 mm
wall thickness and 53 hours of print time. The foot
was printed with TPU with 25% of triangles infill at
235ºC, 0.2mm resolution, 0.8 mm wall thickness, and
55 hours of print time.
3 RESULTS
This section describes the results for the two patients,
the foot drop and the amputee patient.
HEALTHINF 2021 - 14th International Conference on Health Informatics
764
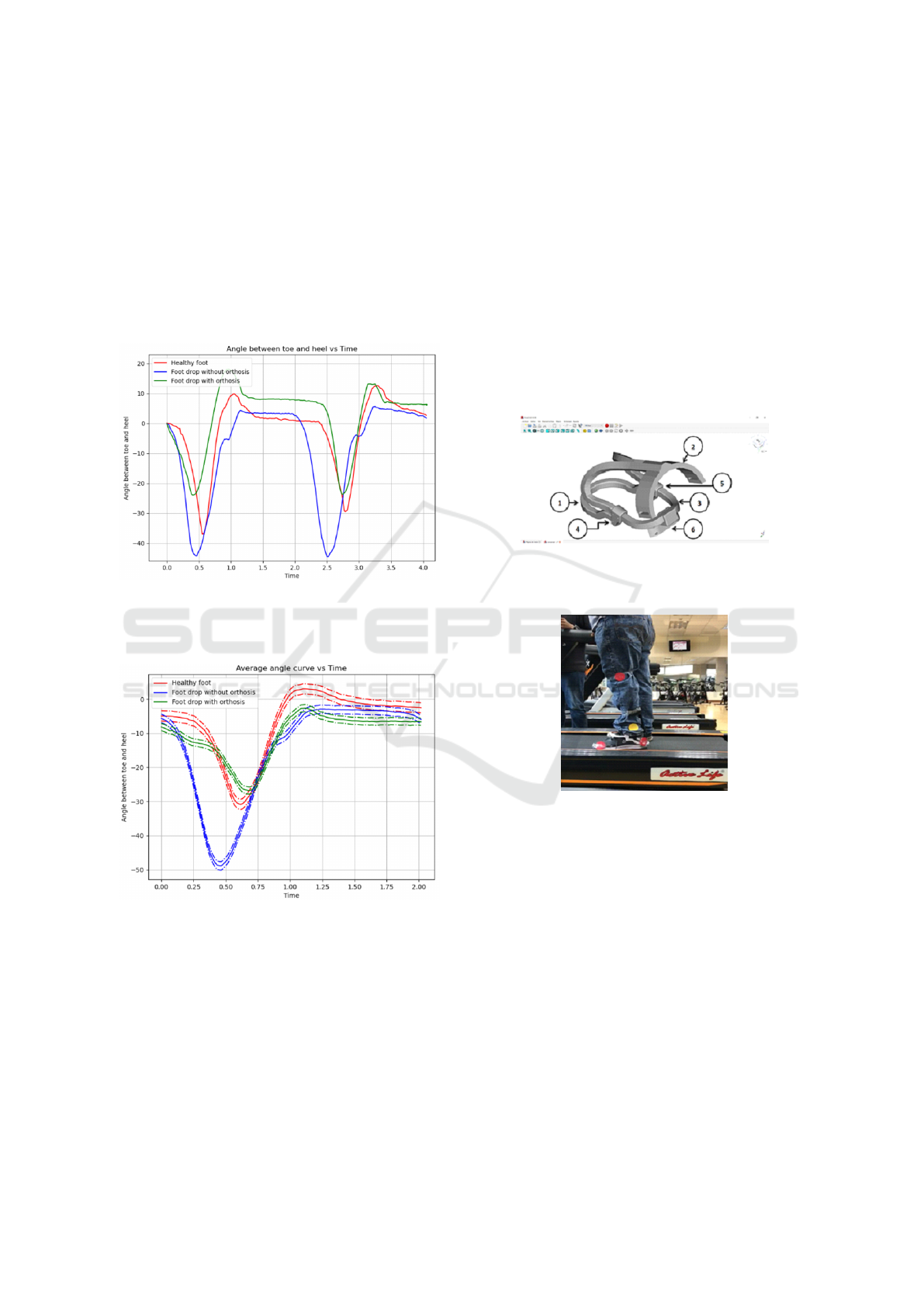
3.1 Foot Drop Patient
The normal gait of the patient was recorded at 1 km/h,
where the curve represents the angle of the ankle dor-
siflexion/plantar flexion. Three different cases are
plotted in figure 1 and 2 for this study; healthy foot,
drop foot without orthosis, and drop foot with an or-
thosis. Additionally, the orthosis 3D model is pre-
sented in figure 3 and 4 shows the patient wearing
the AFO on the treadmill.
Figure 1: The curve of the angle between toe and heel vs.
time. The red line corresponds to a healthy foot. The blue
line corresponds to the foot drop patient without orthosis.
The green line corresponds to the foot drop with an orthosis.
Figure 2: The average curve of the angle between toe and
heel vs. time. The red line corresponds to a healthy foot.
The blue line corresponds to the foot drop patient without
orthosis. The green line corresponds to the foot drop with
an orthosis.
The measurements of the normal gait were
recorded at 1 Km/h to feel comfortable during the
recording process. The peak values of the angles
of each curve were chosen to calculate the aver-
age and its standard deviation, and both angles were
subtracted to obtain the necessary compensation of
the foot drop. The difference between the patient’s
healthy foot compared to his dropped foot is in the
value of the angle that the toe presented with respect
to the heel, causing a difference of 10.1 degrees be-
tween both cases. This occurs because the dropped
foot causes a person to drag their foot while walk-
ing, which increases the angle between the toe and
the heel.
It was necessary to correct the angular difference
because continuing to drag the foot during walking
may cause the thigh to rise at the moment of the march
as if one were climbing stairs. This causes the foot to
hit the floor with every step. As in most patients, the
upper skin part on the foot and toes is sensitive to the
impact created by the movement.
Figure 3: Shows the design of the prosthetic device per-
formed in FreeCad. This model was then exported in STL
format, which was 3D printed in a flexible material (TPU).
Figure 4: Depicts the tracking measures performed with the
foot drop patient using the treadmill.
The angular difference between both feet was re-
lated to the deformation that flexible material can
have so that the angles of the toes of both feet will be
similar. To achieve this, it was necessary to consider
the force required to maintain the foot in the natural
position during the normal gait; thus, the drop foot
moves approximately like the healthy foot.
3.2 Amputee Patient
After removing the support material in both 3D
printed elements, the following table summarizes the
results. Besides, the prototype is shown in figure 5.
The plantarflexion and dorsiflexion angles ob-
tained for the ankle joint were 30º and 25º, respec-
Towards Customized Medicine with Open-source Applications in Developing Countries: Foot Drop and Transtibial Prosthesis
765

Table 1: main settings of the printed elements.
Element Foot Shank
Print time (h) 55 53
Print temperature (ºC) 235 200
Material TPU PLA
Resolution (mm) 0.2 0.4
% infill 25 30
Infill type triangle triangle
Weight (g) 490 220
tively as is shown in figure 6. For the toe joint, the
angular rotation for this flexible hinge was 36º in both
directions. The total cost of printing both items was
USD 80.00, including the material and the printing
itself.
Figure 5: Panel A depicts the assembling of both elements.
Panel B shows the foot printed with flexible material where
1 is the flexible hinge for the toe, 2 the flexible hinge for the
ankle, 3 the cushioning element, and 4 two slots are shown
with their respective holes that allow an elastic band to be
added by screws on each side to complement the elasticity
of the ankle joint if necessary. Panel C shows the printed
foot.
Figure 6: Upper left, it is shown the plantarflexion angle
and, on the right, the dorsiflexion angle. The bottom picture
shows the patient wearing the prosthesis.
4 DISCUSSION AND
CONCLUSIONS
In this work, two customized solutions 3D printed are
presented. The first solution was an orthotic device
for a patient with a foot drop, and the second solution
consists of a transtibial prosthetic device for an am-
putee patient. In both cases, we used a combination
of flexible and rigid material printed with the FDM
technique.
Currently, there are several designs and methods
to manufacture lower limb orthosis. Nevertheless, not
all of them represent viable options due to the cost
of software and manufacturing equipment. Thus, the
choice of using free software and hardware is appeal-
ing for these types of applications, especially in de-
veloping countries. For example, the manufacturing
cost of this case study was USD 55. In the same line,
the majority of commercial transtibial prostheses are
manufactured using expensive techniques and mate-
rials that, in many cases, are unaffordable for low-
income patients.
Even though the free software helps achieve the
objectives of this project, it always is possible to im-
prove the designs. Current applications in this area
use active parts, which represent a significant advan-
tage towards rehabilitation. Nevertheless, the cost
increments, and the more components are used, the
higher is the probability of failure during operation.
Therefore, the present work considers the use of sim-
ple components and designs. Additionally, as the
manufacturing price has dropped considerably, it is
possible to create different designs with the purpose
of rehabilitation and testing. Although, it is necessary
to make a trade-off between potential environmental
effects of the manufacturing and the designs before
moving forward in this direction.
It is important to mention that only the case of the
patient with foot drop was validated through a human
motion kinematics analysis. The case of the transtib-
ial amputation was not possible to evaluate the human
motion kinematics because the patient was within the
phase of physical rehabilitation and was still getting
used to the prosthetic device.
For future work, the methodology presented in
this work needs to be applied to a larger number of
cases, of each type of medical condition, either foot
drop or transtibial amputation. Thus, it may be possi-
ble to make a clinical analysis.
4.1 Conclusion
With the proposed methodology in this work, it is
possible to fabricate orthotic and prosthetic devices
HEALTHINF 2021 - 14th International Conference on Health Informatics
766

through 3D printing techniques, taking advantage of
the characteristics of different materials available in
the market. Further, devices that can improve the foot
drop and amputee problems using free software and
hardware are suitable for developing countries.
ACKNOWLEDGEMENTS
We thank the two patients who voluntarily collabo-
rated with this study.
REFERENCES
Amerinatanzi, A., Zamanian, H., Shayesteh Moghaddam,
N., Jahadakbar, A., and Elahinia, M. (2017). Appli-
cation of the superelastic niti spring in ankle foot or-
thosis (afo) to create normal ankle joint behavior. Bio-
engineering, 4(4):95.
Au, S. K., Weber, J., and Herr, H. (2009). Powered ankle–
foot prosthesis improves walking metabolic economy.
IEEE Transactions on Robotics, 25(1):51–66.
Baronio, G., Harran, S., and Signoroni, A. (2016). A critical
analysis of a hand orthosis reverse engineering and 3d
printing process. Applied bionics and biomechanics,
2016.
Bedotto, R. A. (2006). Biomechanical assessment and treat-
ment in lower extremity prosthetics and orthotics: a
clinical perspective. Physical Medicine and Rehabili-
tation Clinics, 17(1):203–243.
Creylman, V., Muraru, L., Pallari, J., Vertommen, H., and
Peeraer, L. (2013). Gait assessment during the ini-
tial fitting of customized selective laser sintering ankle
foot orthoses in subjects with drop foot. Prosthetics
and orthotics international, 37(2):132–138.
de Souza, M. A., Schmitz, C., Pinhel, M. M., Setti, J. A. P.,
and Nohama, P. (2017). Proposal of custom made
wrist orthoses based on 3d modelling and 3d print-
ing. In 2017 39th Annual International Conference of
the IEEE Engineering in Medicine and Biology Soci-
ety (EMBC), pages 3789–3792. IEEE.
Dombroski, C. E., Balsdon, M. E., and Froats, A. (2014).
The use of a low cost 3d scanning and printing tool
in the manufacture of custom-made foot orthoses: a
preliminary study. BMC research notes, 7(1):1–4.
Flores, M., Glusman, G., Brogaard, K., Price, N. D., and
Hood, L. (2013). P4 medicine: how systems medicine
will transform the healthcare sector and society. Per-
sonalized medicine, 10(6):565–576.
Hood, L. (2008). Systems biology and systems medicine:
from reactive to predictive, personalized, preventive
and participatory (p4) medicine. In 2008 30th Annual
International Conference of the IEEE Engineering in
Medicine and Biology Society, pages cliv–cliv. IEEE.
Jin, Y., Plott, J., Chen, R., Wensman, J., and Shih, A.
(2015). Additive manufacturing of custom orthoses
and prostheses—a review. procedia cirp 36: 199–204.
Lenhart, R. L. and Sumarriva, N. (2008). Design of im-
proved ankle-foot orthosis.
Loayza, F. R., Sola-Mora, J., Castro-Valladares, L., Litardo,
J., Nu
˜
nez-Idrovo, L., and Mora, H. (2018). Pre-
operative patient-specific alloplastic implant design
and manufacturing: cranioplasty application. In
2018 IEEE Third Ecuador Technical Chapters Meet-
ing (ETCM), pages 1–5. IEEE.
Morley, J. E. and Vellas, B. (2017). Patient-centered (p4)
medicine and the older person. Journal of the Ameri-
can Medical Directors Association, 18(6):455–459.
Mutlu, R., Alici, G., in het Panhuis, M., and Spinks, G. M.
(2016). 3d printed flexure hinges for soft monolithic
prosthetic fingers. Soft Robotics, 3(3):120–133.
Pulciani, S., Di Lonardo, A., Fagnani, C., and Taruscio,
D. (2017). P4 medicine versus hippocrates. Annali
dell’Istituto superiore di sanita, 53(3):185–191.
Rodriguez, K., de Groot, J., Baas, F., Stijntjes, M., van der
Helm, F., van der Kooijl, H., and Mugge, W. (2018).
Passive ankle joint stiffness compensation by a novel
ankle-foot-orthosis. In 2018 7th IEEE International
Conference on Biomedical Robotics and Biomecha-
tronics (Biorob), pages 517–522. IEEE.
Salles, A. S. and Gyi, D. E. (2012). The specification of per-
sonalised insoles using additive manufacturing. Work,
41(Supplement 1):1771–1774.
Salles, A. S. and Gyi, D. E. (2013). An evaluation of per-
sonalised insoles developed using additive manufac-
turing. Journal of Sports Sciences, 31(4):442–450.
Stewart, J. D. (2008). Foot drop: where, why and what to
do? Practical neurology, 8(3):158–169.
Tack, P., Victor, J., Gemmel, P., and Annemans, L. (2016).
3d-printing techniques in a medical setting: a system-
atic literature review. Biomedical engineering online,
15(1):115.
Telfer, S., Pallari, J., Munguia, J., Dalgarno, K., McGeough,
M., and Woodburn, J. (2012). Embracing additive
manufacture: implications for foot and ankle orthosis
design. BMC musculoskeletal disorders, 13(1):84.
Towards Customized Medicine with Open-source Applications in Developing Countries: Foot Drop and Transtibial Prosthesis
767
