
SAR-ACT: A Spatial Augmented Reality Approach to Cognitive Therapy
Rui Silva
1,2 a
and Paulo Menezes
1,2 b
1
Department of Electrical and Computer Engineering, University of Coimbra, Coimbra, Portugal
2
Institute of Systems and Robotics, University of Coimbra, Coimbra, Portugal
Keywords:
Interactive Environments, Spatial Augmented Reality, Cognitive Therapy, Elderly Care, Serious Games.
Abstract:
It is predicted that longevity will keep increasing in the forthcoming centuries. Thus, the elder demographic
will grow, and the surge of age-related diseases will become more prevalent. These conditions can affect
autonomy and affect the quality of life by reducing cognitive and motor capacities. While medical interven-
tions have been progressing, preventive and restorative therapies remain an essential part of the rehabilitation
process. Consequently, there is a high demand for tools that can help enhance the effectiveness of therapy.
This work proposes a spatial augmented reality framework for creating card-based serious games for cognitive
therapy. The objectives of the project are: to use this technology to facilitate the adaptability and person-
alization of serious games, to create an engaging tool that helps mitigate frustration in therapy, and to help
therapists to keep track of patients’ progress to adapt future sessions. Two serious games were developed to
test the applicability of the framework. An analysis of the work was made by a specialist that concluded it had
accomplished the desired objectives and that it has promising results for future validation in cognitive therapy.
1 INTRODUCTION
Since the middle of the XIX century, longevity around
the world has increased at an exceptional rate, evolv-
ing from the global average of 29 to 73 years old (in
2019) (Max Roser and Ritchie, 2013). According to
United Nations’ predictions, life expectancy is going
to surpass 100 years by 2300 (United Nations Depart-
ment of Economic and Social Affairs of the United
Nations, 2004). This data gives assurance that the
world’s health will continue its ascending trend, but
also warns us that the population will get consider-
ably older. While it is positive news that people will
have longer-lasting lives, it raises a question on how
will the quality of these lives be (Robine et al., 2009).
Age-related health issues will surge with senescence.
These conditions can occur in multiples ways affect-
ing motor and cognitive skills, and if we do not work
on trying to improve our approach to them, whether
being with lifestyle changes, medically, pharmaceu-
tically and therapeutically, then longer lives will not
translate to healthy lives (Jaul and Barron, 2017). The
surge of neurodegenerative Alzheimer’s or Parkin-
son’s disease and traumatic complications such as
strokes cause cognition to decay. They can signifi-
a
https://orcid.org/0000-0003-4581-7375
b
https://orcid.org/0000-0002-4903-3554
cantly impair the execution of daily tasks, causing el-
ders to lose autonomy and, consequently, their quality
of life (Mioshi et al., 2007).
Cognitive impairments can manifest themselves in
various areas such as attention, memory, judgment,
decision making, logic and abstract thinking, orien-
tation, and language (Glisky, 2019). When patients
manifest symptoms of cognitive decay, it is crucial
to diagnose their condition and evaluate their cogni-
tive skills early to counteract the potential evolution
of the disease (Albert et al., 2011; Svenningsson et al.,
2012). Usually, specialists in areas such as neuropsy-
chology, map a neuropsychological profile by per-
forming examinations to evaluate the patient’s cog-
nitive skills (Harvey, 2012; Yi and Belkonen, 2011).
Following this assessment, they usually establish an
individualized rehabilitation plan (IRP) for cognitive
therapy (CT). This data can also help doctors identify
the disease and its stage of development, and to pre-
scribe appropriate pharmaceuticals. The IRP should
result in a series of restorative and compensatory ther-
apeutic activities that can help the elder rehabilitate
functions or delay the development of the disease.
It is well established that therapies should start as
early as possible, before the brain loses its plastic-
ity, especially with the progression of neurodegener-
ative diseases (Choi and Twamley, 2013; Clare et al.,
292
Silva, R. and Menezes, P.
SAR-ACT: A Spatial Augmented Reality Approach to Cognitive Therapy.
DOI: 10.5220/0010322802920299
In Proceedings of the 16th International Joint Conference on Computer Vision, Imaging and Computer Graphics Theory and Applications (VISIGRAPP 2021) - Volume 1: GRAPP, pages
292-299
ISBN: 978-989-758-488-6
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

2019; Niu et al., 2010). IRPs should include tasks
that stimulate the brain in the affected areas and de-
lay cognitive decline. They should propose methods
to cope with areas where faculties are limited, pro-
moting strategies for enduring plausible advances of
the disease, ensuring patient’s autonomy for as long
as possible.
Serious Games (SGs) can play the necessary ther-
apeutic roles by providing stimuli that aim at sus-
taining executive functions, including visual process-
ing, working memory, attention, language, and ver-
bal communication. Board-, card-, and computer-
based activities can be designed purposely to attain
these therapeutic goals while simultaneously trying to
engage the patients through the exploration of game
principles (Kueider et al., 2012; Lamb et al., 2018;
Peretz et al., 2011; Rocha et al., 2015). Recent
works have explored emerging technologies such as
virtual, augmented and mixed reality (VR, AR, MR)
in this area, intending to bring new tools to the path
of CT (Ferreira and Menezes, 2020a; Ferreira and
Menezes, 2020b; Gamberini et al., 2009; Grealy et al.,
1999; Kirner and Kirner, 2011).
While VR and AR offer great possibilities, the use
of head-mounted devices may lead to discomfort and
rejection by some people. More ecologic approaches
may be achieved with the use of Spatial Augmented
Reality (SAR) principles, integrating, in a naturalis-
tic way, computer-generated graphics with the users’
own physical space, by the use of video mapping tech-
niques (Bimber and Raskar, 2005). Using it, existing
objects can be hidden, highlighted, or have their ap-
pearance modified to fulfill the game’s objectives.
This work comes inline with the above and pro-
poses a framework to support the development of
SAR-based Serious Games for cognitive stimulation.
1.1 Paper Structure
The remainder of this paper is organized as follows:
Section 2 presents an overview of the research con-
ducted in more conventional and recent works in the
area of SGs for CT; section 3 describes a summary of
the process for designing an SG for CT, the challenges
and requirements that are taken into account for out-
lining its development, and illustrates the framework
concept, its development and implementation; section
4 demonstrates the SGs built, describes their function-
ing, and their areas of application. Section 5 com-
prises an overview of a specialist that corroborates the
developed works. A conclusion is made for the po-
tential of the concepts presented through an objective
analysis of the framework and respective SGs built,
comparing them with current and emerging tools for
CT in section 6. In this section, it is also made clear
the intention of future work on this platform.
2 SERIOUS GAMES AND
COGNITIVE THERAPIES
Cognitive exercises frequently simulate everyday
challenges by using various and specific tools (Faria
et al., 2016; Kurz et al., 2009). These tools can pro-
vide stimuli that help patients to relearn the use of
their lost or degrading abilities. As for every learning
process, it requires consistent repetitions with slight
variations of the same activities (Jeffrey A. Kleim and
Jones, 2008). The repetitive nature of the exercises
and the slow recovery often lead to frustration and
tediousness. Therefore, patients can become unmo-
tivated and unwilling to keep up with therapies.
Unsurprisingly, CT’s effectiveness is affected by
the patient’s capacity to endure his assigned exer-
cises (Choi and Twamley, 2013). The main obsta-
cle in developing tools for CT resides in finding two
balances: keeping an acceptable challenge threshold
that induces evolution in players performance while
not being frustrating enough to demotivate, and using
mechanisms in game design to lessen the impact of
repetition in therapeutic tasks, keeping the player en-
gaged and entertained (Burke et al., 2009). By main-
taining the patient engaged, these tools will help the
therapist become free to focus on other aspects, such
as assessing performance evolution and planning the
subsequent exercises. Through the fulfilment of these
objectives, the role of a therapeutic tool is then ac-
complished, and its application will promote the ef-
fectiveness of the IRP.
The design of the SG for CT, for the reasons de-
tailed above, is a crucial stage of development. When
idealising a game, the developer should focus on one
or more of the cognitive deficits it will address. To en-
sure development will result in useful tools, a strategy
may be to base the project on existing certified tools
for the intended therapeutic purpose. Then, new cre-
ative outlooks can be added through new technologies
while keeping the target at the requirements.
Since the patients’ conditions can be varied, their
IRPs can be considerably different even for the same
diseases. It can be challenging for therapists to find
tools that adapt to each specific patient’s needs. By
taking advantage of modern tools, when designing an
SG, one should concentrate on adaptability, customi-
sation, and personalisation (Burke et al., 2009; Faria
et al., 2018). The bigger the granularity of the change-
able elements of the SG is, the easier it will be to adapt
to different IRPs, and the more will it suit each pa-
SAR-ACT: A Spatial Augmented Reality Approach to Cognitive Therapy
293

Figure 1: Sgs’ iterative cycle.
tient’s performance and evolution (Burke et al., 2009;
Tong et al., 2014). With specific personalisation of the
game, by including components of the patient’s life,
like personal objects, or recognisable faces or places,
one can assure that the player will gain some level
of ownership over the therapeutic activities and, this
way, achieve higher levels of engagement and moti-
vation (Faria et al., 2018).
The concept of SGs as therapeutic tools also pro-
poses the gamification of therapy to achieve better
entertainment, engagement, motivation, and a sense
of progression. The developer should adopt elements
from traditional game principles like score, time, dif-
ficulty, and levels. These components can also help
adapt the game to the player and translate their per-
formance while doing therapy. For example, the ther-
apist can specify a game, its difficulty level, and other
parameters for a patient to play during a therapy ses-
sion. Afterward, by analysing the attained score and
execution time, it is possible to infer about perfor-
mance and/or recovery. This way, the SG promotes
changeable iterations of therapy sessions that will
consecutively adapt to the patient’s condition.
To keep players captivated while interacting with
the game, the interface may provide visual and au-
dio stimulus, but their inclusion must be carefully
analysed to make sure they enable the intended
goals. Therefore, a cycle of playing, giving feedback,
analysing performance, and adapting the game is crit-
ical to keep in mind the objectives while establishing
the game design, as portrayed in Figure 1. To allow
every type of person to use it, the game should be flex-
ible and customisable as much as possible. To this
end, it is important to avoid complex control schemes
and dynamics that would be hard to tune or adapt by
the therapist or caregiver.
3 PROPOSING A SAR-BASED
FRAMEWORK FOR CT
From the above, and approaching the available tech-
nological solutions for developing tools supporting
cognitive therapies, spatial augmented reality appears
as an interesting candidate. Contrary to other tech-
nologies, in SAR interfaces the user can benefit from
a wide field of view, and the interaction with the en-
vironment can be made through the handling of phys-
ical objects. Since elderly citizens are most likely not
used to computer interfaces, SAR can present a valid
alternative by replacing accessories like keyboards,
computer mice, HMDs, smartphones or tablets with
real objects that are more familiar to the user. This
particular factor highlighted a great opportunity: to
upgrade the use of common therapeutic card games
with SAR.
By creating a framework that enables and expe-
dites the creation of projection-based serious games
for cognitive therapy for elders, developers can fo-
cus on creating engaging, customizable, and adaptive
environments to enhance therapy effectiveness. This
idea led to the solution proposed in this document, for
which the next section presents the concept and iden-
tified requirements.
3.1 Concept and Requirements
By using a contemporary outlook at a familiar task,
patients can become more captivated in therapy. Con-
sidering they are already used to these objects and
their manoeuvrability, their adaptation process to the
game should be more straightforward. Ideally, by pro-
viding stated benefits, both cognitive stimuli and ther-
apy efficiency can be improved.
The interaction of the SAR Cards Framework
works in the following way:
1. The user will manipulate cards in the projection
area;
2. Cards’ locations are tracked by the system;
3. Projections are adapted based on cards’ locations
and game rules/objectives;
4. Interface provides visual and sound feedback
based on player performance;
5. When the session ends, the player
score/performance is recorded.
A global overview of the SAR Card framework
functionality can be seen in Figure 2.
Given the overall concept of the framework and the
design considerations stated in the previous sections,
the following requirements were defined for the de-
velopment of the framework:
GRAPP 2021 - 16th International Conference on Computer Graphics Theory and Applications
294
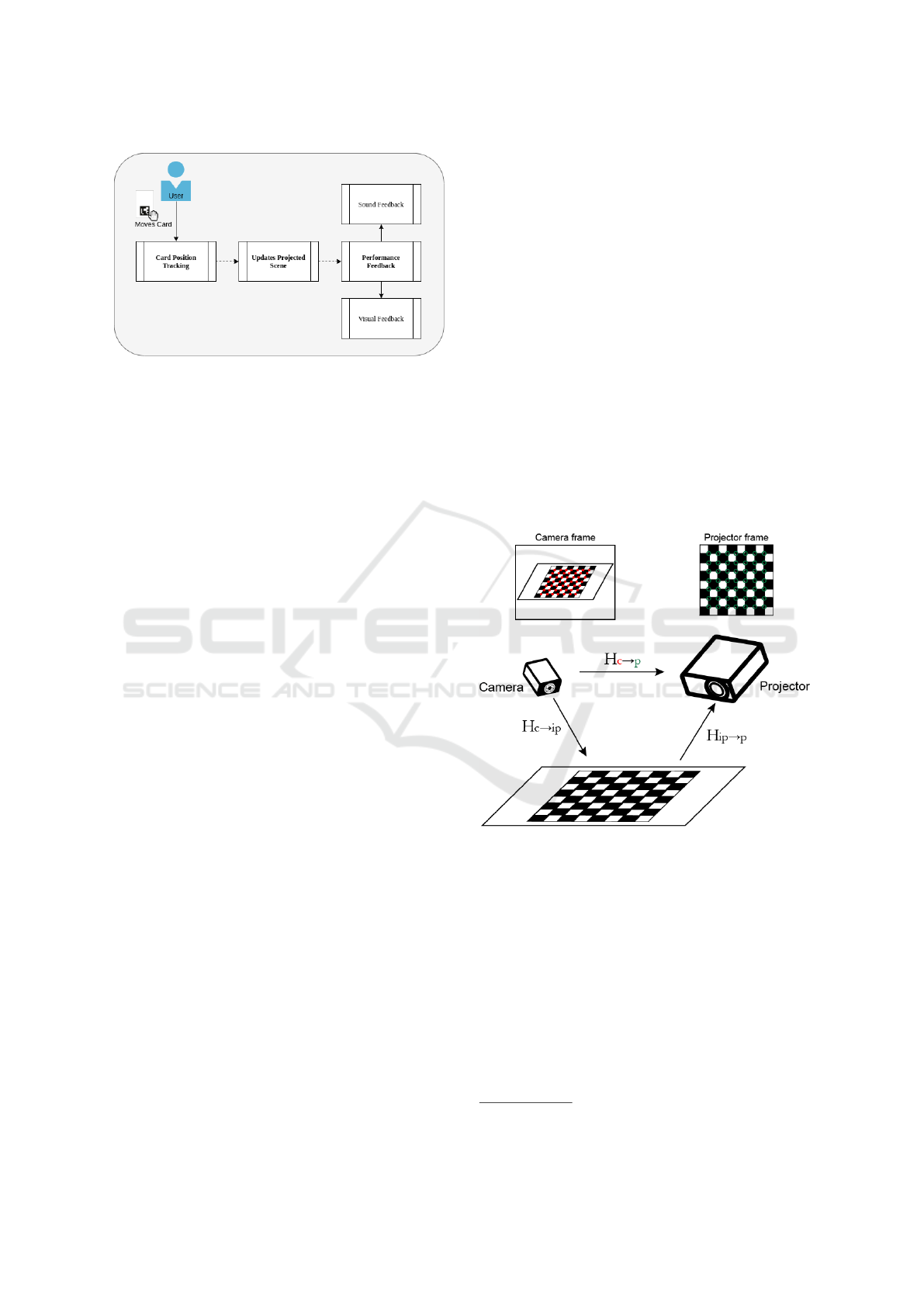
Figure 2: Framework functional overview.
• User manipulation of the cards should be analo-
gous to traditional card games;
• The framework must provide ways to measure
user performance in several parameters to encour-
age self-improvement and for the therapist to an-
alyze;
• Player interactions with the system are made ex-
clusively with cards;
• Inclusion of functionalities to enhance adaption to
the player’s needs;
• Deliver visual and sound feedback to signal if the
user is doing well;
• The system should be flexible and expansible to
promote the development of several types of SGs.
3.2 Implementation
The basic elements required to build a SAR system
are a camera and a video projector. By inquiring about
the logistical aspects of an installation of this kind, it
was concluded that it is common for therapy centres
and assisted living facilities to already own these de-
vices for other purposes, which facilitates the deploy-
ment of the system at reduced cost.
To create the illusion of virtual images registered to
physical cards, the following run-time steps are re-
quired:
1. Obtain cards’ location in the camera’s frame
(tracking stage);
2. Translate their locations to the projector’s frame;
3. Adapt the corresponding images for skewness
(mapping stage);
4. Generate a frame of adapted images in their loca-
tions;
5. Project over the cards in the area of the game, here
defined as the interaction planar surface (IPS).
Firstly, a calibration step is made to retrieve the
relationship between three planar surfaces: the cam-
era’s frame, the interaction planar surface (IPS) and
the projector’s frame. This calibration process con-
sists in capturing the projection of a chessboard pat-
tern onto the IPS from the camera’s point of view
(POV).
It was chosen to use a chessboard pattern due to its
regular geometry that allows robust and accurate fea-
ture extraction. OpenCV
1
library was used to extract
the position of the corners in the camera’s and pro-
jector’s frames, and to establish a correspondence be-
tween projector and camera frames. This correspon-
dence is obtained in a compact form as a homogra-
phy matrix. This relationship also encompasses the
relation of both of them with the IPS. A diagram of
the projective transformations is presented in Figure
3. With these relations defined, for every point in
the physical IPS delimited by the projection area, it
is possible to find its approximate projection on both
the frames of the projector and camera.
Figure 3: Homographies between planar surfaces.
To track the locations of the cards in the game
environment in a quick and flexible manner, each
of them received fiducial markers. For the sake
of simplicity the fiducial markers choice fell on
ARUco (Romero-Ramirez et al., 2018) as their sup-
port is readily available. Besides the markers, the
cards have a blank area used for the projection of im-
ages as described hereafter.
The overall process cycle is as follows:
1. Track cards marker corners positions (X
c
, Y
c
) in
the camera’s frame;
1
https://opencv.org/
SAR-ACT: A Spatial Augmented Reality Approach to Cognitive Therapy
295

2. Transform corners positions to the projector’s
frame (X
p
, Y
p
) (using the matrix H
c→p
obtained in
the calibration stage);
3. Find the perspective transformation between each
marker’s corners of a flat source image of a card
(in pixels) and the correspondent corners in the
projector’s frame;
4. Warp the image to be projected respecting the
found perspective transformation matrix;
5. Add it to the projector’s frame in its correct posi-
tion.
The result will be an overlay image projected onto
the cards disposed on the IPS. This enables that the
projection be perfectly adapted to any moving card,
even if tilted. The projection of the image on a spe-
cific card is only stopped if its marker becomes ob-
structed in the camera view. The setup used to imple-
ment the SAR environment can be observed in Fig-
ure 4. Figure 5 shows a diagram of the complete pro-
cessing pipeline.
Figure 4: Setup used to implement SAR SGs.
4 DEVELOPED GAMES
To demonstrate the applicability of the framework,
two SGs were implemented. These games were based
on established therapeutic tools, and several features
were added to cater to patient’s needs, while the per-
formance of the player was tracked through the use of
game metrics such as score, difficulty and time. The
games were integrated into a web platform (composed
by a database and a website), to provide therapists
with a straightforward way to check on the perfor-
mance development of each patient’s case and decide
how to adapt the next therapeutic tasks.
4.1 SAR Cards Memory Game
Memory card-based games are frequently used as a
tool for CT (Muragaki et al., 2006). Hence, it was
decided to build an enhanced version using SAR.
The patient starts with all the cards facing down
on a table (IPS) and has to find all the matching pairs.
The player flips cards up one at the time trying to find
a pair, if it is a wrong pair, the last two cards have to
be flipped down again, if the pair is correct, the cards
remain face-up, and the player can proceed to find the
next pair. This process is repeated until all the pairs
are found. The game is adaptable in the following
ways:
• The number of cards is dynamic: the more cards,
the harder is the game;
• The images that appear on cards can be com-
pletely customised: this allows us to build many
types of games. E.g. cards appear with pictures
of places, colours, animals, fruits, vegetables, fa-
miliar faces, emotions, and the patient has to find
matching pairs; cards appear with names of fa-
miliars or personal objects, and the players have
to find the card with the corresponding image;
• The game also has an option for providing initial
help, where the player sees which images are on
each card before turning them down.
While the player interacts with the game, the in-
terface provides positive and negative feedback in the
form of visuals and sound.
When the game ends (all pairs found), a celebra-
tory screen is shown with the player’s score. The
score embodies the number of cards (more is better)
and time of completion (less is better) used in that
session.
The images, the number of cards and help mode
should be controlled by the therapist. After finishing
a CT session, the scores, time, and number of tries
are sent to the web platform for posterior analysis. A
demonstration of this SG is showed in Figure 6.
4.2 SAR Cards Pong Game
Pong was one of the first video-games created, and,
from an early stage, its application for cognitive reha-
bilitation was studied. This study helped to introduce
the concept of SGs for CT (Lynch, 1982).
The objective of the game is to score goals, throw-
ing the ball through the defence line of the other
player while defending our line by bouncing the ball
back with the paddle. The game starts with the ball in
the middle of the field and goes into a random direc-
tion, the ball is reset to this position after a goal. A
GRAPP 2021 - 16th International Conference on Computer Graphics Theory and Applications
296
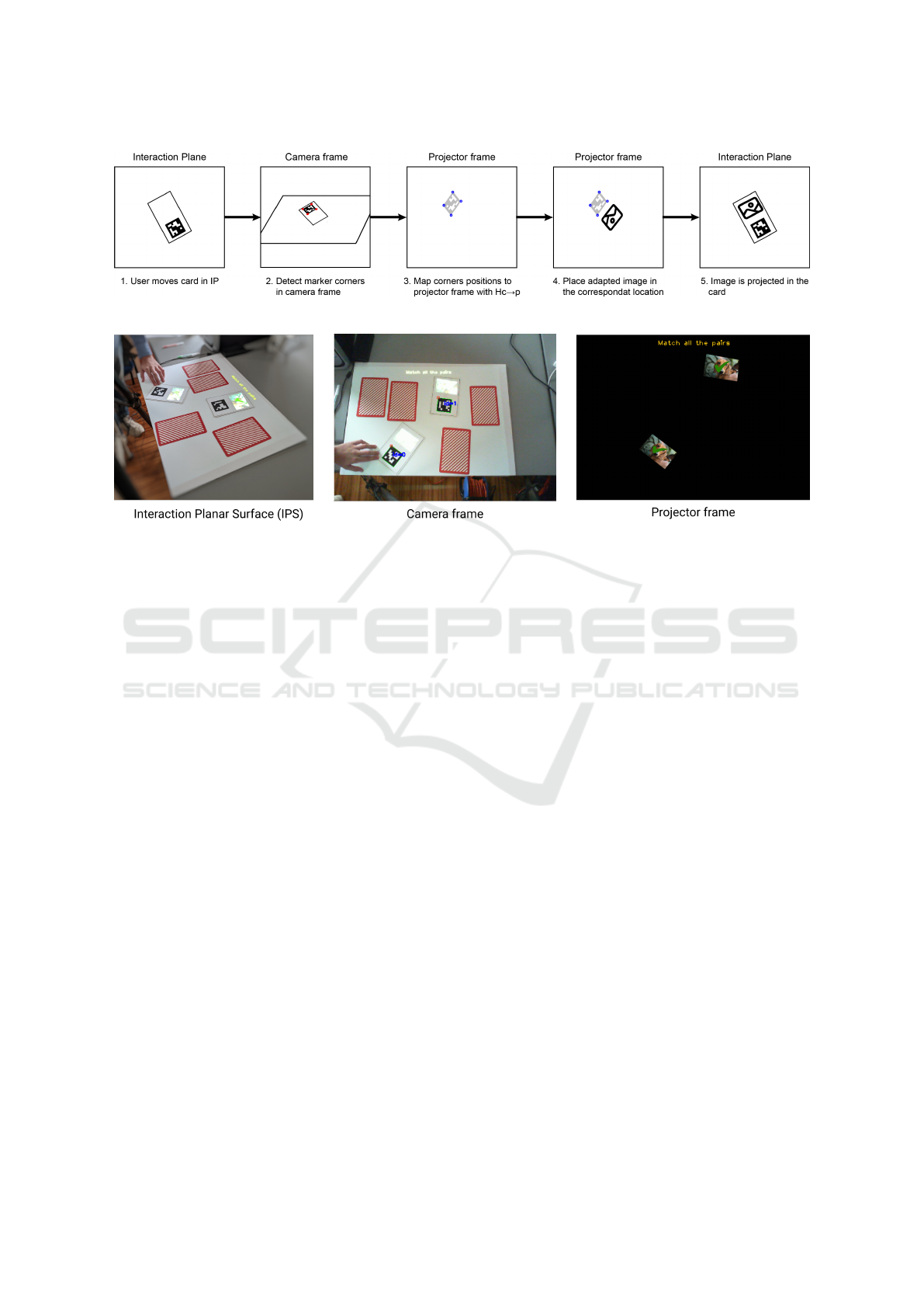
Figure 5: SAR Cards Framework pipeline.
Figure 6: SAR Cards Memory Game demonstration.
SAR implementation of the game was developed us-
ing the framework, where the player controls its pad-
dle position by moving the card vertically in the IPS.
The game-play focuses on the attention span, re-
action speed and spatial awareness of its patients as it
forces the patient to watch, react and predict the tra-
jectory of the ball. The game can be played alone or
with another player (being the therapist, caregiver or
family member/friend). Multiplayer mode can be an
incentive to play since it can be engaging for the pa-
tient to be accompanied while doing therapy.
The therapist can set the following adaptation fac-
tors:
• Game mode: solo or multiplayer;
• Velocity: the velocity of the ball;
• Bounce dynamics: simple or complex;
• Duration of the game: points or time required to
win the match.
The game provides distinct visual and sound feed-
back of the bounces in the walls, paddles, when there
is a goal and when a match is won. The score, the au-
thor of the goal and winner of the match, is presented
on the IPS in textual form. At the end of a match, the
scores, duration, and number of paddle hits are sent to
the platform so they can be analyzed. A demonstra-
tion of this SG is showed in Figure 7.
4.3 Patient Performance Interface
The games were integrated into a therapy SG perfor-
mance analysis web platform. This platform allows us
to download the right therapy parameters for the right
patient and upload the results of each session. The
results are presented with graphs comparing sessions
for more accessible analysis (Figure 8).
5 ANALYSIS
The design principles, requirements, framework, and
the SGs for CT developed were reviewed during and
after the development process by a Superior Educa-
tion Technician. The demonstrated results received
positive feedback. The reviewer considered that the
objectives set for this work were accomplished from
the point of view of the therapist. In her opinion, the
SGs created with the framework show promising fea-
tures that can possibly help in the effectiveness of CT.
Thus, there should be made experiments with patients
in a real therapeutic environment to test the effective-
ness of this SGs. By the specialist’s perspective, only
with real patient-therapist experience, we will gather
information to adapt the SGs to elders’ needs.
SAR-ACT: A Spatial Augmented Reality Approach to Cognitive Therapy
297

Figure 7: Pong game demonstration.
(a) (b)
Figure 8: Login authentication of therapist (a), and patient performance data (b). Created in (Omitted, 2019).
6 CONCLUSION AND FUTURE
WORK
In this paper, we took from the traditional games used
to train cognition in CT and added features to enhance
adaptability, personalization, engagement and perfor-
mance tracking. These features were implemented
through the use of SAR. This technology requires
only a video-projector, a camera, and makes use of the
familiar physical space of its user. By only using these
components, we highlight the benefits of this type of
system when comparing it with more expensive or
cumbersome methods like AR or VR. It was devel-
oped a framework that makes use of SAR for creat-
ing SGs to facilitate cognitive stimulus. The target
audience was older adults that suffer from cognitive
impairments. Two SGs with different cognition tar-
gets were built to test the framework application. The
games were analysed by a specialist who gave a posi-
tive feedback and reinforced the idea that these games
need to be tested with patients in a real-world con-
text. This feedback assures us that our work reveals
promising results to create new CT tools. The next
step will be to study its impact on a small group of
patients to confirm if these benefits translate to more
effective therapy. It will also be interesting to study
if non-cognitive-deficient elders can benefit from this
type of tool.
REFERENCES
Albert, M. S., DeKosky, S. T., Dickson, D., Dubois, B.,
Feldman, H. H., Fox, N. C., Gamst, A., Holtzman,
D. M., Jagust, W. J., Petersen, R. C., Snyder, P. J.,
Carrillo, M. C., Thies, B., and Phelps, C. H. (2011).
The diagnosis of mild cognitive impairment due to
Alzheimer’s disease: Recommendations from the
National Institute on Aging-Alzheimer’s Association
workgroups on diagnostic guidelines for Alzheimer’s
disease. Alzheimer’s and Dementia, 7(3):270–279.
Bimber, O. and Raskar, R. (2005). Spatial Augmented Re-
ality Merging Real and Virtual Worlds. Technical re-
port.
Burke, J. W., McNeill, M. D., Charles, D. K., Morrow, P. J.,
Crosbie, J. H., and McDonough, S. M. (2009). Opti-
mising engagement for stroke rehabilitation using se-
rious games. Visual Computer, 25(12):1085–1099.
Choi, J. and Twamley, E. W. (2013). Cognitive rehabili-
tation therapies for Alzheimer’s disease: A review of
methods to improve treatment engagement and self-
efficacy. Neuropsychology Review, 23(1):48–62.
Clare, L., Kudlicka, A., Oyebode, J. R., Jones, R. W.,
Bayer, A., Leroi, I., Kopelman, M., James, I. A.,
Culverwell, A., Pool, J., Brand, A., Henderson, C.,
Hoare, Z., Knapp, M., Morgan-Trimmer, S., Burns,
A., Corbett, A., Whitaker, R., and Woods, B. (2019).
Goal-oriented cognitive rehabilitation for early-stage
Alzheimer’s and related dementias: the GREAT RCT
Scientific summary Scientific summary Background.
Health Technology Assessment, 23(10).
Faria, A. L., Andrade, A., Soares, L., and I Badia, S. B.
(2016). Benefits of virtual reality based cognitive re-
GRAPP 2021 - 16th International Conference on Computer Graphics Theory and Applications
298

habilitation through simulated activities of daily liv-
ing: a randomized controlled trial with stroke pa-
tients. Journal of NeuroEngineering and Rehabilita-
tion, 13(1):1–12.
Faria, A. L., Pinho, M. S., and Berm
´
udez I Badia, S. (2018).
Capturing Expert Knowledge for the Personalization
of Cognitive Rehabilitation: Study Combining Com-
putational Modeling and a Participatory Design Strat-
egy. JMIR rehabilitation and assistive technologies,
5(2):e10714.
Ferreira, B. and Menezes, P. (2020a). An Adaptive Vir-
tual Reality-Based Serious Game for Therapeutic Re-
habilitation An Adaptive Virtual Reality-Based Seri-
ous Game for Therapeutic Rehabilitation. Interna-
tional Journal of Online and Biomedical Engineering
(iJOE), 16(04):63–71.
Ferreira, B. and Menezes, P. (2020b). Gamifying Motor Re-
habilitation Therapies: Challenges and Opportunities
of Immersive Technologies. Information 2020, Vol.
11, Page 88, 11(2):88.
Gamberini, L., Martino, F., Seraglia, B., Spagnolli, A., Fab-
regat, M., Ibanez, F., Alcaniz, M., and Andr
´
es, J. M.
(2009). Eldergames project: An innovative mixed re-
ality table-top solution to preserve cognitive functions
in elderly people. In Proceedings - 2009 2nd Confer-
ence on Human System Interactions, HSI ’09, pages
164–169. IEEE Computer Society.
Glisky, E. L. (2019). Changes in Cognitive Function in Hu-
man Aging. In Brain Aging, pages 3–20. CRC Press.
Grealy, M. A., Johnson, D. A., and Rushton, S. K. (1999).
Improving cognitive function after brain injury: The
use of exercise and virtual reality. Archives of Physi-
cal Medicine and Rehabilitation, 80(6):661–667.
Harvey, P. D. (2012). Clinical applications of neuropsy-
chological assessment. Dialogues in Clinical Neuro-
science, 14(1):91–99.
Jaul, E. and Barron, J. (2017). Age-Related Diseases and
Clinical and Public Health Implications for the 85
Years Old and Over Population. Frontiers in Public
Health, 5.
Jeffrey A. Kleim and Jones, T. A. (2008). Principles
of Experience-Dependent Neural Plasticity: Implica-
tions for Rehabilitation After Brain Damage. Journal
of Speech, Language, and Hearing Research.
Kirner, C. and Kirner, T. G. (2011). Development of an in-
teractive artifact for cognitive rehabilitation based on
augmented reality. In 2011 International Conference
on Virtual Rehabilitation, ICVR 2011.
Kueider, A. M., Parisi, J. M., Gross, A. L., and Rebok,
G. W. (2012). Computerized Cognitive Training with
Older Adults: A Systematic Review. PLoS ONE,
7(7):e40588.
Kurz, A., Pohl, C., Ramsenthaler, M., and Sorg, C. (2009).
Cognitive rehabilitation in patients with mild cogni-
tive impairment. International Journal of Geriatric
Psychiatry, 24(2):163–168.
Lamb, R. L., Annetta, L., Firestone, J., and Etopio, E.
(2018). A meta-analysis with examination of mod-
erators of student cognition, affect, and learning out-
comes while using serious educational games, serious
games, and simulations. Computers in Human Behav-
ior, 80:158–167.
Lynch, W. J. (1982). The Use of Electronic Games in
Cognitive Rehabilitation. In Cognitive Rehabilitation,
pages 263–274. Springer US.
Max Roser, E. O.-O. and Ritchie, H. (2013). Life Ex-
pectancy. Our World in Data.
Mioshi, E., Kipps, C. M., Dawson, K., Mitchell, J., Gra-
ham, A., and Hodges, J. R. (2007). Activities of daily
living in frontotemporal dementia and Alzheimer dis-
ease. Neurology, 68(24):2077–2084.
Muragaki, C. S., Okamoto, K. H., Furlan, L., Toldr
´
a, R. C.,
Dunlop, J. B., and Sp, C. (2006). A utilizac¸
˜
ao de
jogos pela terapia ocupacional: Contribuic¸
˜
ao para a
reabilitac¸
˜
ao cognitiva. Technical report.
Niu, Y.-X., Tan, J.-P., Guan, J.-Q., Zhang, Z.-Q., and
Wang, L.-N. (2010). Cognitive stimulation ther-
apy in the treatment of neuropsychiatric symptoms in
Alzheimer’s disease: a randomized controlled trial.
Clinical Rehabilitation, 24:1102–1111.
Omitted (2019). Technical report.
Peretz, C., Korczyn, A. D., Shatil, E., Aharonson, V., Birn-
boim, S., and Giladi, N. (2011). Computer-based,
personalized cognitive training versus classical com-
puter games: A randomized double-blind prospec-
tive trial of cognitive stimulation. Neuroepidemiology,
36(2):91–99.
Robine, J. M., Saito, Y., and Jagger, C. (2009). The relation-
ship between longevity and healthy life expectancy.
Quality in Ageing, 10(2):5–14.
Rocha, R., Reis, L. P., Rego, P. A., and Moreira, P. M.
(2015). Jogos S
´
erios na Reabilitac¸
˜
ao Cognitiva:
Modalidades de Interacc¸
˜
ao e Componente Social. In
2015 10th Iberian Conference on Information Systems
and Technologies, CISTI 2015. Institute of Electrical
and Electronics Engineers Inc.
Romero-Ramirez, F. J., Mu
˜
noz-Salinas, R., and Medina-
Carnicer, R. (2018). Speeded up detection of squared
fiducial markers. Image and Vision Computing,
76:38–47.
Svenningsson, P., Westman, E., Ballard, C., and Aarsland,
D. (2012). Cognitive impairment in patients with
Parkinson’s disease: Diagnosis, biomarkers, and treat-
ment.
Tong, T., Chignell, M., Lam, P., Tierney, M. C., and Lee, J.
(2014). Designing Serious Games for Cognitive As-
sessment of the Elderly.
United Nations Department of Economic and Social Affairs
of the United Nations (2004). WORLD POPULA-
TION TO 2300. Technical report, Department of Eco-
nomic and Social Affairs of the United Nations, New
York.
Yi, A. and Belkonen, S. (2011). Neuropsychological Reha-
bilitation. In Encyclopedia of Clinical Neuropsychol-
ogy, pages 1766–1767. Springer New York.
SAR-ACT: A Spatial Augmented Reality Approach to Cognitive Therapy
299
