
SeVA: An AI Solution for Age Friendly Care of Hospitalized
Older Adults
Chongke Wu
1
, Jeno Szep
1
, Salim Hariri
1
, Nimit K. Agarwal
2
, Sumit K. Agarwal
2
and Carlos Nevarez
3
1
NSF Center for Cloud and Autonomic Computing, The University of Arizona, Tucson, Arizona, U.S.A.
2
Department of Medicine, Banner, University Medical Center Phoenix, Phoenix, Arizona, U.S.A.
3
SevaTechnology LLC, Tucson, Arizona, U.S.A.
cwildhorse@gmail.com
Keywords: Artificial Intelligence, Chatbot, Healthcare, Patient Monitoring, Delirium, Internet of Things.
Abstract: As a dangerous syndrome, delirium affects more than 50% of hospitalized older adults and has an economic
burden of 164 billion US dollars per year. It is crucial to prevent, identify and treat this syndrome
systematically on all hospitalized patients to prevent its short and long-term complications. Currently, there
are no AI-based tools being utilized at a large scale focused on delirium management in hospital settings. The
advancement of the Internet of Things in the medical arena can be leveraged to help clinical teams managing
the care of patients in the hospital. The renaissance of Artificial Intelligence brings the chance to analyze a
large amount of monitoring data. Deep neural networks like Convolutional Neural Network and Recurrent
Neural Network revolutionize the fields of Computer Vision and Natural Language Processing. Deep learning
tasks like action recognition and language understanding can be incorporated into the routine workflow of
healthcare staff to improve care. By leveraging AI and deep learning techniques, we have developed a chatbot
based monitoring system (that we refer to as SeVA) to improve the workload of the medical staff by using an
Artificial Emotional Intelligence platform. The SeVA platform includes two mobile applications that provide
timely patient monitoring, regular nursing checks, and health status recording features. We demonstrate the
current progress of deploying the SeVA platform in a healthcare setting.
1 INTRODUCTION
Delirium affects more than 25% of hospitalized
patients and can be seen in more than 50% of
hospitalized older adults, impacting long-term
survival, and quality of life (Marcantonio, 2017). The
continuous and objective monitoring of delirium
similar to blood pressure checks can help medical
staff identify, prevent, and treat delirium and its many
compilations.
The Internet of Things (IoT) technology has the
potential of improving healthcare quality. It
empowers clinicians (physicians and nurses) to
review vast amounts of clinical data efficiently and
meaningfully for clinical decision making by
improving their workflows. Xu et al. present an IoT-
based system for emergency medical service by
providing data access timely and ubiquitously in a
cloud and mobile computing platform (Yu, Beam,
and Kohane, 2018).
As healthcare systems increasingly adopt
Artificial Intelligence (AI) in their decision making,
we are seeing a renaissance of AI in the field of
Healthcare. For example: in the case of patient
monitoring in the intensive care unit or emergency
rooms, an AI-assisted alert system can be helpful to
process a large amount of data generated by routine
monitoring devices (Xu et al., 2014). The vital signs
and Modified Early Warning Score systems can be
used to build a prediction model for cardiac arrest
(Churpek et al., 2012; Szep, Akoglu, Hariri, &
Moukabary, 2018).
The advancement of Natural Language
Processing makes it possible to create an expert
knowledge system to provide ubiquitous service.
Microsoft released the Healthcare Bot service to
empower healthcare organizations to build and
deploy the conversational health care experience at
scale (Microsoft, 2020). It combines medical
intelligence with natural language capabilities. The
Wu, C., Szep, J., Hariri, S., Agarwal, N., Agarwal, S. and Nevarez, C.
SeVA: An AI Solution for Age Friendly Care of Hospitalized Older Adults.
DOI: 10.5220/0010313605830591
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 5: HEALTHINF, pages 583-591
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
583

IBM question-answering computer system Watson is
utilized to help physicians with the treatment of
patients as a “diagnosis and treatment advisor” (IBM,
2020). Extracting the knowledge broadly and
returning the results promptly is an inherent feature
of the AI healthcare knowledge engines. It provides a
significant advantage compared to traditional medical
processes, especially in areas with limited medical
resources.
Healthcare data is very sensitive and requires
security protection. Secure identification is one of the
measures to mitigate the risk of identity theft.
Pacheco et al. propose an IoT security framework for
smart infrastructures against cyber-attacks (Pacheco
and Hariri, 2016). When conducting user group
estimation, local differential privacy can protect user
information without the assumption of the trusted
data server (Gu, Li, Cao, and Xiong, 2019;Gu, Li,
Cheng, Xiong, and Cao, 2020).
By analyzing data coming from monitored
patients we can create a system that can respond to
patient's needs in a timely manner. In this paper, we
present an Age-Friendly patient care platform
connecting seniors, caregivers, healthcare, and
community by leveraging AI and ML techniques:
SeVA (Senior’s Virtual Assistant). With the support
of a Natural Language Processing platform, the SeVA
platform achieves real-time and continuous
monitoring of the patient status as well as capturing
patient intent from the human-computer interactions.
The remaining sections of the paper are organized
as follows: Section II introduces the related research
of artificial intelligence application in the medical
field; In section III, we present the system design of
the SeVA platform; Section IV shows the
implementation details of the platform; Section V
summarizes the work in this paper and discusses
future research plan.
2 BACKGROUND AND RELATED
RESEARCH
2.1 Delirium: Insidious and Dangerous
Syndrome
Delirium is a dangerous syndrome commonly seen in
hospitalized patients. More than half of hospitalized
older adults (> 65 years of age) are affected (around
7 million patients annually) and most of them remain
undiagnosed. Delirium in hospitalized patients leads
to higher hospital length of stay, higher mortality rate,
loss of physical function requiring long term care, and
can even be a precursor to dementia. It costs more
than 164 billion US dollars per year to healthcare
(Inouye et al., 2016). There is no mandatory
prevention program as well as no reporting to the
Centres of Medicare & Medicaid Services (CMS). As
a comparison, around 24 billion dollars are lost due to
sepsis, and every hospital carries a mandatory sepsis
alert program and pathway (Paoli, Reynolds, Sinha,
Gitlin, & Crouser, 2018). The data for sepsis is also
reported to CMS as an adverse event. The gaps in
delirium care include delayed recognition, inadequate
risk modification and prevention, and ineffective
treatment. The major reason for this is the lack of a
standardized multidisciplinary approach for the
management of delirium across hospital systems. The
Hospital Elder Life Program (HELP) developed by
Inouye is a system that relies on volunteer healthcare
workers to engage patients (Inouye et al., 1999);
however, it has only been implemented in a few
hospitals. There certainly is a need for a system that
can be easily implemented, customized and is
scalable across all hospitals that can provide timely
screening, assessment, and recognition, so that the
cause or precipitating factors for delirium can be
removed, and the patient can receive appropriate and
early treatment.
2.2 Gaps in Patient Monitoring
Despite best efforts by nursing staff in hospital
systems, to decrease the risk of falling, management
of uncontrolled pain, even addressing basic patient
needs like using the bathroom, can be easily missed.
For the patient who has cognitive impairment either
as delirium or dementia, this risk becomes even more
profound. Best nursing practices include a systematic
approach to addressing these care needs, e.g.
performing timed nurse rounding checks or checking
for the 4 Ps (Pain, Position, Potty, Periphery).
However, these practices require dedicated nursing
staff and strict protocols which can be difficult to
implement at a large scale due to limited resources
and cost issues. The “Unsupervised Care Windows”
created due to lack of these practices or between the
hours of timed nurse rounding can lead to serious
events like falls. Patient falls have an enormous cost
on the healthcare system according to the data
reported by the National Database of Nursing Quality
Indicators (NDNQI) (AHRQ, 2020; Mitchell,
Lavenberg, Trotta, and Umscheid, 2014).
Prevention of these adverse events by integrating
technology for the detection of unexpected patient
behaviors like unintended falls is the subject of
significant research over the last several years.
HEALTHINF 2021 - 14th International Conference on Health Informatics
584
Various detection systems have been developed and
can be broadly divided into wearable based, non-
wearable based, and fusion-based systems (Chaccour,
Darazi, El Hassani, and Andres, 2016).
The wearable based systems can be placed on
different body parts like feet, knee, waist, etc. To
measure the body motion parameters like
acceleration, the sensors must be tied to the body. The
typical sensors include accelerometer, gyroscope,
magnetometer, etc. With the universal acceptance of
mobile devices, the smartphone-based solution could
be a very competitive alternative to the conventional
dedicated fall detection and prevention tools (Habib
et al., 2014). The shortcomings of wearable based
systems are that they are relatively inflexible and
uncomfortable.
2.3 AI-based Assistant in Healthcare
Many researchers and companies have introduced
artificial intelligence into their mobile medical
applications to make interactions with the patient
easier. The applications can be further categorized as
healthy lifestyle assistants, remote diagnosis systems,
and medical advisors.
Healthy lifestyle assistant applications will
perform more on disease prevention so that the
suggestion will be more general. Pact Care is a startup
that provides a patient-centric healthcare data
solution. Their mobile product Florence is a chatbot
based personal health assistant with medication
reminders and health trackers. It does not provide
medical advice and is only for personal usage (PACT,
2020). Fadhil et al. propose an AI-chatbot scenario
for healthy lifestyle promotion with nutrition
education and behavior change interventions (Fadhil
and Gabrielli, 2017).
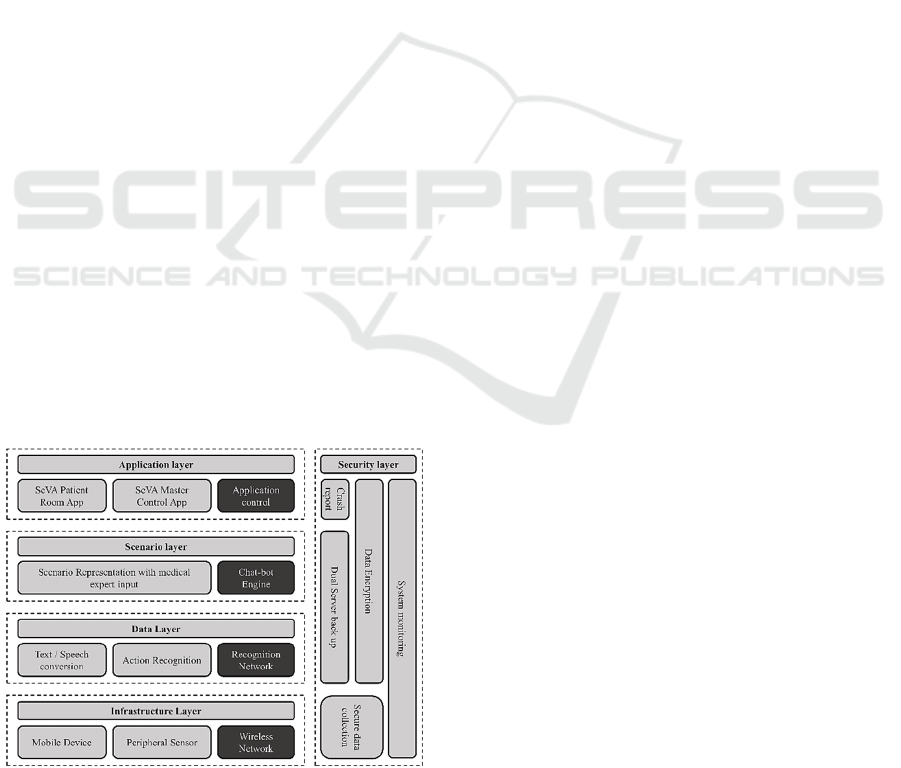
Figure 1: SeVA System Framework.
Remote diagnosis applications will connect the
patient and the physician remotely to mitigate the
medical resource imbalance distribution. The AI part
of the application is focused more on assisting
patients to find the correct doctor. Babylon Health is
a health service provider that offers remote doctor
diagnosis. Their artificial intelligence platform uses a
probabilistic graphical model and natural language
processing to interpret medical questions (Babylon
health, 2020).
Medical advisor applications will give medical
suggestions based on their knowledge base. Buoy
Health makes a digital assistant application that helps
patients self-diagnose and triage for the selection of
appropriate care. The chatbot will ask a series of
medical questions to diagnose customer symptoms
(Buoy Health, 2020). Chung et al. propose a chatbot-
based service with a knowledge base (Chung & Park,
2019). The patient could consult the system with the
picture or text input from the mobile devices. It gives
a fast treatment plan in response to accidents as well
as the change of conditions of a patient with chronic
disease. Comendador et al. develop a pediatric
generic medicine consultant chatbot. It acts as a
medical consultant to suggest generic medicine for
children (Comendador, Francisco, Medenilla, & Mae,
2015).
Our patient care platform SeVA brings the AI
technologies by leveraging Natural Language
Processing and the real-time monitoring of peripheral
sensors. SeVA can be classified as a combination of
the medical advisor and the remote diagnosis system
which is different from the other AI health platforms
which search for often unreliable solutions from the
Internet or other databases, SeVA allows clinicians to
design personalized conversations directly within the
platform. The user interaction in SeVA is easy to use
for older patients who might have limited proficiency
in using technology, or for patients with cognition
issues like dementia or delirium who might not be
able to use plain text-based interactions. It uses
simple gestures like hand waving or simple voice
conversations. This communication mode allows for
the recognition of emotion which can, in turn, allow
interventions like soothing music to mitigate the risk
of delirium. The modular system design provides the
possibility for the integration of additional extra
sensors to accommodates the system in different
environments.
SeVA: An AI Solution for Age Friendly Care of Hospitalized Older Adults
585
3 SYSTEM DESIGN
3.1 SeVA Framework
As shown in Figure 1, the SeVA platform consists of
a five-layer framework: infrastructure layer, data
layer, scenario layer, application layer, and security
layer. This framework provides a general
methodology for building a chatbot-based healthcare
system by utilizing patient real-time data and medical
expert knowledge.
The infrastructure layer provides the basic
hardware requirement of the data collection unit. It
includes the minimum requirement for deploying
SeVA platform to a different environment because
most of SeVA functions are provided as cloud
services. The wireless network block works as a
communication module for real-time data
transmission. The mobile device, such as the tablet or
cell phone, shows the user interface and conducts the
conversation. The peripheral sensor collects patient
movement data to infer the patient's position status
without infringing user privacy. The voice data and
movement data will then be transferred to the upper
layer.
The data layer processes the incoming raw data
from the infrastructure layer. The main task here is
text-to-speech conversion, speech-to-text conversion,
and action recognition. Hence, we need the neural
network as the backbone technique to implement task
functions. For a sequence to sequence problem, the
RNN will provide the majority solution. For the
action recognition which is based on the temporal
movement data, we use a long-short-term memory
neural network to process it. The output of this layer
will be the conversation plain text and the result of the
user action classification.
The scenario layer contains the scenarios provided
by the professional medical expert and returns the
proper conversation to the user. It requires a chatbot
engine to support the scenario representation. More
specifically, the medical expert predefines the
scenario representation with the related incoming
conversation plain text or action class, then it will
provide the conversation and trigger the other
program in the application layer.
The application layer consists of two mobile
applications: the SeVA Patient Room (SPR)
application and the SeVA Master Control (SMC)
application. The first application will work as the
main interface for the patient. It does not only supply
the conversation but also has a predefined workflow
for a regular medical check. The second application
is designed for the medical staff to receive the
notification from the patient room and return quick
feedback to the patient. Behind the user, the mobile
application is the application control system, which is
connected to the SeVA backend server. It manages
the user account database for the authentication
process and controls the communication between
different user applications.
The security layer serves as the auxiliary
component of our system. It protects user data
security and privacy and guarantees SeVA system
robustness. In the infrastructure layer, all the data
collection is compliant with the privacy policy and
with the consent of the user. The data transmission
and storage will be encrypted to guarantee data
confidentiality. We also set up a crash report in the
application layer and system monitoring server to
enable us to achieve a quick response to any
anomalous behavior of the SeVA platform functions.
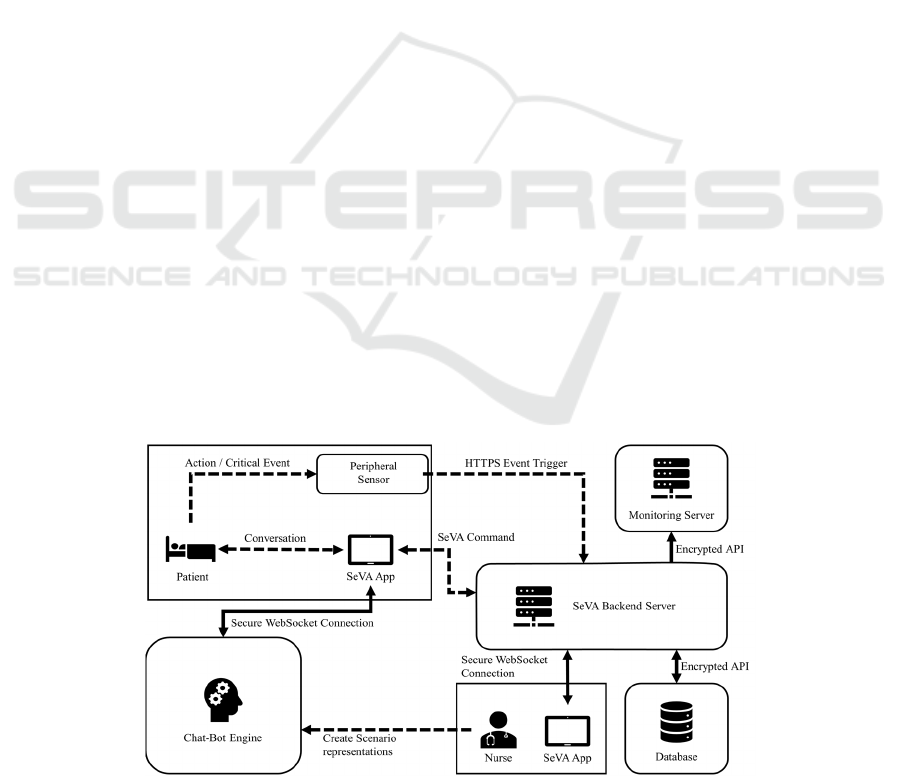
Figure 2: System Architecture of SeVA.
HEALTHINF 2021 - 14th International Conference on Health Informatics
586
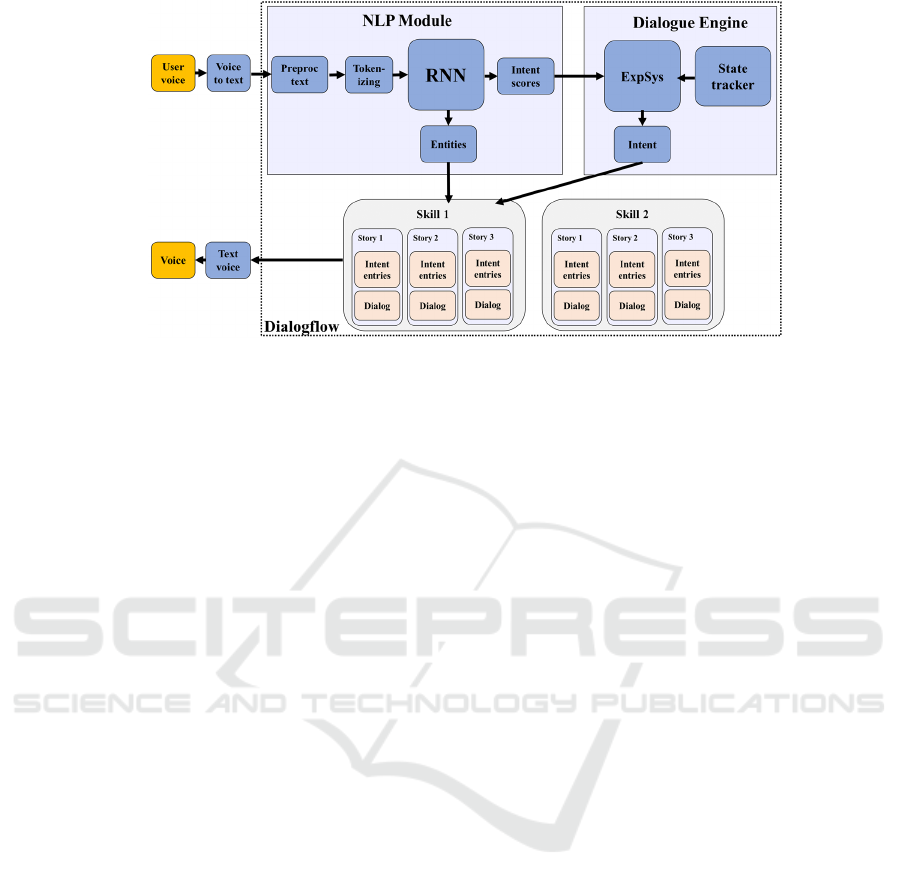
Figure 3: Chatbot Engine skill and story design.
3.2 Components
The SeVA system architecture is shown in Figure 2.
It shows the connection between the main SeVA
components. The arrow represents the information
flow direction. The Chat-bot engine scenario is
defined by the medical staff. Let us consider the
“Waving Hand” event as an example. When a patient
has a request, he/she just waves a hand and then the
peripheral sensor recognizes the action and sends an
HTTPS request to the SeVA backend server. The
request is parsed and fetches the necessary
information, like the room number, from the database
then triggers the chatbot engine to start the
conversation. The SeVA patient room application has
a WebSocket connection with the chatbot engine,
then the conversation will be launched. The
conversation result will be sent to the SeVA backend
server as the format of SeVA Command, which will
be further sent to the SeVA Master Control
application in the nurse room. Then the nurse can
make timely interventions if a critical event happens.
The system running status is monitored by the
Monitoring Server, which guarantees system
reliability.
3.2.1 Peripheral Sensor
We use peripheral sensors to monitor the patient's
status and provide timely interventions in case of any
emergency or critical events. The currently available
sensor is a smart wristband that can detect user
movement sending out the event trigger.
3.2.2 Chatbot Engine
The Chatbot engine architecture is shown in Figure 3.
We build the engine by using the Google NLP
platform Dialogflow. The user's voice is transformed
into plain text and is processed in the NLP module.
The text is first being pre-processed and tokenized,
which result in discrete word and sent to the RNN.
The output of the RNN can be entries, which is the
matching word candidates, or the intent score. The
intent score then is being sent to the expert system
module in a dialogue engine and gives out the final
intent. The intent and the entries serve as the input of
the predefined skills and the skill logic decides the
key content of the conversation. The skill can be
triggered by a request or determined by the intent.
3.2.3 SeVA Backend Server
The SeVA backend server processes the incoming
requests and manages the user data. As a centralized
processing center, it facilitates the management of the
user account as well as providing the API for the
mobile application, database, and monitoring server.
The data sent to the SeVA backend server are
encrypted. When the user tries to use the application,
it must submit the login request to the SeVA backend
server and wait for the authentication token stored in
the database. With the token, it starts the service of
the chatbot engine. The SeVA backend is listening to
the event trigger from the peripheral sensor, which
will be routed to the Chatbot engine to start the
conversation or directly to the SeVA mobile
application.
3.2.4 SeVA Mobile Applications
We have developed two applications: SeVA Patient
Room App (SPR) and SeVA Master Control App
(SMC). As the name indicates, SPR is deployed in the
patient room. SPR uses the Apple built-in Speech
framework for both the Speech-to-Text and Text-to-
Speech conversion. It has the authorization and user
SeVA: An AI Solution for Age Friendly Care of Hospitalized Older Adults
587
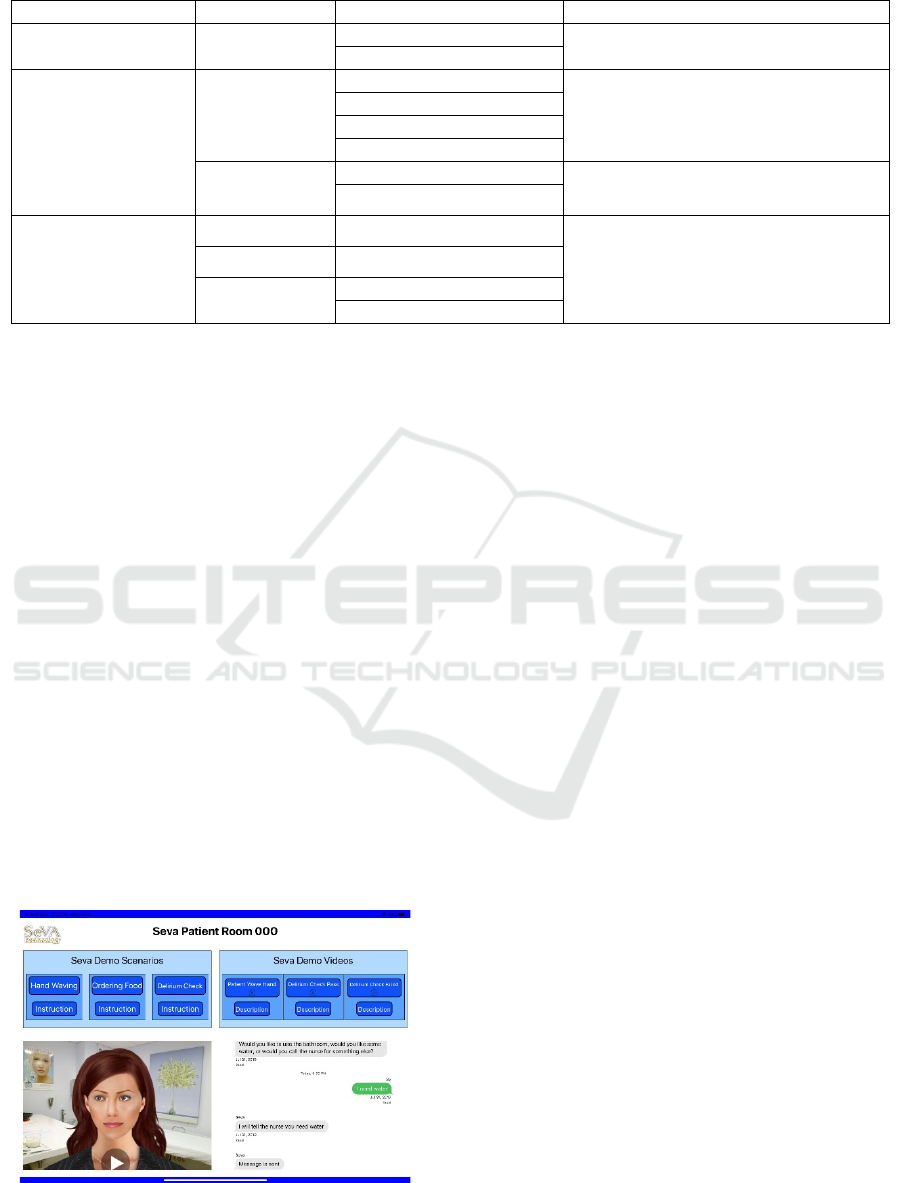
Table 1: SeVA skills in the Dialogflow.
Type Skill Story Description
Movement Response Sensor Response
Fall Detection
Response to patient and notify nurse by
recognize patient movement.
Wave
Regular Check
Hourly Rounding
Feeling Check
Perform regular hourly check to fulfil patient
needs actively.
Restroom Check
Brace Check
Heat pack Check
Delirium Check
What day is today
Perform regular delirium check to evaluate
patient cognition ability.
Spell weekdays in reversed order
Relaxations
Soothing Music Play Music
Use music, jokes, and small talk to improve
patient’s mental state.
Small Talk
Random Talk
Joke
Tell me a joke
More jokes
configuration pages for customizing user service. The
SMC app is deployed in the nurse room. It monitors
the status of all patients by receiving the messages
regularly from SPR and provides feedback to the
nurse immediately.
3.2.5 Monitoring Server
The SeVA backend server provides the monitoring
service. It monitors the API availability, the number
of connected nurses and patients, as well as the
backend server running status. Any abnormal
behaviors, such as backend server API unavailable or
no nurse online, will be reported to the operator
through the email service in the notification module.
4 IMPLEMENTATION
The mobile applications are written using Apple iOS
native program language Swift on Xcode 11, which
runs on the iOS device with iOS 13. The SeVA
backend server has 4 dedicated ARM processors with
2GB memory and the Ubuntu Xenial system.
Figure 4: SPR application user interface.
We use the Chatbot engine Dialogflow developed
by Google, LLC (Google, 2020). Dialogflow is a UI-
based platform for creating smart and proactive
chatbots. Our team’s medical experts define the skills
by setting the intent, trigger, and replies. A skill is
composed of inputs, slots, replies, actions, and
stories. Inputs define events that a bot can react to.
Slots are the memory of the bot for remembering
some information during the conversation. Replies
are all the possible sentences that a bot can reply to a
user. Stories define the logic behind a skill. The input
is classified by the RNN which has been trained with
the sample inputs we supplied. Once the intent
matches, it will continue the conversation in a
predefined way.
As shown in Table 1, the SeVA skill set includes
“Sensor Response”, “Hourly Rounding”, “Delirium
Check”, etc. Each skill contains multiple stories.
Regarding the stories of the “Sensor Response” skill,
when the patient is waving a hand for help, the story
“wave” will be triggered by the HTTPS post, and then
the chatbot engine will send the sentence to the story
part. The story part may contain the trigger of the next
story part, which will facilitate the program reuse. For
the story part of “Morning Check”: when the chatbot
engine receives the trigger, it will send the first
sentence to the SPR, then waits for the returning
sentence. The patient response will then be classified
as the intent “Yes” or “No”, which will continue to
different conversations.
The SPR provides the interaction between the
SeVA platform and the user. The user interface is
shown in Figure 4. Every user is required to register
so the personal profile will be created. After logging
in, the SPR will connect to the SeVA Backend server
through a WebSocket for communication. The
HEALTHINF 2021 - 14th International Conference on Health Informatics
588

conversation can be initiated by hand waving, using
the wake-up word, and simply touching the screen.
For privacy consideration, the SPR microphone is
turned off when there is no conversation and the
wake-up word feature is optional. The SPR will ask a
question every hour (except for the rest hour) to make
sure patient needs are satisfied. The SPR also can play
some of the music selected by the therapist which will
create a calm atmosphere for the patient and relieve
anxiety.
(a) Game “Connect Nodes” (b) Game “Click Animal”
Figure 5: The sample delirium check games embeded in the
SPR. (a) Game “Connect Nodes” for testing patient
visuospatial and executive functions, it require patient
connect numbered nodes in a given order. (b) Game “Click
Animal” for testing patient attention, it require patient click
the animal image which will disappear quickly.
When triggered, SPR starts checking the patient
delirium status by asking questions or launching the
delirium check game. For example, we use a modified
version of Alternating Trail Making from the
Montreal Cognitive Assessment for mental status
assessment in older adults (Julayanont & Nasreddine,
2017). In Figure 5, we display two delirium check
games. The first game “Connect Node” is used for
testing the visuospatial and executive ability. In this
game, the patient is required to connect nodes in a
certain order. If the patient fails the test, a message
will be immediately sent to the SMC. The second
game “Click Animal” tests the patient’s attention.
Pictures will be prompted and then they disappear.
The patient must click at all the animal picture. The
results of the test will also be sent to the SeVA Master
Control application.
Figure 6: SeVA Mater Control application user interface.
The SMC lets the nurse monitor the status of multiple
patient rooms and process the incoming request, as
shown in Figure 6. The SMC shows 6 sub-panels on
the screen. Each sub-panel contains buttons and a
textbox. It will display the request by flashing the
displayed buttons, and the nurse could click the
button to send back the acknowledge message. For
preventing the patient from falling, the SMC will
display the critical movement information like
“Patient is sitting up” on the textbox. Then the nurse
could make a timely intervention.
This system is being deployed at the Banner -
University Medicine Rehabilitation Institute. It has
gotten the approval of the Institutional Review Board
(IRB) and also obtained positive feedback from the
nursing staff at preliminary demonstrations.
5 CONCLUSION
The IoT architecture and AI-based SeVA platform
can improve healthcare quality and nursing
workflows by automating traditional standard clinical
and nursing practices in hospital settings. SeVA
platform implementation uses Artificial Emotional
Intelligence to build a monitoring and diagnosing
system. The system features include: starting a
conversation with the patient to check for delirium;
perform regular round checks to improve nursing
workflows and provide actionable items for nursing
care; detect critical events such as falls, detect
gestures and patient’s motion like walking, waving
for help, detecting emotion and providing
interventions like playing relaxing music. The system
reduces gaps from “Unsupervised Care Windows”
and provides a customized healthcare experience
catered to Age-Friendly Care. We are currently
testing and evaluating the feasibility of the current
SeVA: An AI Solution for Age Friendly Care of Hospitalized Older Adults
589

SeVA platform implementation in a hospital setting.
We are also investigating innovative methods to
quantify cognition and emotion with the goal to
recommend non-pharmacological interventions to
reduce stress during the hospital stay. We will
evaluate the system with patient and nurse surveys as
well as the alarm statistical metrics including True
Positive Rate, False Positive Rate, and False Negative
Rate.
ACKNOWLEDGEMENTS
This work is partly supported by the Air Force Office
of Scientific Research (AFOSR) Dynamic Data-
Driven Application Systems (DDDAS) award
number FA9550-18-1-0427, National Science
Foundation (NSF) research projects NSF-1624668
and NSF-1849113, (NSF) DUE-1303362
(Scholarship-for-Service), National Institute of
Standards and Technology (NIST) 70NANB18H263,
and Department of Energy/National Nuclear Security
Administration under Award Number(s) DE-
NA0003946.
REFERENCES
AHRQ.(2020). How do you measure fall rates and fall
prevention practices? Retrieved from https://
www.ahrq.gov/professionals/systems/hospital/fallpxto
olkit/fallpxtk5.html
Babylonhealth. (2020). Babylon health UK - the online
doctor and prescription services app. Retrieved from
https://www.babylonhealth.com/
Chaccour, K., Darazi, R., El Hassani, A. H., & Andres, E.
(2016). From fall detection to fall prevention: A generic
classification of fall-related systems. IEEE Sensors
Journal, 17 (3), 812–822.
Chung, K., & Park, R. C. (2019). Chatbot-based healthcare
service with a knowledge base for cloud computing.
Cluster Computing, 22 (1), 1925– 1937.
Churpek, M. M., Yuen, T. C., Huber, M. T., Park, S. Y.,
Hall, J. B., & Edelson, D. P. (2012). Predicting cardiac
arrest on the wards: a nested case-control study. Chest,
141 (5), 1170–1176.
Churpek, M. M., Yuen, T. C., Winslow, C., Robicsek, A.
A., Meltzer, D. O., Gibbons, R. D., & Edelson, D. P.
(2014). Multicenter development and validation of a
risk stratification tool for ward patients. American
Journal of Respiratory and Critical Care Medicine, 190
(6), 649–655.
Comendador, B. E. V., Francisco, B. M. B., Medenilla, J.
S., & Mae, S. (2015). Pharmabot: a pediatric generic
medicine consultant chatbot. Journal of Automation
and Control Engineering Vol, 3 (2).
Fadhil, A., & Gabrielli, S. (2017). Addressing challenges in
promoting healthy lifestyles: the al-chatbot approach.
In Proceedings of the 11th EAI International
Conference on Pervasive Computing Technologies for
Healthcare (pp. 261–265).
Google. (2020). Dialogflow | Google Cloud. Author.
Retrieved from https://cloud.google.com/dialogflow
Gu, X., Li, M., Cao, Y., & Xiong, L. (2019). Supporting
both range queries and frequency estimation with local
differential privacy. In 2019 IEEE Conference on
Communications and Network Security (CNS) (pp.
124–132).
Gu, X., Li, M., Cheng, Y., Xiong, L., & Cao, Y. (2020).
PCKV: Locally differentially private correlated key-
value data collection with optimized utility. In 29th
USENIX security symposium (USENIX security 20) (pp.
967–984).
Habib, M. A., Mohktar, M. S., Kamaruzzaman, S. B., Lim,
K. S., Pin, T. M., & Ibrahim, F. (2014). Smartphone-
based solutions for fall detection and prevention:
challenges and open issues. Sensors, 14 (4), 7181–
7208.
Health, B. (2020). Retrieved from https://www.
buoyhealth.com/
IBM. (2020). AI healthcare solutions. Retrieved from
https://www.ibm.com/watson-health
Inouye, S. K., Bogardus Jr, S. T., Charpentier, P. A., Leo-
Summers, L., Acam-pora, D., Holford, T. R., & Cooney
Jr, L. M. (1999). A multicomponent intervention to
prevent delirium in hospitalized older patients. New
England journal of medicine,340(9), 669–676.
Inouye, S. K., Marcantonio, E. R., Kosar, C. M., Tommet,
D., Schmitt, E. M., Travison, T. G., Jones, R. N. (2016).
The short-term and long-term relationship between
delirium and cognitive trajectory in older surgical
patients.
Alzheimer’s & Dementia, 12 (7), 766–775.
Julayanont, P., & Nasreddine, Z. S. (2017). Montreal
cognitive assessment (moca): concept and clinical
review. In Cognitive Screening Instruments (pp. 139–
195). Springer.
Marcantonio, E. R. (2017). Delirium in hospitalized older
adults. New England Journal of Medicine, 377(15),
pp.1456-1466.
Microsoft. (2020, Jul). Microsoft health bot project - ai at
work for your patients. Retrieved from https://www.
microsoft.com/en-us/research/project/health-bot/
Mitchell, M. D., Lavenberg, J. G., Trotta, R., & Umscheid,
C. A. (2014). Hourly rounding to improve nursing
responsiveness: a systematic review. The Journal of
nursing administration,44(9), 462.
Pacheco, J., & Hariri, S. (2016). IoT security framework for
smart cyberinfrastructures. In 2016 IEEE 1st
International workshops on Foundations and
Applications of self* systems (fas* w) (pp. 242–247).
PACT.(2020). Florence your health assistant. Retrieved
from https://www.florence.chat/
Paoli, C. J., Reynolds, M. A., Sinha, M., Gitlin, M., &
Crouser, E. (2018).Epidemiology and costs of sepsis
in the united states—an analysis based on timing of
HEALTHINF 2021 - 14th International Conference on Health Informatics
590

diagnosis and severity level. Critical care
medicine,46(12),1889.
Szep, J., Akoglu, A., Hariri, S., & Moukabary, T. (2018).
Two-level autonomousoptimizations based on ml for
cardiac fem simulations. In 2018 IEEE International
Conf. on Autonomic Computing (ICAC)(pp. 101–110).
Wu, T., Rappaport, T. S., & Collins, C. M. (2015). Safe for
generations to come: Considerations of safety for
millimeter waves in wireless communications. IEEE
Microwave Magazine, 16 (2), 65–84.
Xu, B., Da Xu, L., Cai, H., Xie, C., Hu, J., & Bu, F. (2014).
Ubiquitous data accessing method in IOT-based
information system for emergency medical services.
IEEE Transactions on Industrial informatics, 10 (2),
1578–1586.
Yu, K.-H., Beam, A. L., & Kohane, I. S. (2018). Artificial
intelligence in healthcare. Nature biomedical
engineering, 2 (10), 719–731.
SeVA: An AI Solution for Age Friendly Care of Hospitalized Older Adults
591
