
Development of a Miniaturized Motion Sensor for Tracking Warning
Signs of Low-back Pain
Jérôme Molimard
1
, Tristan Delettraz
1
and Etienne Ojardias
2
1
Mines Saint-Etienne, Univ. Lyon, Univ. Jean Monnet, INSERM, U 1059 Sainbiose,
Centre CIS, F - 42023 Saint-Etienne, France
2
Clinical Gerontology Department, University Hospital of Saint-Étienne, Saint-Étienne, France
Keywords: Low-Back Pain (LBP), Inertial Measurement Unit (IMU), Hip & Shoulder Dissociation, Lumbar Lordosis
Angle, Measuring Device.
Abstract: Low-back pain (LBP) is a widespread disease which can also be highly disabling, but physicians lack of
basic understanding and diagnosis tools. During this study, we have designed and built a new wearable
device capable of detecting features helpful in LBP follow-up while being non-invasive. The device has
been carefully validated, and shows good metrological features, with small noise level (σ = 1°) and no
observable drift. Two simple exercises were proposed to two young volunteers, one of them with LBP
history. These exercises are designed to target two characteristics: the lumbar lordosis angle and the hip &
shoulder dissociation. Even if no general rules can be extracted from this study, we have shown that Inertial
Measurement Units (IMU) are able to pick up those characteristics and the obtained values are meaningful
refereeing to LBP disease. Henceforth, we are confident in going to clinical studies to investigate the link
between back related feature and LBP, in particular the hip & shoulder dissociation which is poorly
documented.
1 INTRODUCTION
Low-back pain (LBP) is a widespread affliction in
most developed and industrialized countries. It is a
major disability factor both at work and in every-day
life (Bauer et al., 2017). Worldwide, it is the most
reported reason for seeking care from a primary care
physician (Traeger et al., 2017). LBP is accountable
for the most sick leaves and it touches 70% of
people at least once in his/her life (Koes et al.,
2006). Therefore, it costs the French government
more than one billion euros each year (Depont et al.,
2010). LBP care is difficult since about 90% of all
patients suffer “non-specific low-back pain” which
means that while the pain is apparent, its cause
remains unknown (Koes et al., 2006). Furthermore,
73% of patients experiencing LBP will go through
an other episode within a year (Koes et al., 2006)
which will usually be more painful than the last one
(Riihimäki et al., 1991).
Hence, a lot of scientific studies have been made
in order to find a way to better monitor the condition
of patients afflicted by LBP, among them the lumbar
lordosis angle (Evcik et al., 2003). Likewise, since
people afflicted by LBP may have trouble
performing normal muscle activities, like bending
their back sideways. The detection and
quantification of some abnormal minute back
movements, like the hip & shoulder dissociation
(Park et al., 2012), could establish a new method to
label the beginning of a serious illness. Both subjects
generated great interest in the medical community
(Baek et al., 2010).
Many methods to monitor those characteristics
have been put forward. For instance,
Electromyography (EMG) is the most popular
technique for muscle activity observation. EMGs
can measure various movements at a high rate, with
almost no added weight. Their most commonly
reported drawbacks are the difficulties to set up the
device and its sensors need to by applied sometimes
invasively under the skin of the patient (Butler et al.,
2010). Moreover, the results given by EMG still
need to be processed to get the desired displacement
or angle.
A popular alternative solution is the use of
optical motion capture system. Nevertheless, the
high cost of the cameras and markers may be a
Molimard, J., Delettraz, T. and Ojardias, E.
Development of a Miniaturized Motion Sensor for Tracking Warning Signs of Low-back Pain.
DOI: 10.5220/0010291701290134
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 1: BIODEVICES, pages 129-134
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
129

limiting factor to its usage, as well as the fact that it
can only handle movements contained in a closed
and limited area (Nakamoto et al., 2018).
Recently, strain sensors were successfully used
to monitor lumbar motion. They also can be made
wearable, unlike the previous two techniques.
Besides, they are lightweight and inexpensive,
which reinforce their portability (Nakamoto et al.,
2018). But their usage still is limited in space and
along one plane only. At the moment, an application
to accurately measure movements of the back from
top to bottom along three axes is still out of reach.
Last, inertial measurement units (IMUs) are
electronic devices composed of 2 or 3 sensors (3-
axes accelerometer, 3-axes gyroscope and optionally
3-axes magnetometer) that can report the
acceleration and orientation of one object using
Attitude and Heading Reference System (AHRS)
algorithm. They are small and can easily be
integrated in a wearable devices (Baek et al., 2010).
In addition, they can measure small motions and
rotations of the back along the axes with ease (Zhao
et al., 2017) and can be combined to tackle a larger
array of movements and be more accurate (Chhikara
et al., 2008). Last, the physical values obtained from
IMUs are very close to the displacements and angles
that are usually sought.
Many works emphased the real time features that
IMUs can provide in order to design a portable
measuring device to gather data on the everyday life
of an affected patient to better his treatment and
warn him of unsafe positions. Recently, Beange et
al. (2019) or Graham et al. (2020) proposed
applications of IMU to monition the spine in the
context of LBP.
The goal of this study is to provide physician a
measuring instrument that could be used to detect
and monitor back disorders. As such, the solution
must be low-cost, usable in a closed environment
without highly-dedicated technical skills. In the
following, we will present an IMU-based solution,
with detailed validation protocol, and give two first
application examples on movement tracking and hip
& shoulder dissociation.
2 MATERIAL AND METHODS
2.1 Device Elements
BackMonitor is an in-house system built on the
Feather M0 development board (Adafruit
Industries
©
, New York, USA), an Arduino
compatible processor that includes a Bluetooth Low
Energy (BLE) module. The sensor (BNO055 Bosch
Sensortec - Kusterdingen, Germany) is a 9 DOF
(accelerometer, gyroscope, and magnetometer) IMU
embedding an AHRS processing. Each sensor has a
size of 20mm×27mm×4mm, and weights 3 g; the
micro-controller board, can easily to be placed in the
trousers pocket (60mm×30mm×25mm, 30g).
2.2 Metrology
In the context of low-back pain monitoring, both
linear acceleration and Euler angles are useful,
respectively for hip & shoulder dissociation
detection and for the lumbar lordosis angle follow-
up. Those two quantities can be directly gathered
from the BNO055 (via an internal fusion algorithm).
BNO055 comes with autocalibration feature.
This process is a black box that ought to be verified
anyway. Acceleration can be 2-points checked easily
by using gravity, but rotation must be studied in
more details. Thus, a calibration protractor with
IMU holder was 3D printed to set angles with an
accuracy of 0.5°.
The angles were measured form each sensor and
in each axis between 0° and 165° every 5° for X and
Z directions and from 0° to 90° for Y direction
according to Euler angle definition. Moreover, the
board was initialized while being at 0°.
2.3 Assembly
The hardware layout for the simultaneous
measurement of data from two sensors is presented
in Fig.1, that shows the electronic circuit diagram.
The two BNO055s are connected to the Feather
M0 Bluefruit by I2C bus. Each BNO055 has a
specific address (respectively 0x29 and 0x28 from
left to right) depending on its ADR pin level.
Besides, a 110 mAh battery was followed by a
switch connected directly to the processor’s power.
It is necessary, since the goal is to conceive a
portable system. A changeover diode soldered onto
the board allows both the USB port and the battery
to be connected without any risks as the battery acts
as a backup power.
Three switches named A, B and C and a blue
LED were added for the user to select the reading
mode (hip & shoulder dissociation detection/lumbar
lordosis angle measure, serial/BLE connection, raw /
AHRS data).
BIODEVICES 2021 - 14th International Conference on Biomedical Electronics and Devices
130
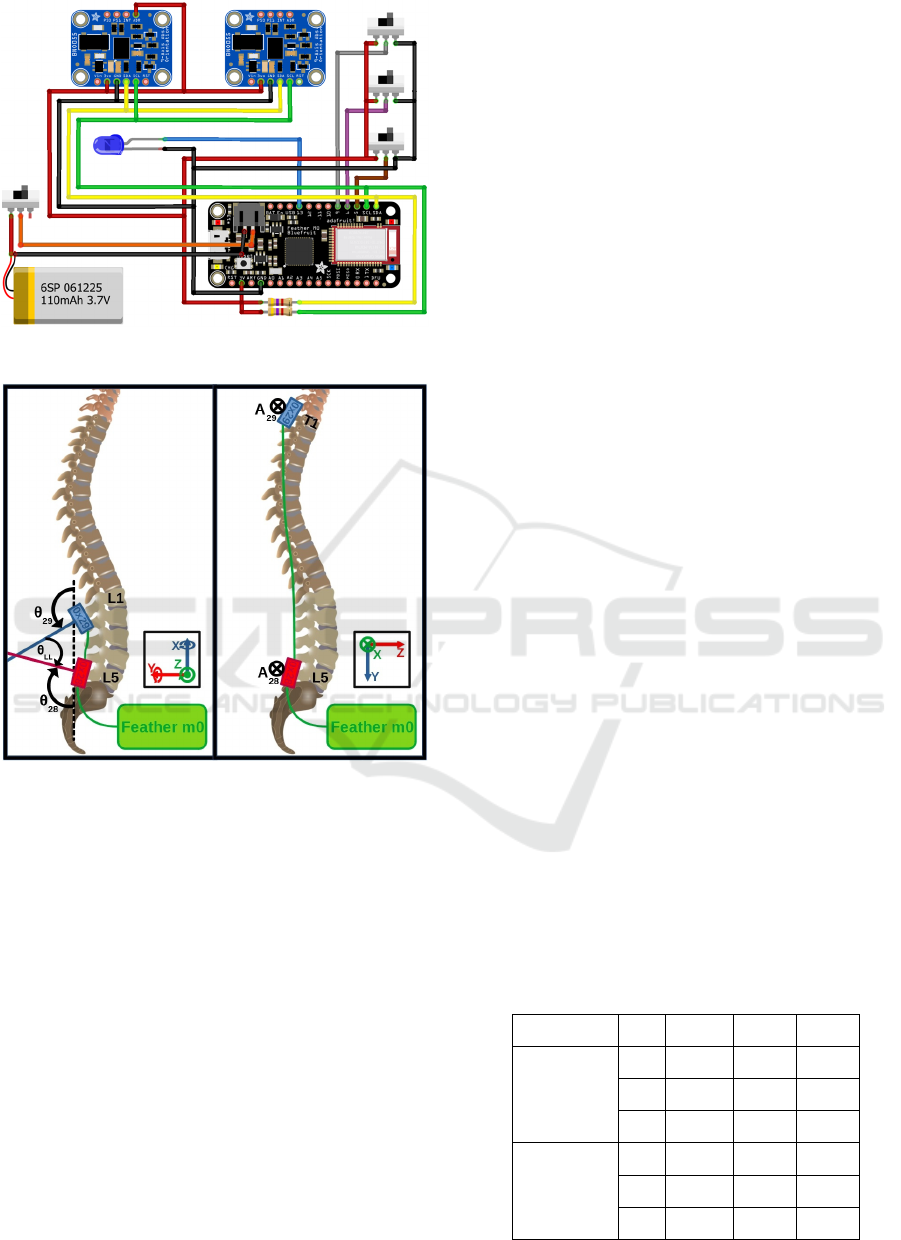
Figure 1: Electrical circuit diagram.
Figure 2: Position of the IMUs for both hip & shoulder
dissociation detection (right) and the lumbar lordosis angle
measure (left).
2.4 Sensors Arrangement
The sensor position along the patient’s back has
been set according to physicians usual practice
(Fig.2). Each sensor is stuck on the patient’s skin
with bio-compatible double-sided adhesive tape.
The lumbar lordosis angle is defined as the angle
formed by the tangent to the superior plate of the
transitional thoraco-lumbar vertebra the most
inclined on the horizontal, usually L1, and the
tangent to the inferior plate L5. Thus, one IMU
should be put over the L1 vertebra and one over the
L5 vertebra. The lumbar lordosis angle θ
LL
can be
defined as the difference between the Euler angles of
the IMUs along the Z axis θ
28
and θ
29
.
Detecting hip & shoulder dissociation is picking
up some conflicting accelerations between the upper
part of the back and the lower part of the back. As a
first suggestion, one IMU is placed over the highest
vertebra on the patient’s back T1, and one over the
lowest L5. The hip & shoulder dissociation will be
characterized as the phase difference between the
analytic signals obtained from IMU antero-posterior
accelerations A
28
and A
29
at T1 and L5.
2.5 Experimental Protocol
A first feasibility test is designed. The system is
tested on two volunteers. They are both youth
women with the same morphology, one with a
medical history of LBP and scoliosis (subject 1) and
the other one without any reported back-related issue
(subject 2).
Two simple exercises were proposed to the
subjects.
First, each subject was asked to sit down on a
chair for about 10 seconds, then, to stand up and to
stand still for the next 10 seconds. An object was
placed 50 cm in front of him and the subject was
asked to bend his back in order to pick it up. After
that, the patient stood up for 10 seconds once more
and then sat down for 10 seconds (Exercise 1).
Second, a time-up-and-go test is done: after 10
seconds on the chair, the patient was asked to walk
for about 3 m, turn back and then go back to the
chair and stay sit for 10 seconds (Exercise 2).
3 RESULTS
3.1 Metrology
Table 1 presents the slope and offset between the
angle given by the protractor and the measured one.
Most of the coefficients of determination R
2
are
higher that 0.99. The slope is close to 1 – and can be
corrected easily. X axis presents the higher
sensitivity drift for both sensors.
Table 1: Linearity parameters.
Sensor name Axis offset Slope R
2
0x28 X -0.5122 0.9312 0.9995
Y 1.2707 0.9844 0.9999
Z 1.6358 0.9879 0.9999
0x29 X -1.9851 0.9065 0.9973
Y 1.0071 0.9692 0.9998
Z 6.1829 0.9411 0.9993
Development of a Miniaturized Motion Sensor for Tracking Warning Signs of Low-back Pain
131
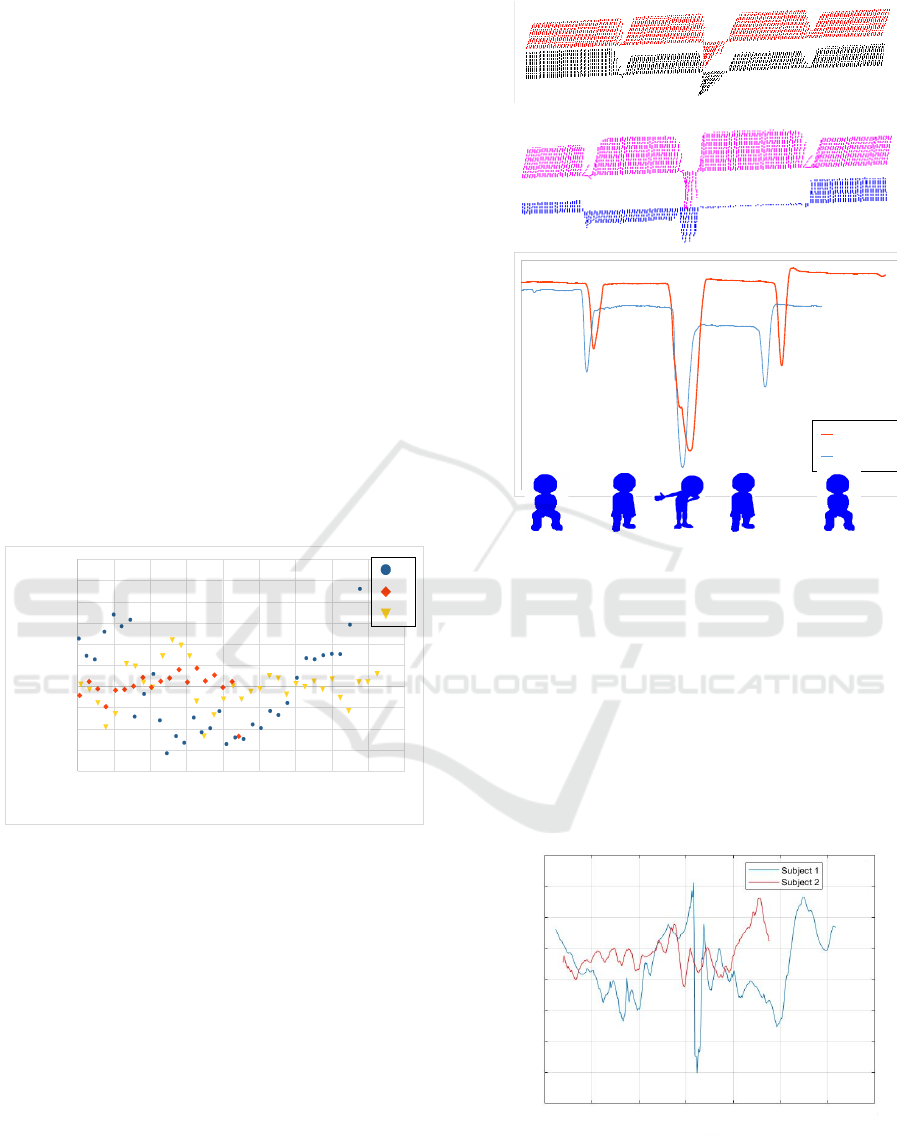
The residue between the best linear fit and the
experimental results are the same for 0x28 and 0x29.
For Y and Z directions, the residues are essentially
random. In the X direction, a 2
nd
order bias appears
and can be easily corrected. In these conditions, the
standard deviation σ is less than 1° (Fig.3).
The IMUs did not show any measurable drift
over a time period of 10 min. Identically, the
calibration procedure was performed 10 days after
the fist measure, and results were in close
agreement. Therefore, it was concluded that
reproducibility was good enough and that this point
was not an issue.
Last, the BNO055 coming with an auto-
calibration feature running after every starting up, it
is worth checking the BON055 measurement
stability. Measurement at 0° and 75° were performed
while varying the starting position. For the Y and Z
direction, and for both IMUs, the returned value
barely changed with the starting position but it was
concluded that the X value was zeroed at the start
whatever the real starting angle. Hence, it is required
to build a stand for the IMUs so that the initial value
for the X axis to be stable for both sensors.
Figure 3: Residues for Euler angles (in degrees) on 0x28.
3.2 Feasability Tests
Fig. 4 presents the sensor 0x28 and 0x29
orientations versus time for the two subjects
performing Exercise 1. Sensors are represented by a
stick corresponding to their longitudinal axis (Y
*
).
The lumbar lordosis angle is calculated from the
angle over the Z axis as follow:
θ
LL
= −180° − θ
28
− θ
29
(1)
Finally, the lumbar lordosis angle corresponding
to each subject was obtained by averaging the values
while standing up.
Figure 4: Sensor orientation and lumbar lordosis angle for
subject 1 and 2 during Exercise 1.
For the hip & shoulder dissociation detection,
charts of linear accelerations along all axis have
been produced. The parts where the subject was sat
down were remove because they were irrelevant
(mostly null) and to better focus on the moving part
of the experiment. As the goal is to pick up an offset
between the two IMUs, analytical signals on the
linear accelerations for the Z axis were calculated
with OCTAVE (Eaton, 2019) in order to find raw
phase differences (Fig.5).
Figure 5: Hip & shoulder phase difference for antero-
posterior (Z) acceleration.
0 20406080100120140160180
-2
-1,5
-1
-0,5
0
0,5
1
1,5
2
2,5
3
X
Y
Z
Angl e (° )
Res i dues ( ° )
Subject 1
Subject 2
0x29
0x28
0x29
0x28
Subject 1
Subject 2
0°
180°
Antero-posterior phase difference (°)
0612
0
180
- 180
Time (s)
BIODEVICES 2021 - 14th International Conference on Biomedical Electronics and Devices
132

4 DISCUSSION
The metrological results showed that the sensor
arrangement gives reliable results, with a
repeatability σ = 1° and no observable drift.
A first test was done, with two women of
comparable age and morphology, one with LBP
history and the other without. Of course, these
results cannot have any statistical meaning;
nevertheless, they have a demonstrative interest.
During Exercise 1, the patient afflicted by LBP
(subject 1) has a mean lumbar lordosis angle in
stand-up phase of −19° and the other −48°. The
lumbar lordosis angle being considered as natural in
the range −45°±9°, subject 1 is out of the safe
interval, unlike subject 2 who is not afflicted by
LBP. Fig. 4 shows a difference between the lumbar
lordosis angle value in stationary stand-up phase
between the 2 subjects. While subject 2’s angle
varies from −25° to −60°, subject 1’s angle stays
always close to −20°. Subject 1’s movements appear
as more restricted in range than subject 2’s. More,
subject 1’s movements are slower than subject 2’s.
This is in agreement with previous works stating a
decrease both in speed and in range of motion for
LBP patients (Errabity et al., 2020).
Exercise 2 focuses on acceleration, and it is
possible to extract basic gait analysis information.
For example here, subject 1 was about 2s slower
than subject 2. But, much detailed observations can
be done: while subject 1’s steps keep a similar shape
and range through time, subject 2’s are fluctuating
through time. The pain might force subject 1 to limit
her walking strategy to few movements while
subject 2 can freely adapt her movements to the
current stance.
The hip & shoulder dissociation presented as a
phase difference on Fig.5 discriminates the two
subjects. Indeed, at the turning point (t ≈ 6.5 s), the
T1 and L5 vertebrae of subject 1 are nearly in
opposition of phase with the lower part of the back
lagging behind the upper part. This is not seen in
subject 2’s case as the phase when turning back (t ≈
5.5 s) is not much different than when subject 2 is
walking. Henceforth, the hip & shoulder dissociation
could be detected for the subject with LBP and not
for the healthy one using phase analysis.
5 CONCLUSION
During this study, we have designed and built a new
wearable device capable of detecting features
helpful in LBP follow-up while being non-invasive.
The metrological validation of BackMonitor
arrangement shows good features, with small noise
level (σ = 1°) and no observable drift.
Two simple exercises, one combining stand-up,
sit and bending movements, the other being a
classical time-up-and-go test, were proposed to two
young volunteers, one of them with a LBP history.
Signal was processed to extract the lordosis angle
and hip & shoulder dissociation. Even if no general
rules can be extracted from this study, we have
shown that IMUs are able to pick up those
characteristics and the obtained values are
meaningful refereeing to LBP disease.
Hence, we are confident in going to clinical
studies to elaborate the link between back related
feature and LBP, in particular the hip & shoulder
dissociation which is poorly documented.
REFERENCES
Bauer, C., Rast, F., Ernst, M., Meichtry, A., Kool, J.,
Rissanen, S., Suni, J., and Kankaanpää, M., 2017. The
effect of muscle fatigue and low back pain on lumbar
movement variability and complexity. Journal of
Electromyography and Kinesiology, 33, 94–102.
Traeger, A., Buchbinder, R., Harris, I., and Maher, C.,
2017. Diagnosis and management of low-back pain in
primary care. CMAJ, 189(45), E1386–E1395.
Koes, B., Van Tulder, M., and Thomas, S., 2006.
Diagnosis and treatment of low back pain. BMJ,
332(7555), 1430–1434.
Depont, F., Hunsche, E., Abouelfath, A., Diatta, T., Addra,
I., Grelaud, A., Lagnaoui, R., Molimard, M., and
Moore, N., 2010. Medical and non-medical direct
costs of chronic low back pain in patients consulting
primary care physicians in France. Fundamental &
clinical pharmacology, 24 (1), 101–108.
Riihimäki, H., 1991. Low-back pain, its origin and risk
indicators. Scandinavian journal of work, environment
& health, 81–90.
Evcik, D., and Yücel, A., 2003. Lumbar lordosis in acute
and chronic low back pain patients. Rheumatology
international, 23 (4), 163–165.
Park, W.-H., Kim, Y. H., Lee, T. R., and Sung, P. S., 2012.
Factors affecting shoulder–pelvic integration during
axial trunk rotation in subjects with recurrent low
back pain. European Spine Journal, 21 (7), 1316–
1323.
Baek, J., and Yun, B.-J., 2010. Posture monitoring system
for context awareness in mobile computing. IEEE
Transactions on instrumentation and measurement, 59
(6), 1589–1599.
Butler, H. L., Lariviere, C., Hubley-Kozey, C. L., and
Sullivan, M. J., 2010. Directed attention alters the
temporal activation patterns of back extensors during
Development of a Miniaturized Motion Sensor for Tracking Warning Signs of Low-back Pain
133

trunk flexion–extension in individuals with chronic low
back pain. European Spine Journal, 19 (9), 1508–
1516.
Nakamoto, H., Yamaji, T., Yamamoto, A., Ootaka, H.,
Bessho, Y., Kobayashi, F., and Ono, R., 2018.
Wearable lumbar-motion monitoring device with
stretchable strain sensors. Journal of Sensors. Article
ID 7480528, 7 pages.
Zhao, H., Wang, Z., Qiu, S., Shen, Y., and Wang, J., 2017.
IMU-based gait analysis for rehabilitation assessment
of patients with gait disorders. In 2017 4th
International Conference on Systems and Informatics
(ICSAI), IEEE, 622–626.
Chhikara, A., Rice, A., McGregor, A. H., and Bello, F.,
2008. Wearable device for monitoring disability
associated with low back pain. World, 10, p. 13.
Beange, K. H., Chan, A. D., Beaudette, S. M., Graham, R.
B., (2019). Concurrent validity of a wearable IMU for
objective assessments of functional movement quality
and control of the lumbar spine. Journal of
Biomechanics, 97, 109356.
Graham, R. B., Dupeyron, A., van Dieën, J. H., 2020.
Between-day reliability of IMU-derived spine control
metrics in patients with low back pain. Journal of
Biomechanics, 113, 110080.
Eaton, J.W., Bateman, D., Hauberg, S., Wehbring, R.,
2019. GNU Octave version 5.2.0 manual: a high-level
interactive language for numerical computations,
online reference: https://www.gnu.org/software/
octave/doc/v5.2.0/.
Errabity, A., Han, W.-S.,Bonnaire, R., Pannetier,, R.,
Molimard, J., 2020. Lumbar spine kinematics in
people with and without low back pain: a systematic
review. Applied Ergonomics, under submission.
BIODEVICES 2021 - 14th International Conference on Biomedical Electronics and Devices
134
